Abstract
Random PCR mutagenesis of the enterococcal aph(2")-Ic gene followed by selection for mutant enzymes that confer enhanced levels of aminoglycoside resistance resulted in mutants of APH(2")-Ic with His-258-Leu and Phe-108-Leu substitutions, all of which conferred rises in the MICs of several aminoglycosides. The mutated residues are located outside conserved regions of aminoglycoside phosphotransferases.
The aph(2")-Ic gene, found in some Enterococcus species, encodes the APH(2")-Ic aminoglycoside phosphotransferase (APH) enzyme that confers aminoglycoside resistance (5). The presence of this or any of three other enterococcal aminoglycoside resistance genes, aac(6′)-Ie-aph(2")-Ia, aph(2")-Ib, or aph(2")-Id, is known to eliminate the synergistic killing achieved by a combination of gentamicin with a cell wall-active antimicrobial agent such as ampicillin (7, 9, 17). No mutant aminoglycoside-modifying enzymes producing increased levels of resistance have been reported in clinical isolates, despite the widespread use of aminoglycosides over many years, whereas numerous mutant β-lactamases with broadened substrate specificities have emerged in response to the use of extended-spectrum β-lactam antibiotics. We have previously used randomized PCR mutagenesis to generate numerous mutants of the TEM-1 β-lactamase that confer increased levels of resistance to various β-lactam agents, including those that have arisen in clinical isolates (18). In this study, we applied randomized PCR to mutagenize the aph(2")-Ic gene and have obtained mutants that confer markedly increased levels of resistance to a number of aminoglycosides compared to the level of resistance conferred by the wild-type gene.
(This work was presented in part at the 41st Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, Ill., 16 to 19 December 2001.)
Bacterial strains and plasmids.
Escherichia coli DH5α {F′ endA1 hsdR17(rk− mk+) glnV44 thi-1 recA1 gyrA (Nalr) relA1 Δ(lacIZYA-argF)U169 deoR [φ80dlacΔ(lacZ)M15]} and E. coli JM83 {F− araΔ(lac-proAB) rpsL (Strr) [φ80dlacΔ(lacZ)M15] thi} were used as hosts for expression of wild-type and mutagenized aph(2")-Ic genes. Oligonucleotide primers were synthesized by Life Technologies (Rockville, Md.). Plasmid DNA was isolated by using a QIAprep Spin Miniprep kit (QIAGEN Inc., Chatsworth, Calif.). The vector pBluescript II KS(+) (Stratagene, La Jolla, Calif.), which contains an ampicillin resistance marker, was used in standard cloning experiments (1). Plasmid pBluescript::aph(2")-Ic was constructed in the following manner. First, we cloned the 1,120-bp BamHI-HindIII fragment including the aph(2")-Ic gene into the polylinker of pBluescript II KS(+). Then, a unique NdeI site that includes the initiation codon was introduced by PCR (Platinum Taq DNA polymerase, high fidelity; Life Technologies) with two primers (primer sequences, 5′-ATG AGA TAG GAG AAC ATA TGA AAC AAA ATA AAC TTC AC-3′ and 5′-GTG AAG TTT ATT TTG TTT CAT ATG TTC TCC TAT CTC AT-3′). After PCR, methylated wild-type DNA was digested with DpnI endonuclease (New England Biolabs, Beverly, Mass.), the resulting digestion mixture was transformed into E. coli DH5α, and selection was performed on plates containing ampicillin (100 μg/ml). DNA from several colonies was analyzed for the presence of the NdeI site, and the complete nucleotide sequence of the gene was verified.
Reagents and chemicals.
Restriction enzymes and T4 ligase were purchased from New England Biolabs or Life Technologies. Netilmicin, dibekacin, and arbekacin were donated by Meiji Seika Kaisha (Tokyo, Japan). Isepamicin was donated by Schering-Plough Research Institute (Kenilworth, N.J.). All other antibiotics were purchased from Sigma Chemical Company (St. Louis, Mo.).
PCR mutagenesis.
Random PCR mutagenesis of the aph(2")-Ic gene was performed with the GeneMorph PCR mutagenesis kit (Stratagene). We used two primers, one containing a unique NdeI site (indicated in boldface) that includes the initiation codon (primer sequence, 5′-GAG ATA GGA GAA CAT ATG-3′) and the other containing a unique HindIII site (indicated in boldface) downstream from the termination codon (primer sequence, 5′-TCG ATA AGC TTC ATT AAG CAC T-3′). pBluescript::aph(2")-Ic was the template for the PCR. The reaction conditions were as suggested by Stratagene to provide a low-range mutation frequency (0 to 3 mutations/kb).
Cloning and mutant selection.
The PCR products were gel purified, digested with NdeI and HindIII, and ligated with pBluescript::aph(2")-Ic digested with the same restriction endonucleases. E. coli DH5α was electroporated with this ligation mixture. After 1 h of growth to allow expression of antibiotic resistance, the transformation mixture was diluted 10-fold with Luria-Bertani (LB) medium containing 100 μg of ampicillin per ml, and the mixture was incubated for an additional 3 h to enrich it with transformants. The ampicillin was removed by centrifugation, the pellets were resuspended in LB medium, and the cells were plated onto agar with an aminoglycoside at and above the MIC for the starting strain. In order to confirm that the observed resistance was due to mutations within the aph(2")-Ic gene cloned in pBluescript and not on the chromosome, we retransformed the DNA from the first-round transformants into E. coli DH5α. Transformants were selected on agar plates containing ampicillin, and individual colonies were tested for aminoglycoside susceptibility.
Susceptibility testing.
Initially, the MICs of various aminoglycosides were determined by a standard broth microdilution method (14). In order to determine more precisely the MICs conferred by various mutant enzymes, we tested additional aminoglycoside concentrations intermediate between standard twofold dilutions. MIC determinations were performed in quadruplicate in at least four independent experiments.
DNA sequencing and analysis.
Nucleotide sequencing was performed at the DNA Sequencing Core Facility, University of Michigan, Ann Arbor. OMIGA (version 2.0) software (Genetics Computer Group, Madison, Wis.) was used for analysis of the nucleotide sequences of wild-type and mutant aph(2")-Ic genes and the deduced amino acid sequences of their corresponding enzymes.
Selection of mutant enzymes.
In order to avoid mutants with alterations in the promoter region of the aph(2")-Ic gene, we introduced an NdeI site that includes the ATG start codon at the beginning of the structural gene and used a PCR primer that would ensure amplification and cloning of the DNA just following the initiating ATG codon. After the first round of random PCR mutagenesis, several E. coli transformants grew on agar with gentamicin at 32 and 64 μg/ml but not with gentamicin at 128 μg/ml. Combined DNA from first-round transformants was retransformed into E. coli DH5α. After selection on ampicillin, the aminoglycoside MICs for second-round transformants were determined. Four colonies for which the gentamicin MICs were the highest (128 μg/ml) were sequenced and were found to have the same point mutation, resulting in a His-258-Leu substitution in the APH(2")-Ic enzyme (one representative mutant was designated 763 [see Table 1]). Initial susceptibility testing of mutant 763 by a standardized twofold dilution method showed not only a fourfold increase in the MIC of gentamicin in comparison to the MIC for the wild-type strain but also a twofold increase in the MICs of tobramycin and dibekacin, a fourfold increase in the MIC of netilmicin, and a fourfold increase in the MIC of kanamycin; the mutation had no effect on susceptibility to neomycin, amikacin, arbekacin, or isepamicin (data not shown).
TABLE 1.
Susceptibility profiles conferred by APH(2")-Ic and its mutants cloned in the vector pBluescript in E. coli JM83
| Aminoglycoside | MIC (μg/ml) for the following mutants [mutation(s)]:
|
||||
|---|---|---|---|---|---|
| 791 (wild type) | 763 (His-258-Leu) | 777 (Phe-108-Leu) | 772 (His-258-Leu, Phe-108-Leu) | E. coli JM83 (pBluescript) | |
| Netilmicin | 2.0 | 12 | 8.0 | 24 | 0.2 |
| Kanamycin | 4.0 | 24 | 12 | 64 | 0.8 |
| Gentamicin | 32 | 128 | 48-64 | 96-128 | 0.25 |
| Tobramycin | 48 | 96 | 48 | 96 | 0.25 |
| Dibekacin | 128 | 256 | 256 | 256 | 0.25 |
| Neomycin | 1.0 | 1.0 | 1.0 | 1.0 | 0.4 |
| Amikacin | 1.0 | 1.0 | 1.0 | 1.0 | 0.8 |
| Arbekacin | 0.5 | 0.5 | 0.5 | 0.5 | 0.25 |
| Isepamicin | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 |
In order to obtain mutant enzymes that confer even higher levels of aminoglycoside resistance, we subjected the aph(2")-Ic structural gene in the recombinant plasmid DNA of mutant 763 to a second round of random PCR mutagenesis. The resulting transformation mixture was plated onto agar containing netilmicin, kanamycin, amikacin, arbekacin, or neomycin at concentrations above their MICs but not onto agar containing gentamicin, tobramycin, or dibekacin, since their MICs for mutant 763 were already high. No growth was observed on plates containing amikacin, arbekacin, or neomycin. The aph(2")-Ic genes from three colonies that grew on netilmicin were sequenced, and each had the same point mutation, producing a Phe-108-Leu substitution in the corresponding enzyme, in addition to the point mutation seen in strain 763 (one representative strain with the double mutation was designated 772 [see Table 1]).
Construction of an enzyme with a single mutation (Phe-108-Leu substitution).
To elucidate the effect of the Phe-108-Leu substitution alone on the aminoglycoside susceptibility profile, a plasmid with the aph(2")-Ic gene containing only the mutation resulting in the Phe-108-Leu substitution was constructed. This was achieved by substitution of a 300-bp ClaI fragment in mutant 772 with the corresponding ClaI fragment from the plasmid construct containing the wild-type aph(2")-Ic gene, thus eliminating the His-258-Leu substitution. The presence of this single mutation (mutant 777 in Table 1) was confirmed by nucleotide sequencing.
Resistance profiles conferred by mutant enzymes.
The effects of each of the enzymes with a single mutation and the enzyme with the double mutation on susceptibilities to various aminoglycosides were evaluated with greater precision. For determination of MICs, we used additional antibiotic concentrations intermediate between those obtained by conventional twofold dilutions. A comparison of the MICs for mutant 763 with those for the wild-type strain (strain 791) revealed that the replacement of His-258 by Leu was associated with two- to sixfold rises in the MICs of netilmicin, kanamycin, gentamicin, tobramycin, and dibekacin and no changes in the MICs of neomycin, amikacin, arbekacin, and isepamicin (Table 1). The Phe-108-Leu replacement in mutant 777 conferred two- to fourfold increases in the MICs of netilmicin, kanamycin, gentamicin, and dibekacin over those for the strain with the wild-type enzyme (Table 1). These increases are somewhat less than the effects exhibited by mutant 763. The two amino acid substitutions in APH(2")-Ic (mutant 772) resulted in 12- and 16-fold increases in the MICs of netilmicin and kanamycin, respectively (Table 1). Thus, the presence of these two mutations together in the aph(2")-Ic gene conferred greater rises in the MICs of netilmicin and kanamycin than the rises conferred by either mutation alone.
Amino acid sequences of APHs.
Comparison of the predicted amino acid sequences of known APHs shows that they contain a number of conserved regions throughout their primary structures (12, 15). Results from active-site labeling, site-directed mutagenesis, and crystallographic studies of APH(3′)-IIIa, plus site-directed mutagenesis of APH(2")-Ia, have shown the importance for ATP binding of a conserved Lys residue in the N-terminal regions of these two APH enzymes (3, 8, 13). On the other hand, mutagenesis and computer modeling studies of the APH(3′)-IIIa enzyme have shown the importance of the carboxy-terminal portion in aminoglycoside recognition and binding (16). Three motifs (motifs 1, 2, and 3) have been recognized within conserved regions in the carboxy half of the APHs and have been hypothesized to play important roles in enzymatic activity (12, 15). Single amino acid substitutions within these three motifs have been found to result in the reduction or elimination of resistance to various aminoglycosides (2, 4, 6, 8, 10, 19). In addition, an eightfold increase in the level of resistance to amikacin was reported to result from a substitution in motif 2 of the aph(3′)-IIa gene. However, the same substitution also resulted in declines in the levels of resistance to five other aminoglycosides (11).
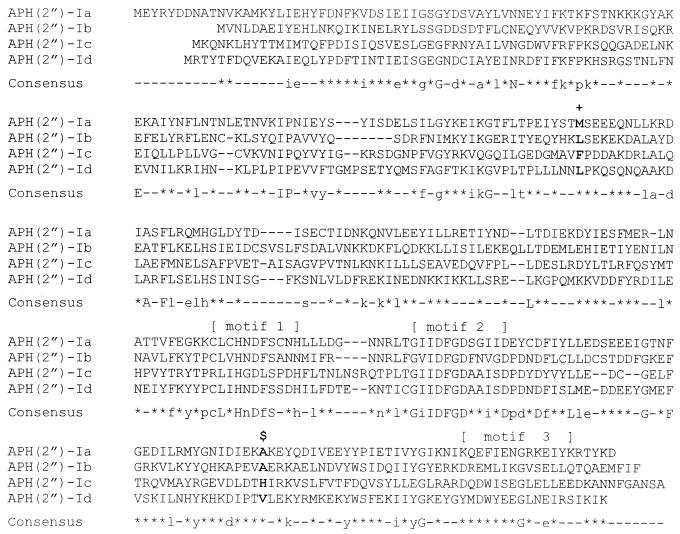
Comparison of amino acid sequences of the four enterococcal APH(2") enzymes indicates that they exhibit from 25 to 33% identity and from 44 to 54% similarity (5, 9, 17). Alignment of their amino acid sequences shows that they contain multiple conserved regions in both the N- and C-terminal halves (see the consensus sequence in Fig. 1). Regions corresponding to motifs 1, 2, and 3 in the other classes of APHs [the APH(3′), APH(3"), APH(4), and APH(6) enzymes] (15) are also identifiable in the APH(2") enzymes. Motif 2 is especially well conserved; in fact, there is 100% identity in motif 2 between APH(2")-Ic and APH(2")-Id (Fig. 1). Motif 1 is easily recognizable, but the degree of conservation in the region corresponding to motif 3 is much less (Fig. 1). It is noteworthy that neither the Phe-108-Leu substitution nor the His-258-Leu substitution generated in this study is located within motif 1, 2, or 3. Examination of the amino acid residues in the alignment at position 108 of APH(2")-Ic (Fig. 1) shows that APH(2")-Ic has a bulky aromatic Phe, whereas the others have an aliphatic Leu or Met. It is of note that the Phe-108-Leu substitution increased the degree of conservation at this position. Similarly, the His-258-Leu substitution increased the degree of conservation at this site. This substitution replaced a charged residue with a hydrophobic amino acid; the other three enterococcal phosphotransferases, APH(2")-Ia, APH(2")-Ib, and APH(2")-Id, also have a hydrophobic residue at this position (Fig. 1).
FIG. 1.
Alignment of APH(2") enzymes from enterococci. In the consensus sequence, capital letters indicate identical amino acids in all four sequences, lowercase letters indicate identical amino acids in three of the sequences, and asterisks indicate identical amino acids in two of the sequences. +, site of the Phe-108-Leu substitution; $, site of the His-258-Leu substitution.
In contrast to previous studies in which mutants of aminoglycoside-modifying enzymes were obtained by specific mutagenesis of a relatively small number of residues within conserved regions, we introduced by PCR random mutations throughout the entire gene and selected for enhanced resistance. We were able to obtain a single mutation (at position 258) sufficient to confer elevated levels of aminoglycoside resistance. A second round of PCR mutagenesis allowed us to generate an additional mutation at position 108 that increased the level of resistance even further. Both of these mutations that we obtained are at positions outside the recognized conserved regions of APH enzymes (15).
Although it is clear that the alterations in aminoglycoside resistance of the mutants arose from the observed mutations in APH(2")-Ic, the mechanism(s) for this enhancement of resistance is not known. These mutations could have resulted in increased amounts of mutant enzymes and/or alteration of their specific activities against various substrates. The quantity of APH(2")-Ic protein from wild-type and mutant strains that was observed in sodium dodecyl sulfate-polyacrylamide gels could not be correlated precisely with resistance levels (data not shown). The possible role of altered catalytic activity in determining the resistance profiles of the mutants remains to be investigated by kinetic analyses of their enzymes. Further studies such as X-ray crystallographic analysis should also help to elucidate the roles of our mutant residues.
Acknowledgments
This study was supported by a merit review grant from the Medical Research Service of the Department of Veterans Affairs.
REFERENCES
- 1.Ausubel, F. M., R. Brent, R. E. Kingston, D. D. Moore, J. G. Seidman, J. A. Smith, and K. Struhl. 1995. Current protocols in molecular biology, vol. 1. John Wiley & Sons, Inc., New York. N.Y.
- 2.Blázquez, J., J. Davies, and F. Moreno. 1991. Mutations in the aphA-2 gene of transposon Tn5 mapping within the regions highly conserved in aminoglycoside-phosphotransferases strongly reduce aminoglycoside resistance. Mol. Microbiol. 5:1511-1518. [DOI] [PubMed] [Google Scholar]
- 3.Boehr, D. D., W. S. Lane, and G. D. Wright. 2001. Active site labeling of the gentamicin resistance enzyme AAC(6′)-APH(2") by the lipid kinase inhibitor wortmannin. Chem. Biol. 8:791-800. [DOI] [PubMed] [Google Scholar]
- 4.Boehr, D. D., P. R. Thompson, and G. D. Wright. 2001. Molecular mechanism of aminoglycoside antibiotic kinase APH(3′)-IIIa. J. Biol. Chem. 276:23929-23936. [DOI] [PubMed] [Google Scholar]
- 5.Chow, J. W., M. J. Zervos, S. A. Lerner, L. A. Thal, S. M. Donabedian, D. D. Jaworski, S. Tsai, K. J. Shaw, and D. B. Clewell. 1997. A novel gentamicin resistance gene in Enterococcus. Antimicrob. Agents Chemother. 41:511-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daigle, D. M., G. A. McKay, P. R. Thompson, and G. D. Wright. 1999. Aminoglycoside antibiotic phosphotransferases are also serine protein kinases. Chem. Biol. 6:11-18. [DOI] [PubMed] [Google Scholar]
- 7.Ferretti, J. J., K. S. Gilmore, and P. Courvalin. 1986. Nucleotide sequence analysis of the gene specifying the bifunctional 6′-aminoglycoside acetyltransferase 2"-aminoglycoside phosphotransferase enzyme in Streptococcus faecalis and identification and cloning of gene regions specifying the two activities. J. Bacteriol. 167:631-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hon, W. C., G. A. McKay, P. R. Thompson, R. M. Sweet, D. S. C. Yang, G. D. Wright, and A. M. Berghuis. 1997. Structure of an enzyme required for aminoglycoside antibiotic resistance reveals homology to eukaryotic protein kinases. Cell 89:887-895. [DOI] [PubMed] [Google Scholar]
- 9.Kao, S. J., I. You, D. B. Clewell, S. M. Donabedian, M. J. Zervos, J. Petrin, K. J. Shaw, and J. W. Chow. 2000. Detection of the high-level aminoglycoside resistance gene aph(2")-Ib in Enterococcus faecium. Antimicrob. Agents Chemother. 44:2876-2879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kocabiyik, S., and M. H. Perlin. 1992. Site-specific mutations of conserved C-terminal residues in aminoglycoside 3′-phosphotransferase II: phenotypic and structural analysis of mutant enzymes. Biochem. Biophys. Res. Commun. 185:925-931. [DOI] [PubMed] [Google Scholar]
- 11.Kocabiyik, S., and M. H. Perlin. 1992. Altered substrate specificity by substitutions at Tyr218 in bacterial aminoglycoside 3′-phosphotransferase II. FEMS Microbiol. Lett. 93:199-202. [DOI] [PubMed] [Google Scholar]
- 12.Martin, P., E. Jullien, and P. Courvalin. 1988. Nucleotide sequence of Acinetobacter baumannii aphA-6 gene: evolutionary and functional implications of sequence homologies with nucleotide-binding proteins, kinases and other aminoglycoside-modifying enzymes. Mol. Microbiol. 2:615-625. [DOI] [PubMed] [Google Scholar]
- 13.McKay, G. A., R. A. Robinson, W. S. Lane, and G. D. Wright. 1994. Active-site labeling of an aminoglycoside antibiotic phosphotransferase (APH(3′)-IIIa). Biochemistry 33:14115-14120. [DOI] [PubMed] [Google Scholar]
- 14.National Committee for Clinical Laboratory Standards. 1999. Approved standard M7-A5: methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 5th ed. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 15.Shaw, K. J., P. N. Rather, R. S. Hare, and G. H. Miller. 1993. Molecular genetics of aminoglycoside resistance genes and familial relationships of the aminoglycoside-modifying enzymes. Microbiol. Rev. 57:138-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson, P. R., J. Schwartzenhauer, D. W. Hughes, A. M. Berghuis, and G. D. Wright. 1999. The COOH terminus of aminoglycoside phosphotransferase (3′)-IIIa is critical for antibiotic recognition and resistance. J. Biol. Chem. 274:30697-30706. [DOI] [PubMed] [Google Scholar]
- 17.Tsai, S. F., M. J. Zervos, D. B. Clewell, S. M. Donabedian, D. F. Sahm, and J. W. Chow. 1998. A new high-level gentamicin resistance gene. aph(2")-Id, in Enterococcus spp. Antimicrob. Agents Chemother. 42:1229-1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vakulenko, S. B., B. Geryk, L. P. Kotra, S. Mobashery, and S. A. Lerner. 1998. Selection and characterization of β-lactam-β-lactamase inactivator-resistant mutants following PCR mutagenesis of the TEM-1 β-lactamase gene. Antimicrob. Agents Chemother. 42:1542-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yenofsky, R. L., M. Fine, and J. W. Pellow. 1990. A mutant neomycin phosphotransferase II gene reduces the resistance of transformants to antibiotic selection pressure. Proc. Natl. Acad. Sci. USA 87:3435-3439. [DOI] [PMC free article] [PubMed] [Google Scholar]