Short abstract
Most new human infections are of animal origin, but there is rarely sufficient evidence to make a risk assessment of the zoonotic potential of emerging animal diseases. An algorithm for early qualitative public health risk assessment has been developed to guide risk management
Most newly emerging human infections of global importance are of animal origin,1 w1 but early accurate predictions of zoonotic risk of emerging animal diseases are difficult, as shown by the epidemic of bovine spongiform encephalopathy and variant Creutzfeldt-Jakob disease in the United Kingdom.w2 Miscalculation, delays, or poor risk communication can result in failure to protect the public's health and undermine public trust,2 but overreaction can waste resources and even harm the economy of countries, as in the case of suspected plague in India.3 The public are increasingly anxious to understand the basis on which a government's decisions on risk management are taken,w3 but scientists and government may be reluctant to engage with the public at an early stage because of the fear of provoking a public scare. However, since the BSE epidemic, it has been accepted that the criteria used and the evidence considered in risk assessments should be open and explicit.4 w4 w5
In this article we describe and illustrate such an approach, one that explicitly distinguishes evidence of lack of zoonotic potential from lack of evidence. The algorithm, endorsed by the UK government's Zoonoses Groupw6 and by the National Expert Panel on New and Emerging Infection,w7 is being used by the Human and Animal Infections and Risk Surveillance Group of the Health Protection Agency.5
Methods
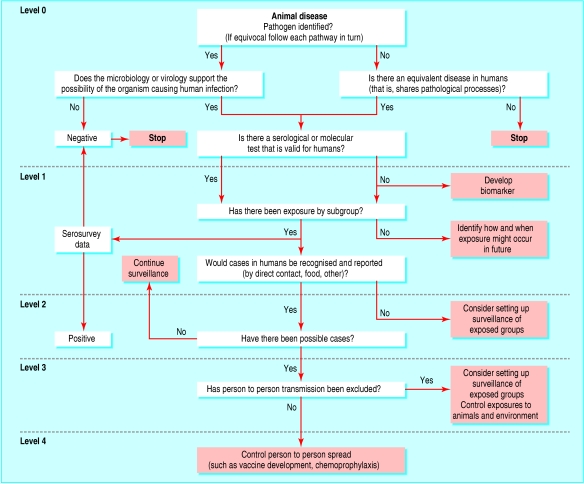
The algorithm (figure) is used to categorise the evidence of zoonotic potential into four levels (box 1) by considering three key stages in the transmission of zoonoses:
Figure 1.
Template for qualitative risk assessment of zoonotic potential of animal diseases
The risk of cross species transmission—Seek to identify criteria that might exclude the possibility of human infection if exposure occurred (box 2). If these criteria do not support human infection, or there is no equivalent disease process in humans, it is defensible to take no further action. If human infection is biologically plausible then the availability and use of a serological or molecular test for exposed humans should be considered.
Exposure of humans to infected animals and secondary sources—The full range of possible exposures needs to be addressed systematically, including occupational, recreational, domestic, food and waterborne, and travel. Negative serosurveys reduce concern about the zoonotic potential.
Human infection and subsequent human to human transmission—The absence of reported cases must be assessed in relation both to opportunities for exposure and the sensitivity of surveillance systems to detect human cases. At each point of assessment, the quality and completeness of available data must be considered.
Box 1: Levels of confidence of risk of zoonotic transmission of animal diseases
Level 0: Not zoonotic—Evidence of lack of zoonotic potential. Good grounds for not taking further action
Level 1: Potential zoonosis—Possibility of human pathogenicity not excluded. Work needed on biomarkers of infection and pathways of exposure
Level 2: Potential zoonosis—Serological evidence of infection, or human exposure has occurred but surveillance not sufficiently reliable. Enhanced surveillance needed
Level 3: Confirmed zoonosis—Human cases have been reported, but evidence against person to person spread. Enhanced surveillance needed. Control exposure of humans to animals and environmental sources
Level 4: Confirmed zoonosis—Human cases have occurred, with subsequent person to person spread not excluded. Control of direct or indirect person to person spread needed
Worked examples
The algorithm was applied to five emerging animal diseases of concern to public health authorities. A possible link between porcine dermatitis and nephropathy syndrome (PDNS) and Henoch-Schönlein purpuraw8 was raised by medical practitioners in East Anglia and was referred to the Public Health Laboratory Service Advisory Committee on Zoonoses by the Department of Health. Clostridium difficile in pigs was referred to the advisory committee by the director of the Public Health Laboratory Service because of recent reports from the United States that piglet neonatal enteritis due to C difficile had become epidemic there,w9 and that typing studies had suggested that pig isolates had also been documented in human cases. Porcine hepatitis E,w10 bovine norovirus,w11 and Borna disease virusesw12 were identified by the advisory committee itself as priorities for assessment.
Porcine hepatitis E
Pathogen—Hepatitis E virus.6
Agent characteristics—Unclassified and is recognised in pigs, rats, and humans with no important virological differences in the agents.
Disease characteristics—Usually a self limiting illness, but fulminant hepatitis is recognised in high risk groups such as pregnant women.w10 No disease is identified in pigs. Hepatitis E is a recognised human infection in the UK, mainly associated with travel abroad.7
Biomarkers in humans—Virological diagnosis is possible by serology and virus characterisation by the polymerase chain reaction and sequencing.w13
Exposure—Infection is common in UK pigs,w14 and direct occupational human exposure is likely. Occupation exposure studies have not been carried out to our knowledge in the UK. Virus was considered likely to contaminate food and the environment.
Diagnosis or recognition—Serological diagnosis is available, but testing is not routine for hepatitis cases in the UK without a history of foreign travel; therefore, sporadic cases may well be missed.
Box 2: Some virological criteria to consider to assess zoonotic risk of viral infections
Viral factors
Virus family, genus, and species
Evidence of interspecies transmission in virus family
Any related human viruses
Phylogenetic relationship with human strains
Genetic stability or diversity RNA or DNA Segmented genome
Culturable in human cells
Virus host factors
Virus specific host receptors
Poikilothermic v homoeothermic body temperature
Putative cases—Human cases of hepatitis E associated with pigs have been reported since the appraisal was conducted.7 There have also been few human cases in the UK with no foreign travel history from whom hepatitis E with a sequence very close to the European pig strain have been characterised. In other countries serosurveys show higher prevalence of infection with hepatitis E virus in veterinarians and pig farmers than controls.w15
Person to person transmission—No cases documented yet to our knowledge.
Conclusion and recommendation—Level 2 zoonosis. Porcine hepatitis E might cause human infections, but sporadic cases in the UK may be missed since the epidemiology of human infections is lacking. We cannot therefore be confident that the absence of reported cases indicates absent or low risk. Enhanced surveillance of cases of non-A, non-B, non-C hepatitis should be instituted, and occupational exposure studies should be carried out.
Porcine circovirus
Pathogen—Circovirus infection is believed to be associated with post-weaning multi-systemic wasting syndrome (PMWS) and PDNS disease in pigs, but its aetiological agent is still debated.8
Agent characteristics—Circovirus is similar to but distinct from human transfusion transmitted (TT) virus.w16 There are insufficient direct studies looking for circovirus in humans to exclude the possibility of human infection.
Disease characteristics—Suggested similarities between the pathology of Henoch-Schönlein purpura in humans and PDNS led to the review.w14
Biomarkers in humans—Virological diagnosis by serology and virus characterisation by the polymerase chain reaction and sequencing is possible.w16
Exposure—The disease is widespread in pigs,w14 and the agent could contaminate meat and the environment.
Diagnosis or recognition—There is no surveillance system for Henoch-Schönlein purpura, and human cases occurring in conjunction with infected pigs could easily be missed. However, a US serosurvey of 50 veterinarians exposed to PMWS found no seropositive cases.9 Surveys of blood donors have also proved negative.w16
Putative cases—Time trends and geographical patterns of human Henoch-Schönlein purpura across England and Wales have been compared with the evolution of the PMWS epidemic, and there is no evidence of a link between the two diseases.w14
Conclusion and recommendation—Level 0 zoonosis. Though theoretically plausible, infection has not been shown in humans exposed to infected pigs. The epidemiological pattern of Henoch-Schönlein purpura is not related to the epidemiology of PMWS in the UK. To date, there is some evidence that porcine circovirus is not a significant zoonotic risk to occupationally exposed groups. Further serological studies in exposed groups in the UK would strengthen this conclusion.
Bovine norovirus
Pathogen—Norovirus (previously known as Norwalk-like or small round structured virus).w17
Agent characteristics—Noroviruses cause infection and illness in cattle, pigs, and humans. Virological studies suggest recombination events are common.w18 Interspecies transmission is established for viruses belonging to the caliciviridae family.w19
Disease characteristics—Gastroenteritis in humans and cattle.
Biomarkers in humans—The polymerase chain reaction and sequencing are widely used for diagnosis and would identify bovine strains in human infections. Serology is available by means of recombinant capsids.w19
Exposure—Bovine infection is widespread, and human occupational exposure is likely. In theory milk might become contaminated, although pasteurisation should destroy the virus. Shellfish contamination was also considered possible through slurry.
Diagnosis or recognition—Viral gastroenteritis in humans is so common that sporadic cases from bovine contact are unlikely to be recognised epidemiologically.w20
Putative cases—Several thousand strains of norovirus from human infections have been sequenced over the past 10 years, and no porcine or bovine norovirus strains have been detected among these strains infecting humans.10,11
Conclusion and recommendation—Level 0 zoonosis. There is good evidence that bovine norovirus is not a significant zoonosis, even though agent characteristics provide grounds for concern about zoonotic potential. No specific action is recommended.
Borna disease virus
Pathogen—Borna disease virus causes a neurological disease of horses and other domesticated animals.12
Agent characteristics—Wide host range, high sequence homology of virus isolates has been reported.12
Disease characteristics—Causes behavioural abnormalities in experimentally infected primates.12
Biomarkers in humans—Serological and molecular tests have been developed for human samples, but their specificity is still debatable.13
Exposure—Human exposure to infected animals is widespread in central Europe.
Diagnosis or recognition—Borna disease virus has been proposed as the cause of a range of common chronic diseases—including depression, schizophrenia, and chronic fatigue syndrome—but it is most unlikely that occasional cases of mental illness caused by the virus would be identified.
Putative cases—Cases have been proposed, but diagnostic and serological studies are controversial.13 There is some evidence of increased prevalence of antibodies to the virus in certain patient groups (such as patients with schizophrenia or neurological disease).14
Person to person spread—Higher seroprevalence has been reported in relatives of schizophrenic patients and mental health workers. Family clusters of Borna disease have been reported in Germany.13
Conclusion and recommendation—Level 2 zoonosis. The weakness in the evidence of the zoonotic potential of Borna disease virus is because of the uncertain specificity of human serological tests, and therefore the interpretation of serosurveys in humans. Better serological and molecular tests should be developed and applied to exposed groups.
Clostridium difficile
Pathogen—Clostridium difficile.15
Agent characteristics—Widespread in animal hosts and the environment, with many subtypes shared between animals and humans.w21 The a and b toxins have been shown to cause disease in humans.15
Disease characteristics—Pseudomembranous colitis is seen mainly in people aged > 65 years who have recently had antimicrobial treatment.w22
Biomarkers in humans—Reliable tests to detect both a and b toxins in faeces are available commercially.15 C difficile may also be cultured from faeces of patients with diarrhoea caused by toxins in the gut.15
Exposure—Occupational human exposure to infected or colonised animals was thought probable.
Diagnosis or recognition—Strains of C difficile causing animal disease have also been identified in human cases.w21
Putative cases—No human cases linked to specific animal infection have yet been reported.
Person to person spread—Cross infection can occur in hospital wards.w22
Conclusion and recommendation—Level 2 zoonosis. Human exposure from animal cases is likely, but, since human infection usually only occurs in debilitated patients who have recently taken antibiotics, zoonotic cases are unlikely. However, current surveillance is not sensitive enough to detect such sporadic occurrences. No additional action is recommended at this time.
Discussion
We sought explicit criteria to judge the possibility of animal infections causing human diseases. However, even in the special case of xenotransplantation there does not seem to be an agreed approach, beyond “sound professional judgment” of panels of experts representing all scientific fields.16 w23 Special attention has been devoted in the literature to porcine endogenous retroviruses,w24 w25 where nucleic acid sequence homology, cellular receptors, and the potential for protein and gene expression suggest multiple possible sites for infection in humans.w26 However, the real test of zoonotic potential, the occurrence of infection in exposed people, has not been found, although study numbers are small.17
Only rarely will the biological evidence available for risk assessment be so detailed as for porcine endogenous retroviruses. A more common scenario is illustrated by Audelo-del-Valle et al,18 who argue that Taura syndrome virus of penaeid shrimps is a member of the “picornavirus superfamily,” which includes human pathogens, and that it could “potentially represent a public health threat.” However, the questions for public health are how much weight should be given to this concern and what resources should be given to assessing the risk. The authors reported infection of cultured human and monkey cell lines with Taura syndrome virus,18 but others have failed to replicate the findings.19
At current levels of knowledge, only rarely could the possibility of human infection be excluded on microbiological or virological grounds, and as virological knowledge increases even well established human infections may be recognised as zoonoses, as in the case of rotavirus.20 w27 Absence of growth in human cells in culture is not a reliable criterion, since many human viruses do not grow in commonly used cell cultures (such as norovirus).w28 Physiological differences between cold blooded and warm blooded animal cells may be an important barrier to transmission, as was concluded for infectious salmon anaemia,21 w29 w30 but there are examples of avian viruses, such as avian fluw31 and Newcastle disease,w32 overcoming smaller temperature barriers (avian body temperature 40°C, human body temperature 37°C).
In developing a broader public health approach in which absence of evidence is distinguished from evidence of no risk, it is worth noting that human exposure is often likely to occur first in occupational groups,w33 and serosurveys of such groups are helpful. For example, the absence of infection in workers exposed to porcine circovirus suggests that this virus is not a zoonosis.9 On the other hand, seropositivity in handlers of macaques infected with simian parvovirus22 would designate it as a level 2 zoonosis and would justify enhanced surveillance of human cases, as well as extra precautions for seronegative pregnant women who might be exposed. Development of serum archives representing occupational groups at risk would be a major and urgently needed strategic response to emerging infections.23 w34-w36
The algorithm we developed provides a discipline that ensures that the strength of evidence and the adequacy of surveillance are addressed and provides stopping rules necessary for public health decision makers. We have distinguished four levels of zoonotic potential, although this is not essential to the process and the usefulness of setting levels has yet to be established. The important outputs of the algorithm are the decisions made to enhance surveillance or develop and use serological tests.
Summary points
Most serious emerging infections are of animal origin
When a new animal disease emerges virological and microbiological criteria are usually insufficient to make the risk assessment of zoonotic potential
An algorithm for early qualitative public health risk assessment has been developed that exposes the strengths and weaknesses of available evidence on risk
Assessment with this approach indicated the need for further investigation of the zoonotic potential of porcine hepatitis E, but not for porcine circovirus and bovine norovirus at this time
Systematic enhanced surveillance of occupationally exposed groups is recommended
Supplementary Material
 Extra references w1-w36 appear on bmj.com
Extra references w1-w36 appear on bmj.com
We thank the members of the ad hoc panel of experts who performed one or more of the risk assessments described above: Jim Gray, Miren Iturriza, Chong-Gee Teo, Virus Reference Department, Health Protection Agency Centre for Infections, London; M Banks, Central Veterinary Laboratory, Weybridge; J Bridger, Royal Veterinary College, Camden, London; J Gentsch, Viral Gastroenteritis Laboratory, CDC, Atlanta GA, USA; D Thomas, National Public Health Service for Wales, Cardiff; and Tim Coleman, Hereford Public Health Laboratory.
Competing interests: None declared.
References
- 1.Taylor LH, Latham SM, Woolhouse ME. Risk factors for human disease emergence. Philos Trans R Soc Lond B Biol Sci 2001;356: 983-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanska DJ. The mad cow problem in the UK: risk perceptions, risk management, and health policy development. J Public Health Policy 1998;19: 160-83. [PubMed] [Google Scholar]
- 3.Cash RA, Narasimhan V. Impediments to global surveillance of infectious diseases: consequences of open reporting in a global economy. Bull World Health Organ 2000;78: 1358-67. [PMC free article] [PubMed] [Google Scholar]
- 4.Strategy Unit, Cabinet Office. Risk: improving government's capability to handle risk and uncertainty. London: Strategy Unit, 2002 (www.strategy.gov.uk/downloads/su/risk/risk/report/report/downloads/su-risk.pdf).
- 5.Morgan D. The Human Animal Infections and Risk Surveillance group (poster No 33). In: Proceedings of the 2nd International Conference on the Prevention and Control of Zoonoses, from Science to Policy. 2005 Jun 15-17; In: Liverpool, UK. www.hpazoonosesconference.org.uk/PrevCtrlZoon05_posters.pdf (accessed 14 Nov 2005).
- 6.Meng X-J. Zoonotic and xenozoonotic risks of the hepatitis E virus. Infect Dis Rev 2000;2: 35-41. [Google Scholar]
- 7.Ijaz S, Arnold E, Banks M, Bendall RP, Cramp ME, Cunningham R, et al. Non-travel-associated hepatitis e in England and Wales: demographic, clinical, and molecular epidemiological characteristics. J Infect Dis 2005;192: 1166-72. (Epub 2005 Aug 22.) [DOI] [PubMed] [Google Scholar]
- 8.Chae C. A review of porcine circovirus 2-associated syndromes and diseases. Vet J 2005;169: 326-36. [DOI] [PubMed] [Google Scholar]
- 9.Ellis JA, Wiseman BM, Allan G, Konoby C, Krakowka S, Meehan BM, et al. Analysis of seroconversion to porcine circovirus 2 among veterinarians from the United States and Canada. J Am Vet Med Assoc 2000;217: 1645-6. [DOI] [PubMed] [Google Scholar]
- 10.Oliver SL, Dastjerdi AM, Wong S, El-Attar L, Gallimore C, Brown DW, et al. Molecular characterization of bovine enteric caliciviruses: a distinct third genogroup of noroviruses (Norwalk-like viruses) unlikely to be of risk to humans. J Virol 2003;77: 2789-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smiley JR, Hoet AE, Traven M, Tsunemitsu H, Saif LJ. Reverse transcription-PCR assays for detection of bovine enteric caliciviruses (BEC) and analysis of the genetic relationships among BEC and human caliciviruses. J Clin Microbiol 2003;41: 3089-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cotto E, Neau D, Cransac-Neau M, Auriacombe M, Pellegrin JL, Ragnaud JM, et al. Borna disease virus RNA in immunocompromised patients in southwestern France. J Clin Microbiol 2003;41: 5577-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chalmers RM, Thomas DR, Salmon RL. Borna disease virus and the evidence for human pathogenicity: a systematic review. Q J Med 2005;98: 255-74. [DOI] [PubMed] [Google Scholar]
- 14.Davidson F, Lycett C, Petrik J, Fazakerley JK. Investigation of frequency of active Borna disease virus infection in Scottish blood donors. Vox Sang 2004;86: 148-50. [DOI] [PubMed] [Google Scholar]
- 15.Poxton IR. Clostridium difficile. J Med Microbiol 2005;54: 97-100. [Google Scholar]
- 16.World Health Organization. Xenotransplantation: guidance on infectious disease prevention and management. In: Emerging and other communicable diseases surveillance and control. Geneva: WHO, 1998. (WHO/EMC/200/98.1.)
- 17.Boneva RS, Folks TM. Xenotransplantation and risks of zoonotic infection. Ann Med 2004;36: 504-17. [DOI] [PubMed] [Google Scholar]
- 18.Audelo-del-Valle J, Clement-Mellado O, Magana-Hernandez A, Flisser A, Montiel-Aguirre F, Briseno-Garcia B. Infection of cultured human and monkey cell lines with extract of penaeid shrimp infected with Taura syndrome virus. Emerg Infect Dis 2003;9: 265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pantoja CR, Navarro SA, Naranjo J, Lightner DV, Gerba CP. Nonsusceptibility of primate cells to Taura syndrome virus. Emerg Infect Dis 2004;10: 2106-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cook N, Bridger J, Kendall K, Gomara MT, El-Attar L, Gray J. The zoonotic potential of rotavirus. J Infect 2004;48: 289-302. [DOI] [PubMed] [Google Scholar]
- 21.Scientific Committee on Animal Health and Animal Welfare. Assessment of zoonotic risk from infectious salmon anaemia virus. Brussels: European Commission Health and Consumer Protection Directorate-General, 2000. (http://europa.eu.int/comm/food/fs/sc/scah/out44_en.pdf).
- 22.Brown KE, Liu Z, Gallinella G, Wong S, Mills IP, O'Sullivan MG. Simian parvovirus infection: a potential zoonosis. J Infect Dis 2004;190: 1900-7. [DOI] [PubMed] [Google Scholar]
- 23.Thomas DR, Salmon RL, Coleman TJ, Morgan-Capner P, Sillis M, Caul EO, et al. Occupational exposure to animals and risk of zoonotic illness in a cohort of farmers, farm workers and their families in England. J Agric Saf Health 1999;5: 373-82. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.