Abstract
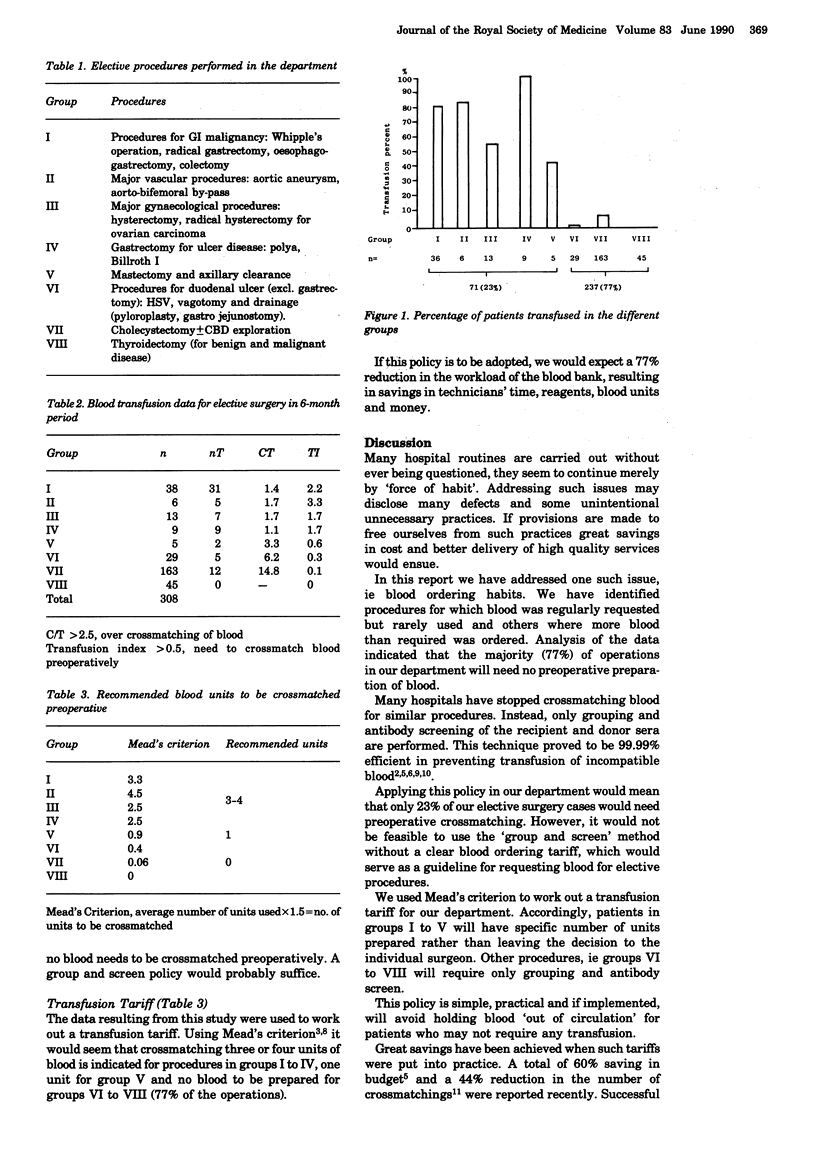
A prospective study was carried out for 6 months to determine the efficacy of blood ordering routines for elective surgery. It was found that only 23% of procedures needed preoperative crossmatching of blood (transfusion index 'TI' greater than 0.5). There was an excessive over-ordering of blood for 77% of the operations (crossmatch/transfusion ratio greater than 2.5). In addition, the transfusion index for the latter group showed that there was no need to prepare blood preoperatively (TI less than 0.5). A transfusion tariff is worked out which abandons crossmatching for the majority of procedures (cholecystectomy, thyroidectomy and surgery for duodenal ulcer excluding gastrectomy). Instead a 'group and screen' policy is suggested.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Argov S., Shechter Y. Is routine crossmatching for two units of blood necessary in elective surgery? Am J Surg. 1981 Sep;142(3):370–371. doi: 10.1016/0002-9610(81)90351-2. [DOI] [PubMed] [Google Scholar]
- Boral L. I., Dannemiller F. J., Stanford W., Hill S. S., Cornell T. A. A guideline for anticipated blood usage during elective surgical procedures. Am J Clin Pathol. 1979 Jun;71(6):680–684. doi: 10.1093/ajcp/71.6.680. [DOI] [PubMed] [Google Scholar]
- Dodsworth H., Dudley H. A. Increased efficiency of transfusion practice in routine surgery using pre-operative antibody screening and selective ordering with an abbreviated crossmatch. Br J Surg. 1985 Feb;72(2):102–104. doi: 10.1002/bjs.1800720210. [DOI] [PubMed] [Google Scholar]
- Friedman B. A. An analysis of surgical blood use in United States hospitals with application to the maximum surgical blood order schedule. Transfusion. 1979 May-Jun;19(3):268–278. doi: 10.1046/j.1537-2995.1979.19379204208.x. [DOI] [PubMed] [Google Scholar]
- Lee K., Lachance V. Type and screen for elective surgery. Results of one year's experience in a small community hospital. Transfusion. 1980 May-Jun;20(3):324–326. doi: 10.1046/j.1537-2995.1980.20380214900.x. [DOI] [PubMed] [Google Scholar]
- Mead J. H., Anthony C. D., Sattler M. Hemotherapy in elective surgery: an incidence report, review of the literature, and alternatives for guideline appraisal. Am J Clin Pathol. 1980 Aug;74(2):223–227. doi: 10.1093/ajcp/74.2.223. [DOI] [PubMed] [Google Scholar]
- Napier J. A., Biffin A. H., Lay D. Efficiency of use of blood for surgery in south and mid Wales. Br Med J (Clin Res Ed) 1985 Sep 21;291(6498):799–801. doi: 10.1136/bmj.291.6498.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathi V. L., Ghosh S., Cuschieri A. It's Scotland's blood, so why waste it? A survey of blood ordering habits in the Tayside Region. J R Coll Surg Edinb. 1987 Apr;32(2):69–71. [PubMed] [Google Scholar]
- Seshadri R. S., Odell W. R., Roxby D., Morley A. A. Effective use of blood in elective surgical procedures. Med J Aust. 1979 Dec 1;2(11):575–578. doi: 10.5694/j.1326-5377.1979.tb127191.x. [DOI] [PubMed] [Google Scholar]
- Smallwood J. A. Use of blood in elective general surgery: an area of wasted resources. Br Med J (Clin Res Ed) 1983 Mar 12;286(6368):868–870. doi: 10.1136/bmj.286.6368.868. [DOI] [PMC free article] [PubMed] [Google Scholar]



