Abstract
Objective: Contemporary health care places enormous health information management demands on laypeople. Insights into their skills and habits complements current developments in consumer health innovations, including personal health records. Using a five-element human factors model of work, health information management in the household (HIMH) is characterized by the tasks completed by individuals within household organizations, using certain tools and technologies in a given physical environment.
Design: We conducted a descriptive-exploratory study of the work of HIMH, involving 49 community-dwelling volunteers from a rural Midwestern community.
Measurements: During in-person interviews, we collected data using semistructured questionnaires and photographs of artifacts used for HIMH.
Results: The work of HIMH is largely the responsibility of a single individual, primarily engaged in the tasks of acquiring, managing, and organizing a diverse set of health information. Paper-based tools are most common, and residents develop strategies for storing information in the household environment aligned with anticipated use. Affiliative relationships, e.g., parent-child or spousal, within the household serve as the organization that gives rise to health information management practices. Synthesis of these findings led to identification of several storage strategies employed in HIMH. These strategies are labeled “just-in-time,” “just-because,” “just-in-case,” and “just-at-hand,” reflecting location of the artifacts of health information and anticipated urgency in the need to retrieve it.
Conclusion: Laypeople develop and employ robust, complex strategies for managing health information in the home. Capitalizing on these strategies will complement and extend current consumer health innovations to provide functional support to people who face increasing demands to manage personal health information.
When health care migrates to the community and the home, the talents, behaviors, and active involvement of residents in a specific household complement the work in health care institutions. In taking increasing responsibilities for their own health, laypeople face growing health information management challenges. Their efforts in “keeping things under control,” knowing which prevention recommendations to follow, deciding which information to attend to, which self-assessments to perform, and which health observations must be reported to health care practitioners, taxes even the most diligent person in their personal health information management. Consequently, what was an optional choice by an individual to engage in or eschew, health information management has become an essential responsibility.
What laypeople actually do with the health information they search for and retrieve, where they are when using these resources, or how they integrate health information and resources in their daily lives are rarely addressed in health services or medical informatics research. Exploring health information management in the context where most of these activities take place, i.e., the household, can provide rich insights into the kinds of information and sources used, and the strategies and procedures employed in health information management in the household (HIMH). In addition, insight to HIMH may point to the health and illness situation of a community. Effective HIMH could, for example, ensure that poison-control instructions or directions regarding biological exposures would be accessible in every home. Consequently, systematic collection, storage, and handling of health information in the household are significant to the health of individuals and the public health of the community.
In this paper, we report from the study Advanced Technologies for Health@Home, exploring HIMH through the lens of the household's self-identified information manager.
Background
Consumer health informatics (CHI) innovations include access to telehealth,1 relevant tailored health information,2 peer-support groups,3 communication resources for collaborative care and treatment post-discharge,4 patient portals to view the personal health record and/or agency-specific information (see, for example, www.patientsite.org), as well as health-related Web sites like WebMD™. CHI is largely computer-based interventions informed by one of two frameworks. The more common behavioral change approach applies sociocognitive theories. These theories guide the type of content to include and the manner in which systematic application of this content help to motivate individual behaviors to achieve health care goals.5 Because everyday health behaviors occur in communities, homes, and family structures, these content-specific, individually oriented resources might be more effective if informed by the context in which they are intended to be used. The other approach to CHI design, business process models,6 emphasizes information flow and affords insights to the role of personal health information management in the health care process. However, the usefulness of business process models seem restricted to fairly well-understood, repetitive information processing tasks, such as medication renewal and appointment setting.
Promoting engagement and facilitating self-management to enhance self-care is integral to ensuring the benefits of professionally provided health care services.2,4 In order to meet health goals and accomplish self-care, laypeople's responsibilities for health information management in the physical environment of their household increases. Self-care and HIMH are activities in which deliberate use of available sources and strategies represents a learned, practical response to demands or anticipated situations.7 Consideration of the person and his or her health goals, the context within which they reside, and the health information management demands engendered by health care practices complement current efforts in CHI.
Studies of the household as the context for health information management reveal that households are complex arenas. There are a multitude of meanings attached to a home, and most artifacts found there carry multiple functions.8 In addition, activities are distributed throughout multiple spaces of varying significance that convey meaning about information uses, routines, responsibilities, rights, and obligations.9,10,11 The kitchen serves as the primary space for awareness, coordination, internal communication, and shared information production and management in a household.12 Routine activities are like “glue” to everyday life,13 and health information management is one such activity. However, the coordination and awareness of activities like information management, self-care, and health maintenance taking place in the home remain largely invisible and underarticulated.14,15
Membership in a household is more emotionally based than a work setting, and belonging to a household may be less voluntary. Authority patterns can be different, and collaboration conforms to unwritten rules as well as contracted relationships. Households can be compared to microsocial systems similar to small, shared work settings.16 Devices like computers, once restricted to industrial environments but now adopted for personal purposes, allow a wider range of activities to go on in the household.8 Personal health information management is carried out in the household setting and is most realistically explored in its unique environment.
Considering HIMH as a type of “work” rather than a personal health behavior provides a richer base from which we can identify strategies and information technologies that support complexities of contemporary health care.15 Rather than focusing on discrete tasks and individual human cognition,17,18 the sociotechnical approach19,20 offers a structure to explore interwoven networks of people, tools, routines, sources, and responsibilities.
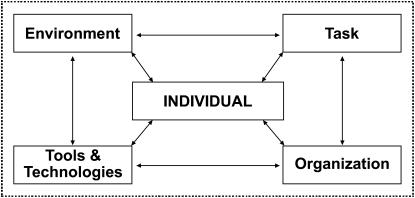
For this study, the sociotechnical approach is best illuminated through a framework from human factors engineering. We chose the Balance Model,21,22 a framework developed to study human response in the workplace, for our investigation of HIMH. The Balance Model enumerates components and interrelationships among those components that lead to production of work. Although originally established for assessing paid work, the similarities of the unpaid work of personal health information management to the overall work of clinical data management make the Balance Model acceptable for this study. In the present study, the Balance Model provided guidance for efficiently analyzing components of HIMH. ▶ depicts the Balance Model.
Figure 1.
The Balance Model of work (taken from Smith and Carayon: Ref 22). The model illustrates interdependent relationships between the identified components in order to accomplish work.
At the center of the model is the individual, whose knowledge, perceptions, thoughts, and life experiences provide the filter for perceiving the remaining factors: tasks, tools and technologies, organizations and environment. The tasks constitute the full set of activities applied coherently to achieve purposeful work. Tools and technologies include both the artifacts employed in the accomplishment of work as well as the processes that one creates or adapts in the accomplishment of work. Organizations form the sociopolitical context of work and shape communication pathways, rights and responsibilities, and authority relationships. The environment provides the physical context within which work occurs.21,22 The concept of “balance” refers to reciprocal, compensatory and interdependent relationships between the components in the model. According to the Balance Model, the activities and strategies in one's work are directed toward goals and consequences of tasks undertaken by the individual using specific tools and technologies related to the internal and external organization within a given physical environment.
Methods
Design
The work reported here was done as part of a larger set of projects under way in collaboration with a local community health planning group. In the study Advanced Technologies for Health@Home, we used a community-centered approach to health information systems planning. An important aspect of our approach is to understand CHI challenges in the context of the local health resources, including the community resources of libraries, health care providers, and health education opportunities. This approach permitted task analysis of how laypeople manage health information, mindful of the available local institutions to provide health information.23,24 In this paper, we present findings based on the task analysis of how laypeople manage health information in their household.
Setting
The investigation of HHIM occurred in a two-county rural community in the midwestern United States. We collaborated with a local voluntary planning organization that coordinates the health planning for this community of 150,000 people. The community partner offered support for recruitment and provided a credible introduction to the community residents. As part of this partnership, our research goals are always established in conjunction with the community partner's input. Where possible without compromising the scientific questions, we take into account community needs and preferences. For example, in the present study, we oversampled Latinos because the community partner had noted a recent rapid increase in this population and wanted to better understand their health information needs.
Sample
Following human subjects' approval from the University of Wisconsin Health Sciences Institutional Review Board, we sought a purposive sample of healthy volunteers. The sample was recruited through public advertising, health fairs, and local community gathering places. We successfully recruited representatives of 49 households in the time frame allotted and reached the 20% Spanish-speaking participation requested by our community partner.
The recruited informants were self-identified information managers who served as primary informants and representatives of the households. Data were obtained through visits to the informant's main residence (n = 39) or a location of the informant's choice (n = 10). During an approximately 90-minute interaction, data were collected in a semistructured interview guided by model case scenarios and predefined questions about common HIMH situations. Demographic and household data were obtained. The model case scenarios were brief text descriptions: for example, “After meeting with your doctor, he/she gives you a prescription and a follow-up appointment. Take me/us through how you would fill the prescription, remember the doctor's orders, and the follow up appointment and so forth.” Additional questions focused on typical situations, for example, “How do you keep track/manage health information at home? Include where this information is stored and please describe as specifically as possible how you store each of the different types of health information.” Where possible, we made digital photographs of HIMH artifacts, i.e., tools and devices, as identified and pointed out by the informant during the interview. These photographs captured the context and location of the artifact without focusing on the content or persons in the household. This paper reports findings from analysis of the data obtained in the semistructured interviews and uses photographs of HIMH artifacts as illustration of these findings.
Data Analysis
Health information management in the household is observable through the verbalizations of individuals and documented by pictures of artifacts. These collected textual and visual representations provided snapshots about health information management and were useful and appropriate to explore and describe an understudied phenomenon like HIMH.25
The data from the interviews were subject to content analysis.26 Operational description of the Balance Model's five components (individual, task, tools and technologies, organization, and environment) related to HIMH provided broad categories for the coding scheme.27 In addition, we established the category “other” for data not captured by the operational descriptions of the Balance Model's components. The QSR NVIVO software28 was used for coding and reorganizing the collected data prior to further abstraction. Data were coded by one person and analyzed by another person, who also served to check agreement of initial coding. The coded data were subjected to sorting according to assigned codes and abstracted to the findings presented for each of the categories in the Balance Model.
Data analysis also included examination of photographs of artifacts (tools and technologies) shown by the informants as examples of what they used or kept to assist them in HIMH. We obtained digital photographs of artifacts from 38 of the 49 households. In total, 176 pictures were taken. The images were examined and categorized according to the physical object present in the picture and the location, i.e., where in the household the picture was taken. This process was an inductive, systematic, and observational categorization or inductive content analysis,29 assigning metadata and reorganizing them according to the representation in the picture.
Results
Demographics
Demographics of the recruited sample (N = 49) are summarized in ▶.
Table 1.
Demographics of the Recruited Sample of 49 Households
| 1.Ethnicity | ||||||||
| 40 households: White Caucasian | ||||||||
| 9 households: Latinos | ||||||||
| 2.Gender | ||||||||
| 47 of 49 self-identified health information managers were women | ||||||||
| 3.Age and gender distribution in the household | ||||||||
| Age | Male | Female | Total | |||||
| 0–6 | 4 | 9 | 13 (10%) | |||||
| 7–18 | 13 | 14 | 27 (20%) | |||||
| 19–25 | 9 | 3 | 12 (9%) | |||||
| 26–64 | 28 | 31 | 59 (45%) | |||||
| 65–84 | 7 | 10 | 17 (13%) | |||||
| 85+ | 0 | 4 | 4 (3%) | |||||
| 4.Perception of health in the household | ||||||||
| a.Informant's perceived personal health | ||||||||
| 32 (65%): very good or excellent | ||||||||
| 16 (33%): good or fair | ||||||||
| b.Informant's perceptions of household member's health | ||||||||
| 26 (57%): very good or excellent | ||||||||
| 15 (31%): good or fair | ||||||||
| 1 (2%): poor | ||||||||
| 5.Informants' self-assessment of their involvement in HIMH | ||||||||
| Households with children | Adults only | Seniors only | Total | |||||
| I manage all health information in the household | 13 | 8 | 10 | 31 (64%) | ||||
| I manage most health information in the household | 7 | 3 | 5 | 15 (31%) | ||||
| Someone else manages health information in the household | 1 | 1 | 1 | 3 (6%) | ||||
| Total | 21 (43%) | 12 (24%) | 16 (33%) | N = 49 | ||||
| 6.Residence type | ||||||||
| Separate homes: 34 | ||||||||
| Attached homes: 6 | ||||||||
| Not assessed: 9 (informants were not interviewed in main residence) | ||||||||
| 7.Sufficient income | ||||||||
| Yes: 43 (88%) households | ||||||||
| No: 2 (4%) households | ||||||||
| No answer: 4 (8%) households | ||||||||
HIMH = Health Information Management in the Household.
▶ shows that the majority of self-identified information managers responding in this study manage all information of the household. They reported having sufficient income to meet their needs. The primary informant described their health slightly better than other household members' health. In common with previous studies,30 female household members continue to assume primary responsibilities for health information management, prevention, maintenance, and informal care.
HIMH Analyzed According to the Balance Model
Findings for each of the categories in the Balance Model are presented first. Most data were captured by the operational definitions of the Balance Model's components. There were more data coded as “tools and technologies” or as “tasks” than “organization” and “environment,” possibly reflecting focus of attention in the model case scenarios and questions in the interview. Since these components are interdependent and act in concert, synthesizing them led to the identification of differentiated storage strategies to accomplish HIMH.
Individual
The category individual represents findings about the information manager per se. The majority of the self-identified health information managers were women (47 of 49 or 95%, N = 49); 65% managed all the health information in the household alone.
Health information management seems largely a solitary, individual responsibility. As already shown in ▶, HIMH was most often carried out by the self-identified information manager. Their concerns, sources, and needs varied, but their health information management issues arose from health issues experienced by household members. The informants often had more concern for other household members' health, e.g., elders or children, than their personal health. The goals identified in HIMH ranged from
prevention, e.g., childhood infectious disease immunization, flu shots
managing identified health problems in the household including cardiovascular problems, respiratory problems, nutritional concerns, cancer, and mental health problems
self-assessment, identifying appropriate health care services for the household given constraints of insurance coverage, available funds, and language skills
In most white households, the information managers reported confidence in their ability to get information when needed. Representatives of the Latino households expressed difficulties in obtaining information in a language they fully commanded or understood. These respondents found it difficult to locate necessary information and experienced additional challenges in HIMH. These informants also expressed difficulties when interacting with the health care system because the providers' style or attitude did not match their expectation for information or instructions, especially about self-care and child development. As a consequence, they often involved a more competent English-speaking family member or friend to make sure they got what they otherwise might be unable to acquire.
Tasks
Analysis of responses coded as tasks identified three different types of activities in HIMH:
observing, assessing, and surveying household members' health conditions
organizing, separating, and differentiating information types according to perceived importance or relevance
obtaining, retrieving, and keeping track of health information according to household needs, from sources like family, friends, one's own memory, providers, libraries, drug stores, and the Internet
Only a few respondents expressed a sense of information overload, choosing not to take on tasks or look up information because they found it too confusing.
Health information comes from a variety of sources. ▶ presents a summary of sources from which health information is acquired, ranked according to the frequency of identification.
Table 2.
Sources for Health Information, Ranked by Frequency of Identification (N = 49)
| Doctor's visits | 45 (92%) |
| Family and friends | 39 (80%) |
| Clinics or hospitals | 36 (73%) |
| News reports | 34 (70%) |
| Reference books | 24 (49%) |
| Health magazines | 23 (47%) |
| Internet | 23 (47%) |
| Classes | 16 (33%) |
| Public library | 14 (29%) |
| Public health nurse | 11 (22%) |
| Alternative medical sources | 10 (20%) |
| School | 9 (18%) |
| Hotlines | 3 (6%) |
| Other | 5 (10%) |
As shown in ▶, the most commonly used sources are family doctor and family or friends, especially those who were health professionals, older, or perceived as more experienced. News media and the Internet helped indicate “normal” experiences regarding health conditions, strategies for prevention, or experiences in a specific trajectory. An interpretation of a condition's perceived seriousness or urgency seems to determine the kind of sources to consult for a task. Several informants revealed that if they considered a situation very serious, they contacted their physician first, but when it was perceived as less urgent, they just as likely consulted family or friends or used the library or the Internet.
Tools and Technologies
Analysis of material coded as tools and technologies showed a variety of artifacts employed for the work of HIMH. Most of the used tools and technologies were paper based. In fact, in 95% of the 176 images of the tools and technologies, the artifacts shown to us and photographed were paper based.
To support HIMH, most tools and technologies were used by the individual to keep up with:
health information management to support for future use, e.g., calendars, phonebook, medical history or separate sheets of paper with information of procedures, medication side effects, and, less commonly, as personal digital assistants or personal computers
health information management specific to health condition management in a household, e.g., special cards holding vital information like medication, blood type, medication information; folders and notebooks with personal health information or insurance information; medical record information; and general books, printouts from Internet searches, and information from mass media, most commonly television and radio
household-specific health condition management, e.g., support devices like walker, crutches, knee brace, wheelchairs, monitoring devices like a blood pressure and monitor, scale, glucose meter, thermometer, and treatment devices like a first aid kit, insulin pump, asthma chambers, pill box organizer and medication containers
The tools and technologies contained embedded mechanisms that provided cues to keep on top of tasks.
Organization
Responses coded as organization included the communication pathways, authority relationships, and rights and responsibilities. In HIMH, we found that a range of formal and informal groups was consulted for health information management activities for the household. The household, generally a nuclear or extended family, were the primary informal group. Health care providers were examples of formal groups, and they serve as both sources of health information and entities with which to exchange information.
There were different types of information exchanged in these pathways for the informal and formal groups. ▶ summarizes the information types as logistic information, personal information, and reference material identified for HIMH, ranked according to frequency of identification.
Table 3.
Health Information Types Consulted for HIMH, Grouped and Ranked by Frequency of Identification (N = 49)
| Logistic information | ||
| Doctor's appointment | 46 (94%) | |
| Health insurance | 43 (88%) | |
| Doctor's contact information | 42 (86%) | |
| Prescription information | 36 (73%) | |
| Provider information | 34 (69%) | |
| Doctor hospital clinic information | 29 (59%) | |
| Medical schedules | 29 (59%) | |
| Personal information relevant to household member, including informant | ||
| Birth/death certificates | 37 (76%) | |
| Medical history | 28 (57%) | |
| Immunization records | 28 (57%) | |
| Personal observations | 27 (55%) | |
| Lab results | 20 (41%) | |
| X-rays | 8 (16%) | |
| Reference material | ||
| Literature | 35 (71%) | |
| Instructions on self-care | 23 (47%) | |
| Poison control | 22 (45%) | |
As shown in ▶, information to keep up with the logistics of HIMH is the most often exchanged type of information and indicates coordination responsibilities and interactional aspects in HIMH.
Environment
Material coded as the category environment includes data about where the work of HIMH occurs. Findings from the interviews and the pictures reveal that consistently across the visited households most often information was kept in shared household spaces like the kitchen, office, bathroom, and bedroom, indicating that much of the work of HIMH occurs here. Some information was kept with the individual, in a purse or billfold, but more health information or artifacts were kept in a kitchen drawer, boxes, cake pans, or book shelves in living room or hallway or filed in a home office or a cabinet in a bedroom or the basement. Of the 176 collected photographs, 65 were of artifacts kept in the kitchen and 27 were of artifacts kept in the home office. Such use of the environment as a location for health information seemed to reflect trade-offs between accessibility, visibility and some anticipated future use for the information.
Interconnectedness of the Balance Model's Components
Synthesizing analysis of these five components of the Balance Model shows HIMH as a variable set of interdependent activities that occur in concert, requiring employment of strategies based on health concerns, experiences, and exposures to health issues.
The analysis revealed how frequently used or important tools and technologies were kept within sight or in designated areas, implying a reminder function, accessible and well known to the household members. We found that health information or artifacts for daily or frequent use were kept visible in shared spaces, and health information or artifacts for less frequent use were kept in well-known places, usually out of sight, but familiar and available for the household members' access. Some health information, e.g., blood type and allergies, insurance cards, and medication whose discontinuation would be life threatening, seemed regarded as vital and kept with the individual household member most times, e.g., kept in a purse or billfold, available in case of an unexpected event or emergency.
This interdependence of the “tasks,” available “tools and technologies,” “organization,” and “environment” by the “individual” demonstrates purposeful ways to perform tasks with available tools and technologies and attaching cues to optimize HIMH. This is an important aspect that demonstrates the interconnectedness of the Balance Model's components. Employment of storage strategies aligned with anticipated use emerge as the most important insight about HIMH in relation to an informatics perspective and led to identification of various storage strategies.
Model Formulation: Differentiated Storage Strategies
Conceptualizing and analyzing HIMH as work revealed that growing amounts of health information are brought into the household and kept under assumptions of future needs. Exploring structural dimensions of HIMH illuminates sophisticated, complex, and robust storage strategies. This finding is captured as differentiated health information storage strategies named:
“Just-in-time” is a storage strategy where information and/or artifacts are with a household member at most times. ▶ gives an example of this storage strategy.
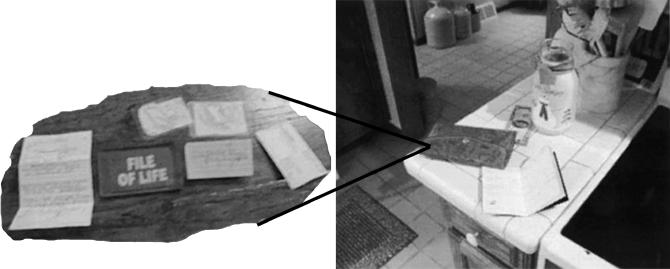
“Just-at-hand” is a storage strategy where information and/or artifacts are visible or stored in readily accessible, highly familiar locations in the household. ▶ gives an example of this storage strategy.
“Just-in-case” is a storage strategy where information and/or artifacts, either personal health files or general health information resources, are kept away but accessible within reasonable time for any future situation. ▶ gives an example of this storage strategy.
“Just-because” is a storage strategy where information and/or artifacts about a health concern are brought into and kept in the household but, because of a temporal relevance, no other storage strategy is assigned. ▶ gives an example of this storage strategy.
Figure 2.
Example of “just-in-time” storage strategy.
Figure 3.
Example of “just-at-hand” storage strategies.
Figure 4.
Example of “just-in-case” storage strategy.
Figure 5.
Example of “just-because” storage strategy.
These storage strategies are further explicated in ▶.
Table 4.
Differentiated Storage Strategies Employed in HIMH
| Strategy | Description |
|---|---|
| Just-in-time | Artifacts/information is with a person at most times, reflecting anticipation of being important/necessary to declare in unexpected event/emergency or perceived important to be (re)produced regardless of location, situation, or time. |
| Just-at-hand | Artifact/information may be visible or stored in readily accessible, highly familiar locations to the person(s); has some permanence and serves logistical functions: reminding, monitoring, coordination. |
| Just-in-case | Artifact/information is either personal health files or general health information resources kept for a purpose in any future situation. |
| Just-because | Artifact/information about a health concern brought into and kept in the household, having a temporal relevance in a given point in time but has to make decision to toss or keep and file. |
Model Validation
The variability in the proposed storage strategies comes from the location of different types of information or artifacts, assigned importance of information or an artifact, visibility for cues or reminders, and anticipated urgency or available time to locate the information or artifact when the need arises. While validation of the storage strategy model awaits testing in new environments, we present here an in-depth description and critical appraisal of the four types of storage strategies observed in this project.
The “just-in-time” and “just-at-hand” storage strategies share that visibility and accessibility is important for the health information management activities these strategies support. However, the differences between the “just-in-time” and “just-at-hand” strategies rest in the function and perceived importance of the information. Information stored according to a “just-in-time” strategy seems important regardless of location and time and therefore with the person at most times. Information stored according to the “just-at-hand” strategy was typically kept in a designated location to remind about appointments and contact information to providers, e.g., family doctor, or self-monitoring activities for household members. This may imply support for coordination with implicit (or explicit) trade-offs where information kept visible may compromise privacy but be more likely to be remembered.
For the “just-in-case” and “just-because” storage strategies, information or artifact's visibility seems less important. A “just-in-case” storage strategy reflects the case when the individual recognizes that information will be required at some point in the future. This applies to personal information like medical record extracts, X-rays, or birth/death certificates and reference material and general health information resources. Thus, the individual stores it in a place where it will be out of the way, filed under a heading known as meaningful for locating the materials later and accessible within reasonable time should the need arise. A “just-because” strategy is apparent when the person recognizes that the information is likely to be important but lacks the immediate relevance that would enable classification and assign another storage strategy. This strategy was typically applied to material like pamphlets or printouts explaining a health condition of general or possible relevance to the household. Such information was kept in an aggregate collection with other similar information, with the hope of rummaging through all the materials to locate it in the event a need arises.
These differentiated storage strategies reflect synergy of location, information, or artifact, and anticipation about future need or use of the information. Therefore, they resonate with and expand earlier described “just-in-time” approaches to inventory management.31 The household can be seen as an arena handling growing inventories of health information. Applying ideas from “just-in-time” approaches complies with current trends like (1) emerging self-directedness in health information management, (2) requiring information specific to the situation at hand, (3) readiness to acquire information, and (4) perceived relevance of information to imminent experience or challenge.32,33,34 Therefore, ideas from the “just-in-time” approach to inventory management can be helpful to further explicate the work of HIMH. However, further validation of these identified storage strategies should be further explored. We will include this aspect in upcoming studies in collaboration with our community partner.
Implications for CHI Innovations
Laypeople's actual work related to self-care and health maintenance remains largely invisible and underarticulated. As such, HIMH is still not fully understood.
Our analysis of HIMH leading to identification of differentiated information storage strategies highlights structural aspects with implications for future CHI innovations. Similar to previous studies of the home environment, this work points out that the storage of information and activities in HIMH are distributed throughout multiple spaces,13 that there seem to be trade-offs in how accessible health information or artifacts are kept,12 and that visibility of information or artifacts is important for coordination and awareness in the process of HIMH.14 We suggest that CHI innovations capitalize on people's current storage strategies to provide support for HIMH and use of health information for self-care and health maintenance.
A striking finding from this study is the extensive reliance on paper media. Whether in paper format or on a computer screen, the plethora of important and incidental health information places management demand on laypeople and requires them to create and employ sophisticated information management strategies for storage and future use.35 Drawing from our findings, we suggest that CHI innovations for the near future must encompass both paper and electronic media and provide ways to better integrate these two disparate media.
In addition, self-care, health maintenance, and health information management is a personal health management responsibility but also something done for household members. How people keep information or particular artifacts varies, but the strategies they employ seem to embed cues and reminders pointing to trade-offs of visibility and time to locate information according to how they think the information or artifact will be used in the future by themselves or by household members. We therefore suggest that CHI innovations support anticipation of future use of information by an individual, but also for household members, and align with use of spaces to support health information activities in a household.
Limitations to the Analysis Leading to Identification of Differentiated Storage Strategies
Health information management is likely to vary within households, families, culture groups, and societies. Therefore, the identified, differentiated storage strategies need further exploration and verification.
Limitations to the analysis presented in this paper relate especially to (1) data collection during home visits followed a rather structured interview possibly drawing attention to the model case scenarios and predefined questions; (2) focus on the health-related information, current tasks, and tools and technologies in use, at the cost of other information management responsibilities; (3) little attention to household behaviors over time or how they are changing related to life span development or when illnesses are acquired; (4) only seeing parts of the household where access was allowed or did not feel intimidating; and (5) the rather extensive and purposeful approaches to HIMH identified here may not apply to less well-organized lives. To suggest scalable, representative, and transferable storage strategies, the importance and significance of de facto variability and heterogeneity of households, cultures, and societies and the methodological challenges reflected herein need further exploration.
Conclusions
In this paper, we have characterized HIMH as work and used a sociotechnical approach illuminated by a human factors framework to examine structural components contributing to the accomplishment of this work. This led to identification of differentiated storage strategies as an important structural dimension of HIMH. Our study demonstrates that laypeople develop robust, complex strategies to store health information or artifacts guided by how they think they might use the information in the future. Most CHI innovations focus on improved access to health information, e.g., the electronic health record, agency-specific information material for post-discharge care or treatment, or in-home monitoring technologies. Differentiated storage strategies complement and carry implications for design of CHI resources more aligned with what laypeople do with health information they retrieve and store.
The analysis in this paper is notable by its emphasis on the household to understand HIMH as work and explicitly setting out to examine activities, technologies, and context of health information use. Through the lens of the household's self-identified information manager, the study demonstrates differentiated storage strategies. This is an important insight to HIMH that requires timely, functional support for laypeople to handle personal health information and the myriad of instructions for prevention, surveillance, and management of health problems.
Further analysis of how household spaces are used for HIMH and specific motivators for the differentiated storage strategies of health information and artifacts identified here is necessary. However, contextual assessment to explore one of the most important but understudied settings, the household, is a valuable starting point to appreciate laypeople's work of HIMH. Support for differentiated information storage strategies to keep up with household's growing health information management challenges can make future CHI innovations more efficient resources to support HIMH.
The study Advanced Technologies for Health@Home is funded through a grant from the Intel Corporation to the University of Wisconsin-Madison (Dr. Brennan, Principal Investigator). We acknowledge contributions from Chris Brunnette, MS, past project manager, research assistants Jared Wickus, MS, and Teresa Zayas-Cabán, MS, PhD, who did most of the home visits, and collaboration with the Dodge-Jefferson Community, as well as support from the Health Systems Lab at UW-Madison. Dr. Moen was supported by a grant from the US-Norway Fulbright Association and a postdoctoral fellowship from the Norwegian Research Council, and PFB is supported by the Moehlman Bascom Fund, University of Wisconsin–Madison.
References
- 1.Brennan PF. Telehealth: bringing health care to the point of living. Med Care. 1999;37:115–6. [DOI] [PubMed] [Google Scholar]
- 2.Brennan PF, Moore SM, Bjornsdottir G, Jones J, Visovsky C, Rogers M. HeartCare: an Internet-based information and support system for patient home recovery after coronary artery bypass graft (CABG) surgery. J Adv Nurs. 2001;35:699–708. [DOI] [PubMed] [Google Scholar]
- 3.Gustafson DH, Hawkins RP, Boberg EW, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int J Med Inf. 2002;65:169–77. [DOI] [PubMed] [Google Scholar]
- 4.Safran C. The collaborative edge: patient empowerment for vulnerable populations. Int J Med Inf. 2003;69:185–90. [DOI] [PubMed] [Google Scholar]
- 5.Kreuter M, Farrell D, Olevitch L, Brennan L. Tailoring health messages. Customizing communication with computer technology. London: Lawrence Erlbaum, 2000.
- 6.Deming WE. Quality, productivity, and competitive position. Cambridge, MA: Massachusetts Institute of Technology, Center for Advanced Engineering Study, 1982.
- 7.Orem DE, Taylor SG, Renpenning KM. Nursing, concepts of practice. , 6th ed St. Louis: Mosby, 2001.
- 8.Cummings JN, Kraut R. Domesticating computers and the Internet. Inform Soc. 2002;18:221–31. [Google Scholar]
- 9.Mentas M, Salvador T, Scholtz J, Sorensen D. Engineering Ethnography of the Home. In: Tauber MJ, editor. Conference companion on human factors in computing systems: common ground (CHI'96). Vancouver, Canada: ACM; 1996. p. 283–4.
- 10.O'Brien J, Rodden T. Interactive systems in domestic environments. In: Coles S, editor. Proceedings of the Conference on Designing Interactive Systems: Processes, Practices, Methods, and Techniques. Amsterdam, The Netherlands: ACM Press; 1997. p. 247–59.
- 11.Hindus D, Mainwaring SD, Leduc N, Hagström AE, Bayley O. Casablanca: designing social communication devices for the home. In: Jacko J, Sears A, editors. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. Seattle, WA: ACM Press; 2001. p. 325–32.
- 12.Crabtree A, Hemmings T, Rodden T. Pattern-based support for interactive design in domestic settings. In: Mackay W, Amowitz J, Gaver W, editors. Proceedings of the Conference on Designing Interactive Systems: Processes, Practices, Methods, and Techniques. New York: ACM Press; 2002.
- 13.Tolmie P, Pycock J, Diggins T, MacLean A, Karsenty A. Unremarkable computing. In: Wixon D, editor. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems: Changing Our World, Changing Ourselves. New York: ACM Press; 2002.
- 14.Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform. 2004;37:128–37. [DOI] [PubMed] [Google Scholar]
- 15.Unruh KT, Pratt W. Patients as actors: patients' role in detecting and preventing medical errors. Paper presented at IT in Health Care 2004: Socio-technical Approaches—To Err Is System. Portland, OR: OSHU 2004.
- 16.Vitalari NP, Venkatesh A, Gronhaug K. Computers in the Home: Shifts in the Time Allocation Patterns of Households. Communications of the ACM. 1985;28:512–22. [Google Scholar]
- 17.Patel VL, Arocha JF, Kaufman DR. A primer on aspects of cognition for medical informatics. J Am Med Inform Assoc. 2001;8:324–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaufman DR, Patel VL, Hilliman C, et al. Usability in the real world: assessing medical information technologies in patients' homes. J Biomed Inform. 2003;36:45–60. [DOI] [PubMed] [Google Scholar]
- 19.Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inf. 1999;55:87–101. [DOI] [PubMed] [Google Scholar]
- 20.Iversen KR, Grøtan TO. Socio-technical aspects of the use of health related personal information for management and research. Int J Biomed Comput. 1996;43:83–92. [DOI] [PubMed] [Google Scholar]
- 21.Smith MJ, Sainfort-Carayon P. A balance theory of job design for stress reduction. Int J Indust Ergon. 1989;4:67–79. [Google Scholar]
- 22.Smith MJ, Carayon P. New technology, automation, and work organization: stress problems and improved technology implementation strategies. Int J Hum Factor Manufact. 1995;5:99–116. [Google Scholar]
- 23.Dym CL, Little P. Engineering design: a project-based introduction. New York: John Wiley & Sons; 2000.
- 24.Ford JM, Wood LE. An overview of ethnography and system design. In: Wixon D, Ramey J, editors. Field methods casebook for software design. New York: John Wiley & Sons; 1996. p. 269–82.
- 25.van't Riet A, Berg M, Hiddema F, Sol K. Meeting patient's needs with patient information systems; potential benefits of qualitative research methods. Int J Med Inf. 2001;64:1–14. [DOI] [PubMed] [Google Scholar]
- 26.Cavanagh S. Content analysis: concepts, methods and applications. Nurse Res. 1997;4:5–16. [DOI] [PubMed] [Google Scholar]
- 27.Ford K, Oberski I, Higgins S. Computer-aided qualitative analysis of interview data: some recommendations for collaborative working. Qual Rep. 2000;4. http://www.nova.edu/ssss/QR/QR4-3/oberski.html.
- 28.QSR. QSR NUD·IST User guide. , 4th ed Thousand Oaks, CA: Sage; 1997.
- 29.Bell P. Content analysis of visual images. In: van Leeuwen T, Jewitt C, editors. Handbook of visual analysis. London: Sage; 2001.
- 30.Levine SA, Boal J, Boling PA. Home care. JAMA. 2003;290:1203–7. [DOI] [PubMed] [Google Scholar]
- 31.Svensson G. Just-in-time: the reincarnation of past theory and practice. Manag Decis. 2001;39:866–79. [Google Scholar]
- 32.Cheuh H, Barnett GO. “Just-in-time” clinical information. Acad Med. 1997;72:512–7. [DOI] [PubMed] [Google Scholar]
- 33.Whitson D. Applying just-in-time systems in health care. IIE Solutions. 1997;29:32–8. [Google Scholar]
- 34.Davenport TH, Glaser J. Just-in-time delivery comes to knowledge management. Harv Bus Rev. 2002;80:107–11. [PubMed] [Google Scholar]
- 35.Jones W. Finders, keepers? The present and future perfect in support of personal information management. First Monday. 2004;9.