Abstract
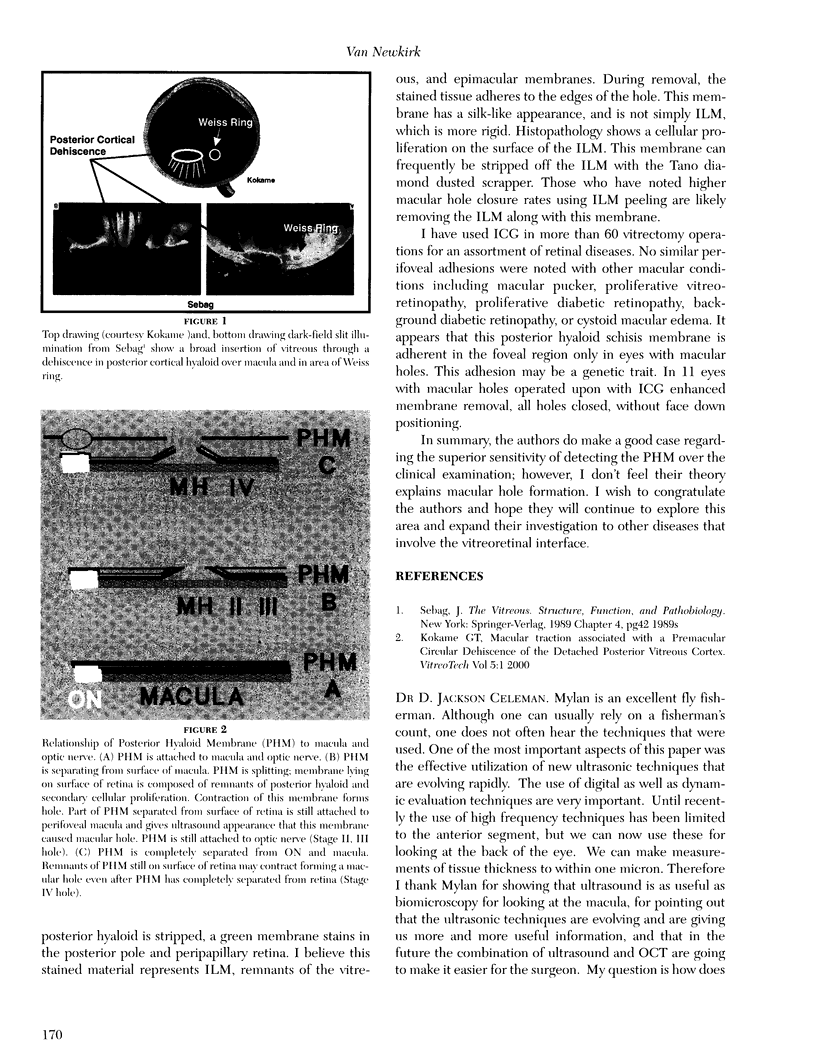
PURPOSE: To prospectively evaluate the relationship between the posterior hyaloid membrane (PHM) and the retina in eyes with idiopathic macular hole. METHODS: Ninety-four eyes of 94 consecutive patients with macular hole underwent complete ophthalmologic examination, contact lens biomicroscopy, and B-scan ultrasonography and/or vitreoretinal surgery. RESULTS: In 93 of 94 patients (99%), the relationship between the PHM and posterior retina could be visualized during echographic examinations or at surgery. Among these 93 patients, the PHM was detectable biomicroscopically in 36 (39%). Persistent PHM attachment to the foveola with partial separation of the PHM from the perifoveal retina was evident with ultrasonography in 5 of 6 patients (83%) with stage 1 hole and in 12 of 18 patients (67%) with stage 2 hole. When axial views were included, separation of the PHM from the perifoveal retina was evident in 13 of 13 patients (100%) with stage 1 and stage 2 hole. Separation of the PHM from the fovea and perifoveal retina with attachment to the peripapillary retina was evident with ultrasonography in 65 of 65 patients (100%) with stage 3 macular hole and pseudo-operculum and was evident biomicroscopically in 22 of the 65 patients (34%) in this group. CONCLUSIONS: These findings suggest that high-resolution axial and paraxial ultrasonographic examination directly on the surface of the eye is more sensitive in detecting separation of the PHM from the retina than biomicroscopy in idiopathic macular holes. The perifoveal detachment of the PHM may be involved in the pathogenesis of macular holes.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chauhan D. S., Antcliff R. J., Rai P. A., Williamson T. H., Marshall J. Papillofoveal traction in macular hole formation: the role of optical coherence tomography. Arch Ophthalmol. 2000 Jan;118(1):32–38. doi: 10.1001/archopht.118.1.32. [DOI] [PubMed] [Google Scholar]
- Fisher Y. L., Slakter J. S., Yannuzzi L. A., Guyer D. R. A prospective natural history study and kinetic ultrasound evaluation of idiopathic macular holes. Ophthalmology. 1994 Jan;101(1):5–11. doi: 10.1016/s0161-6420(94)31356-x. [DOI] [PubMed] [Google Scholar]
- Foos R. Y. Postoral peripheral retinal tears. Ann Ophthalmol. 1974 Jul;6(7):679–687. [PubMed] [Google Scholar]
- Foos R. Y. Ultrastructural features of posterior vitreous detachment. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975 Aug 6;196(2):103–111. doi: 10.1007/BF00414796. [DOI] [PubMed] [Google Scholar]
- Foos R. Y. Vitreoretinal juncture; topographical variations. Invest Ophthalmol. 1972 Oct;11(10):801–808. [PubMed] [Google Scholar]
- Gass J. D. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988 May;106(5):629–639. doi: 10.1001/archopht.1988.01060130683026. [DOI] [PubMed] [Google Scholar]
- Gass J. D. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995 Jun;119(6):752–759. doi: 10.1016/s0002-9394(14)72781-3. [DOI] [PubMed] [Google Scholar]
- Gass J. D., Van Newkirk M. Xanthic scotoma and yellow foveolar shadow caused by a pseudo-operculum after vitreofoveal separation. Retina. 1992;12(3):242–244. doi: 10.1097/00006982-199212030-00007. [DOI] [PubMed] [Google Scholar]
- Gaudric A., Haouchine B., Massin P., Paques M., Blain P., Erginay A. Macular hole formation: new data provided by optical coherence tomography. Arch Ophthalmol. 1999 Jun;117(6):744–751. doi: 10.1001/archopht.117.6.744. [DOI] [PubMed] [Google Scholar]
- Hee M. R., Puliafito C. A., Wong C., Duker J. S., Reichel E., Schuman J. S., Swanson E. A., Fujimoto J. G. Optical coherence tomography of macular holes. Ophthalmology. 1995 May;102(5):748–756. doi: 10.1016/s0161-6420(95)30959-1. [DOI] [PubMed] [Google Scholar]
- Kishi S., Demaria C., Shimizu K. Vitreous cortex remnants at the fovea after spontaneous vitreous detachment. Int Ophthalmol. 1986 Dec;9(4):253–260. doi: 10.1007/BF00137539. [DOI] [PubMed] [Google Scholar]
- Kohno T., Sorgente N., Ishibashi T., Goodnight R., Ryan S. J. Immunofluorescent studies of fibronectin and laminin in the human eye. Invest Ophthalmol Vis Sci. 1987 Mar;28(3):506–514. [PubMed] [Google Scholar]
- Mori K., Abe T., Yoneya S. [Vitreoretinal tomography and foveolar traction in macular hole development and macular pseudohole]. Nippon Ganka Gakkai Zasshi. 1999 May;103(5):371–378. [PubMed] [Google Scholar]
- Russell S. R., Shepherd J. D., Hageman G. S. Distribution of glycoconjugates in the human retinal internal limiting membrane. Invest Ophthalmol Vis Sci. 1991 Jun;32(7):1986–1995. [PubMed] [Google Scholar]
- Sadda S. R., Campochiaro P. A., de Juan E., Jr, Haller J. A., Green W. R. Histopathological features of vitreous removed at macular hole surgery. Arch Ophthalmol. 1999 Apr;117(4):478–484. doi: 10.1001/archopht.117.4.478. [DOI] [PubMed] [Google Scholar]
- Sebag J., Balazs E. A. Human vitreous fibres and vitreoretinal disease. Trans Ophthalmol Soc U K. 1985;104(Pt 2):123–128. [PubMed] [Google Scholar]
- Takahashi M., Trempe C. L., Schepens C. L. Biomicroscopic evaluation and photography of posterior vitreous detachment. Arch Ophthalmol. 1980 Apr;98(4):665–668. doi: 10.1001/archopht.1980.01020030659002. [DOI] [PubMed] [Google Scholar]
- Van Newkirk M. R., Gass J. D., Callanan D., Byrne S. F., Hughes J. R. Follow-up and ultrasonographic examination of patients with macular pseudo-operculum. Am J Ophthalmol. 1994 Jan 15;117(1):13–18. doi: 10.1016/s0002-9394(14)73009-0. [DOI] [PubMed] [Google Scholar]
- Weber-Krause B., Eckardt C. Häufigkeit einer hinteren Glaskörperabhebung im Alter. Ophthalmologe. 1997 Sep;94(9):619–623. doi: 10.1007/s003470050170. [DOI] [PubMed] [Google Scholar]