Abstract
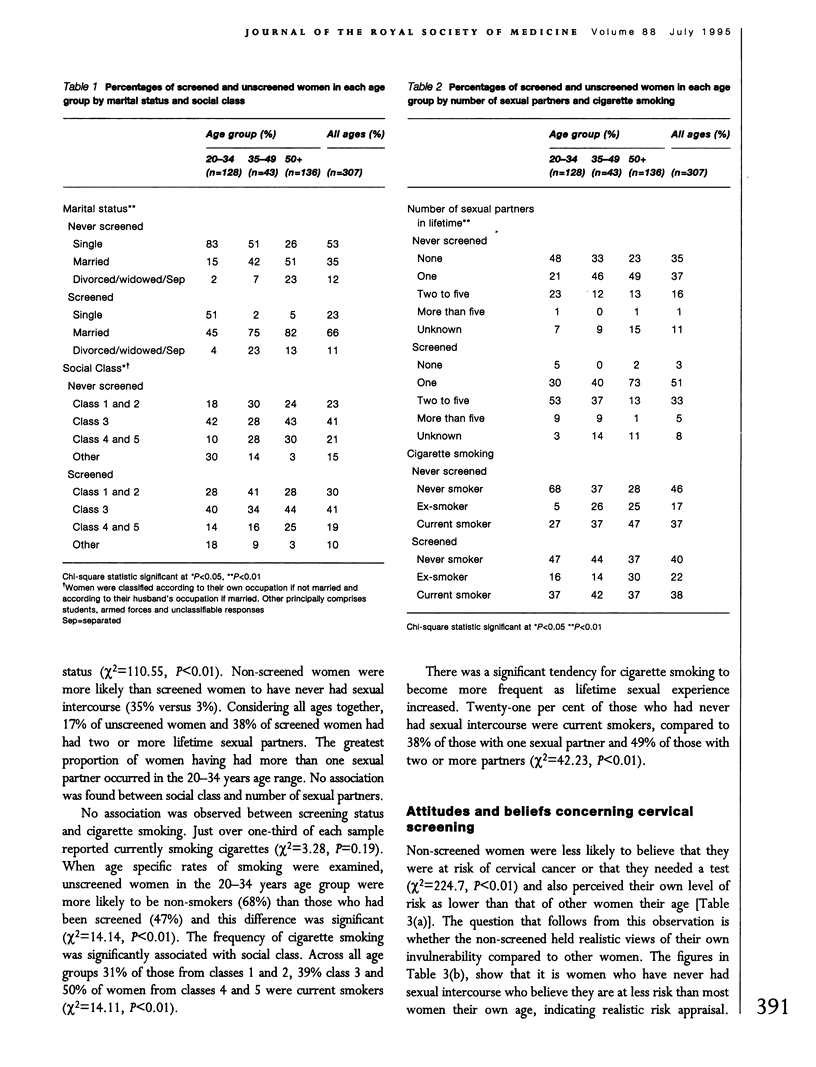
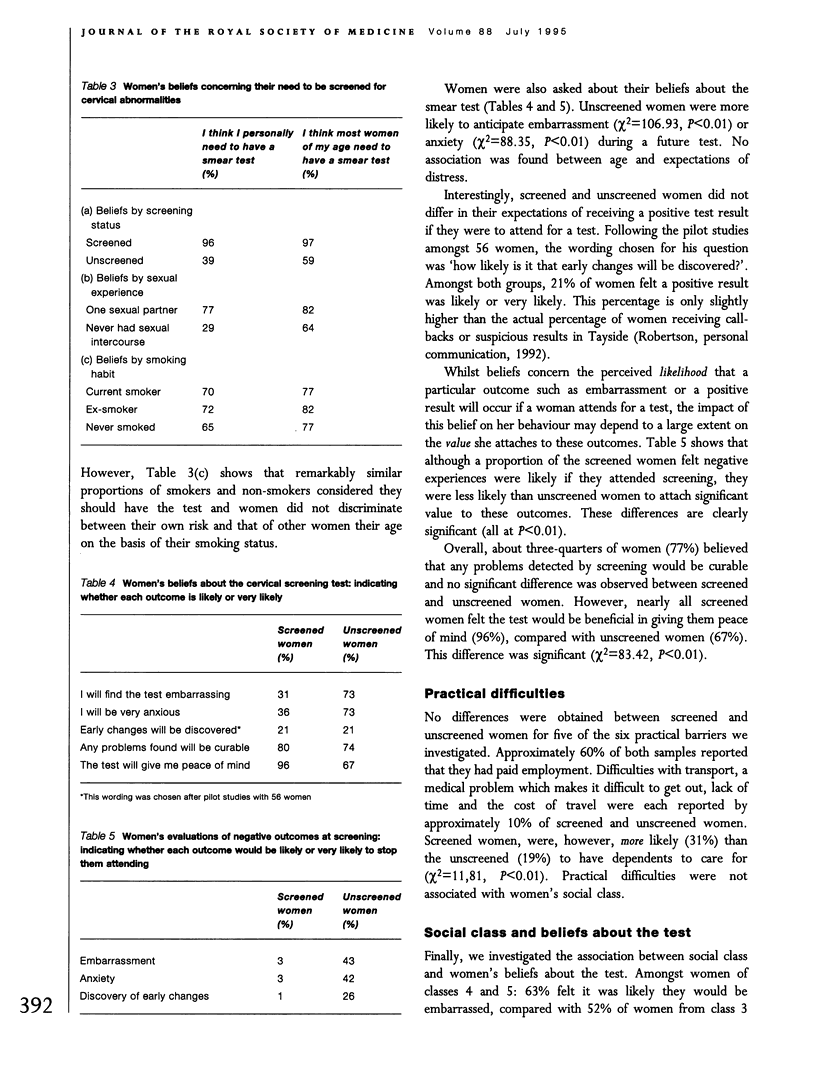
A case-control study was conducted to assess the effectiveness of a regional call programme in reaching women at risk of cervical cancer. Home interviews were conducted with a random sample of 614 women aged 20-64 who were identified from a computerized register as either having had a smear test within the previous 3 years or not having an up-to-date smear history. Unscreened women fell principally into two age cohorts: under 35 years and over 50 years. A small social class differential was found to persist following the campaign. Overall, unscreened women were not at epidemiologically higher risk than the screened population. Thirty-five per cent of unscreened women reported never having had sexual intercourse compared to 3% of screened women: 17% of the unscreened and 38% of screened women reported two or more lifetime sexual partners. No difference was observed between screened and unscreened women in the frequency of current cigarette smoking (37% unscreened, 38% screened). Cigarette smoking was, however, associated with social class (31% classes 1 or 2 compared with 50% classes 4 and 5). Level of practical difficulties did not differentiate those who attended from those who did not, suggesting that recent changes to delivery or screening services have been effective in ensuring equity of access. Non-attenders and lower class women held more negative attitudes towards the test procedure and were less likely to believe that they were at risk of cervical cancer. Perceived personal risk was not associated with cigarette smoking, suggesting that further attention might be given to this factor in educational campaigns.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carstairs V., Morris R. Deprivation and health in Scotland. Health Bull (Edinb) 1990 Jul;48(4):162–175. [PubMed] [Google Scholar]
- Chisholm J. W. The 1990 contract: its history and its content. BMJ. 1990 Mar 31;300(6728):853–856. doi: 10.1136/bmj.300.6728.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crombie I. K., Orbell S., Johnston G., Robertson A. J., Kenicer M. Cervical screening: the optimum visit plan for contacting users and non-users in Scotland. J Epidemiol Community Health. 1994 Dec;48(6):586–589. doi: 10.1136/jech.48.6.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkind A. K., Haran D., Eardley A., Spencer B. Reasons for non-attendance for computer-managed cervical screening: pilot interviews. Soc Sci Med. 1988;27(6):651–660. doi: 10.1016/0277-9536(88)90014-7. [DOI] [PubMed] [Google Scholar]
- Meadows P. Study of the women overdue for a smear test in a general practice cervical screening programme. J R Coll Gen Pract. 1987 Nov;37(304):500–503. [PMC free article] [PubMed] [Google Scholar]
- Reid G. S., Robertson A. J., Bissett C., Smith J., Waugh N., Halkerston R. Cervical screening in Perth and Kinross since introduction of the new contract. BMJ. 1991 Aug 24;303(6800):447–450. doi: 10.1136/bmj.303.6800.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson A. J., Reid G. S., Stoker C. A., Bissett C., Waugh N., Fenton I., Rowan J., Halkerston R. How complete can cervical screening be? The outcome of a call screening programme for women aged 20-60 years in Perth and Kinross. Cytopathology. 1990;1(1):3–12. doi: 10.1111/j.1365-2303.1990.tb00320.x. [DOI] [PubMed] [Google Scholar]
- Roworth M., Carter H. Screening for cervical cancer in Fife. Public Health. 1988 Mar;102(2):121–127. doi: 10.1016/s0033-3506(88)80038-6. [DOI] [PubMed] [Google Scholar]
- Waller D., Agass M., Mant D., Coulter A., Fuller A., Jones L. Health checks in general practice: another example of inverse care? BMJ. 1990 Apr 28;300(6732):1115–1118. doi: 10.1136/bmj.300.6732.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]


