Abstract
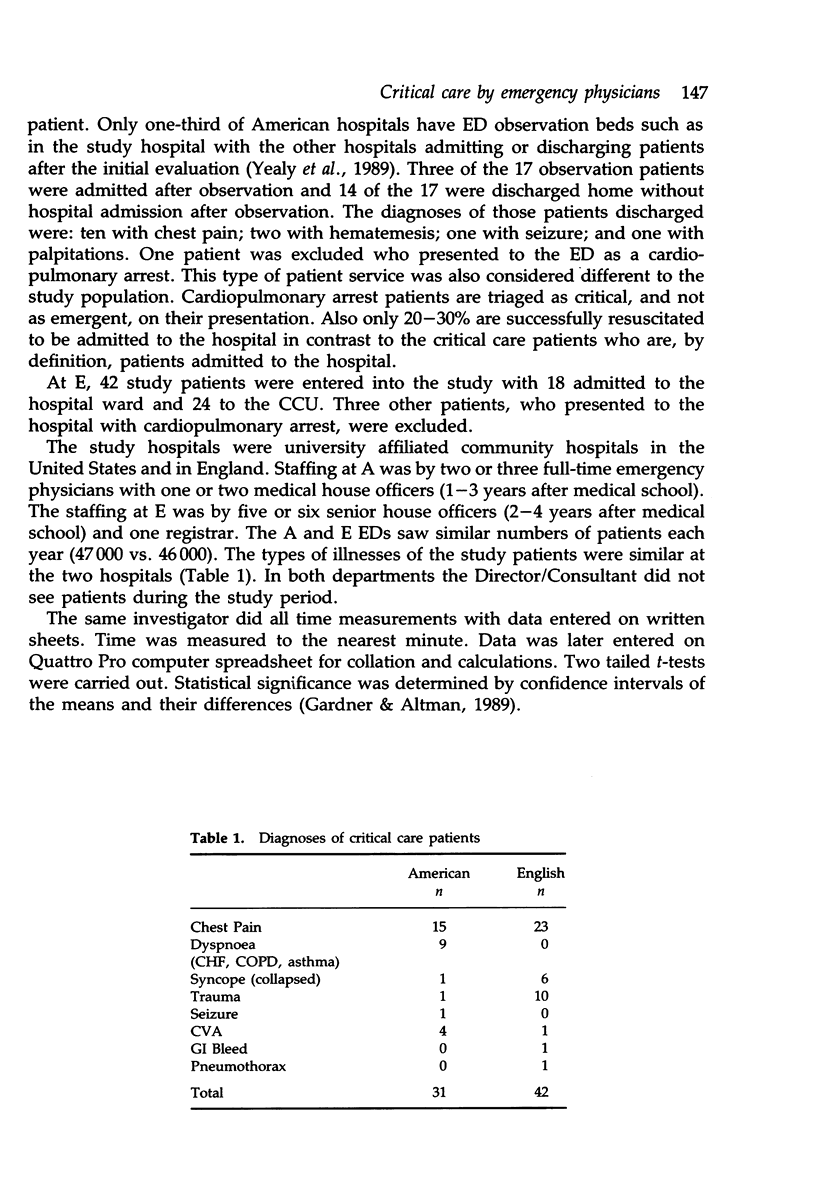
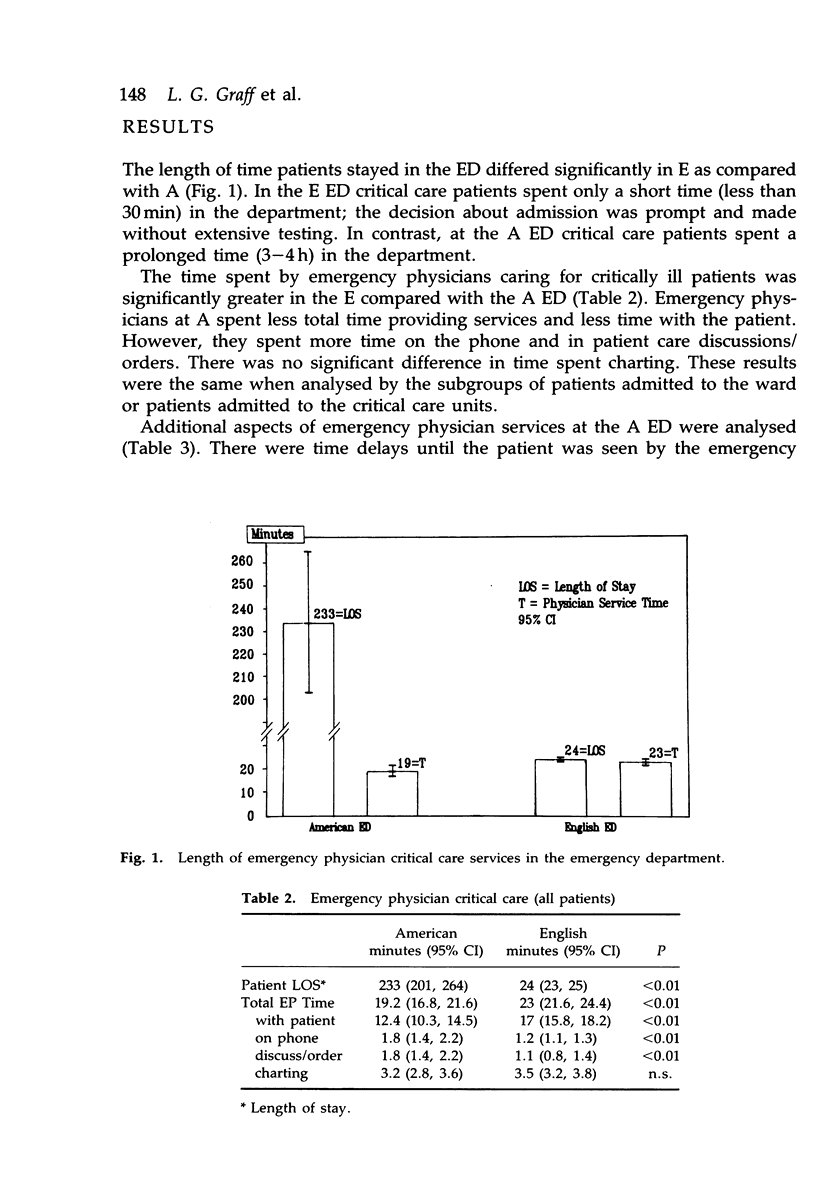
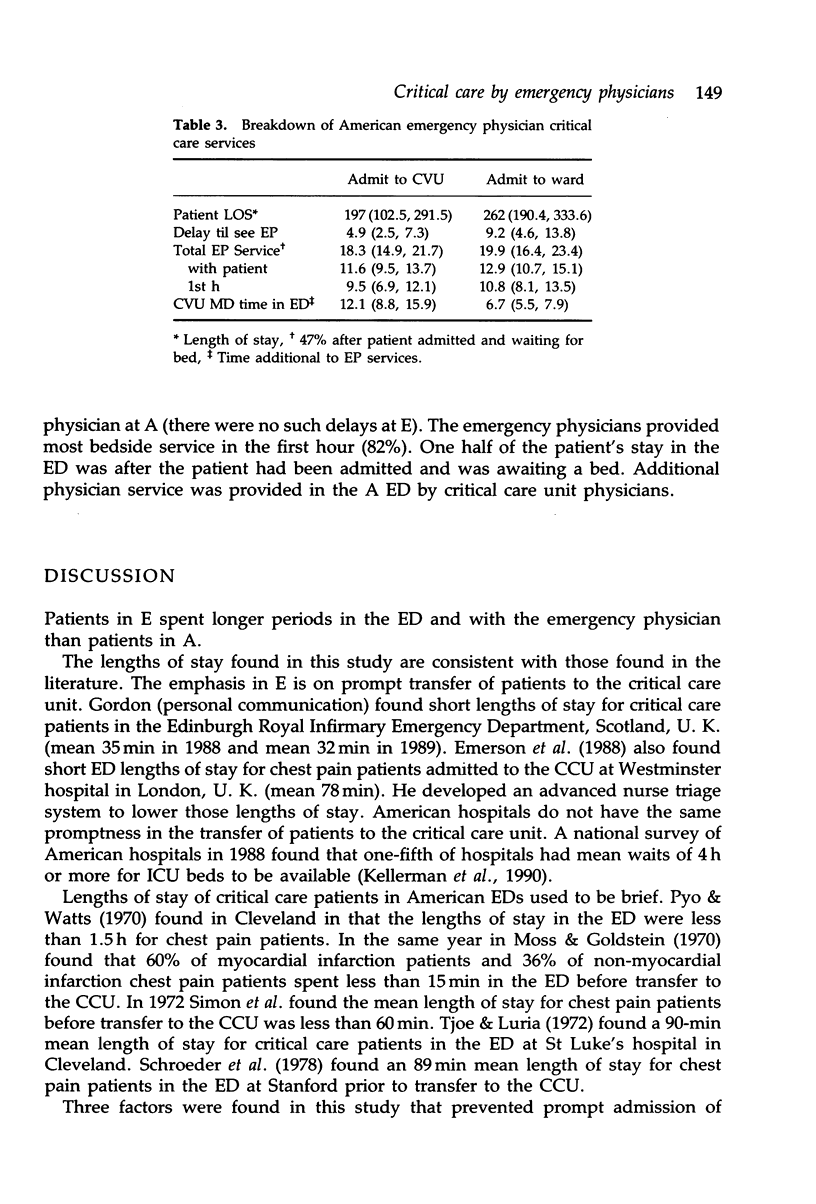
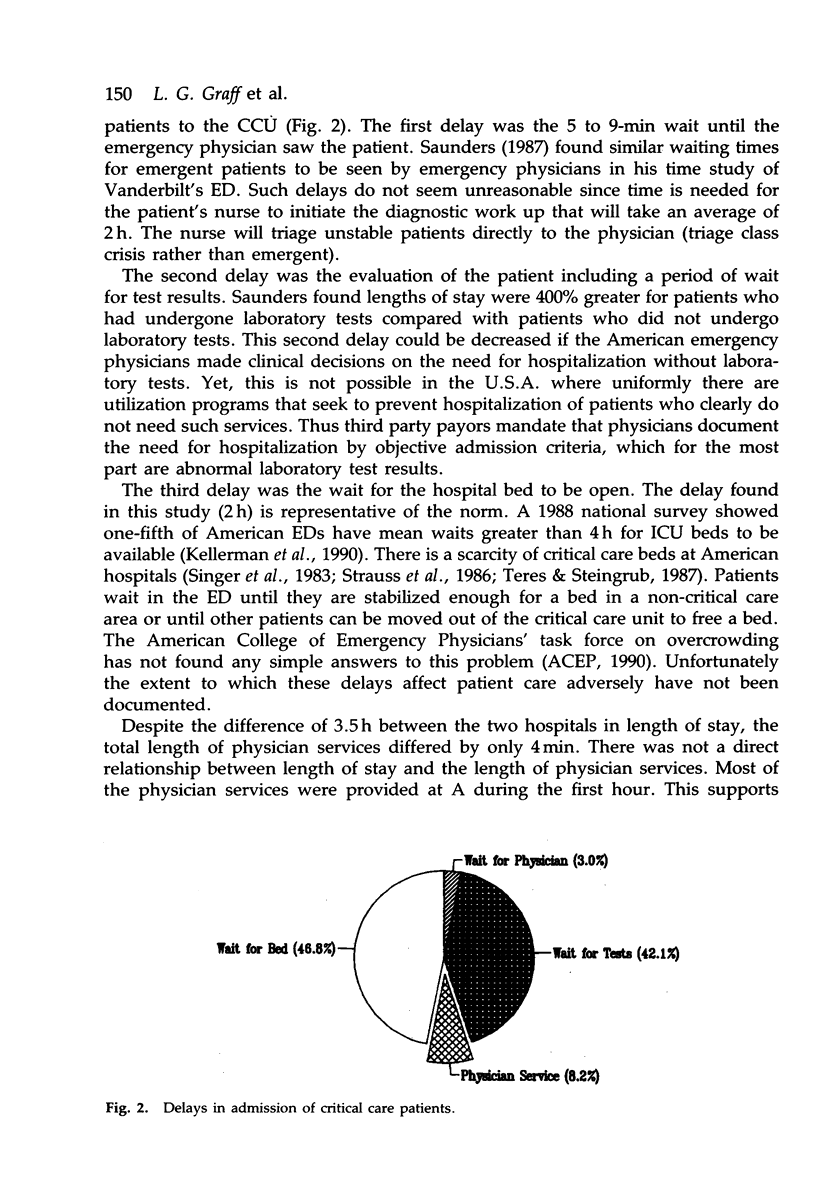
The object of this study was to compare emergency physician critical care services in an American (A) and an English (E) Emergency Department (ED). A prospective case comparison trial was used. The study was carried out at two university affiliated community hospitals, one in the U.S.A and one in England. Subjects were consecutive patients triaged as requiring critical care services and subsequently admitted to the hospital ward (A, n = 17; E, n = 18) or the intensive/critical care unit ([ICU] A, n = 14; E, n = 24). The study time period was randomly selected 8-h shifts occurring over a 4-week period. All patients were treated by standard guidelines for critical care services at the study hospital emergency department. For all study patients mean length of stay was significantly longer for the American (233 min, 95% CI 201, 264) than the English ED (24 min, 95% CI 23, 25). American emergency physicians spent less total time providing physician services (19.2 min, 95% CI 16.8, 21.6) vs. (23 min, 95% CI 21.6, 24.4) than English emergency physicians. American emergency physicians spent less time with the patient than English emergency physicians: 12.4 min (95% CI 10.3, 14.5) vs. 17 min (95% CI 15.8, 18.2). American emergency physicians spent more time on the telephone 1.8 min (95% CI 1.4, 2.2) vs. 1.2 min (95% CI 1.1, 1.3), and in patient care discussions/order giving 1.8 min (95% CI 1.4, 2.2) vs. 1.1 min (95% CI .8, 1.4), There was no significant difference in time charting (3.2 min, 95% CI 2.8, 3.6 vs. 3.5 min, 95% CI 3.2, 3.8). Results did not vary significantly whether analysed subgroups or the whole study group. American emergency physicians provided 81% of their service during the first hour. There were delays at the American hospital until the physician saw the patient: 4.9 min (95% CI 2.5, 7.3) for patients admitted to the ICU/CVU (Cardiovascular Unit), and 9.2 min (95% CI 4.6, 13.8) for patients admitted to the ward. At the American hospital, ICU/CVU physicians provided additional physician services in the emergency department whether the patient was admitted to the ward (6.7 min, 95% CI 5.5, 7.9) or the ICU/CVU (12.1 min, 95% CI 8.8, 15.9). For patients admitted to the ICU/CVU 47% of the length of stay was spent waiting for a bed to become available after the decision to admit had been made. Emergency physicians at E provided critical care services almost continuously during a short stay in the ED. Emergency physicians at A provided services intermittently with most services during an initial period of stabilization. Further study is necessary to identify what factors contribute to these different approaches to critical care in the ED.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Braun P., Hsiao W. C., Becker E. R., DeNicola M. Evaluation and management services in the Resource-Based Relative Value Scale. JAMA. 1988 Oct 28;260(16):2409–2417. [PubMed] [Google Scholar]
- Cue F., Inglis R. Improving the operations of the emergency department. Hospitals. 1978 Jul 1;52(13):110-3, 119. [PubMed] [Google Scholar]
- Gifford M. J., Franaszek J. B., Gibson G. Emergency physicians' and patients' assessments: urgency of need for medical care. Ann Emerg Med. 1980 Oct;9(10):502–507. doi: 10.1016/s0196-0644(80)80187-9. [DOI] [PubMed] [Google Scholar]
- Graff L. G., Radford M. J. Formula for emergency physician staffing. Am J Emerg Med. 1990 May;8(3):194–199. doi: 10.1016/0735-6757(90)90320-y. [DOI] [PubMed] [Google Scholar]
- Graff L., Mucci D., Radford M. J. Decision to hospitalize: objective diagnosis-related group criteria versus clinical judgment. Ann Emerg Med. 1988 Sep;17(9):943–952. doi: 10.1016/s0196-0644(88)80677-2. [DOI] [PubMed] [Google Scholar]
- Hannas R. R., Jr Staffing the emergency department. Hospitals. 1973 May 16;47(10):83–86. [PubMed] [Google Scholar]
- Jacobs A. R., Gavett J. W., Wersinger R. Emergency Department utilization in an urban community. Implications for community ambulatory care. JAMA. 1971 Apr 12;216(2):307–312. [PubMed] [Google Scholar]
- KLUGE D. N., WEGRYN R. L., LEMLEY B. R. THE EXPANDING EMERGENCY DEPARTMENT. JAMA. 1965 Mar 8;191:801–805. doi: 10.1001/jama.1965.03080100019005. [DOI] [PubMed] [Google Scholar]
- LeTourneau B., Blegen C. N., Clinton J. E., Ruiz E. Critical care in an emergency department. Ann Emerg Med. 1980 Mar;9(3):126–130. doi: 10.1016/s0196-0644(80)80266-6. [DOI] [PubMed] [Google Scholar]
- Lister J. Shattuck lecture--the politics of medicine in Britain and the United States. N Engl J Med. 1986 Jul 17;315(3):168–174. doi: 10.1056/NEJM198607173150306. [DOI] [PubMed] [Google Scholar]
- Moss A. J., Goldstein S. The pre-hospital phase of acute myocadial infarction. Circulation. 1970 May;41(5):737–742. doi: 10.1161/01.cir.41.5.737. [DOI] [PubMed] [Google Scholar]
- Navarro V. The public/private mix in the funding and delivery of health services: an international survey. Am J Public Health. 1985 Nov;75(11):1318–1320. doi: 10.2105/ajph.75.11.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinhardt U. E. The compensation of physicians: approaches used in foreign countries. QRB Qual Rev Bull. 1985 Dec;11(12):366–377. [PubMed] [Google Scholar]
- Rusnak R. A., Stair T. O., Hansen K., Fastow J. S. Litigation against the emergency physician: common features in cases of missed myocardial infarction. Ann Emerg Med. 1989 Oct;18(10):1029–1034. doi: 10.1016/s0196-0644(89)80924-2. [DOI] [PubMed] [Google Scholar]
- Rutherford W. H., Evans R. C. Accident and emergency medicine in the United Kingdom. Am J Emerg Med. 1983 Jul;1(1):107–109. doi: 10.1016/0735-6757(83)90043-8. [DOI] [PubMed] [Google Scholar]
- Saunders C. E. Time study of patient movement through the emergency department: sources of delay in relation to patient acuity. Ann Emerg Med. 1987 Nov;16(11):1244–1248. doi: 10.1016/s0196-0644(87)80232-9. [DOI] [PubMed] [Google Scholar]
- Schroeder J. S., Lamb I. H., Hu M. The prehospital course of patients with chest pain. Analysis of the prodromal, symptomatic, decision-making, transportation and emergency room periods. Am J Med. 1978 May;64(5):742–748. doi: 10.1016/0002-9343(78)90512-0. [DOI] [PubMed] [Google Scholar]
- Simon A. B., Feinleib M., Thompson H. K., Jr Components of delay in the pre-hospital phase of acute myocardial infarction. Am J Cardiol. 1972 Oct;30(5):476–482. doi: 10.1016/0002-9149(72)90037-9. [DOI] [PubMed] [Google Scholar]
- Singer D. E., Carr P. L., Mulley A. G., Thibault G. E. Rationing intensive care--physician responses to a resource shortage. N Engl J Med. 1983 Nov 10;309(19):1155–1160. doi: 10.1056/NEJM198311103091905. [DOI] [PubMed] [Google Scholar]
- Strauss M. J., LoGerfo J. P., Yeltatzie J. A., Temkin N., Hudson L. D. Rationing of intensive care unit services. An everyday occurrence. JAMA. 1986 Mar 7;255(9):1143–1146. [PubMed] [Google Scholar]
- Teres D., Steingrub J. Can intermediate care substitute for intensive care? Crit Care Med. 1987 Mar;15(3):280–280. doi: 10.1097/00003246-198703000-00025. [DOI] [PubMed] [Google Scholar]
- Tjoe S. L., Luria M. H. Delays in reaching the cardiac care unit: an analysis. Chest. 1972 Jun;61(7):617–621. doi: 10.1378/chest.61.7.617. [DOI] [PubMed] [Google Scholar]
- Trautlein J. J., Lambert R. L., Miller J. Malpractice in the emergency department--review of 200 cases. Ann Emerg Med. 1984 Sep;13(9 Pt 1):709–711. doi: 10.1016/s0196-0644(84)80733-7. [DOI] [PubMed] [Google Scholar]
- Weinerman E. R., Ratner R. S., Robbins A., Lavenhar M. A. Yale studies in ambulatory medical care. V. Determinants of use of hospital emergency services. Am J Public Health Nations Health. 1966 Jul;56(7):1037–1056. doi: 10.2105/ajph.56.7.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yealy D. M., De Hart D. A., Ellis G., Wolfson A. B. A survey of observation units in the United States. Am J Emerg Med. 1989 Nov;7(6):576–580. doi: 10.1016/0735-6757(89)90277-5. [DOI] [PubMed] [Google Scholar]
- Yoon H., Watts R. W. A mobile coronary care unit: an evaluation for its need. Ann Intern Med. 1970 Jul;73(1):61–66. doi: 10.7326/0003-4819-73-1-61. [DOI] [PubMed] [Google Scholar]


