Abstract
Recently, it has become evident that entry of some retroviruses into host cells is dependent upon a vesicle-localized, low-pH step. The entry mechanism of equine infectious anemia virus (EIAV) has yet to be examined. Here, we demonstrate that wild-type strains of EIAV require a low-pH step for productive entry. Lysosomotropic agents that inhibit the acidification of internal vesicles inhibited productive entry of EIAV. The presence of ammonium chloride (30 mM), monensin (30 μM), or bafilomycin A (50 nM) in the medium dramatically decreased the number of EIAV antigen-positive cells. We found that a low-pH step was required for EIAV infection of tissue culture cell lines as well as primary cells, such as endothelial cells and monocyte-derived macrophages. The ammonium chloride treatment did not reduce virion stability, nor did the treatment prevent virion binding to cells. Consistent with a requirement for a low-pH step, virion infectivity was enhanced more than threefold by brief low-pH treatment following binding of viral particles to permissive cells. A superinfecting variant strain of EIAV, vMA-1c, did not require a low-pH step for productive infection of fibroblasts. However, lysosomotropic agents were inhibitory to vMA-1c infection in the other cell types that vMA-1c infected but did not superinfect, indicating that the entry pathway used by vMA-1c for superinfection abrogates the need for the low-pH step.
The glycoproteins of enveloped viruses bind to cellular receptors to facilitate entry. Following receptor interactions, enveloped viruses must induce membrane fusion to deliver the viral capsid into the target cell. Some viral glycoprotein-cellular receptor interactions can induce direct membrane fusion between the viral and cellular membranes that is independent of a low-pH step. Examples of such viruses are Sendai virus (10, 30), human immunodeficiency virus type 1 (HIV-1), and human T-cell leukemia virus (20, 21). In contrast, other enveloped viruses enter the cell through vesicle uptake and require an acidic environment to undergo cell-virus membrane fusion. Examples of low-pH-dependent viruses include influenza virus (39, 40), alpha viruses (12, 39), and rhabdoviruses (38, 39). Recently, several retroviruses, including foamy virus (31), avian leukosis virus (8, 23), and mouse mammary tumor virus (3, 35), have been shown to enter cells through a low-pH mechanism.
To date, those lentiviruses that have been characterized for entry have been shown to productively enter cells through a pH-independent mechanism (21, 37). In this study, we have explored the entry mechanism of equine infectious anemia virus (EIAV). Equine infectious anemia (EIA), caused by the lentivirus EIAV, is a worldwide problem that can cause high levels of morbidity and mortality in the equine population. In vivo, EIAV is primarily if not exclusively macrophage tropic; however, in vitro the virus is able to adapt to infect additional cell types, including endothelial cells and fibroblasts (24, 36). Here we demonstrate that EIAV entry into cells relevant to in vivo infection is sensitive to compounds that alter endosomal pH. Time course studies with vesicle pH-altering compounds demonstrated that neutralization of the early endosomal compartment resulted in EIAV virions being sequestered within endosomes, preventing productive infection. Washout of the compounds eliminated the inhibitory effect. This finding indicates that neutralization of endosomal pH results in sequestration but not degradation of the virions. We found that the EIAV glycoprotein on infected cells did not elicit membrane fusion under low-pH conditions. However, EIAV particles were more infectious at low pH, suggesting the EIAV envelope conformation in the viral particle is not the same as that found on the surface of infected cells. These results are in general agreement with the conclusions drawn by Jin et al. using independent experiments with a different strain of EIAV, as described in the companion paper appearing in this issue (14).
MATERIALS AND METHODS
Lysosomotropic agents and endocytosis inhibitors.
Ammonium chloride, monensin, and bafilomycin A were obtained from Sigma (St. Louis, Mo.). The following concentrations were used in the inhibition experiments: 10, 20, and 30 mM ammonium chloride, 30 μM monensin, and 50 nM bafilomycin A. The ammonium chloride solutions were prepared from a 1 M stock, pH 7.4. The drug concentrations used did not affect the pH of the cell culture medium.
Cell lines and viral strains.
Primary equine cells and equine cell lines were used to characterize the entry requirements for EIAV. ED cells, an equine fibroblastic cell line derived from dermal cells (ATCC CCL57), primary umbilical cord endothelial cells (UVECs), and primary monocyte-derived macrophages (MDMs) were used for infection. Cells were maintained in high-glucose Dulbecco's modified Eagle's medium (DMEM) with penicillin and streptomycin. Medium was supplemented with 10% fetal calf serum for ED cells, 40% fetal calf serum for UVECs, and 15% horse serum and 15% newborn calf serum for MDMs.
Various tissue culture strains of EIAV were used in this study. Th.1 is a macrophage-tropic strain of EIAV obtained from the first viremic episode of a horse inoculated with a field isolate from Massachusetts (6). MA-1 is an avirulent, tissue culture-adapted strain of Th.1 (6). vMA-1c is a cytopathic, superinfecting strain of EIAV that was derived by serial passages of MA-1 in ED cells, as described in reference 18. pSP19 is a nonvirulent molecular clone of EIAV (29). WSU5 is an EIAV strain from Washington State University that was derived from Wyoming strain and continues to be passaged in equine fetal kidney cells and back-passaged through ponies to maintain virulence (26).
Generation and titer determinations of viral stocks.
Viral stocks of MA-1, vMA-1c, and WSU5 were produced in ED cells. Th.1 stocks were produced in equine UVECs. SP19 stocks were produced by the transfection and passage of the molecular clone pSPeiav19 in D17 cells. Supernatants were harvested from cells that were >95% positive for EIAV antigen as determined by EIAV antigen immunostaining (19). Supernatants were centrifuged for 5 min at 13,500 × g to remove cell debris, aliquoted, and frozen at −80°C until needed. Viral titers were determined by infection of ED cells with serial dilutions of stock, followed by 75% acetone-25% water fixation at 40 h postinfection and anti-EIAV immunostaining of the cells as previously described (19). The EIAV antigen-positive cells within the infected cell monolayer were counted, and titers were determined. In all experiments cells were infected with a multiplicity of infection of 0.005. The titers were determined in ED cells or UVECs for ED and UVEC experiments, respectively, and in UVECs for macrophage Th.1 experiments.
Detection of EIAV replication.
EIAV infection was determined by immunostaining of viral antigens as previously described (19). Acetone-fixed cells were immunostained with polyclonal horse anti-EIAV antiserum (1:800) from a long-term-infected horse (WSU 2085). This antiserum primarily recognizes envelope (gp90 and gp46) and Gag proteins, as well as Gag precursor polyproteins. Primary antiserum was incubated for 3 h at 37°C, followed by several washes with phosphate-buffered saline. Peroxidase-conjugated goat anti-horse immunoglobulin (1:800; Jackson Immunoresearch) was incubated as the secondary antibody for 45 min at 37°C. Peroxidase activity was detected with the substrate 3-amino-9-ethylcarbazole (Sigma).
MDM studies.
To test for the ability of macrophage-tropic virus to enter cells in the presence of ammonium chloride, equine macrophages were isolated as previously described (9, 13). The macrophages were seeded into a 48-well tissue culture dish and infected with Th.1 in the presence of increasing concentrations of ammonium chloride. At 18 h postinfection the ammonium chloride medium was removed and replaced with DMEM supplemented with 15% horse serum and 15% newborn calf serum to minimize cell toxicity. Supernatants from the infected populations were collected every 24 h, and a reverse transcriptase assay was performed (33).
Studies with lysosomotropic agents. (i) Ammonium chloride.
ED cells or UVECs were seeded onto a 48-well plate and allowed to grow to 95% confluence. The cells were then infected in the presence or absence of various concentrations of ammonium chloride. The cells were fixed and stained 40 h postinfection as described above.
(ii) Monensin.
ED cells were seeded onto a 48-well plate and allowed to grow to 95% confluence. The cells were incubated with or without 30 μM monensin for 30 min and infected in the presence of monensin. Six hours postinfection the medium was removed, the cells were washed with medium, and the medium was replaced with DMEM-10% fetal calf serum. The cells were fixed and stained 40 h postinfection as described above.
(iii) Bafilomycin A.
ED cells were seeded onto a 48-well plate and allowed to grow to 95% confluence. The cells were then incubated with or without 50 nM bafilomycin A and then infected in the presence of the drug. Sixteen hours postinfection the medium was removed, the cells were washed, and the medium was replaced with DMEM-10% fetal calf serum. The cells were fixed and stained 40 h postinfection as described above.
Cell viability.
ED, UVEC, or MDM cells were plated and treated with lysosomotropic agents as described above. Forty hours posttreatment, cell viability was monitored by ATPLite assay (Packard Biosciences) per the manufacturer's instructions.
Virion stability studies.
MA-1 viral stock was incubated in DMEM-10% fetal calf serum or DMEM-10% fetal calf serum plus 20 mM ammonium chloride. The virion stock was maintained at 37°C and used to infect ED cells at various time points post-initial infection. The final concentration of ammonium chloride when diluted on the cells was 0.13 mM. The cells were fixed and immunostained for the production of EIAV proteins. The number of EIAV antigen-positive cells at the various time points following 37°C incubation was compared to the number of positive cells when the virus was immediately used for infection.
Virion binding studies.
MA-1 viral stock was bound to ED cells at 4°C in cell medium or medium containing 20 mM ammonium chloride. Neutralizing anti-EIAV horse serum (1:30 and 1:300) was added as a positive control for binding inhibition. The viral inoculum and ammonium chloride treatment were removed after 1 h, cell medium was refreshed, and the cells were transferred to 37°C. The cells were fixed and immunostained for the production of EIAV antigens 40 h postinfection.
Ammonium chloride washout studies.
ED cells were infected with MA-1 in the presence or absence of 25 mM ammonium chloride. The virus-containing medium was removed at various time points postinfection, and the cells were washed with citric acid buffer (pH 3) for 30 seconds to remove any surface virions. The buffer was removed, the cells were washed four times in fresh medium, and the medium was replaced. The cells were then fixed and immunostained for EIAV antigens as described above.
Ammonium chloride addition studies.
ED cells were infected in the absence of ammonium chloride. At various time points postinfection 1 M ammonium chloride stock was added to the ED culture medium to a final concentration of 25 mM. The cells were fixed and stained 40 h postinfection as described above.
Low-pH-induced fusion.
ED cells were incubated at 4°C and inoculated with MA-1 virus to allow binding, but not internalization. The multiplicity of infection was reduced to 0.0005 because titers were found to be higher when virus was allowed to bind at 4°C. The viral inoculum was removed 1 hour postinfection, and DMEM with decreasing pHs was added to the cells for 1 min. The low-pH medium was removed, the cells were washed, and new ED medium was replaced. The cells were incubated at 37°C for 40 h and then stained for EIAV antigen.
RESULTS
EIAV infection is inhibited by ammonium chloride.
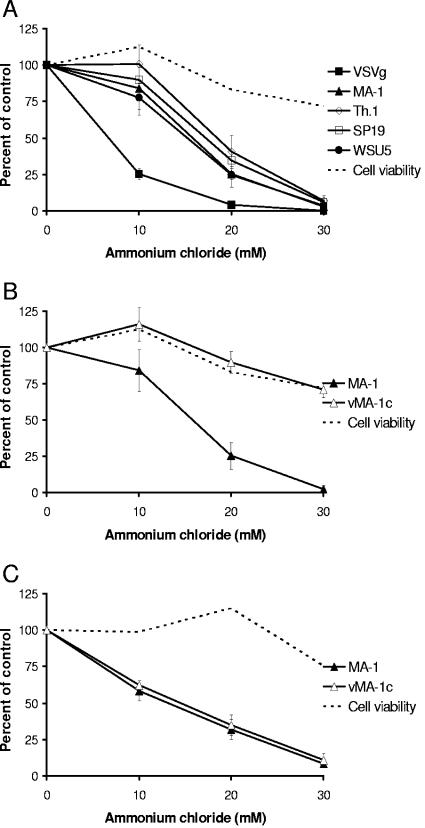
The dependence of vesicle acidification for EIAV entry was explored by adding ammonium chloride to the cell medium (Fig. 1A). Ammonium chloride is a weak base that diffuses into the endosome and serves as a proton sink, thus inhibiting the acidification of the endosome (25). Increasing concentrations of ammonium chloride, pH 7.4, were added to the cell medium. Ammonium chloride-treated ED cells were infected with four strains of EIAV or vesicular stomatitis virus G protein (VSV-G)-pseudotyped retroviral particles that served as a positive control (7, 31). Ammonium chloride was maintained on the cells throughout the experiment. Forty hours postinfection the cells were acetone fixed and immunostained for EIAV antigen as previously described (19). While EIAV did not appear to be as sensitive to ammonium chloride treatment as VSV-G-pseudotyped virions, the macrophage- and tissue culture-adapted strains of EIAV, Th.1, MA-1, WSU5, and SP19 showed a dose-dependent inhibition of replication (Fig. 1A). On average, virus infectivity was reduced more than 90% by 30 mM ammonium chloride. These inhibitory concentrations are similar to those previously reported to inhibit the low-pH-dependent entry of avian leukosis virus and influenza virus (23, 40). Consistent with previous studies, inhibition of HIV entry was not observed in the presence of ammonium chloride (data not shown) (2). The decrease in EIAV infection by endosomal pH neutralization suggested that EIAV enters ED cells through a low-pH-dependent mechanism. EIAV is the first lentivirus identified to be dependent on a low-pH step during entry. An ATPlite assay was used to determine cell viability in the presence of different concentrations of ammonium chloride. Although ammonium chloride reduced the cell viability by 25% at the highest concentration (Fig. 1A), this effect did not account for the profound inhibition of EIAV entry.
FIG. 1.
Ammonium chloride treatments inhibit EIAV entry. ED cells (A and B) or UVECs (C) were infected with EIAV in the presence of increasing concentrations of ammonium chloride. The cells were immunostained 40 h postinfection. The infectivity in the presence of ammonium chloride is shown as a percentage of control. The number of EIAV-positive cells when no ammonium chloride was present was set to 100% in order to calculate the percentage of control. Data represent the means and standard errors of the means from three separate experiments performed in triplicate.
A variant strain of EIAV, vMA-1c, exhibited a unique low-pH-independent phenotype in ED cells. vMA-1c has been shown to superinfect and induce syncytia and cell death in ED cells and primary equine fibroblasts, but not other cells, such as endothelial cells (18). In parallel with wild-type EIAV strains, vMA-1c was tested for productive infection of ED cells in the presence of ammonium chloride (Fig. 1B). Unlike the other EIAV strains, vMA-1c did not show a dose-dependent inhibition of infectivity. At higher concentrations of ammonium chloride, a 25% reduction in vMA-1c infectivity was observed; however, this decrease closely correlated with the decrease in the number of viable cells present, suggesting that this superinfecting strain of virus did not require a low-pH step during infection of ED cells. Consistent with the possibility that vMA-1c enters the cell through fusion at the plasma membrane, vMA-1c was highly fusogenic, inducing prominent syncytia in ED cells at neutral pH (18).
In contrast with our findings in equine dermal fibroblasts, both MA-1 and vMA-1c entry into equine endothelial cells (UVECs) was inhibited by increasing concentrations of ammonium chloride, indicating that the viruses entered UVECs in a low-pH-dependent manner (Fig. 1C). Previous studies within the lab indicated that vMA-1c does not superinfect UVECs (W. Maury, personal communication). Thus, the ability of vMA-1c to enter cells in a pH-independent manner correlated with a loss of receptor interference.
Ammonium chloride inhibits EIAV at an early stage in the viral life cycle.
The presence of ammonium chloride during the course of infection was observed to decrease the infectivity of the wild-type strains of EIAV. To determine if viral infectivity was reduced as a specific consequence of ammonium chloride-induced degradation of virions, infectivity studies were performed with viral particles as well as in infected cells over time. The stability of the viral particles was determined by incubating the virus in medium or in medium with ammonium chloride at 37°C. Aliquots were placed onto ED cells at various times post-addition of ammonium chloride, and relative infectivity was determined by immunostaining the cells 40 h postinfection. The inoculum when placed on the cells had a final concentration of 0.13 mM ammonium chloride, which did not affect viral infectivity (data not shown). The decrease in MA-1 infectivity when no ammonium chloride was present closely followed the infectivity when the virions were incubated with ammonium chloride (Fig. 2A). The similar levels of infectivity over time suggest that the ammonium chloride does not adversely affect the virion particles and that the decrease in infectivity seen in Fig. 1 was not due to virion instability in the presence of ammonium chloride.
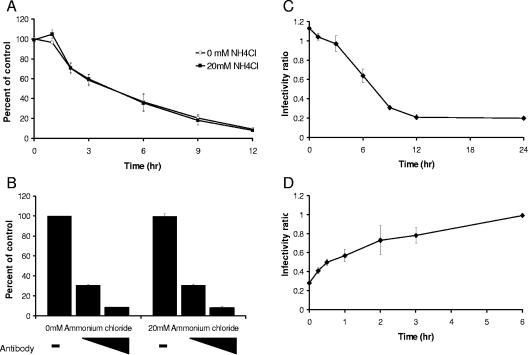
FIG. 2.
Ammonium chloride inhibits MA-1 early in the viral life cycle. (A) MA-1 stock was incubated at 37°C for the times noted in medium or medium plus ammonium chloride. Incubated virus was added to ED cells, and the quantity of infectious virions remaining was determined by immunostaining for viral antigen. (B) MA-1 stock was bound to ED cells at 4°C with or without ammonium chloride and 1:300 or 1:30 dilutions of neutralizing anti-EIAV antibodies for 1 h. The viral inoculum was then removed and replaced with DMEM that did not contain any ammonium chloride or antibody. Viral infectivity was examined 40 h postinfection and is expressed as a percentage of control (the number of EIAV-positive cells when no antibody or ammonium chloride was present). (C) ED cells were infected with MA-1 in the absence or presence of ammonium chloride. At the indicated time points postinfection, the ammonium chloride-containing medium was removed and replaced with fresh medium. Viral infectivity is expressed as a ratio of the number of EIAV-positive cells with ammonium chloride over the number of EIAV-positive cells without ammonium chloride at the indicated time point. (D) Ammonium chloride was added to MA-1-infected ED cells at the indicated time points postinfection. Cells were fixed and stained 40 h postinfection. Results are shown as a ratio of EIAV antigen-positive cells with ammonium chloride added at the indicated time compared to the number of EIAV-positive cells without ammonium chloride added. Data represent the means and standard errors of the means from two separate experiments performed in triplicate.
In order to determine if the ammonium chloride inhibition altered the ability of virions to bind to cells, MA-1 virions were incubated with ED cells at 4°C in the presence or absence of ammonium chloride. The viral inoculum was then removed, the cells were washed, medium was replaced, and the cells were placed at 37°C. The presence of ammonium chloride during the binding step did not inhibit viral entry; however, increasing amounts of neutralizing anti-EIAV antibodies prevented viral infection (Fig. 2B). Therefore, the ammonium chloride is inhibiting EIAV at a postbinding step.
To more clearly define the time frame of inhibition, time course experiments were performed with ammonium chloride. To establish the time frame of ammonium chloride inhibition, ED cells were infected in the presence of ammonium chloride and the compound was washed away at various time points postinfection (Fig. 2C). The infectivity ratio presented at each time point represents the number of EIAV antigen-positive cells in the presence of ammonium chloride compared with the number of EIAV-positive cells in the absence of ammonium chloride treatment. If ammonium chloride was removed as late as 3 h postinfection, the compound had no affect of virion infectivity. This finding suggested that the internalized infectious virions remain stable during this time (compare Fig. 2A and C). Because the ammonium chloride was not affecting stability or binding of the virions, this suggested that virions were sequestered within a cellular endosome, and if the acidification block were reversed, the remaining virions could complete the infection of the cell. To complement the washout studies, ammonium chloride was added to MA-1-infected ED cells at various time points postinfection to determine when the compound was no longer effective at blocking infectivity (Fig. 2D). Ammonium chloride was able to inhibit viral protein expression in more than 50% of cells when added to the cells within the first hour postinfection. Addition of ammonium chloride 2 hours postinfection inhibited 20% of the infectious virions, while addition of ammonium chloride 6 hours postinfection had no inhibitory effect. These findings were consistent with ammonium chloride treatment blocking early, postbinding events within the life cycle of EIAV.
Low-pH medium enhances MA-1 infectivity.
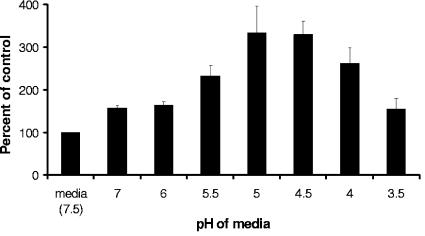
Low-pH-dependent viruses require an acidic environment in order for conformational changes that facilitate membrane fusion to occur. Some low-pH-dependent viruses can produce large syncytia when infected cells are added to permissive cells and are exposed to a low pH, presumably due to low-pH conformational changes in the viral envelope that facilitate fusion (23). Incubation of MA-1-infected ED cells with uninfected ED cells did not result in cell-cell fusion when exposed to low-pH medium (data not shown). Some retroviral envelope proteins only become fusion ready in the viral particles after a cleavage event by the viral protease has occurred, producing the mature envelope protein (1, 32). To determine if EIAV particle infectivity was enhanced by a low-pH treatment, viral particles were bound to ED cells at 4°C and then exposed to low-pH medium ranging from pH 3.5 to 6 (Fig. 3). Bound viral particles exposed to medium at pH 4.5 or 5.0 produced three times as many EIAV-positive cells as cells treated with DMEM (pH 7.5). Thus, an acidic environment stimulated fusion of virus and permissive cells.
FIG. 3.
Low-pH medium increases EIAV entry. MA-1 virus was bound to ED cells for 1 hour at 4°C. The medium was then removed, and low-pH medium was put on the cells for 1 min. The cells were washed, medium was replaced, and cells were incubated at 37°C for 40 h, after which they were fixed and stained. The level of infectivity was compared to that of the cells that were incubated with normal DMEM as a control. Data represent the means and standard errors of the means from three separate experiments performed in triplicate.
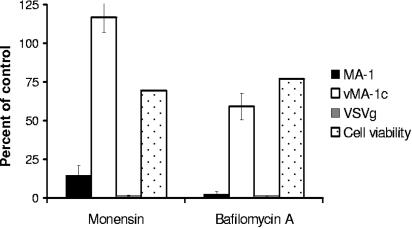
Lysosomotropic agents inhibit entry of MA-1 but not vMA-1c in ED cells.
To confirm the ammonium chloride results, other lysosomotropic agents were examined for their ability to inhibit entry of EIAV. Due to cell toxicity, bafilomycin A, a vacuolar H+-ATPase inhibitor (30), and monensin, a carboxylic ionophore (17), were removed 16 h and 6 h postinfection, respectively. This short treatment of cells with bafilomycin A and monensin reduced cell viability by approximately 30% (Fig. 4). The bafilomycin A and monensin treatments inhibited MA-1 but did not alter vMA-1c infectivity appreciably in ED cells (Fig. 4). VSV-G-pseudotyped retroviral particles were also found to be profoundly inhibited by the treatments, as previously reported (7, 31). These findings confirm our observations with ammonium chloride that indicate the wild-type EIAV strains require a low-pH step for productive entry.
FIG. 4.
Lysosomotropic agents inhibit EIAV entry. ED cells were infected in the presence of 30 μM monensin or 50 nM bafilomycin A, both drugs were removed 6 and 16 h postinfection, respectively, and cells were analyzed for viral antigen expression 40 h postinfection. Data represent the means and standard errors of the means from three separate experiments performed in triplicate.
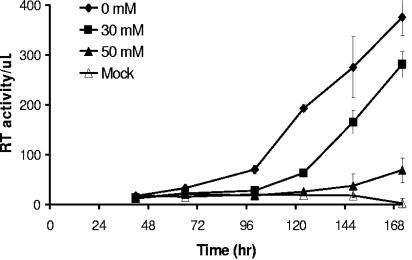
EIAV entry into primary MDMs is inhibited by ammonium chloride.
In order to determine the entry requirements for EIAV in a cell type relevant to an in vivo infection, the impact of ammonium chloride on EIAV entry into primary equine MDMs was examined (Fig. 5). MDM cultures were infected with the macrophage-tropic EIAV strain, Th.1, on the day of isolation of the cells in the presence of ammonium chloride for the initial 18 h of the infection. Following this initial treatment, ammonium chloride was removed to preserve cell viability over the course of the study. The infection was monitored by supernatant reverse transcriptase activity during a 6-day period. As we observed in ED cells, entry of Th.1 was inhibited by ammonium chloride in MDMs. At a concentration of 30 mM ammonium chloride, delayed kinetics of supernatant RT activity were observed and, at early time points, RT activity was reduced. However, at this lower ammonium chloride concentration the rate of virus production increased over time, presumably due to replication and spread of the limited number of virions that were able to enter during the initial infection step. Higher concentrations of ammonium chloride (50 mM) completely abrogated detectable levels of virus replication throughout the experiment. These data demonstrate that EIAV enters both cell lines and primary cells through a low-pH-dependent mechanism.
FIG. 5.
EIAV enters primary MDMs in a low-pH-dependent manner. MDMs were infected with Th.1 in the presence of increasing concentrations of ammonium chloride. Culture supernatant reverse transcriptase activity was measured over time. Ammonium chloride was present in the medium for the initial 18 h and then removed due to ammonium chloride cytotoxicity. Shown are data from a single experiment as a representative sample.
DISCUSSION
Our results provide strong evidence that EIAV enters cells through a low-pH-dependent mechanism and are consistent with studies performed by Jin and Montelaro (14). Several lysosomotropic agents that prevent acidification of endosomal compartments through different mechanisms, such as the weak base ammonium chloride, the carboxylic ionophore monensin, and the H+-ATPase inhibitor bafilomycin A, inhibited EIAV infection. The inhibition caused by ammonium chloride did not alter virion binding of cells but was only effective if the ammonium chloride was present during the initial 3 h postinfection. This finding indicates that the block occurs early during the viral life cycle following particle binding onto the cell. Since retroviral integration has been reported to occur between 4 and 12 h postinfection (4, 5, 15), the ammonium chloride inhibition appears to be affecting a preintegration step, consistent with previous reports with other low-pH-dependent retroviruses (3, 23). The kinetics of inhibition were very similar to the effects of ammonium chloride on avian leukosis virus A, a retrovirus that requires a low-pH step in order to productively enter target cells (23). EIAV is the first lentivirus that has been described to require endocytosis into an acidic environment to mediate productive infection of target cells.
The acidic requirements of many low-pH-dependent viruses have been examined. Influenza virus requires an acidic pH of 5.2 to induce the necessary conformational changes that will result in membrane fusion (16), whereas Sindbis virus requires pH 5.8 (22), and VSV requires a drop in pH to 5.9 (28). The pH requirements for EIAV have not been precisely defined but appear to be optimal between pH 4.5 and 5. The lower pH requirements for EIAV fusion compared to VSV fusion may account for EIAV's decreased sensitivity to the various lysosomotropic agents. Within a given cell there are several populations of endosomal vesicles. It has been reported that 82% of the endosomal vesicles within epidermal fibroblasts are acidic, with an average pH of 5.1 and a range of pH 4.8 to 5.3, while the remaining vesicles are neutral, with an average pH of 7.15 (27). The optimal pH between 4.5 and 5.0 is, therefore, physiologically relevant, because the low-pH environment required for EIAV fusion can be found within cellular endosomal vesicles.
The acidic environment required for EIAV entry is presumed to cause conformational changes in the envelope protein structure such that fusion events can occur. The pH-independent entry of HIV may be explained by the virus' utilization of both a receptor and a coreceptor. This two-step process may be sufficient for triggering conformational changes required for fusion (11). Our findings that EIAV requires a low-pH step for entry supports a single-receptor model for EIAV entry which was recently identified (41). Nef appears to be necessary for HIV's ability to productively enter cells when fusing directly with the plasma membrane (7). EIAV does not contain a Nef homologue and, perhaps as a consequence, requires endocytosis to productively infect.
The novel superinfecting strain of EIAV, vMA-1c, did not require acidification of the endosomal compartments to productively enter ED cells. However, a low-pH step was required for vMA-1c to infect cells that the virus does not superinfect. This finding suggests that vMA-1c may be able to enter ED cells through interactions with a cellular receptor or receptors that other strains of EIAV are unable to utilize and that vMA-1c is unable to utilize this pH-independent pathway for entry into other cell types. Alternatively, vMA-1c may utilize the same receptor as wild-type EIAV; however, it may not be under the same constraints as wild-type EIAV. For instance, vMA-1c contains 18 amino acid changes in the envelope protein compared to its parental strain as well as a truncation of the cytoplasmic tail. The changes in vMA-1c envelope protein may alter the conformation of the protein such that it no longer requires an acidic pH to induce membrane fusion. If this is the case, it is not currently clear why the vMA-1c particles are not low-pH independent in other cell types.
It has long been recognized that EIAV-infected cells do not induce syncytia when incubated with permissive cell populations. Here, we extend these observations by demonstrating that ED cells expressing viral envelope were unable to produce syncytia after exposing the cells to a low pH (data not shown). However, acidification of viral particles bound to permissive cells enhanced viral infectivity. The envelope transmembrane protein of EIAV contains a long cytoplasmic tail. It has been hypothesized that the envelope protein becomes fusion ready in the viral particle due to a cleavage event that removes part of the cytoplasmic tail, similar to the R peptide of murine leukemia virus (32, 34). The particle specific cleavage event would be consistent with our findings. Furthermore, vMA-1c envelope protein contains a marked truncation of the cytoplasmic tail. This truncation may produce a fusion-ready TM that allows syncytium formation in infected ED populations.
In summary, the present study demonstrates that equine infectious anemia virus enters cells through an acidic vesicle. The superinfecting variant vMA-1c can superinfect cells through a pH-independent mechanism. The mutations found in the envelope of vMA-1c may mimic the conformational changes caused by the acidic environment that allow fusion to occur. Future examination of the mutations that promote pH-independent entry may give insight into the conformational changes required for virus-cell membrane fusion.
Acknowledgments
This work was supported by the grant Training in Molecular Virology T32 A1007533 from the NIAID.
We thank Kimberly P. Schmitt and Jian Shao for technical assistance. We also thank Paul McCray for the FIV packaging system.
REFERENCES
- 1.Aguilar, H. C., W. F. Anderson, and P. M. Cannon. 2003. Cytoplasmic tail of Moloney murine leukemia virus envelope protein influences the conformation of the extracellular domain: implications for mechanism of action of the R peptide. J. Virol. 77:1281-1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aiken, C. 1997. Pseudotyping human immunodeficiency virus type 1 (HIV-1) by the glycoprotein of vesicular stomatitis virus targets HIV-1 entry to an endocytic pathway and suppresses both the requirement for Nef and the sensitivity to cyclosporin A. J. Virol. 71:5871-5877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolander, F. F., Jr. 1996. Requirements for mouse mammary tumour virus internalization in mouse mammary epithelial cells. J. Gen. Virol. 77:793-796. [DOI] [PubMed] [Google Scholar]
- 4.Brussel, A., and P. Sonigo. 2003. Analysis of early human immunodeficiency virus type 1 DNA synthesis by use of a new sensitive assay for quantifying integrated provirus. J. Virol. 77:10119-10124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Butler, S. L., E. P. Johnson, and F. D. Bushman. 2002. Human immunodeficiency virus cDNA metabolism: notable stability of two-long terminal repeat circles. J. Virol. 76:3739-3747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carpenter, S., and B. Chesebro. 1989. Change in host cell tropism associated with in vitro replication of equine infectious anemia virus. J. Virol. 63:2492-2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chazal, N., G. Singer, C. Aiken, M. L. Hammarskjold, and D. Rekosh. 2001. Human immunodeficiency virus type 1 particles pseudotyped with envelope proteins that fuse at low pH no longer require Nef for optimal infectivity. J. Virol. 75:4014-4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diaz-Griffero, F., S. A. Hoschander, and J. Brojatsch. 2002. Endocytosis is a critical step in entry of subgroup B avian leukosis viruses. J. Virol. 76:12866-12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.English, D., and B. R. Andersen. 1974. Single-step separation of red blood cells. Granulocytes and mononuclear leukocytes on discontinuous density gradients of Ficoll-Hypaque. J. Immunol. Methods 5:249-252. [DOI] [PubMed] [Google Scholar]
- 10.Fan, D. P., and B. M. Sefton. 1978. The entry into host cells of Sindbis virus, vesicular stomatitis virus and Sendai virus. Cell 15:985-992. [DOI] [PubMed] [Google Scholar]
- 11.Gallo, S. A., C. M. Finnegan, M. Viard, Y. Raviv, A. Dimitrov, S. S. Rawat, A. Puri, S. Durell, and R. Blumenthal. 2003. The HIV Env-mediated fusion reaction. Biochim. Biophys. Acta 1614:36-50. [DOI] [PubMed] [Google Scholar]
- 12.Helenius, A., J. Kartenbeck, K. Simons, and E. Fries. 1980. On the entry of Semliki forest virus into BHK-21 cells. J. Cell Biol. 84:404-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hines, R., B. R. Sorensen, M. A. Shea, and W. Maury. 2004. PU.1 binding to ets motifs within the equine infectious anemia virus long terminal repeat (LTR) enhancer: regulation of LTR activity and virus replication in macrophages. J. Virol. 78:3407-3418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jin, S., B. Zhang, O. A. Weisz, and R. C. Montelaro. 2005. Receptor-mediated entry by equine infectious anemia virus utilizes a pH-dependent endocytic pathway. J. Virol. 79:14489-14497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar, R., N. Vandegraaff, L. Mundy, C. J. Burrell, and P. Li. 2002. Evaluation of PCR-based methods for the quantitation of integrated HIV-1 DNA. J. Virol. Methods 105:233-246. [DOI] [PubMed] [Google Scholar]
- 16.Maeda, T., and S. Ohnishi. 1980. Activation of influenza virus by acidic media causes hemolysis and fusion of erythrocytes. FEBS Lett. 122:283-287. [DOI] [PubMed] [Google Scholar]
- 17.Marsh, M., J. Wellsteed, H. Kern, E. Harms, and A. Helenius. 1982. Monensin inhibits Semliki Forest virus penetration into culture cells. Proc. Natl. Acad. Sci. USA 79:5297-5301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maury, W., P. J. Wright, and S. Bradley. 2003. Characterization of a cytolytic strain of equine infectious anemia virus. J. Virol. 77:2385-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maury, W. J., S. Carpenter, K. Graves, and B. Chesebro. 1994. Cellular and viral specificity of equine infectious anemia virus Tat transactivation. Virology 200:632-642. [DOI] [PubMed] [Google Scholar]
- 20.McClure, M. O., M. Marsh, and R. A. Weiss. 1988. Human immunodeficiency virus infection of CD4-bearing cells occurs by a pH-independent mechanism. EMBO J. 7:513-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McClure, M. O., M. A. Sommerfelt, M. Marsh, and R. A. Weiss. 1990. The pH independence of mammalian retrovirus infection. J. Gen. Virol. 71:767-773. [DOI] [PubMed] [Google Scholar]
- 22.Meyer, W. J., S. Gidwitz, V. K. Ayers, R. J. Schoepp, and R. E. Johnston. 1992. Conformational alteration of Sindbis virion glycoproteins induced by heat, reducing agents, or low pH. J. Virol. 66:3504-3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mothes, W., A. L. Boerger, S. Narayan, J. M. Cunningham, and J. A. Young. 2000. Retroviral entry mediated by receptor priming and low pH triggering of an envelope glycoprotein. Cell 103:679-689. [DOI] [PubMed] [Google Scholar]
- 24.Oaks, J. L., T. C. McGuire, C. Ulibarri, and T. B. Crawford. 1998. Equine infectious anemia virus is found in tissue macrophages during subclinical infection. J. Virol. 72:7263-7269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohkuma, S., and B. Poole. 1978. Fluorescence probe measurement of the intralysosomal pH in living cells and the perturbation of pH by various agents. Proc. Natl. Acad. Sci. USA 75:3327-3331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Rourke, K., L. E. Perryman, and T. C. McGuire. 1988. Antiviral, anti-glycoprotein and neutralizing antibodies in foals with equine infectious anaemia virus. J. Gen. Virol. 69:667-674. [DOI] [PubMed] [Google Scholar]
- 27.Overly, C. C., K. D. Lee, E. Berthiaume, and P. J. Hollenbeck. 1995. Quantitative measurement of intraorganelle pH in the endosomal-lysosomal pathway in neurons by using ratiometric imaging with pyranine. Proc. Natl. Acad. Sci. USA 92:3156-3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pak, C. C., A. Puri, and R. Blumenthal. 1997. Conformational changes and fusion activity of vesicular stomatitis virus glycoprotein: [125I]iodonaphthyl azide photolabeling studies in biological membranes. Biochemistry 36:8890-8896. [DOI] [PubMed] [Google Scholar]
- 29.Payne, S. L., J. Rausch, K. Rushlow, R. C. Montelaro, C. Issel, M. Flaherty, S. Perry, D. Sellon, and F. Fuller. 1994. Characterization of infectious molecular clones of equine infectious anaemia virus. J. Gen. Virol. 75:425-429. [DOI] [PubMed] [Google Scholar]
- 30.Perez, L., and L. Carrasco. 1994. Involvement of the vacuolar H+-ATPase in animal virus entry. J. Gen. Virol. 75:2595-2606. [DOI] [PubMed] [Google Scholar]
- 31.Picard-Maureau, M., G. Jarmy, A. Berg, A. Rethwilm, and D. Lindemann. 2003. Foamy virus envelope glycoprotein-mediated entry involves a pH-dependent fusion process. J. Virol. 77:4722-4730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ragheb, J. A., and W. F. Anderson. 1994. pH-independent murine leukemia virus ecotropic envelope-mediated cell fusion: implications for the role of the R peptide and p12E TM in viral entry. J. Virol. 68:3220-3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reed-Inderbitzin, E., and W. Maury. 2003. Cellular specificity of HIV-1 replication can be controlled by LTR sequences. Virology 314:680-695. [DOI] [PubMed] [Google Scholar]
- 34.Rice, N. R., L. E. Henderson, R. C. Sowder, T. D. Copeland, S. Oroszlan, and J. F. Edwards. 1990. Synthesis and processing of the transmembrane envelope protein of equine infectious anemia virus. J. Virol. 64:3770-3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ross, S. R., J. J. Schofield, C. J. Farr, and M. Bucan. 2002. Mouse transferrin receptor 1 is the cell entry receptor for mouse mammary tumor virus. Proc. Natl. Acad. Sci. USA 99:12386-12390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sellon, D. C., S. T. Perry, L. Coggins, and F. J. Fuller. 1992. Wild-type equine infectious anemia virus replicates in vivo predominantly in tissue macrophages, not in peripheral blood monocytes. J. Virol. 66:5906-5913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stein, B. S., S. D. Gowda, J. D. Lifson, R. C. Penhallow, K. G. Bensch, and E. G. Engleman. 1987. pH-independent HIV entry into CD4-positive T cells via virus envelope fusion to the plasma membrane. Cell 49:659-668. [DOI] [PubMed] [Google Scholar]
- 38.Superti, F., M. Derer, and H. Tsiang. 1984. Mechanism of rabies virus entry into CER cells. J. Gen. Virol. 65:781-789. [DOI] [PubMed] [Google Scholar]
- 39.White, J., K. Matlin, and A. Helenius. 1981. Cell fusion by Semliki Forest, influenza, and vesicular stomatitis viruses. J. Cell Biol. 89:674-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yoshimura, A., K. Kuroda, K. Kawasaki, S. Yamashina, T. Maeda, and S. Ohnishi. 1982. Infectious cell entry mechanism of influenza virus. J. Virol. 43:284-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang, B., S. Jin, J. Jin, F. Li, and R. C. Montelaro. 2005. A tumor necrosis factor receptor family protein serves as a cellular receptor for the macrophage-tropic equine lentivirus. Proc. Natl. Acad. Sci. USA 102:9918-9923. [DOI] [PMC free article] [PubMed] [Google Scholar]