Abstract
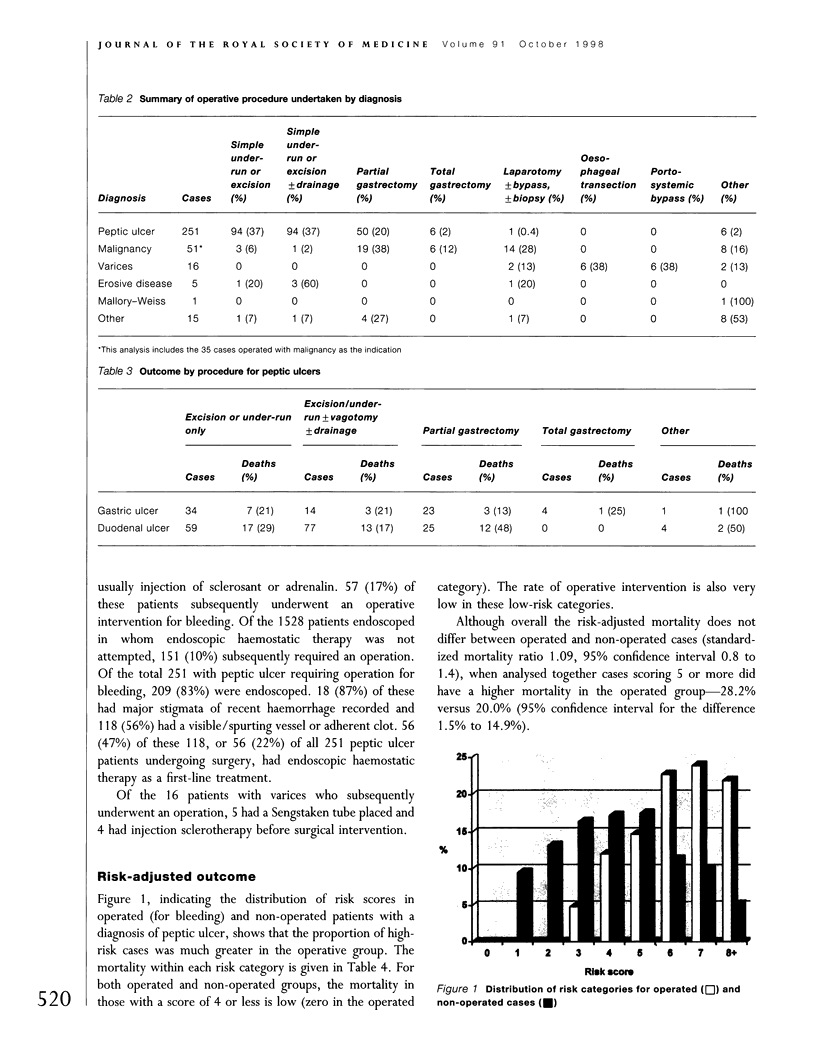
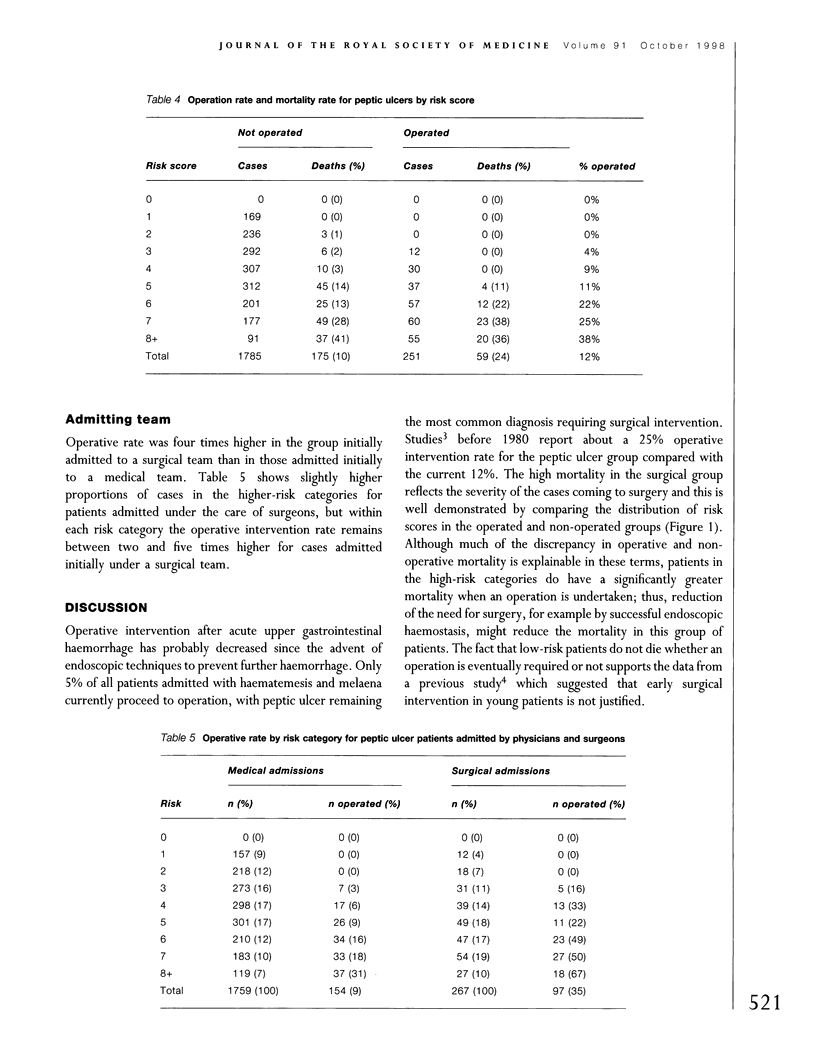
Most patients with acute upper gastrointestinal haemorrhage are managed conservatively or with endoscopic intervention but some ultimately require surgery to arrest the haemorrhage. We have conducted a population-based multicentre prospective observational study of management and outcomes. This paper concerns the subgroup of 307 patients who had an operation because of continued or recurrent haemorrhage or high risk of further bleeding. The principal diagnostic group was those with peptic ulcer. Of 2071 patients with peptic ulcer presenting with acute haemorrhage, 251 (12%) had an operative intervention with a mortality of 24%. In the non-operative group mortality was 10%. The operative intervention rate increased with risk score, ranging from 0% in the lowest risk categories to 38% in the highest. Much of the discrepancy between operative and non-operative mortality was explainable by case mix; however, for high-risk cases mortality was significantly higher in the operated group. In 78% of patients who underwent an operation for bleeding peptic ulcer there had been no previous attempt at endoscopic haemostasis. For patients admitted to surgical units, the operative intervention rate was about four times higher than for those admitted under medical teams. In patients with acute upper gastrointestinal haemorrhage operative intervention is infrequent and largely confined to the highest-risk patients. The continuing high mortality in surgically treated patients is therefore to be expected. The reasons for the low use of endoscopic treatment before surgery are not revealed by this study, but wider use of such treatments might further reduce the operative intervention rate. Physicians and surgeons have not yet reached consensus on who needs surgery and when.
Full text
PDF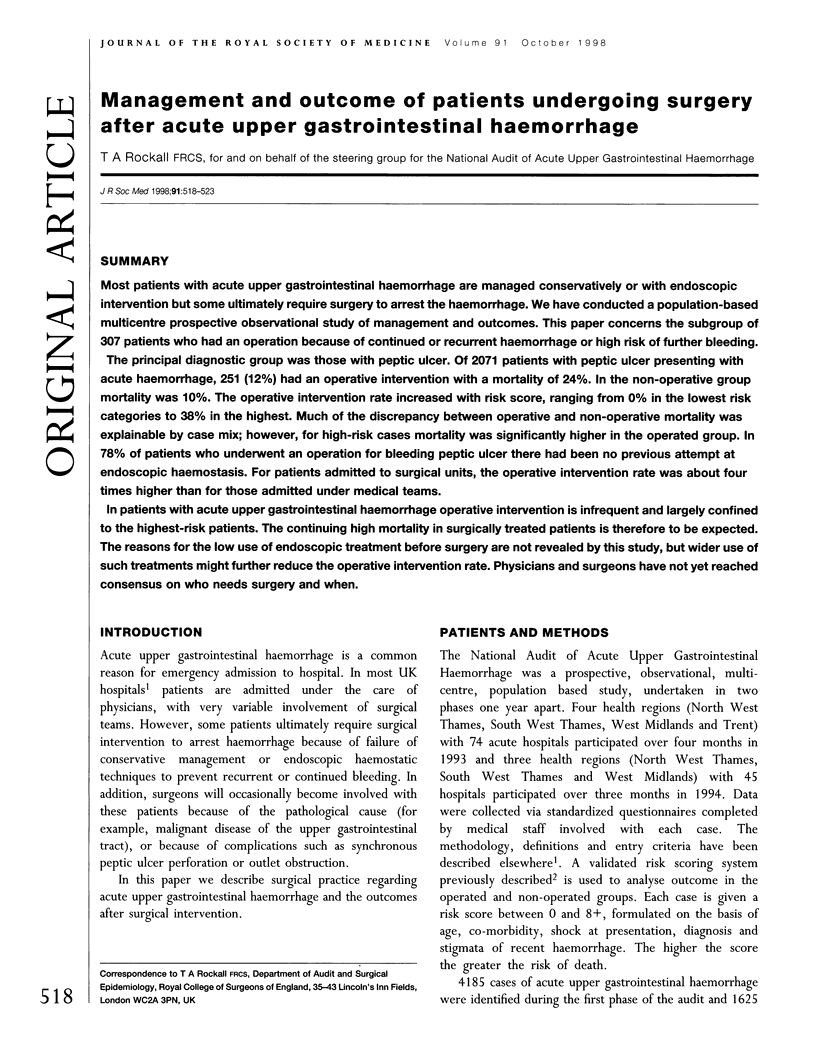

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Guidelines for good practice in and audit of the management of upper gastrointestinal haemorrhage. Report of a joint working group of the British Society of Gastroenterology, the Research Unit of the Royal College of Physicians of London and the Audit Unit of the Royal College of Surgeons of England. J R Coll Physicians Lond. 1992 Jul;26(3):281–289. [PMC free article] [PubMed] [Google Scholar]
- Hunt P. S., Hansky J., Korman M. G. Mortality in patients with haematemesis and melaena: a prospective study. Br Med J. 1979 May 12;1(6173):1238–1240. doi: 10.1136/bmj.1.6173.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden M. V., Griffith G. H. Management of upper gastro-intestinal bleeding in a district general hospital. J R Coll Physicians Lond. 1986 Jul;20(3):212–215. [PMC free article] [PubMed] [Google Scholar]
- Morris D. L., Hawker P. C., Brearley S., Simms M., Dykes P. W., Keighley M. R. Optimal timing of operation for bleeding peptic ulcer: prospective randomised trial. Br Med J (Clin Res Ed) 1984 Apr 28;288(6426):1277–1280. doi: 10.1136/bmj.288.6426.1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockall T. A., Logan R. F., Devlin H. B., Northfield T. C. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ. 1995 Jul 22;311(6999):222–226. doi: 10.1136/bmj.311.6999.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockall T. A., Logan R. F., Devlin H. B., Northfield T. C. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996 Mar;38(3):316–321. doi: 10.1136/gut.38.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks H. S., Chalmers T. C., Blum A. L., Berrier J., Pagano D. Endoscopic hemostasis. An effective therapy for bleeding peptic ulcers. JAMA. 1990 Jul 25;264(4):494–499. doi: 10.1001/jama.264.4.494. [DOI] [PubMed] [Google Scholar]
- Steele R. J. Endoscopic haemostasis for non-variceal upper gastrointestinal haemorrhage. Br J Surg. 1989 Mar;76(3):219–225. doi: 10.1002/bjs.1800760305. [DOI] [PubMed] [Google Scholar]
- Vellacott K. D., Dronfield M. W., Atkinson M., Langman M. J. Comparison of surgical and medical management of bleeding peptic ulcers. Br Med J (Clin Res Ed) 1982 Feb 20;284(6315):548–550. doi: 10.1136/bmj.284.6315.548. [DOI] [PMC free article] [PubMed] [Google Scholar]



