Abstract
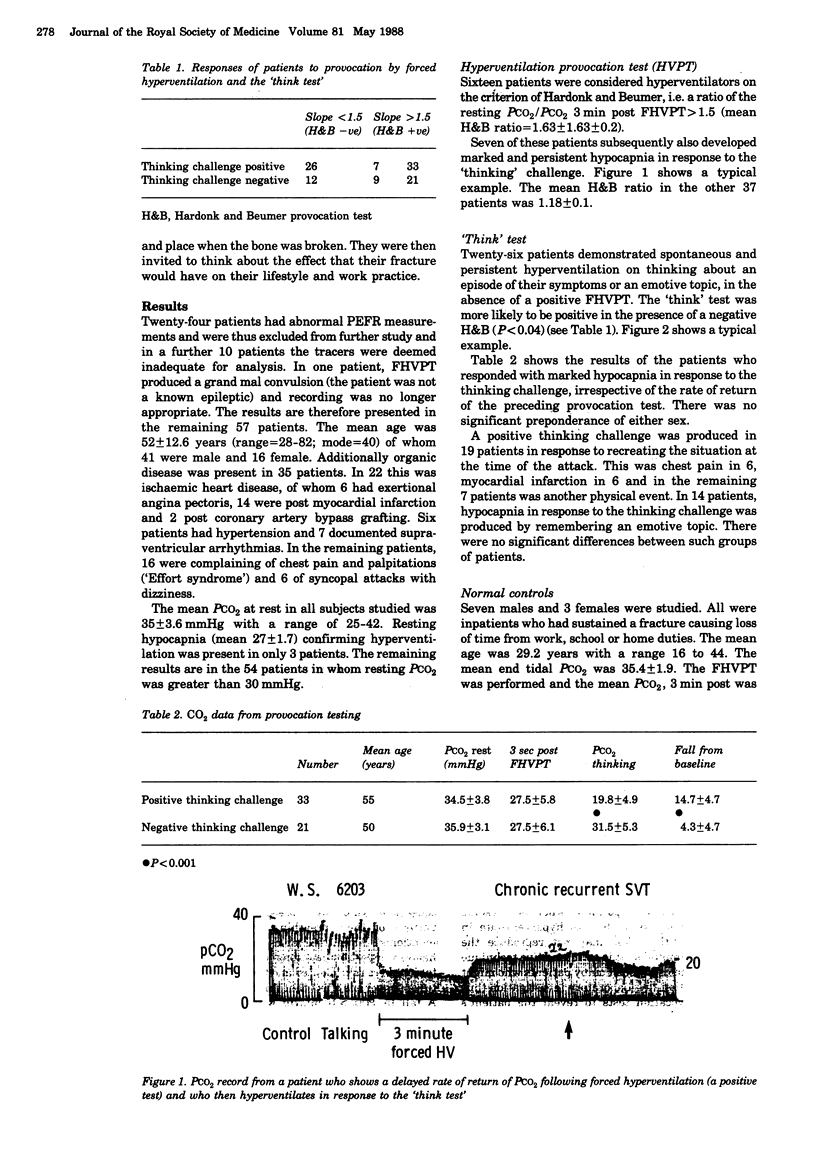
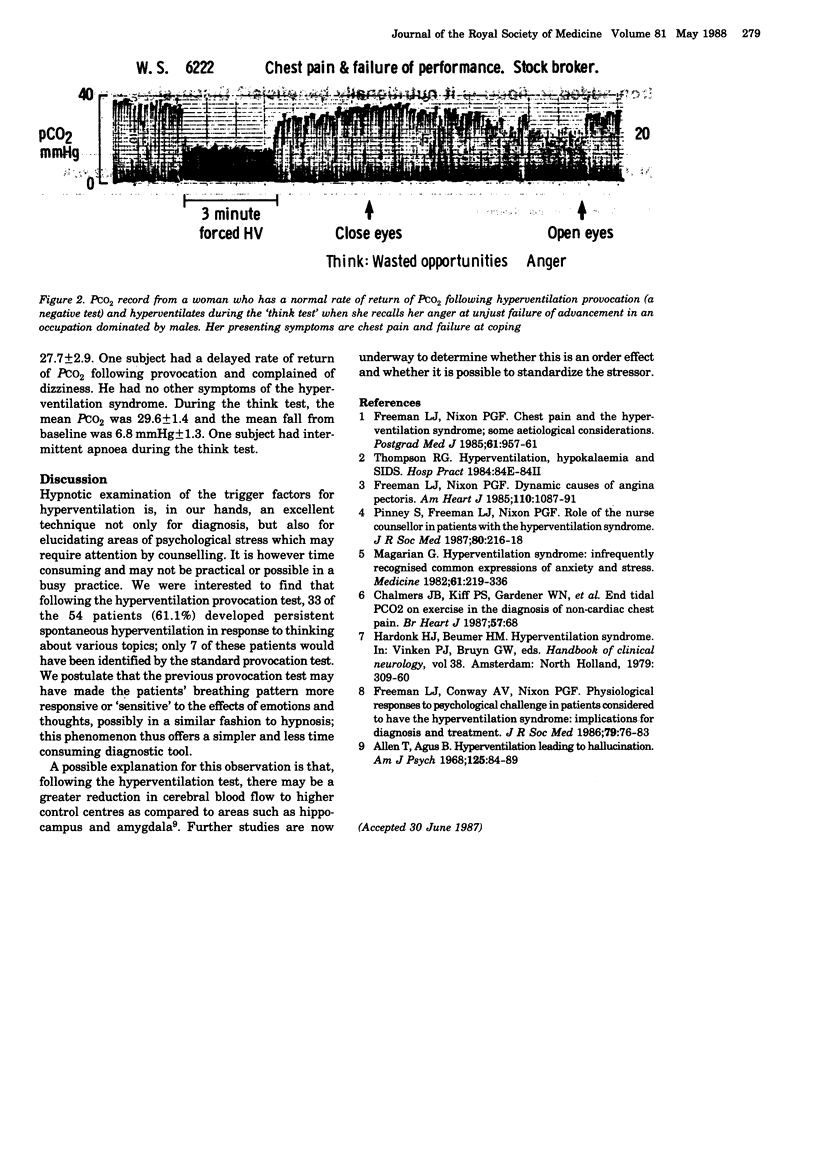
Hyperventilation can undermine cardiovascular homeostasis by generating autonomic imbalance, sympathetic dominance, hypokalaemia, and intracellular alkalosis with calcium ion shifts. The role of hyperventilation in episodic disorders such as arrhythmia and coronary vasospasm can be difficult to identify if the patient does not present in an attack and so a provocation challenge is required. Today, the standard challenge is the forced hyperventilation provocation test (FHPT). A capnograph enables the resting end-tidal PCO2 to be compared with the level 3 min after the period of overbreathing. We report the use of a patient-specific challenge. After the FHPT, the subject is invited to close his eyes and think about the circumstances of an attack, feelings and sensations experienced (breathing is not mentioned) or topics that were seen to disturb the rhythm of breathing when the medical history was taken. A fall of end-tidal PCO2 of 10 mmHg or more lasting at least one minute was taken as a positive response. Out of 57 patients with cardiovascular symptoms suggesting a hypocapnic influence, resting hypocapnia (end-tidal PCO2 = 30 mmHg) was present in 3 (5%). Of the remaining 54, the FHPT was positive in 16 (30%) and the 'think test' in 33 (61%). This suggests that patient-specific stimulation has advantages over an unspecific challenge in testing for episodic hypocapnia.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Freeman L. J., Conway A., Nixon P. G. Physiological responses to psychological challenge under hypnosis in patients considered to have the hyperventilation syndrome: implications for diagnosis and therapy. J R Soc Med. 1986 Feb;79(2):76–83. doi: 10.1177/014107688607900206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman L. J., Nixon P. G. Chest pain and the hyperventilation syndrome--some aetiological considerations. Postgrad Med J. 1985 Nov;61(721):957–961. doi: 10.1136/pgmj.61.721.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman L. J., Nixon P. G. Dynamic causes of angina pectoris. Am Heart J. 1985 Nov;110(5):1087–1092. doi: 10.1016/0002-8703(85)90221-2. [DOI] [PubMed] [Google Scholar]
- Magarian G. J. Hyperventilation syndromes: infrequently recognized common expressions of anxiety and stress. Medicine (Baltimore) 1982 Jul;61(4):219–236. [PubMed] [Google Scholar]
- Pinney S., Freeman L. J., Nixon P. G. Role of the nurse counsellor in managing patients with the hyperventilation syndrome. J R Soc Med. 1987 Apr;80(4):216–218. doi: 10.1177/014107688708000408. [DOI] [PMC free article] [PubMed] [Google Scholar]



