Abstract
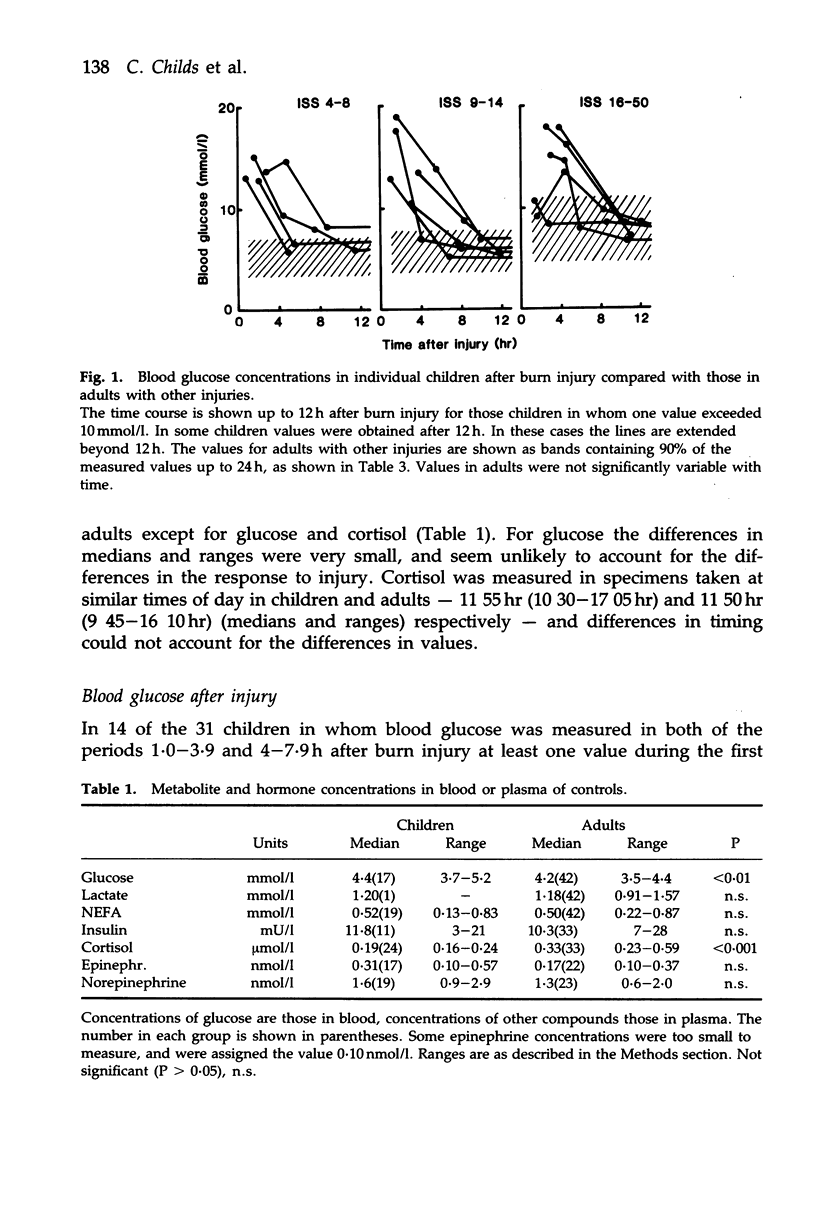
Plasma and blood metabolites were measured in 31 children over the first day after burn injury. In 14 of them blood glucose peaked, rising within 1-4h to 10-20 mmol/l and then falling, by 4-8 h, to 5-10 mmol/l. Usually the peak value preceded treatment and the fall occurred during infusion of dextrose-saline. Peak incidence was independent of burn severity. There was no evidence of similar peaks in children or adults with other injuries, or in 8 adults with burn injuries; through high glucose levels have been reported in children with head injuries. Lactate, non-esterified fatty acids, insulin, cortisol, epinephrine and norepinephrine were also measured. Values in the first 4 h were similar to those reported in adults with other injuries, except for lactate, which rose less in the children. Unexpectedly, the hyperglycemia in the children with burns was poorly related to epinephrine concentration at all times to 24h. Insulin resistance probably developed within the first hour or two; but from 8 h did not seem to depend on synergism between epinephrine and cortisol.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baker S. P., O'Neill B., Haddon W., Jr, Long W. B. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974 Mar;14(3):187–196. [PubMed] [Google Scholar]
- Barton R. N. Neuroendocrine mobilization of body fuels after injury. Br Med Bull. 1985 Jul;41(3):218–225. doi: 10.1093/oxfordjournals.bmb.a072054. [DOI] [PubMed] [Google Scholar]
- Bessey P. Q., Watters J. M., Aoki T. T., Wilmore D. W. Combined hormonal infusion simulates the metabolic response to injury. Ann Surg. 1984 Sep;200(3):264–281. doi: 10.1097/00000658-198409000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clutter W. E., Bier D. M., Shah S. D., Cryer P. E. Epinephrine plasma metabolic clearance rates and physiologic thresholds for metabolic and hemodynamic actions in man. J Clin Invest. 1980 Jul;66(1):94–101. doi: 10.1172/JCI109840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copes W. S., Champion H. R., Sacco W. J., Lawnick M. M., Keast S. L., Bain L. W. The Injury Severity Score revisited. J Trauma. 1988 Jan;28(1):69–77. doi: 10.1097/00005373-198801000-00010. [DOI] [PubMed] [Google Scholar]
- Copes W. S., Lawnick M., Champion H. R., Sacco W. J. A comparison of Abbreviated Injury Scale 1980 and 1985 versions. J Trauma. 1988 Jan;28(1):78–86. doi: 10.1097/00005373-198801000-00011. [DOI] [PubMed] [Google Scholar]
- Eigler N., Saccà L., Sherwin R. S. Synergistic interactions of physiologic increments of glucagon, epinephrine, and cortisol in the dog: a model for stress-induced hyperglycemia. J Clin Invest. 1979 Jan;63(1):114–123. doi: 10.1172/JCI109264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frayn K. N. Hormonal control of metabolism in trauma and sepsis. Clin Endocrinol (Oxf) 1986 May;24(5):577–599. doi: 10.1111/j.1365-2265.1986.tb03288.x. [DOI] [PubMed] [Google Scholar]
- Frayn K. N. Insulin secretion after injuries of differing severity in the rat. Br J Exp Pathol. 1976 Jun;57(3):316–320. [PMC free article] [PubMed] [Google Scholar]
- Frayn K. N., Little R. A., Maycock P. F., Stoner H. B. The relationship of plasma catecholamines to acute metabolic and hormonal responses to injury in man. Circ Shock. 1985;16(3):229–240. [PubMed] [Google Scholar]
- Frayn K. N., Maycock P. F. Sample preparation with ion-exchange resin before liquid-chromatographic determination of plasma catecholamines. Clin Chem. 1983 Jul;29(7):1426–1428. [PubMed] [Google Scholar]
- Gelfand R. A., Matthews D. E., Bier D. M., Sherwin R. S. Role of counterregulatory hormones in the catabolic response to stress. J Clin Invest. 1984 Dec;74(6):2238–2248. doi: 10.1172/JCI111650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottstein U., Held K., Sebening H., Walpurger G. Der Glucoseverbrauch des menschlichen Gehirns unter dem Einfluss intravenöser Infusionen von Glucose, Glucagon und Glucose-Insulin. Klin Wochenschr. 1965 Sep 15;43(18):965–975. doi: 10.1007/BF01747857. [DOI] [PubMed] [Google Scholar]
- Heath D. F., Corney P. L. The effects of starvation, environmental temperature and injury on the rate of disposal of glucose by the rat. Biochem J. 1973 Nov;136(3):519–530. doi: 10.1042/bj1360519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson R. A., Hamling J. B., Blix P. M., Sim B. M., Hawa M. I., Jaspan J. B., Belin J., Nabarro J. D. The influence of graded hyperglycemia with and without physiological hyperinsulinemia on forearm glucose uptake and other metabolic responses in man. J Clin Endocrinol Metab. 1986 Sep;63(3):594–604. doi: 10.1210/jcem-63-3-594. [DOI] [PubMed] [Google Scholar]
- Little R. A., Stoner H. B., Frayn K. N. Substrate oxidation shortly after accidental injury in man. Clin Sci (Lond) 1981 Dec;61(6):789–791. doi: 10.1042/cs0610789. [DOI] [PubMed] [Google Scholar]
- Nilsson L. H. Liver glycogen content in man in the postabsorptive state. Scand J Clin Lab Invest. 1973 Dec;32(4):317–323. doi: 10.3109/00365517309084354. [DOI] [PubMed] [Google Scholar]
- Parish R. A., Webb K. S. Hyperglycemia is not a poor prognostic sign in head-injured children. J Trauma. 1988 Apr;28(4):517–519. doi: 10.1097/00005373-198804000-00017. [DOI] [PubMed] [Google Scholar]
- Saccà L., Vigorito C., Cicala M., Corso G., Sherwin R. S. Role of gluconeogenesis in epinephrine-stimulated hepatic glucose production in humans. Am J Physiol. 1983 Sep;245(3):E294–E302. doi: 10.1152/ajpendo.1983.245.3.E294. [DOI] [PubMed] [Google Scholar]
- Shamoon H., Hendler R., Sherwin R. S. Synergistic interactions among antiinsulin hormones in the pathogenesis of stress hyperglycemia in humans. J Clin Endocrinol Metab. 1981 Jun;52(6):1235–1241. doi: 10.1210/jcem-52-6-1235. [DOI] [PubMed] [Google Scholar]
- Stoner H. B., Frayn K. N., Barton R. N., Threlfall C. J., Little R. A. The relationships between plasma substrates and hormones and the severity of injury in 277 recently injured patients. Clin Sci (Lond) 1979 Jan;56(6):563–573. doi: 10.1042/cs0560563. [DOI] [PubMed] [Google Scholar]
- Vitek V., Lang D. J., Cowley R. A. Admission serum insulin and glucose levels in 247 accident victims. Clin Chim Acta. 1979 Jul 2;95(1):93–104. doi: 10.1016/0009-8981(79)90341-3. [DOI] [PubMed] [Google Scholar]
- WALKER W. F., ZILELI M. S., REUTTER F. W., SHOEMAKER W. C., FRIEND D., MOORE F. D. Adrenal medullary secretion in hemorrhagic shock. Am J Physiol. 1959 Oct;197:773–780. doi: 10.1152/ajplegacy.1959.197.4.773. [DOI] [PubMed] [Google Scholar]
- Yki-Järvinen H., Young A. A., Lamkin C., Foley J. E. Kinetics of glucose disposal in whole body and across the forearm in man. J Clin Invest. 1987 Jun;79(6):1713–1719. doi: 10.1172/JCI113011. [DOI] [PMC free article] [PubMed] [Google Scholar]


