Abstract
The Medical Library Association's “Standards for Hospital Libraries 2002” have been developed as a guide for hospital administrators, librarians, and accrediting bodies to ensure that hospitals have the resources and services to effectively meet their needs for knowledge-based information. Specific requirements for knowledge-based information include that the library be a separate department with its own budget. Knowledge-based information in the library should be directed by a qualified librarian who functions as a department head and is a member of the Academy of Health Information Professionals. The standards define the role of the medical librarian and the links between knowledge-based information and other functions such as patient care, patient education, performance improvement, and education. In addition, the standards address the development and implementation of the knowledge-based information needs assessment and plans, the promotion and publicity of the knowledge-based information services, and the physical space and staffing requirements. The role, qualifications, and functions of a hospital library consultant are outlined. The health sciences library is positioned to play a key role in the hospital. The increasing use of the Internet and new information technologies by medical, nursing, and allied health staffs; patients; and the community require new strategies, strategic planning, allocation of adequate resources, and selection and evaluation of appropriate information resources and technologies. The Hospital Library Standards Committee has developed this document as a guideline to be used in facing these challenges.
Editor's Note: The “Standards for Hospital Libraries 2002” were approved by the members of the Hospital Library Section during MLA '02 in Dallas, Texas. They were subsequently approved by Section Council and received final approval from the MLA Board of Directors in June 2002. They succeed the Standards for Hospital Libraries published in 1994 and the Minimum Standards for Health Sciences Libraries in Hospitals from 1983. A Frequently Asked Questions document discussing the development of the new standards can be found on the Hospital Library Section Website at http://www.hls.mlanet.org.
INTRODUCTION
The Medical Library Association's “Standards for Hospital Libraries 2002” have been developed as a guide for hospital administrators, librarians, and accrediting bodies to ensure that hospitals have the resources and services to effectively meet their needs for knowledge-based information (KBI). KBI refers to current expert information, produced externally to the organization, including:
journals, texts, documents, and databases in print or electronic format
benchmarks, best practices, guidelines, and consensus development statements
research studies
quality-filtered Internet resources
KBI is vital to the hospital, in that it supports:
patient care
managerial and strategic decision making
performance improvement and patient safety
lifelong learning and professional competence of hospital and medical staff
patient and family education
research initiatives
The medical librarian, as a specialized information professional, is uniquely prepared to provide the oversight and management of KBI resources and services to the hospital or health system. The medical librarian brings specialized competencies to the institution for the selection, organization, dissemination, and integration of KBI resources into the day-to-day operations of the institution.
STANDARD 1
The library serves as the primary department responsible for developing systems and services to meet the knowledge-based information (KBI) needs of the organization. The library has its own budget, and the director, as a department head, reports to the senior management of the organization.
Intent
As reflected in the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) process and documentation, access to knowledge-based information is one of the four primary components of the information management requirements for a hospital or health system. To enable the development of systems, resources, and services to meet this functional requirement, the needs, concerns, and contribution of the library must be communicated to decision makers at the highest levels in the organization. Departmental status facilitates this process. The continuous interaction of the librarian with other departmental managers and with administrators fosters a deeper understanding of the information needs of the organization. This interaction can also provide access to institutional resources and data necessary for the provision of information to satisfy the needs of customers.
The term “senior management” refers to the administrative level. In a large teaching hospital, the director of medical education may be considered senior management.
STANDARD 2
KBI systems and services are directed by a qualified librarian. Membership in the Academy of Health Information Professionals is preferred.
Intent
A qualified librarian is a person who has earned a master's degree from a program accredited by the American Library Association or its successor accrediting organization or from a master's level program in library and information studies accredited or recognized by the appropriate national body of another country.
Membership in the Medical Library Association's Academy of Health Information Professionals is one indication of a knowledgeable, capable medical librarian. The Special Libraries Association's Competencies for Special Librarians of the 21st Century outlines the competencies and skills expected of special librarians, including health sciences librarians.
The unique competencies of the hospital librarian include in-depth knowledge of print and electronic information resources in the health sciences and related fields and the design and management of information services that meet the strategic information needs of the individual or group being served. In support of this mission, the role of the medical librarian includes:
coordinating the function of the library with the primary mission of the institution
strategic planning for library operations
budgeting for library operations
providing effective leadership in KBI
recommending appropriate professional and support staffing for the library
recommending appropriate space for the library
developing and implementing KBI-related policies and procedures
developing a performance improvement program for the KBI function
hiring and evaluating the performance of the library staff
providing training and educational opportunities for the library staff
selecting and evaluating information resources in any format for incorporation into the physical or virtual collection
evaluating new information technologies and assessing their application to library management and services
negotiating license agreements with vendors of publications and databases
responding in a timely manner to all requests for information related to patient care or patient safety
performing mediated searches of Internet and KBI resources
training users in searching and evaluating information resources
providing tailored information to groups or individuals within the institution
performing other activities as appropriate
Reliance on a commercial electronic resource for clinical information cannot substitute for a qualified medical librarian.
STANDARD 3
The library staffing formula is used to determine hospital library staffing needs.
Intent
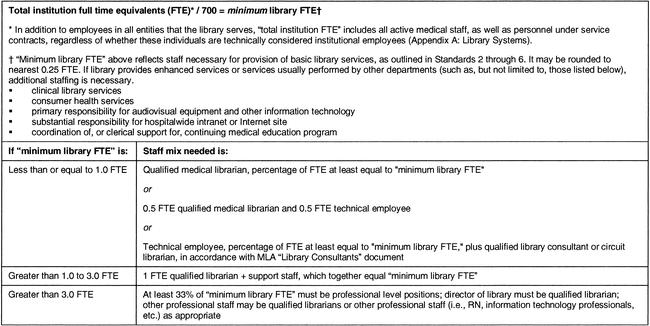
An understaffed library cannot fully serve the KBI needs of the hospital and medical staff. Workload is driven by the size and complexity of the institution served (Figure 1).
Figure 1 Library staffing formula
STANDARD 4
The librarian, as the key KBI professional in the organization, is an active member of the information management teams.
Intent
The medical librarian is involved during planning for internal computer networks and external linkages to help ensure adequacy, coordination, and accessibility of all KBI resources within the organization.
STANDARD 5
Evidence demonstrates effective connections between KBI and patient care and patient education, performance improvement and patient safety functions, educational functions for hospital and medical staff, and other appropriate functions.
Intent
The library serves all user groups in the hospital. The functions listed above are among the most dependent on knowledge-based information. Examples of connections and evidence include:
Patient care: frequent provision of information on which patient care decisions are based, integration of KBI resources into point-of-care systems, provision of clinical library services or attendance at morning report or rounds, and provision of case-specific literature in support of rounds and related activities
Performance Improvement and Patient Safety: active membership of the librarian on performance improvement and patient safety team(s), as reflected in minutes or other documentation (preferred); frequent provision of information on which performance improvement and patient safety decisions are based; and documentation of regular routing to appropriate individuals of current literature relevant to the hospital's quality indicators, top diagnoses, performance improvement projects, patient safety, identified problem areas, or any combination of these
Patient education: active membership of the librarian on the patient education team(s), as reflected in minutes or other documentation (preferred); consultation with the team concerning selection, creation, and quality filtering of sources for patient-education materials; provision of, or facilitation of access to, patient-education materials for clinical staff; provision and marketing of library services directly to patients and families; and teaching of search skills for patient-education electronic resources
Education of hospital and medical staff: active membership of the librarian on the team(s) directing educational functions, as reflected in minutes or other documentation; regular provision of material in support of planning and preparing educational activities; education of hospital and medical staff on information management and use of information technology; identification of print and electronic resources for further individualized learning on topics presented in educational sessions; joint library and continuing medical education (CME) committee(s); inclusion of librarian on CME/graduate medical education (GME) committee(s); provision of case-specific literature in support of grand rounds and related activities; and provision of access to quality alternatives to traditional CME, such as Web-based CME resources, teleconferencing, and other technology
STANDARD 6
The librarian provides evidence of an ongoing assessment of the KBI needs of the organization and the development and implementation of a plan to provide appropriate resources, services, and technology to meet those identified needs.
Intent
The librarian uses a variety of tools and techniques, both formal and informal, to assess the KBI needs of the hospital and medical staff. The needs assessment should address the timeliness of information services and document delivery. In response, resources and services are made available to meet those identified needs. Techniques may include, but are not limited to: focus groups, surveys, analysis of usage patterns, budget and strategic planning, inventory of collections, and one-on-one conversations with health care leaders regarding clinical and organizational information needs.
Tools to be used include recognized guidelines, standards, lists of recommended resources, and benchmarking resources appropriate to the size and scope of the organization. Examples include MLA's benchmarking survey, the “Brandon/Hill Selected List of Print Books and Journals for the Small Medical Library,” and other recognized resource guides for health sciences specialties.
STANDARD 7
The library actively promotes KBI services and resources to all user groups and provides evidence thereof.
Intent
Promotion increases the users' awareness and efficient use of the available services and resources. The library serves not only clinical staff, but other groups within the hospital, including:
residents and interns in medical and other programs
nursing staff
administrative and managerial staff
research staff
allied health staff
staff in offsite locations
students in affiliated programs
patients and their families
other groups as applicable
Promotion of services may take the form of:
announcements to hospital and medical staff of new services, resources, or offerings
inclusion of library services and resources in orientation of interns and residents, if applicable, and new medical and hospital staff members
activities in observance of National Library Week or National Medical Librarians Month
bibliographies on special topics
participation in information fairs or authors' day celebrations
promotion of existing current awareness services or proactive provision of these services
plans for reaching library nonusers
participation in new employee orientations
presentations to groups on what the library can offer them
STANDARD 8
All KBI functions are performed in compliance with applicable federal, state, and local laws and regulations.
STANDARD 9
KBI resources are available to clinical staff twenty-four hours a day, seven days a week.
Intent
Because clinical decisions are often made outside normal working hours, access to knowledge-based information must be continuously available. This access may take multiple forms, depending on the size and complexity of the institution. A broad selection of resources may be made available on the hospital's intranet, or through other electronic means, if connectivity is reliable and users are educated in the effective use of those resources. A physical library may be also made accessible to clinical staff during off hours by means of keys, entry by badge readers, request for entry through security staff, or similar arrangements.
STANDARD 10
The physical library will be large enough to accommodate the library staff, the inhouse collection, an appropriate amount and selection of personal computers or other information technology hardware, and seating for an appropriate number of users. A separate office will be provided for at least the professional library staff.
Intent
A library that cannot comfortably accommodate its staff, users, equipment, and collection is likely to be underutilized. Separate areas for staff enable privacy of communication among library staff and with persons requesting information.
APPENDIX A
Library systems
Several ways a hospital system may provide knowledge-based information (KBI) services and resources for its affiliates are:
Each affiliate hospital may maintain a separate library.
Services and resources may be provided from a central location.
Support staff may be present at each location, with professional services provided centrally.
Support staff may be present at each location, with a circuit librarian arrangement.
A hybrid system, in which arrangements differ among affiliates, may be used.
Coordinated resource sharing among the libraries may be used.
A substantial network of electronic resources available to all affiliates may exist.
These standards do not attempt to dictate a single manner in which services must be provided throughout a system. Rather, they provide a standard for the amount and nature of services and staffing that must be available for the system as a whole.
Depending on a host of factors, including physical proximity of the affiliates and the extent of electronic access to resources, the librarian and health system administrators will collaborate in decision making about centralization or decentralization of library resources and services and the extent of staffing in the libraries. The committee strongly recommends that there be at least support staffing in each location, so that users may obtain assistance in finding needed information, and the smooth flow of operations may be ensured. The amount of staffing—both professional and support level—throughout the system must be at least at the level specified in the library staffing formula, taking all components of the health care system into account. Whether each hospital is treated separately in determining staffing levels, or the system is taken as a whole, is left to the judgment of the librarian and administrators. The important point is that staffing is sufficient to serve the number of users.
If a decision is made to maintain and staff libraries at multiple locations, a level of staffing above that specified in the library staffing formula will be necessary,
to the extent that tasks will be duplicated; and
to the extent that the time of the staff will be used to travel among institutions.
Each separate library location should have convenient, reliable access to a quality core collection of KBI resources, tailored to the needs of the institution. Whether this collection is provided as an inhouse print collection or a reliable electronic collection is a decision that may be made locally. An arrangement whereby core materials are physically housed in a central location and transmitted to other locations on demand, by fax or other means, is not an option, as such arrangements preclude access to information needed for patient care during hours when the library is not staffed. This option may, however, be viable for materials over and above the core collection.
APPENDIX B
Hospital library consultants 2002
Role statement for hospital library consultants
The hospital library consultant serves as advisor to the hospital administration, medical staff, library staff, library committee, or any combination thereof in defining and designing hospital library services and facilities to meet the informational, educational, research, and patient care–related needs of the entire hospital community including, where appropriate, the instructional needs of patients. Consultation is provided on a contractual basis. Hiring a hospital library consultant is not a substitute for the employment of permanent library personnel.
Qualifications for hospital library consultants
A hospital library consultant must have a master's degree in library or information science from a program that is accredited by the American Library Association or its successor accrediting organization or from a master's level program in library and information studies accredited or recognized by the appropriate national body of another country. The consultant should be a member of the Medical Library Association and its Academy of Health Information Professionals. Membership in local, state, regional, or other national professional library associations is desirable. The consultant should have at least three years of administrative hospital library experience.
If the consultant does not have all of the above qualifications, the consultant should have an equivalent combination of training and experience, such as eight years of progressively responsible health sciences library experience including at least five years of hospital library management, administration of a medical center library, or work with hospital libraries in a consultative capacity.
The consultant should have supervisory and administrative experience with the ability to provide assistance on personnel and fiscal issues. The hospital library consultant must show evidence of regular participation in continuing education courses in consulting, management, health sciences, or hospital librarianship such as those sponsored by the Medical Library Association or other professional associations.
The consultant must be familiar with existing national, state, and local library networks and have a working knowledge of the functions of the National Network of Libraries of Medicine. The consultant should also have a thorough working knowledge of the Joint Commission on Accreditation of Healthcare Organizations' (JCAHO) Information Management standards and other hospital library–related standards.
Note: Hospital library consultants for certain types of facilities such as federal or psychiatric hospitals may require additional qualifications.
Functions and process for hospital library consultants
1. identify objectives with the hospital administrator, library staff, or library committee or a combination thereof and other appropriate hospital personnel
2. negotiate a contractual agreement with the hospital administrator that would include:
consultant and client responsibilities
purpose of consultation
period of contract
number and frequency of visits or amount of time to be spent by consultant during the contractual period
verbal and written reporting mechanisms
fee for service
terms of termination by either party
3. conduct a needs assessment for library services profiling all disciplines in the total hospital environment; functional elements identified may include:
placement of library staff within the hospital organizational structure
job descriptions for library staff
library staff recruitment, training, and development
budget
facility planning and space allocation
policies and procedures
availability of current materials for each discipline at the hospital
acquisition, cataloging, arrangement, organization, and evaluation of library materials in any format
negotiation of licensing agreements with vendors of electronic resources
answering of reference questions, performance of searches of KBI resources, and provision of other information
circulation or control of materials
notification of hospital staff of new information in their areas of interest
audiovisual services
provision of patient education materials
promotion of library services
cooperation with other libraries
4. provide specific written recommendations for administrator, library manager, library committee, or a combination thereof
5. develop a methodology for implementation of recommendations by hospital employee(s) assigned to the library
6. evaluate and assess progress regularly during the contractual period
Recommendations for the documentation of consultative visits
The hospital library consultant shall document each visit. At minimum, such documentation should include:
a record of the date and length of each visit
an account of the consultant's activities during each visit
recommendations for action based on the needs assessment
progress reports
suggestions for follow-up
A record of documented visits shall be maintained on file for reviews by the appropriate reviewing or surveying agencies and for continued reference by the administration, library staff, library committee, or a combination thereof. Meetings with the administrator, library manager, and library committee to discuss recommendations, questions, or concerns should be held as needed and followed by a formal written report.
APPENDIX C
Glossary
AHIP: The Academy of Health Information Professionals, which is the Medical Library Association's peer-reviewed professional development and career recognition program.
Circuit librarian: A librarian who is employed by two or more institutions and splits time among different physical locations according to a predetermined schedule.
Clinical librarian: A librarian who attends rounds with a health care team and provides case-specific information to assist with patient care.
Consumer health services: An umbrella term encompassing the continuum extending from the specific information needs of patients to the broader provision of health information for lay people.
Continuing medical education (CME): Educational opportunities designed to enable physicians to remain up-to-date with the knowledge and skills they need to provide their patients with optimum care. CME programs are accredited by the Accreditation Council for Continuing Medical Education (ACCME); by intrastate sponsors, which are in turn accredited by the ACCME; or by the Council on Continuing Medical Education (CCME) of the American Osteopathic Association.
Core collection: Those comprehensive, authoritative print or electronic works to which users refer most often. The core collection should be tailored to the needs of a particular institution and can be expected to contain information pertinent to the majority of reference queries. It may be supplemented by other resources.
Current awareness services: Services designed to keep users up-to-date on new developments and resources in their field of interest.
Health care system: Formal affiliation of two or more health care institutions under unified management.
Information management team: The staff directing the information management functions of the hospital or health care system.
Intranet: An Internet site intended for the internal use of an institution. It is usually protected from outside access by a firewall or other security means. It is distinguished from Internet sites intended for the use of vendors, customers, or others outside the institution.
Knowledge-based Information (KBI): KBI consists of systems, resources, and services to help health professionals acquire the knowledge and skills needed to maintain and improve competence; support clinical, managerial, and business decision making; support performance improvement and activities to reduce risk to patients; provide needed information and education to patients and families; and satisfy research-related needs.
Library consultant: A hospital library consultant serves as advisor to the hospital administration, medical staff, library staff, or library committee in defining and designing hospital library services and facilities to meet the informational, educational, research, and patient care–related needs of the entire hospital community.
Library systems: One or more libraries that together provide coordinated services and resources for a health care system or two or more libraries that together provide coordinated services for a single hospital.
License agreement: A written contract setting forth the terms under which a licensor grants a license to a licensee. The licensee, often a library or educational or research organization, generally pays the licensor a fee for permission to use digital information.
Mediated searches: Searches of the literature performed by a librarian on behalf of a library user.
MLA: Medical Library Association.
MLS: Master's degree in library science. In some institutions, the degree awarded may actually be master of science in library science, master of arts in library science, master of library and information science, etc. These are equivalent.
Needs assessment: A systematic process designed to determine the need for specific services or types of information by the library's user group. This may take the form of surveys, focus groups, interviews of groups or individuals, or other methods.
Patient education: The provision of information to help inpatients or outpatients, or their family members, understand and cope with the condition for which they are receiving medical care. This education assists patients and their families in taking an active role in health care decision making.
Performance improvement: The continuous study and adaptation of a health care organization's functions and processes to increase the probability of achieving desired outcomes and to better meet the needs of individuals and other users of services.
Qualified librarian: A person who has earned a master's degree from a program accredited by the American Library Association or its successor accrediting organization or from a master's level program in library and information studies accredited or recognized by the appropriate national body of another country.
Quality filtering: The determination of the appropriateness of specific information for a given purpose, taking into account factors such as research methodology, level of writing, intended audience, qualifications and affiliations of author, currency, etc.
Technical employee: The hospital employee(s) assigned to the library, performing the day-to-day library-related work, under the guidance of a hospital library consultant.
APPENDIX D
Bibliography
Hill DR, Stickell HN. Brandon/Hill selected list of print books and journals for the small medical library. Bull Med Libr Assoc 2001 Apr;89(2):131–53. (updated biennially.)
Holst R, Philips SA, eds. The Medical Library Association guide to managing health care libraries. New York, NY: Neal-Schuman, 2000.
Joint Commission on Accreditation of Healthcare Organizations. CAMH: comprehensive accreditation manual for hospitals: the official handbook. Oakbrook Terrace, IL: JCAHO, 2002.
Klein MS, Ross FV, Adams DL, Gilbert CM. Effect of online literature searching on length of stay and patient care costs. Acad Med 1994 Jun;69(6):489–95.
Medical Library Association. Academy of Health Information Professionals. [Web document]. Chicago, IL: The Association. [rev 15 Jan 2002; cited 4 Mar 2002]. <http://www.mlanet.org/academy/>.
Special Committee on Competencies for Special Librarians, Special Libraries Association. Competencies for special librarians of the 21st century. [Web document]. Washington, DC: The Association, 1996. [rev 3 May 2001; cited 4 Mar 2002]. <http://www.sla.org/content/SLA/professional/meaning/competency.cfm>.
Stanley EH. Competencies for hospital librarians. National Network 2000 Apr;24(4):12–3,20.
Wellik KE, Jarvis MJ, Schardt C. Accreditation and the hospital library: information management plans and assessment tools. Chicago, IL: Medical Library Association, 1997. (MLA DocKit #10.)
Contributor Information
Jeannine Cyr Gluck, Email: jgluck@mmhosp.chime.org.
Robin Ackley Hassig, Email: robin.hassig@danhosp.org.
Leeni Balogh, Email: leeni.balogh@kp.org.
Margaret Bandy, Email: bandym@exempla.org.
Jacqueline Donaldson Doyle, Email: jacque.doyle@bannerhealth.com.
Michael R. Kronenfeld, Email: mkronenfeld@ashs.edu.
Katherine Lois Lindner, Email: kathy.lindner@ehmc.com.
Kathleen Murray, Email: afktm@uaa.alaska.edu.
JoAn Petersen, Email: jpetersen@sbhcs.com.
Debra C. Rand, Email: rand@lij.edu.