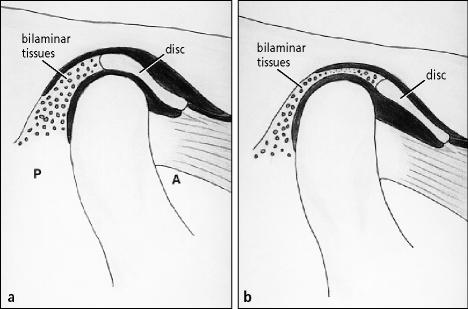
The temporomandibular joint (TMJ) is a bilateral diarthrodial joint of the jaws in the human skeleton. This unique joint can perform both hinge and sliding functions and is the only synovial joint in humans whose articulating surfaces are covered by fibrocartilage. The joint is formed by the bony articulations of the mandibular condyle and the temporal bone (glenoid fossa and articular eminence). Interposed between the condyle and the fossa is a piece of dense, avascular fibrous connective tissue, the TMJ articular disc. This disc divides the joint into superior and inferior joint compartments, which normally do not communicate with each other. The disc and condyle are in a normal anatomic relationship if the posterior band of the disc is located above the condylar head when the mandibular condyle is centrically positioned in the fossa (Figure 1a). The disc is attached to the condylar neck by ligamentous soft tissue attachments. The joint is circumferentially surrounded by a fibrous capsule and has multiple ligamentous attachments that provide stability, especially in a lateral direction.
Figure 1.
(a) Normal temporomandibular joint anatomy with a harmonious disc-condyle relationship. A indicates anterior; P, posterior. (b) The disc is anteriorly displaced, with the bilaminar tissues interposed between the condyle and fossa.
TMJ dysfunction is a relatively common condition: an estimated 12% to 87% of the US population has at least 1 sign of TMJ dysfunction (1, 2). TMJ dysfunction occurs more frequently in women than men (8:1 ratio). The most common cause of TMJ dysfunction is anterior and/or medial displacement of the articular disc (also known as internal derangement of the TMJ) (Figure 1b). Displacement of the TMJ articular disc can result in decreased joint space; clicking, popping, or crepitation during jaw function; arthritis; condylar resorption; jaw deformities; malocclusion; inflammation; and compression of the bilaminar tissue— all of which can cause various degrees of pain and dysfunction (3). Chronic disc displacement can lead to deformation of the disc, loss of flexibility, vascularization of the disc (a normal disc is avascular), and breakdown of the fibrocartilage covering the condyle and fossa. The disc or, more commonly, the bilaminar tissue posterior to the disc, can perforate, and intracapsular adhesions can develop. These changes can lead to progressive worsening of jaw function and pain. Some common clinical symptoms of TMJ dysfunction include TMJ sounds/noises, TMJ pain, facial pain, headaches, limited range of mandibular movement, change in occlusion, masticatory difficulty, earaches, tinnitus, vertigo, and neck, shoulder, and back pain. Some patients with pathological internal derangement of the TMJ, however, are asymptomatic or have relatively innocuous clinical symptoms.
Previously reported clinical results of surgical TMJ discrepositioning procedures have been variable, with failures related to a lack of long-term stability, indicating a need for improved methods of disc stabilization (4, 5). Disc displacement is often accompanied by a loss of structural integrity of the posterior, medial, and lateral supporting ligaments. Traditional disc-repositioning techniques involve suturing (plication) of these inflamed and often degenerated ligaments, contributing to the instability of the disc after surgery. To overcome this problem, Wolford et al (6) developed a surgical technique that uses a bone anchor (Mitek mini anchor, Mitek Products Inc., Westwood, Mass) to stabilize the TMJ articular disc. This article presents some of the clinical and research experience at Baylor University Medical Center and Baylor College of Dentistry with the use of the Mitek anchor in TMJ articular disc-repositioning surgery.
REVIEW OF PUBLISHED REPORTS
Although Annandale first described surgical repositioning of the displaced temporomandibular articular disc in 1887 (7), it was not until 1978, when Wilkes used arthrography to describe the anatomy, form, and function of the TMJ, that disc repositioning became an accepted surgical technique (3, 8). Wilkes theorized that there was a “very high probability that the signs and symptoms of the temporomandibular joint pain-dysfunction syndrome are direct manifestations of internal derangement of the joint (articular disc displacement).” Before that time, routine recommended treatment for TMJ internal derangement was either to do nothing or to remove the disc (diskectomy). In 1979, McCarty et al reported a 94% success rate for disc-repositioning surgery; their technique involved removing 3 to 4 mm of the posterosuperior condylar surface and a posterior wedge resection (2 mm) of the bilaminar zone with suture reapproximation (9). Other surgeons, however, did not experience similar success with this technique, and this led to development of numerous new and modified techniques for disc-repositioning surgery, which had varying degrees of success (5, 6, 10–18). Some authors have proposed arthroscopic suturing techniques to reposition the disc (19, 20). However, the reliability of an arthroscopic approach for predictably repositioning and stabilizing the TMJ disc has not been documented.
THE MITEK MINI ANCHOR
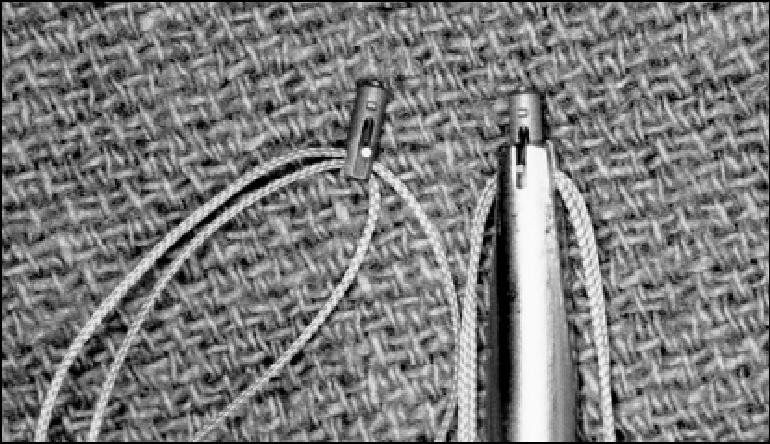
Mitek anchors were originally developed for use in orthopaedic surgery procedures, such as rotator cuff repair, medial and lateral collateral ligament repair, biceps tendon reattachment, and other muscle, ligament, and tendon repairs (21, 22). Although the anchors are available in various sizes, the Mitek mini anchor (Figure 2) is the most adaptable for TMJ disc stabilization. The successful use of the device for TMJ articular disc repositioning has been previously reported in the literature by Wolford et al (6, 17, 18, 23).
Figure 2.

The body of the Mitek mini anchor is 1.8 × 5 mm and is composed of titanium alloy, with wings of nickel-titanium alloy.
The Mitek mini anchor is cylindrical, measuring 1.8 mm in diameter and 5.0 mm in length. The body of the anchor is composed of titanium alloy (titanium 90%, aluminum 6%, vanadium 4%), while its wings are composed of a nickel-titanium (Nitinol) alloy that uses superelastic shape memory properties. An eyelet in the posterior aspect of the anchor allows placement of sutures, which can function as artificial ligaments (Figure 3).
Figure 3.
Two 0-Ethibond sutures passed through the eyelet of the Mitek mini anchor on the left will function as artificial ligaments to stabilize the disc in the proper position. The anchor on the right has been loaded on an inserting device, which is used to place the anchor in the condyle.
SURGICAL TECHNIQUE
A modified short endaural incision is used by the authors to gain access to the TMJ area. The superior and inferior joint spaces are entered, and the disc is identified and mobilized. The anterior, lateral, and sometimes the medial ligamentous attachments are freed, if indicated, to permit passive repositioning of the articular disc over the condylar head. If necessary, discoplasty, arthroplasty, and/or eminoplasty are performed to optimize the fit of the disc, condyle, and fossa. Arthroplasty and eminoplasty are avoided if possible, since these procedures can create postsurgical adhesions of the disc to the fossa and/or condyle, contributing to decreased joint mobility, degenerative joint disease, and, possibly, continued pain.
A 2 × 10 mm hole is made in the posterior head of the condyle, 8 to 10 mm below the top of the condyle and just lateral to the midsagittal plane, by using a standard Mitek drill bit (Figure 4). The Mitek anchor, with 2 0-Ethibond braided polyester sutures (Ethicon, Inc., Somerville, NJ) threaded through its eyelet, is then placed into the prepared hole by using an inserter device. The nickel-titanium wings, which possess superelastic properties, are pressed against the body of the anchor as they pass through the more dense cortical bone and are reopened when they enter the softer medullary bone (Figure 4a). This effectively locks the anchor into place within the condylar head. The 2 Ethibond sutures are then secured to the disc in a horizontal mattress fashion. One suture is placed through the medial aspect of the posterior band of the disc, and the other is placed through the lateral aspect of the posterior band (Figure 4b). The remaining bilaminar tissues, capsule, subcutaneous tissue, and skin are then closed in a routine manner. Any orthognathic (jaw) surgical procedures indicated to maintain the original occlusion or to correct a coexisting dentofacial deformity are then performed. Postsurgical physical therapy may be indicated at the discretion of the surgeon. Postsurgical imaging demonstrates the presence of the Mitek anchor in the condylar head (Figure 5).
Figure 4.
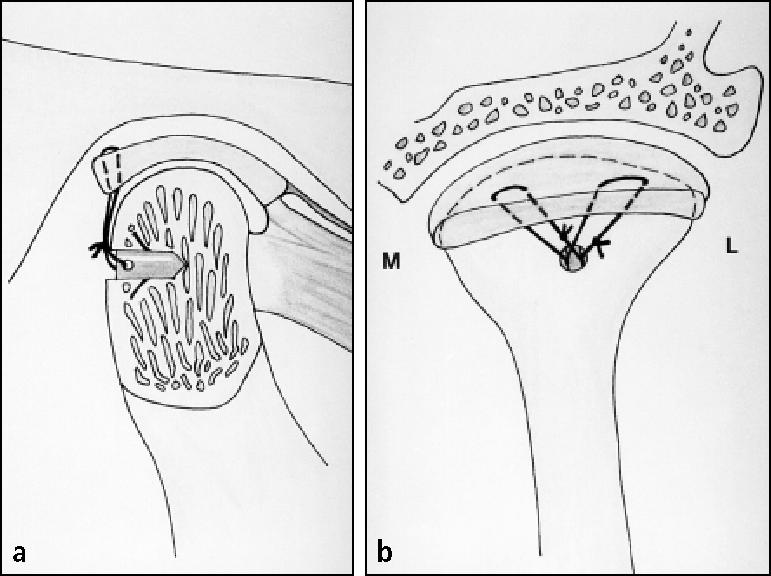
(a) The cross-section of the condyle illustrates the Mitek anchor positioned beneath the posterior cortical bone, with the wings expanded, locking it in position. Usually, the anchor is inserted 8 to 10 mm below the condylar head and just lateral to the midsagittal plane. (b) A posterior view of the condyle shows the artificial ligaments (0-Ethibond sutures) secured to the posterior band of the repositioned articular disc. Two sutures (one posteromedial and the other posterolateral) are passed from the anchor to the disc in horizontal mattress fashion to stabilize the repositioned disc. M indicates medial; L, lateral.
Figure 5.
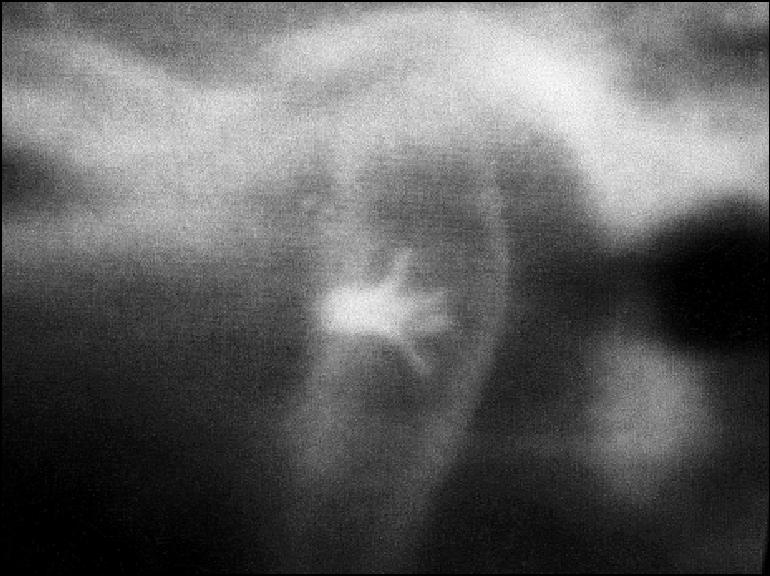
A postsurgical tomogram showing the position of the anchor within the condylar head.
EXPERIENCE AT BAYLOR UNIVERSITY MEDICAL CENTER
The senior author (LMW) has used the Mitek anchor for TMJ articular disc repositioning since 1992 with good results. Laboratory and clinical research studies conducted at Baylor University Medical Center and Baylor College of Dentistry led to Food and Drug Administration approval of the Mitek mini anchor specifically for use in TMJ surgery in 1999 (6, 17, 23– 26).
Laboratory research
Fields, Cardenas, and Wolford evaluated the pullout strength of 20 Mitek mini anchors placed in human cadaver condyles (24). Pullout thresholds were reached when the cortical bone overlying the anchor gave way (18 condyles) or when the suture broke (2 condyles). There was no breakage, deformation, or failure of the anchors. The pullout strength averaged 16.02 lbs (range, 8.5 to 28.4 lbs), which appears to be adequate to stabilize the anchor during osseointegration. Fields, Franco, and Wolford also demonstrated that osseointegration of the Mitek mini anchors predictably occurs in human mandibular condyles (25).
Clinical research
Wolford and coworkers have published their clinical results after disc-repositioning surgery using the Mitek anchor (6, 17, 23). Criteria for success in TMJ surgery include skeletal and occlusal stability, significant decreases in TMJ and myofascial pain, and a jaw opening of >35 mm. Wolford et al reported a success rate of 91% in a group of 43 patients (78 joints) with an average postsurgical follow-up duration of 2½ years (23). Cardenas, Wolford, and Goncalves studied 66 Mitek anchors after placement in the TMJ for vertical and horizontal positional changes based on standardized lateral cephalometric tomograms and found excellent stability of the Mitek anchors within condylar bone, with statistically insignificant minor positional changes (–0.01 mm with a range of –1.5 to 1.5 mm) long term (26).
We recently performed a retrospective study evaluating 105 patients (89 women and 16 men) who underwent TMJ disc repositioning (27). Criteria for inclusion in the study were as follows: 1) presurgical TMJ disc displacement based on magnetic resonance imaging (MRI) and clinical examination; 2) no prior TMJ surgery; 3) salvageable articular disc; 4) surgery for TMJ disc repositioning and stabilization with the Mitek mini anchor; 5) absence of known connective tissue/autoimmune disease; 6) absence of postsurgical trauma; and 7) a minimum of 12 months postsurgical follow-up. Clinical and radiographic evaluations were done before surgery (T1), immediately after surgery (T2), and at last follow-up (T3). Clinical evaluations were performed by 1 clinician and included both an objective evaluation of maximal incisal opening, lateral excursions, and TMJ noises and a subjective evaluation using visual analog scales for TMJ pain, facial pain, and headaches (0 = no pain, 10 = worst pain); jaw function (0 = normal, 10 = no function); diet (0 = no restriction, 10 = liquids only); and disability (0 = no disability, 10 = total disability). Acetate tracings of standardized lateral cephalometric tomograms taken at T2 and T3 were superimposed to evaluate anchor stability and assess for condylar resorption. Student t test was used for statistical analysis of results, and a P value <0.01 was considered to be statistically significant. An asterisk (*) denotes statistically significant findings.
Mean patient age at the time of surgery was 33 years, and the mean postsurgical follow-up period was 46 months. A total of 188 disc-repositioning procedures were performed on the 105 patients. Simultaneous orthognathic surgery was performed in 88 patients (83.8%) for correction of coexisting dentofacial deformities. Mean visual analog scale scores for the parameters assessed were as follows: TMJ pain* = 5.2 (T1) and 1.6 (T3); facial pain/ headache* = 7.2 (T1) and 2.4 (T3); jaw function* = 3.8 (T1) and 1.9 (T3); diet* = 3.8 (T1) and 1.7 (T3); and disability* = 3.6 (T1) and 1.1 (T3). Eighty-eight patients (83.8%) had TMJ noises before surgery, and 6 patients (5.7%) had TMJ noises at last follow-up. Mean maximum interincisal opening measurements were 42.8 (T1) and 43.7 (T3). Mean lateral excursion values were as follows: left, 5.3 mm (T1) and 5.1 mm (T3); right, 5.1 mm (T1) and 5 mm (T3). Fifty-eight patients (55%) reported severe TMJ pain before surgery, while only 4 patients (3.8%) reported severe pain at T3. Seventy-eight patients (74%) had complete absence of TMJ pain at T3, whereas only 19 patients (18%) had no TMJ pain at T1. Only 2 patients (1.9%) had a jaw opening of <35 mm at T3. In no patient did TMJ pain or interincisal opening get worse after surgery. Radiographic examination at T3 demonstrated no significant condylar resorption or positional changes in the anchors.
DISCUSSION
TMJ dysfunction is a relatively common condition, with a 12% to 87% reported incidence in the population (1). Clinical symptoms of TMJ dysfunction can mimic many other medical disease processes, as patients can present with 1 or more of the following symptoms: TMJ pain; headaches; myofascial pain; neck, shoulder, and back pain; decreased jaw function; clicking or popping of the jaw joint(s); earaches; tinnitus; and vertigo. It is recommended that patients with such symptoms be screened for TMJ pathology along with other appropriate medical diagnostic tests. Clinical and radiographic examination are essential parts of the initial screening appointment for patients with possible TMJ dysfunction. Specialized imaging techniques, including MRI, computed tomographic scans, and tomograms of the TMJ, may be required to confirm clinically suspected TMJ articular disc displacement or other TMJ pathology.
Factors that can predispose to or cause TMJ disc displacement and dysfunction include trauma, parafunctional habits, gender, malocclusion, hormones, bacterial and viral infections, and systemic or local disease. Discs become displaced because of rupture, tearing, herniation, stretching, or degeneration of the ligaments that normally support the disc in position. Any of these conditions can create significant loss of integrity to the supportive ligaments of the disc, rendering the ligaments unsuitable for disc stabilization. Functional loading of the joint following attempted ligament repair may cause subsequent failure of the procedure and recurrent displacement of the disc with continued degeneration within the joint. Thus, the concept of using a bone anchor and artificial ligaments for disc stabilization seems attractive, as it does not depend on the structural integrity of soft tissues for maintaining postsurgical disc stabilization.
Osseointegration of the Mitek anchor to the human condylar bone is a unique feature, as it ensures stability of the anchor after placement in the TMJ. Fields et al showed that osseointegration of the Mitek anchor was noted as early as 3 months after placement in the TMJ, despite probable intermittent application of low-magnitude forces to the anchor (25). While the magnitude of functional loading in a healthy TMJ is a subject of considerable debate, the force applied to a newly placed Mitek mini anchor in the mandibular condyle is difficult to estimate in terms of both magnitude and vector. Our present technique involves placing a pair of number 0 Ethibond sutures through the anchor eyelet for 2-point stabilization of the articular disc. One suture is placed through the posteromedial aspect of the articular disc, while the second suture is placed more laterally (Figure 4).
Wolford et al found that the length of time from the onset of TMJ symptoms to the performance of the disc-repositioning surgery had a significant influence on the success of the procedure (17, 18). They found that surgeries performed within 4 years of the onset of symptoms had a success rate in the 90th percentile range; after 4 years following the onset of TMJ symptoms, the success rate dropped significantly, to approximately 68%. These results support the concept that early identification of disc displacement and prompt surgical repositioning may stop further progression of osteoarthritis and disc degeneration, provided there are no other predisposing factors such as connective tissue or autoimmune diseases or infective agents affecting the joints.
Most patients with displaced articular discs will have decreased joint space between the condyle and fossa. In addition, once discs get displaced, they tend to shorten in length and become thicker with time. In patients with normal occlusions, repositioning such deformed discs will usually shift the mandible and chin in a downward and forward direction, resulting in a malocclusion. Surgical repositioning of the mandible with sagittal split ramus osteotomies will maintain the original occlusion and create space within the joint to accommodate the disc. In patients with coexisting jaw or facial deformities, we prefer to reposition the displaced discs and correct the jaw or facial deformities at the same operation because a simultaneous procedure 1) exposes patients to only 1 general anesthetic and surgery; 2) balances jaw structures, occlusion, TMJ, and muscles at 1 time; and 3) decreases overall treatment time. If the surgeon prefers, the orthognathic surgery can be delayed and performed at a later time, but in that case the occlusion must be carefully controlled so that the TMJs are not overloaded between the surgical stages.
References
- 1.Flynn B, Brown DT, Lapp TH, Bussard DA, Roberts WE. A comparative study of temporomandibular symptoms following mandibular advancement by bilateral sagittal split osteotomies: rigid versus nonrigid fixation. Oral Surg Oral Med Oral Pathol. 1990;70:372–380. doi: 10.1016/0030-4220(90)90163-m. [DOI] [PubMed] [Google Scholar]
- 2.Gross A, Gale EN. A prevalence study of the clinical signs associated with mandibular dysfunction. J Am Dent Assoc. 1983;107:932–936. doi: 10.14219/jada.archive.1983.0354. [DOI] [PubMed] [Google Scholar]
- 3.Wilkes CH. Structural and functional alterations of the temporomandibular joint. Northwest Dent. 1978;57:287–294. [PubMed] [Google Scholar]
- 4.Mercuri LG, Biery K, Quigg R. Surgical management of temporomandibular joint pathology. A therapeutic follow-up study. Proceedings of the Ninth International Conference in Oral and Maxillofacial Surgery, Vancouver, BC, Canada, May 1986.
- 5.Kerstens HC, Tuinzing DB, van der Kwast WA. Eminectomy and discoplasty for correction of the displaced temporomandibular joint disc. J Oral Maxillofac Surg. 1989;47:150–154. doi: 10.1016/s0278-2391(89)80106-5. [DOI] [PubMed] [Google Scholar]
- 6.Cottrell DA, Wolford LM. The Mitek mini anchor in maxillofacial surgery. J Oral Maxillofac Surg Educational Summaries and Outlines. 1993;57(3):150. [Google Scholar]
- 7.Annandale T. On displacement of the interarticular cartilage of the lower jaw and its treatment by operation. Lancet. 1887;1:411–412. [Google Scholar]
- 8.Wilkes CH. Arthrography of the temporomandibular joint in patients with the TMJ pain-dysfunction syndrome. Minn Med. 1978;61:645–652. [PubMed] [Google Scholar]
- 9.McCarty WL, Farrar WB. Surgery for internal derangements of the temporomandibular joint. J Prosthet Dent. 1979;42:191–196. doi: 10.1016/0022-3913(79)90174-4. [DOI] [PubMed] [Google Scholar]
- 10.Leopard PJ. Anterior dislocation of the temporomandibular disc. Br J Oral Maxillofac Surg. 1984;22:9–17. doi: 10.1016/0266-4356(84)90002-0. [DOI] [PubMed] [Google Scholar]
- 11.Walker RV, Kalamchi S. A surgical technique for management of internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 1987;45:299–305. doi: 10.1016/0278-2391(87)90347-8. [DOI] [PubMed] [Google Scholar]
- 12.Weinberg S, Cousens G. Meniscocondylar plication: a modified operation for surgical repositioning of the ectopic temporomandibular joint meniscus. Rationale and operative technique. Oral Surg Oral Med Oral Pathol. 1987;63:393–402. doi: 10.1016/0030-4220(87)90247-7. [DOI] [PubMed] [Google Scholar]
- 13.Mercuri LG, Campbell RL, Shamaskin RG. Intra-articular meniscus dysfunction surgery. A preliminary report. Oral Surg Oral Med Oral Pathol. 1982;54:613–621. doi: 10.1016/0030-4220(82)90073-1. [DOI] [PubMed] [Google Scholar]
- 14.Zetz MR, Ash DC. Double-layer closure for temporomandibular joint discoplasty. J Oral Maxillofac Surg. 1990;48:427–429. doi: 10.1016/0278-2391(90)90447-a. [DOI] [PubMed] [Google Scholar]
- 15.Anderson DM, Sinclair PM, McBride KM. A clinical evaluation of temporomandibular joint disk plication surgery. Am J Orthod Dentofacial Orthop. 1991;100:156–162. doi: 10.1016/S0889-5406(05)81522-7. [DOI] [PubMed] [Google Scholar]
- 16.Dolwick MF, Nitzan DW. The role of disc-repositioning surgery for internal derangements of the temporomandibular joint. Oral Maxillofac Surg North Am. 1994;6:271–275. [Google Scholar]
- 17.Wolford LM. Temporomandibular joint devices: treatment factors and outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:143–149. doi: 10.1016/s1079-2104(97)90105-0. [DOI] [PubMed] [Google Scholar]
- 18.Wolford LM, Karras SC. Simultaneous TMJ and orthognathic surgery. J Oral Maxillofac Surg. 1994;52:98. [Google Scholar]
- 19.Hoffman DC, Sansevere JJ. A new method of TMJ disc stabilization during open joint surgery. J Oral Maxillofac Surg. 1993;51:149. [Google Scholar]
- 20.Tarro AW. TMJ arthroscopic diagnosis and surgery: clinical experience with 152 procedures over a 21.2-year period. Cranio. 1991;9:107–119. doi: 10.1080/08869634.1991.11678355. [DOI] [PubMed] [Google Scholar]
- 21.Obrist J, Genelin F, Neureiter H. [Bankart operation with the Mitek anchor system] Unfallchirurgie. 1991;17:208–212. doi: 10.1007/BF02588688. [DOI] [PubMed] [Google Scholar]
- 22.Pederson B, Tesoro D, Wertheimer SJ, Coraci M. Mitek Anchor System: a new technique for tenodesis and ligamentous repair of the foot and ankle. J Foot Surg. 1991;30:48–51. [PubMed] [Google Scholar]
- 23.Wolford LM, Cottrell DA, Karras SC. Proceedings of SMST-94 of the First International Conference on Shape Memory and Superelastic Technologies. Monterrey, Calif: MIAS; 1995. Mitek mini anchor in maxillofacial surgery; pp. 477–492. [Google Scholar]
- 24.Fields RT, Jr, Cardenas LE, Wolford LM. The pullout force for Mitek mini and micro suture anchor systems in human mandibular condyles. J Oral Maxillofac Surg. 1997;55:483–487. doi: 10.1016/s0278-2391(97)90697-2. discussion 487–488. [DOI] [PubMed] [Google Scholar]
- 25.Fields T, Franco PF, Wolford LM. Osseous-integration of the Mitek anchor in the human condyle. J Oral Maxillofac Surg. 1997;55:92. [Google Scholar]
- 26.Cardenas L, Wolford LM, Goncalves J. Mitek anchor in TMJ surgery: positional changes and condylar effects. J Oral Maxillofac Surg. 1997;55:114. [Google Scholar]
- 27.Mehra P, Wolford LM. TMJ disc repositioning using the Mitek mini anchor. Int J Oral Maxillofac Surg. In press. [DOI] [PubMed]