Infection with carcinogenic types of human papillomavirus (HPV) is necessary for the development of cervical intraepithelial neoplasia (CIN).1,2 The development of high-grade CIN and progression to cancer are associated with persistent infection with carcinogenic HPV.3,4 Because older women are at increased risk for invasive cervical carcinoma, investigation into the prevalence of infection with carcinogenic HPV and associations with cervical cytologic abnormalities in this group will help to clarify the role of HPV in the development of cervical cancer.
Two peaks in the prevalence of infection with carcinogenic HPV have been identified among Costa Rican women: one among women aged less than 25 years and one among women over the age of 59 years.5 From May 1998 to January 1999, we conducted a population-based survey of women aged 15–49 years in the province of Ontario, from which we reported a peak prevalence among women aged 20–24 years and a significantly higher prevalence among women aged 45–49 years compared with women aged 40–44 years.6 To explore the upward trend, we extended our investigation of prevalence and risk factors to women aged 50 years and more, using the same methodology as in our earlier survey.
Fifteen of the family practices that participated in our earlier survey also participated in the survey of older women, conducted from September 1999 to May 2000. Women visiting their family physician for annual cytologic screening were recruited according to 2:3 random sampling, later amended to 1:1 to attain the required numbers in a timely manner. The recruited women provided written, informed consent and completed a questionnaire concerning risk factors. Extension of the survey to older women was approved by the St. Joseph's Healthcare Research Ethics Board, Hamilton, Ont.
The clinical procedure, specimen transport and laboratory analyses by the hybrid capture II (HCII) assay and polymerase chain reaction (PCR) have been described previously.6 HCII detects the presence of one or more of a group of 13 carcinogenic types of HPV (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68); PCR with genotyping detects any of the same 13 carcinogenic genotypes as well as 4 noncarcinogenic types (6, 11, 42 and 53) (data not provided here). Specimens were excluded from the analysis of PCR results if they remained β-globin-negative after dilution to reduce the effect of inhibitors and to control for the presence of tissue DNA.
Samples were obtained from 156 of the 167 women eligible for the study (refusal rate 6.6%); 56 were aged 50–54 years, 47 were aged 55–59 years and 53 were aged 60 years or more. Two specimens were inadequate for PCR testing, because they did not contain intact DNA. Carcinogenic HPV was detected by the HCII assay in 8.3% (13/156) of the women and by PCR in 3.2% (5/154); 9.6% (15/156) of the women were HPV-positive by either test. The prevalence rates in this group of women and in the younger women surveyed previously are shown by age group in Fig. 1. We calculated a moving average across the age groups (k – 3) to smooth the fluctuations in data and to show the prevalence rates more clearly, while maintaining consistency with the presentation of data from the earlier survey.
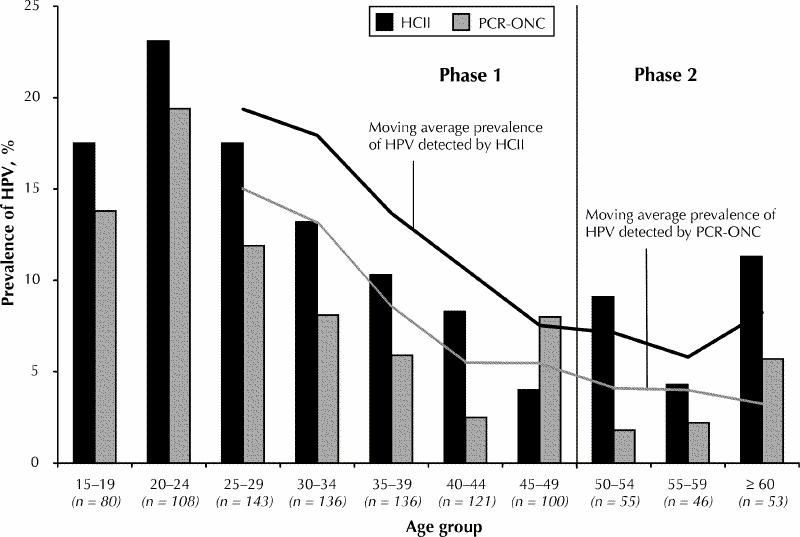
Fig. 1: Age-specific prevalence rates of infection with human papillomavirus (HPV) as detected by the hybrid capture II (HCII) assay (a test for carcinogenic types of HPV) and the polymerase chain reaction with probing for carcinogenic types of HPV (PCR-ONC). The data are for 824 women aged 15–49 years, for whom the results were reported previously (phase 1),6 and 154 women aged 50 years and more for whom the results of both tests were available (phase 2).
We performed univariate logistic regression analyses for factors associated with the presence of carcinogenic HPV as detected by the HCII assay using the putative risk factors tested previously in younger women, namely, cervical cytologic results (negative, atypical squamous cells of undetermined significance [ASCUS], low-grade squamous intraepithelial lesions [LSIL] or high-grade squamous intraepithelial lesions [HSIL]), previous abnormal cytologic results, treatment for CIN, geographic region, marital status, lifetime number of sexual partners, number of sexual partners in the past year, age at first intercourse, parity, current smoking status and current use of oral contraceptives. The number of women using oral contraceptives in this older group was very low (4), and none of the women reported having more than 1 sexual partner in the past year.
Age below the median at first intercourse (20 years) was significantly associated with the presence of carcinogenic HPV as detected by the HCII assay (odds ratio [OR] 4.4, 95% confidence interval [CI] 1.2–16.7; p = 0.03). Women who did not appear to have a stable sexual partnership (those who were single, separated or divorced) were significantly more likely to be HPV-positive than women who were cohabiting (OR 6.7, 95% CI 1.9–23.6; p = 0.003). Multivariate logistic regression analyses performed with age at first intercourse and marital status revealed that both age less than 20 years at first intercourse and apparent absence of a stable sexual partnership remained statistically significant (OR 5.4, 95% CI 1.3–22.6, and OR 8.1, 95% CI 2.0–31.9, respectively).
The high prevalence of HPV among the women aged 60 years or more is consistent with the second peak after the age of 59 years among Costa Rican women.5 We have previously suggested that, after infection, HPV may become latent and then be reactivated in some women as they age and immune surveillance decreases.6
Our finding of an association between young age at first intercourse and the presence of carcinogenic HPV is also consistent with findings in other studies.7,8 The other factors that we examined were consistent with those investigated in women aged 15–49 years but may have limited meaning for older women, because sexual behaviour changes over a lifetime, and infection might have been acquired much earlier in connection with different behaviours.
Because persistent HPV infection is associated with increased risk of CIN and lesion progression,3,7,8 and because carcinogenic HPV was relatively common in these older women, longitudinal studies of Canadian women across age groups would help to clarify the natural history of HPV infection and the pathogenesis of invasive cervical carcinoma.
Acknowledgments
Funding was provided as a research grant by the Division of STD Prevention and Control, Bureau of HIV/AIDS and STD, Health Canada, and as an unrestricted research grant by the Pharmaceuticals Division, 3M Corporation, Minneapolis, Minn. The HCII kits were provided at no charge by Digene Corporation. We extend our sincere thanks to Dr. Margaret Fearon, Ontario Public Health Laboratories, Toronto, Ont., for the assistance provided to the project.
Footnotes
This article has been peer reviewed.
Contributors: All authors contributed ideas to this paper. Dr. Sellors contributed to the study design and reviewed the manuscript for important intellectual content. Ms. Karwalajtys coordinated the data collection, analyzed data and drafted the manuscript. Dr. Kaczorowski contributed to the study design and supervised the analysis and reporting of results. Dr. Mahony contributed to the study design and coordinated the laboratory analysis. Dr. Lytwyn contributed to the study design. Ms. Chong performed analyses and contributed to the reporting of results. Ms. Sparrow coordinated the data collection and performed initial analyses. Dr. Lorincz contributed to the study design. Drs. Mahony, Lytwyn and Lorincz and Ms. Sparrow reviewed the manuscript for important intellectual content.
Competing interests: Dr. Sellors received partial support from Digene Corporation to attend a conference on HPV and the health economics of cervical cancer prevention in Geneva, Switzerland, in 2001. Dr. Lorincz is an employee of Digene Corporation. None declared for Ms. Karwalajtys, Dr. Kaczorowski, Dr. Mahony, Dr. Lytwyn, Ms. Chong and Ms. Sparrow.
Correspondence to: Dr. John W. Sellors, Program for Appropriate Technology in Health, 1455 NW Leary Way, Seattle WA 98107, USA; fax 206 285-6619; jsellors@path.org
References
- 1.Walboomers JMM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999;189:1-3. [DOI] [PubMed]
- 2.Munoz N. Human papillomavirus and cancer: the epidemiological evidence. J Clin Virol 2000;19(1-2):1-5. [DOI] [PubMed]
- 3.Remmink AJJ, Walboomers JMM, Helmerhorst TJM, Voorhorst FJ, Rozendaal L, Risse EKJ, et al. The presence of persistent high-risk HPV genotypes in dysplastic cervical lesions is associated with progressive disease: natural history up to 36 months. Int J Cancer 1995;61:306-11. [DOI] [PubMed]
- 4.Schlecht NF, Kulaga S, Robitaille J, Ferreira S, Santos M, Miyamura RA, et al. Persistent human papillomavirus infection as a predictor of cervical intraepithelial neoplasia. JAMA 2001;286:3106-14. [DOI] [PubMed]
- 5.Herrero R, Schiffman MH, Bratti C, Hildesheim A, Balmaceda I, Sherman ME, et al. Design and methods of a population-based natural history study of cervical neoplasia in a rural province of Costa Rica: the Guanacaste Project. Pan Am J Public Health 1997;1:362-75. [DOI] [PubMed]
- 6.Sellors JW, Mahony JB, Kaczorowski J, Lytwyn A, Bangura H, Chong S, et al. Prevalence and predictors of human papillomavirus infection in women in Ontario, Canada. CMAJ 2000;163(5):503-8. [PMC free article] [PubMed]
- 7.Ho GYF, Bierman R, Beardsley L, Chang CJ, Burk RD. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998;338:423-8. [DOI] [PubMed]
- 8.Koutsky LA, Holmes KK, Critchlow CW, Stevens CE, Paavonen J, Beckmann AM, et al. A cohort study of the risk of intraepithelial neoplasia grade 2 or 3 in relation to papillomavirus infection. N Engl J Med 1992;327:1272-8. [DOI] [PubMed]


