Abstract
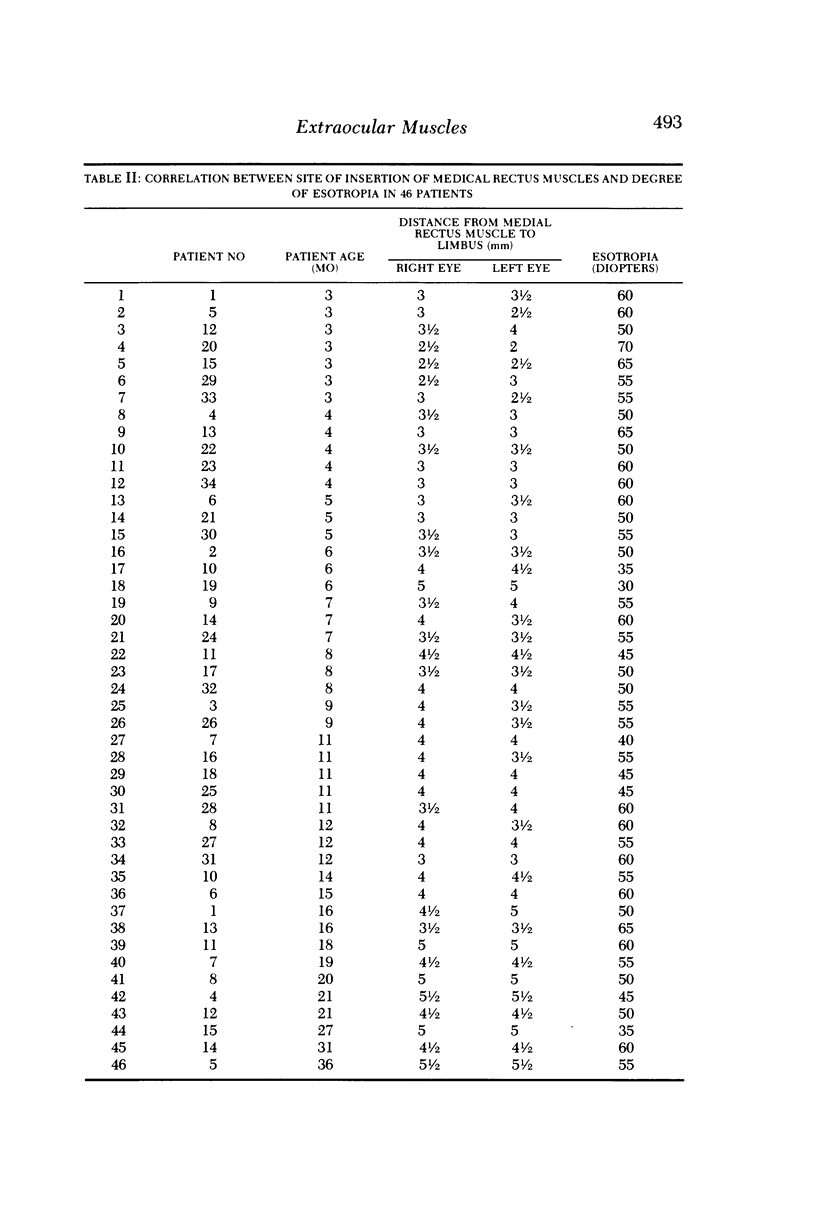
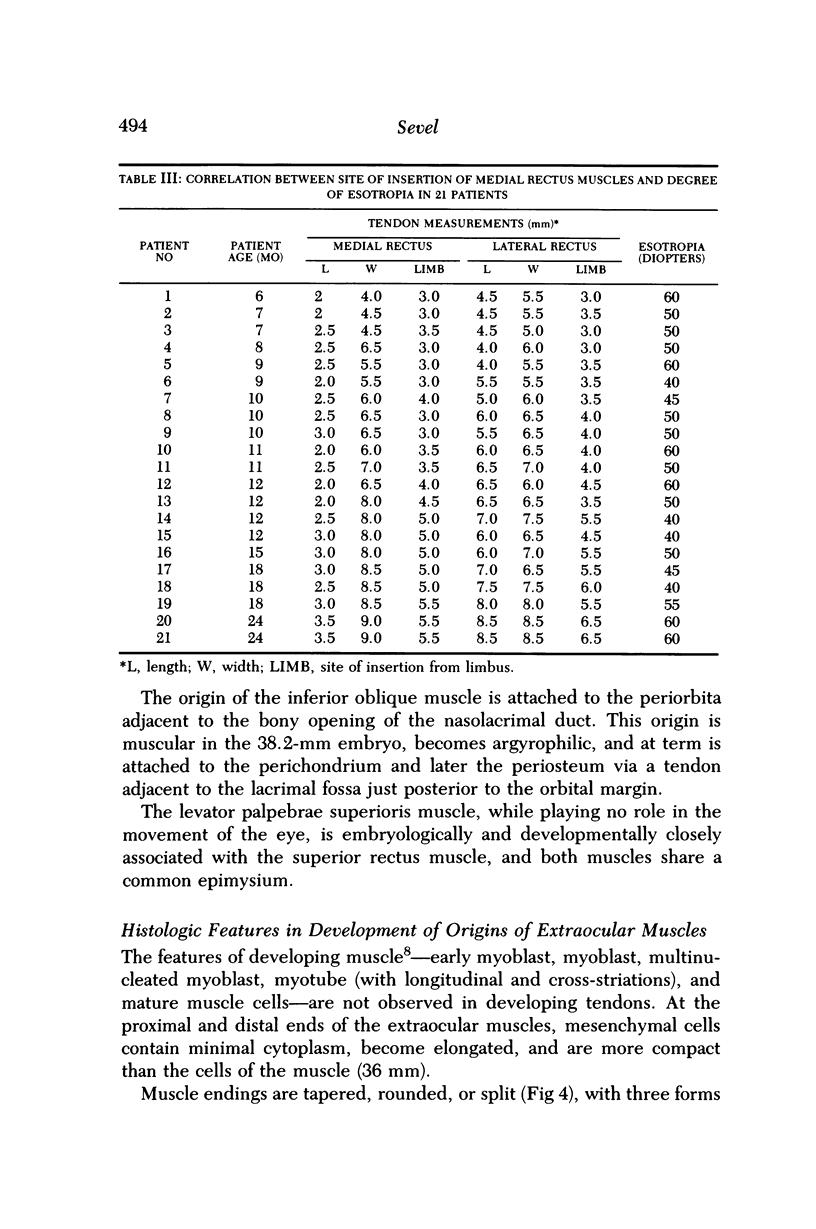
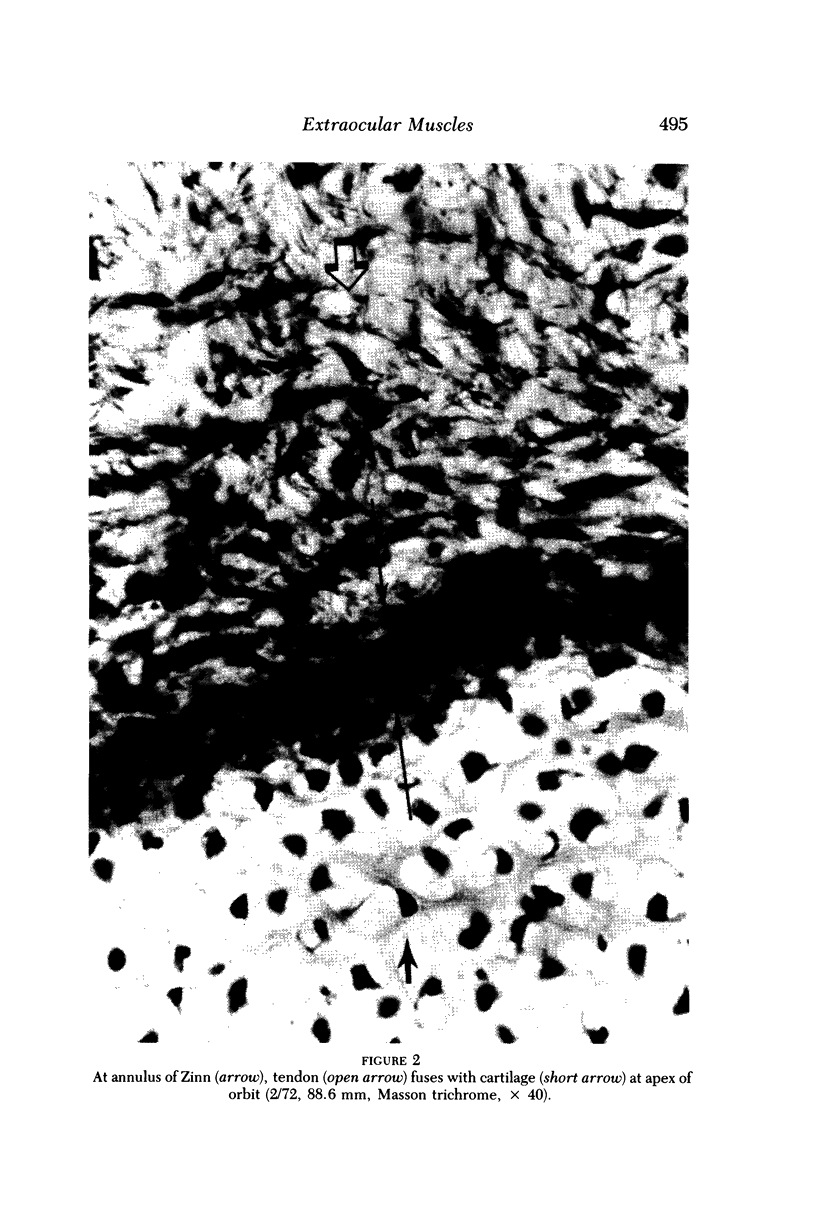
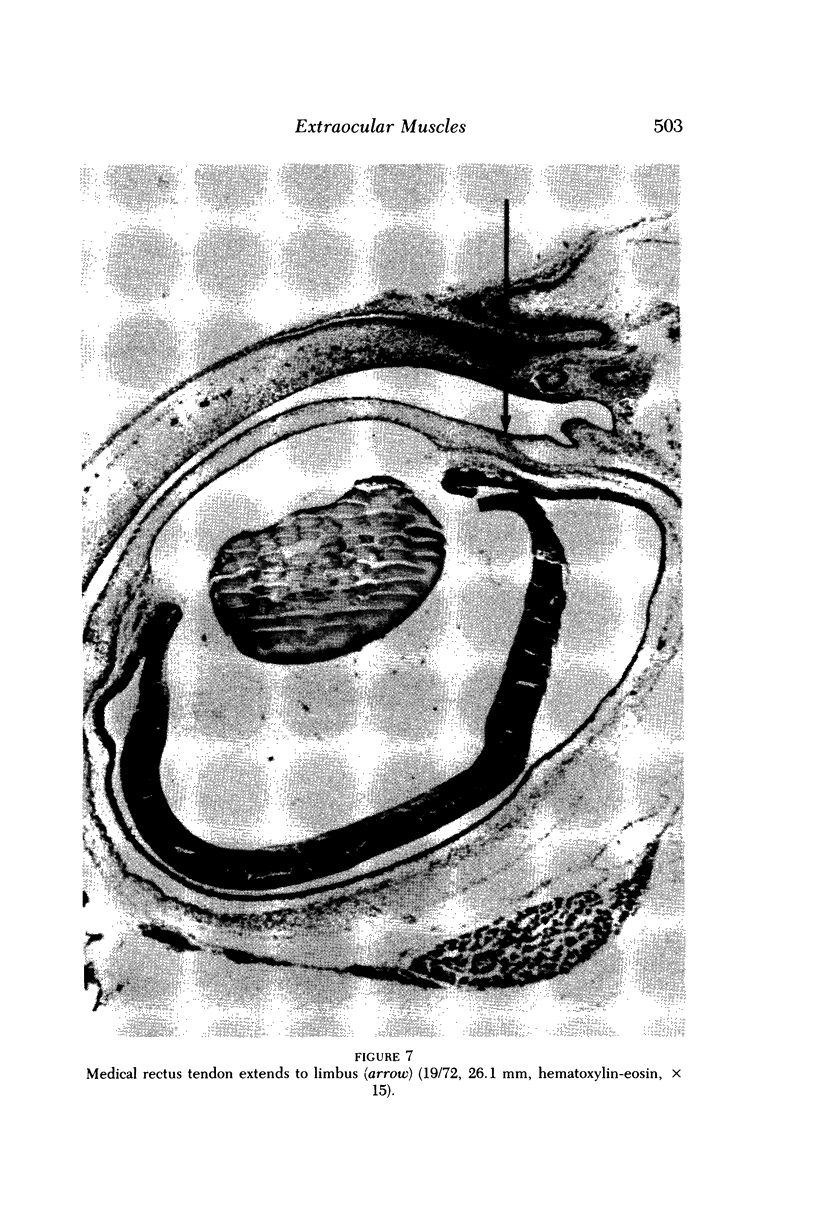
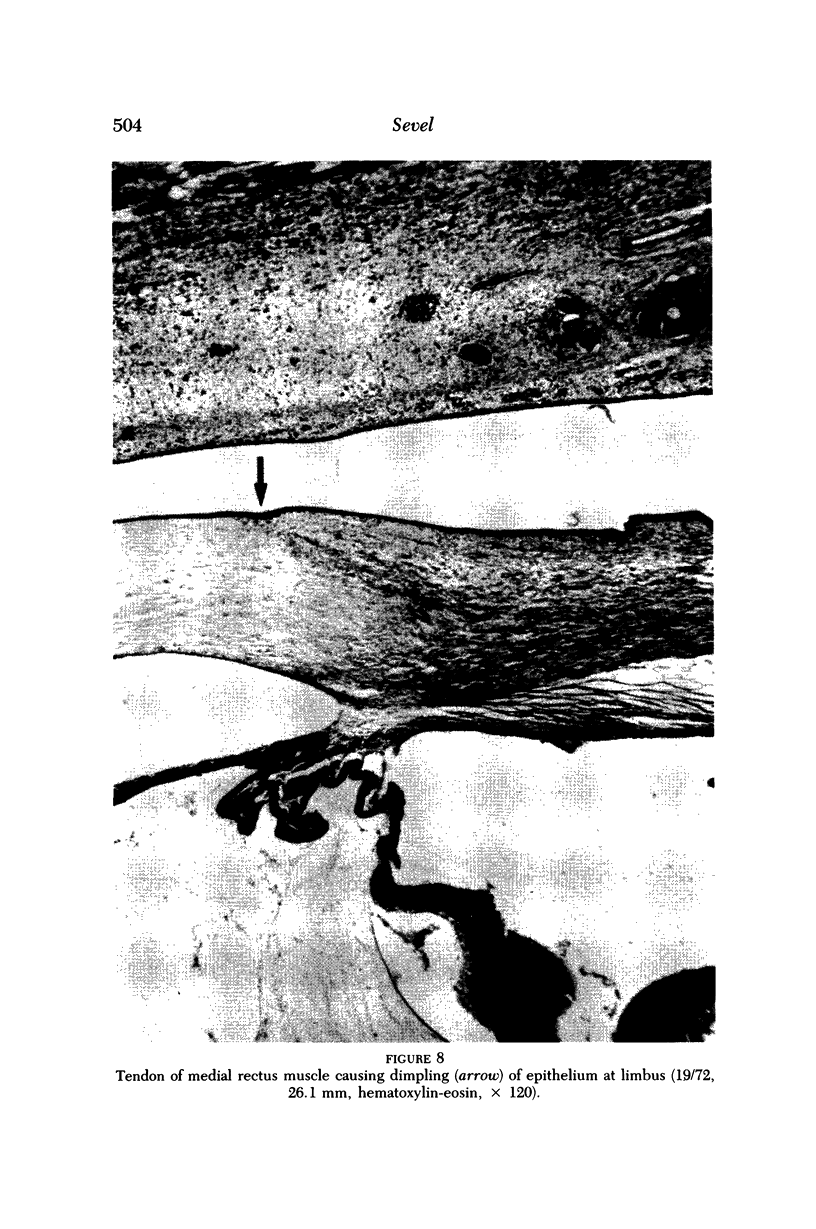
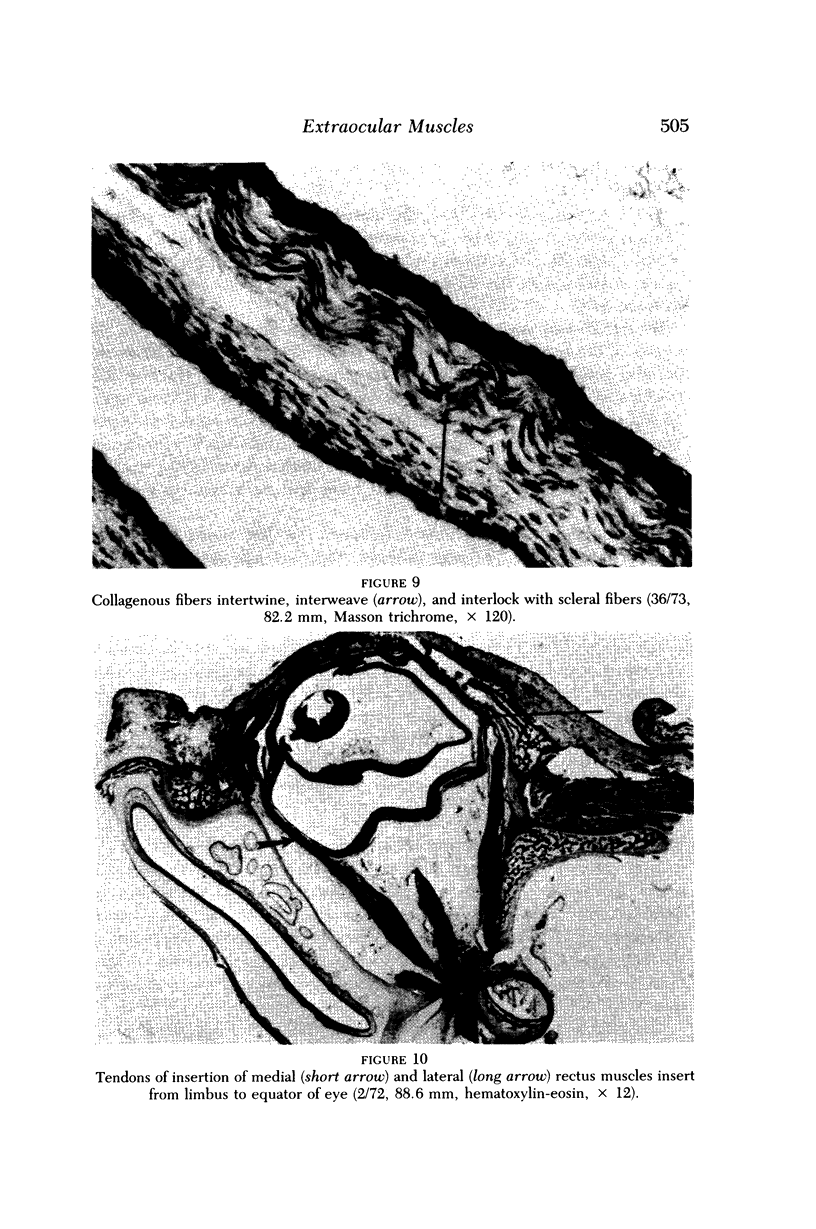
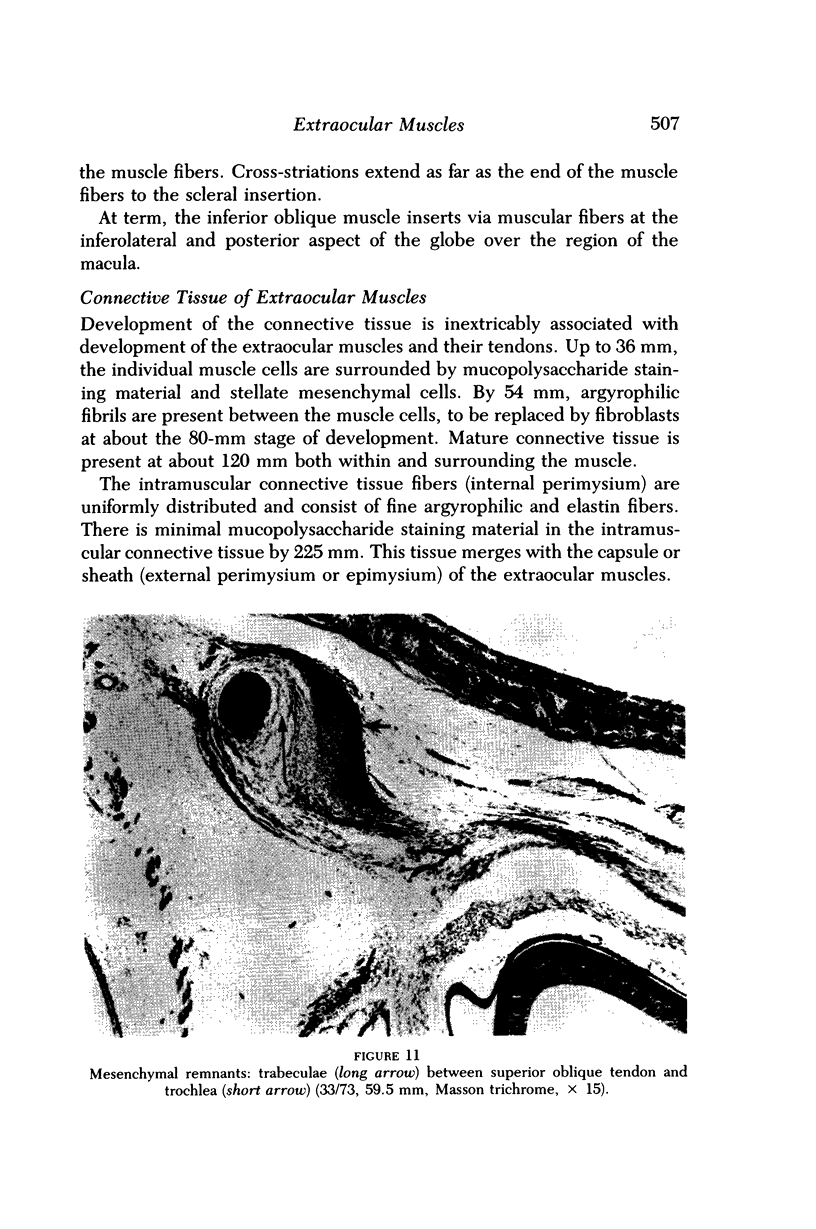
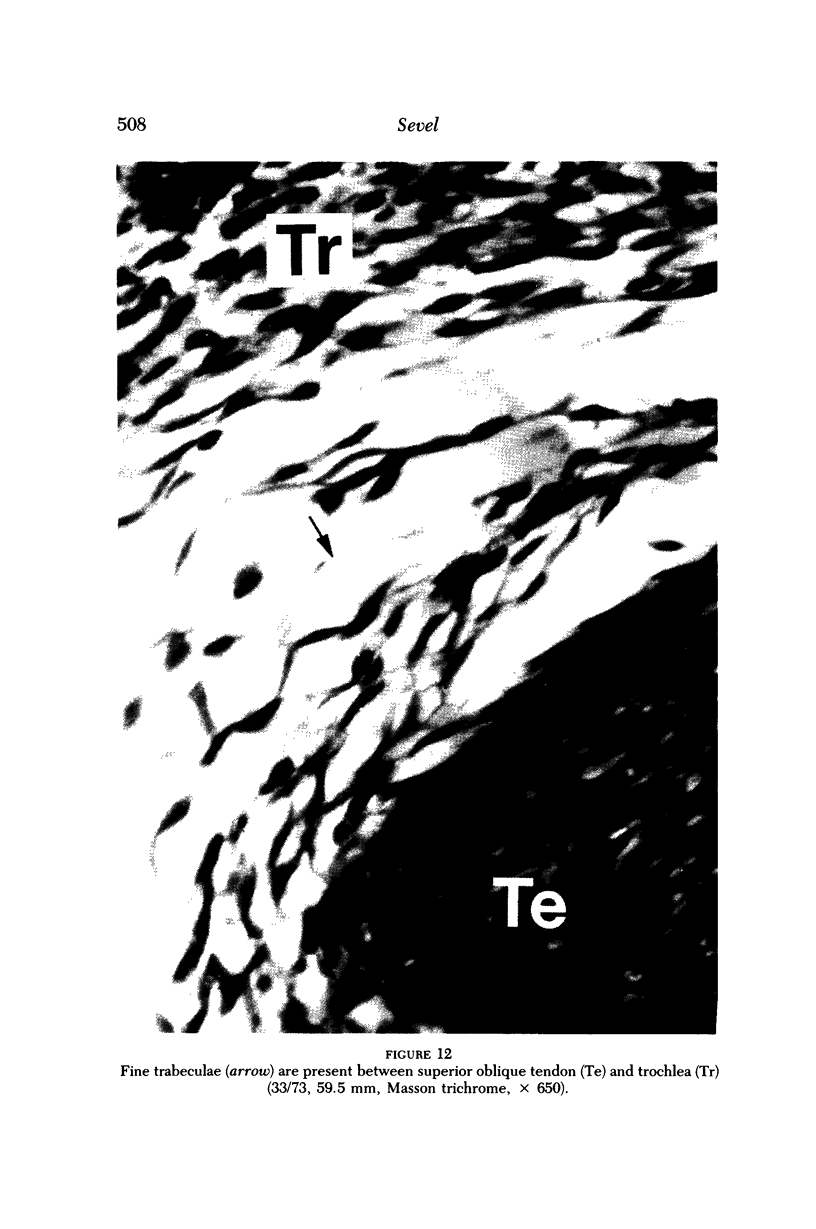
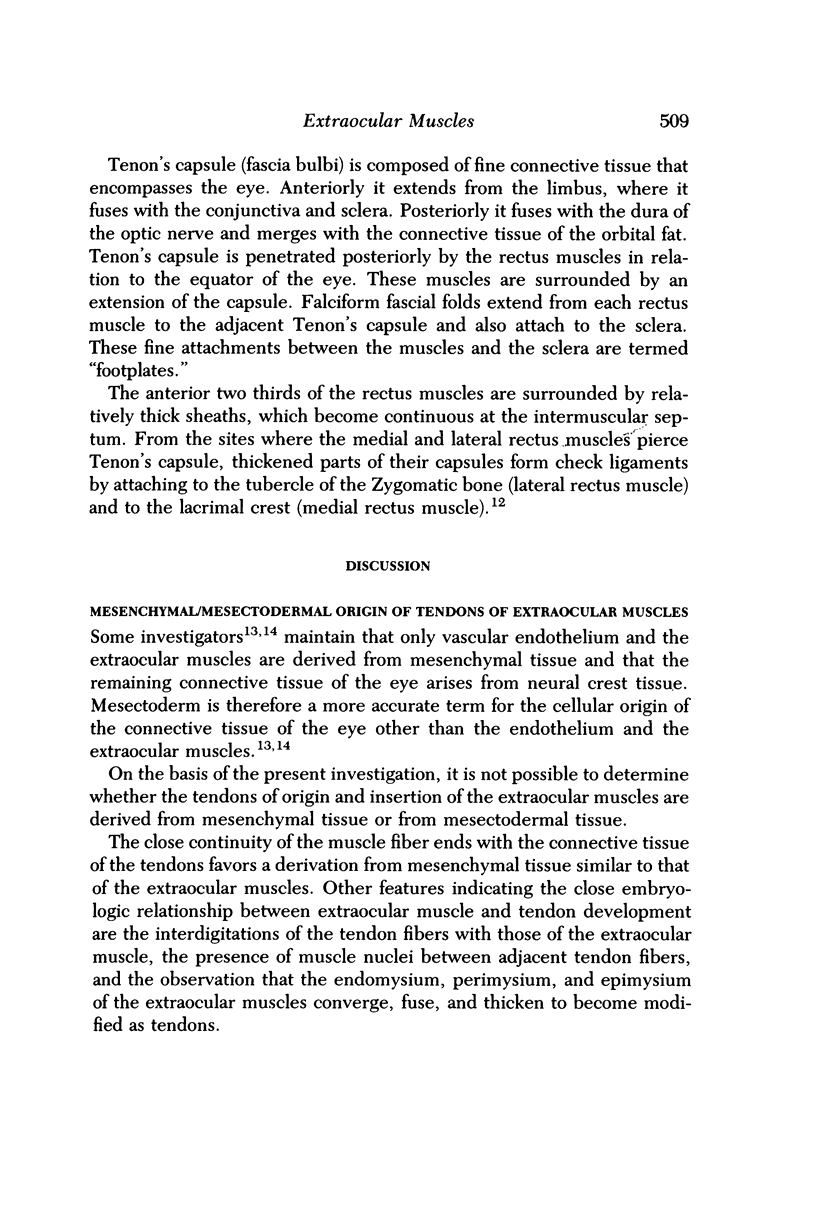
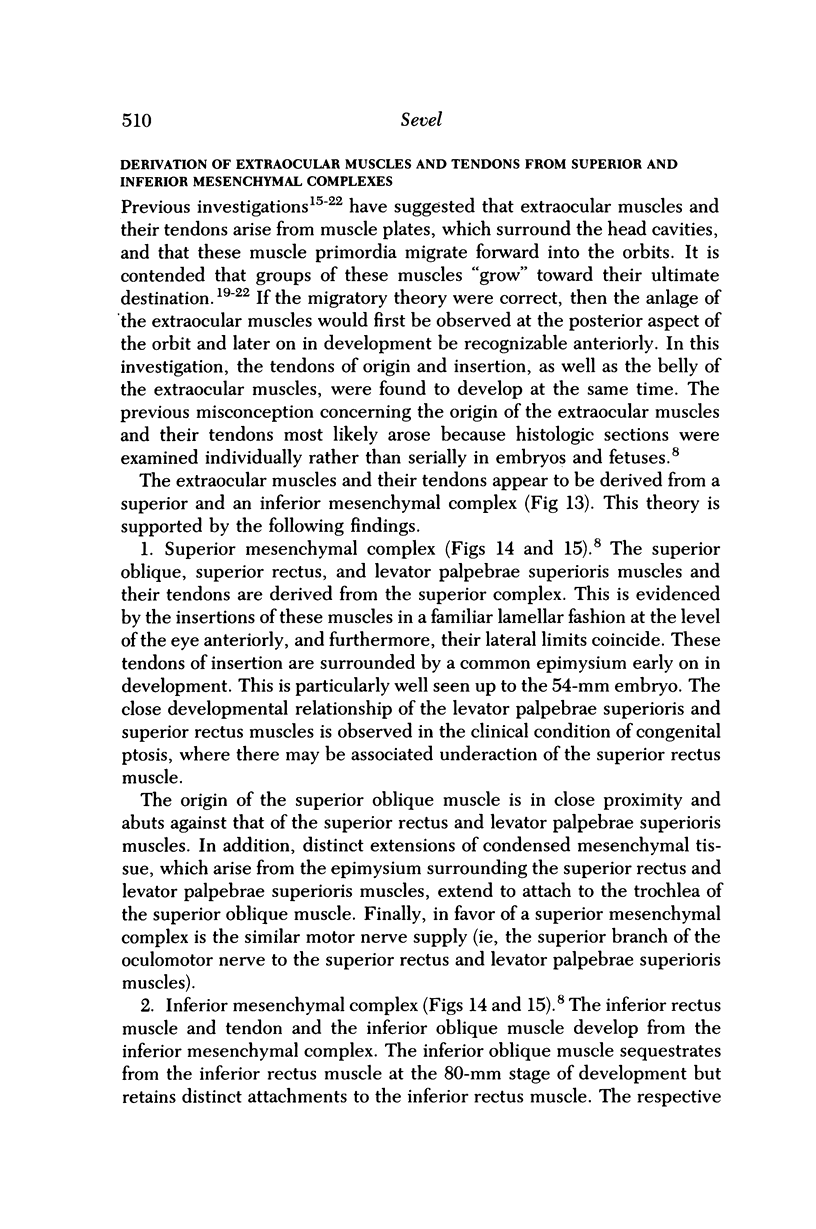
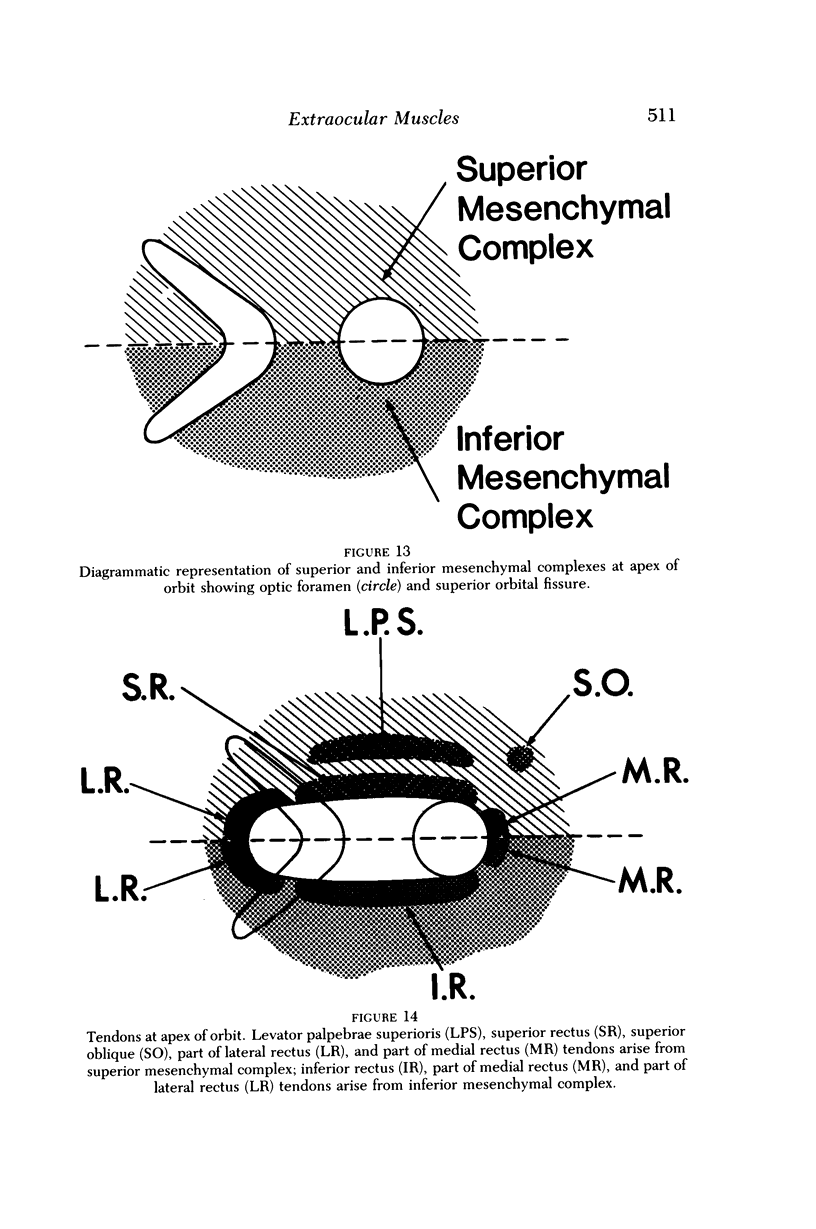
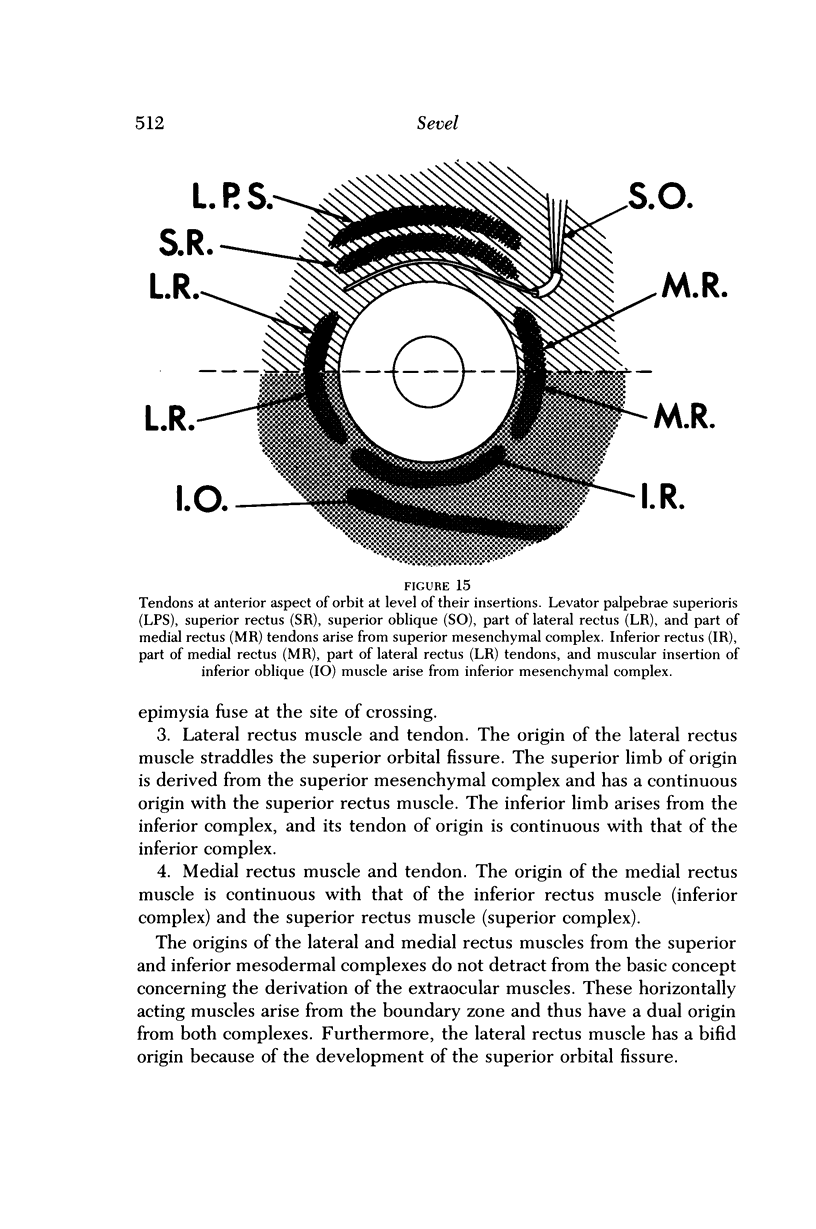
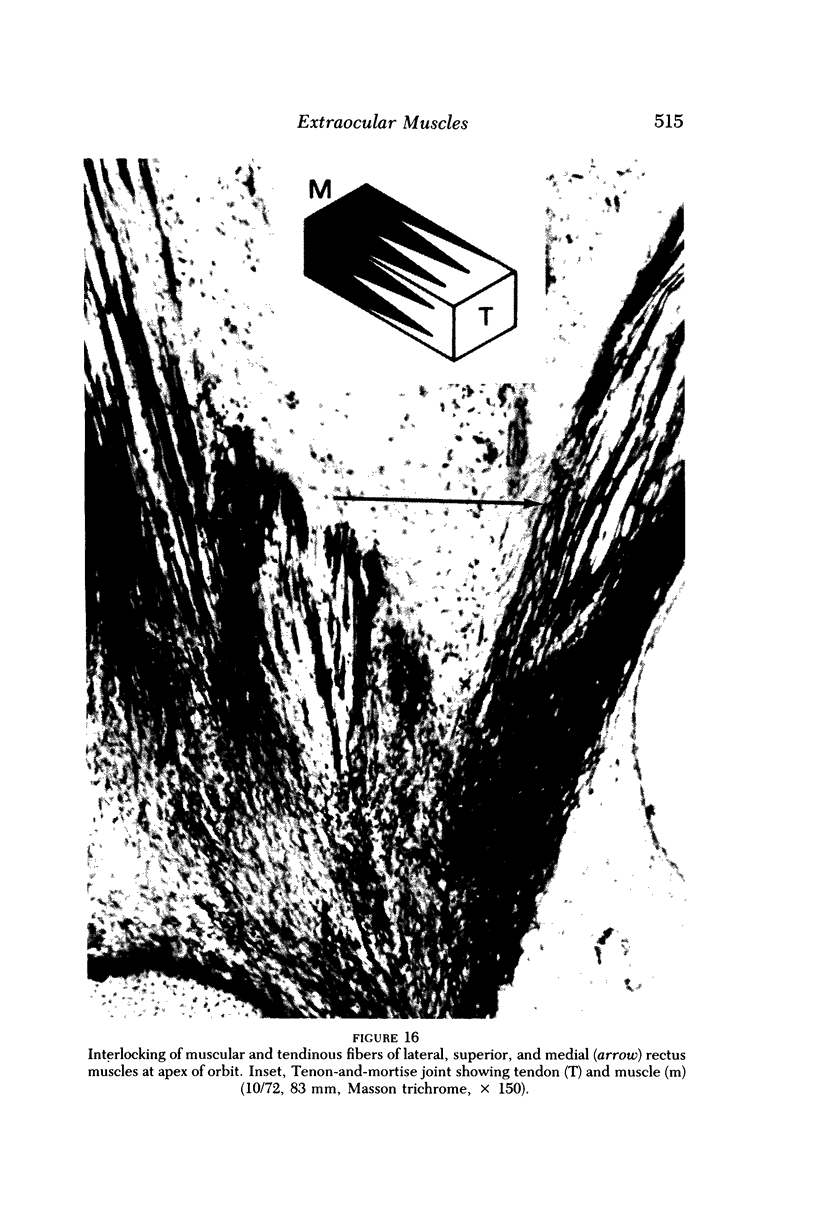
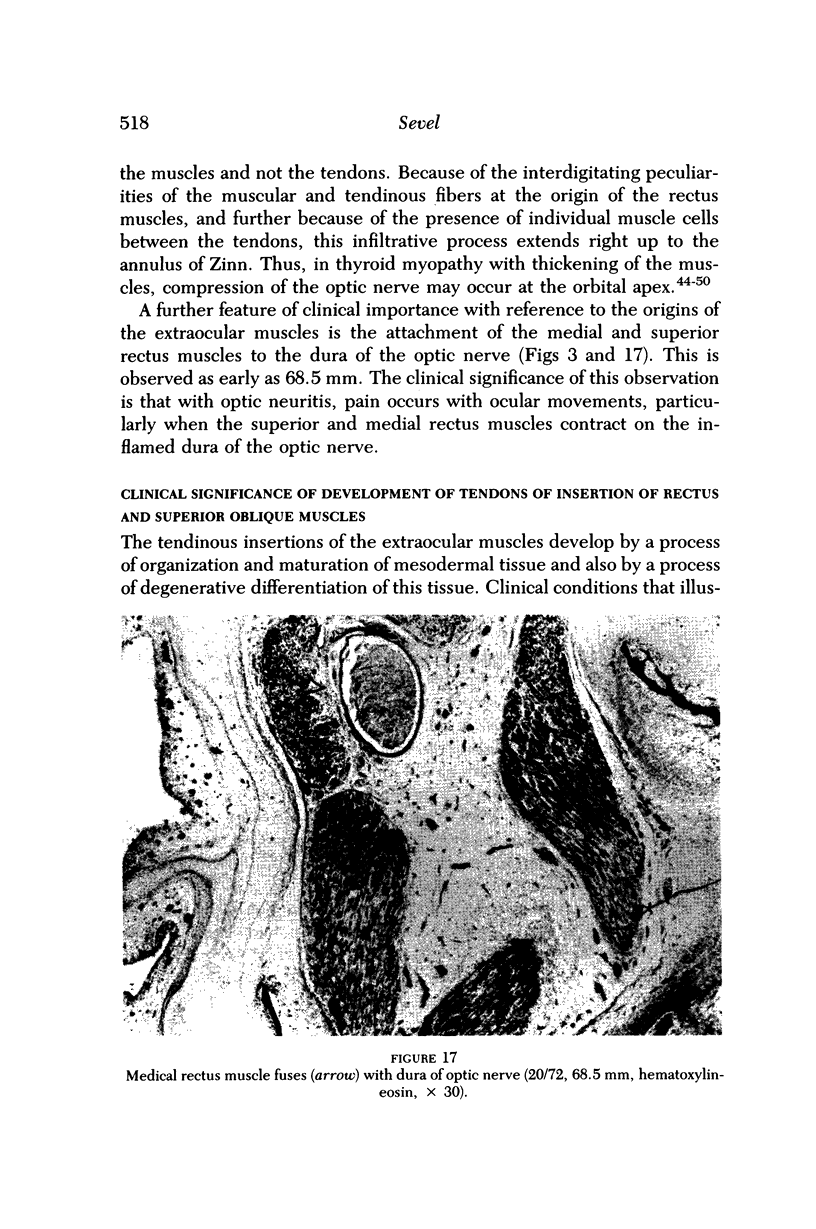
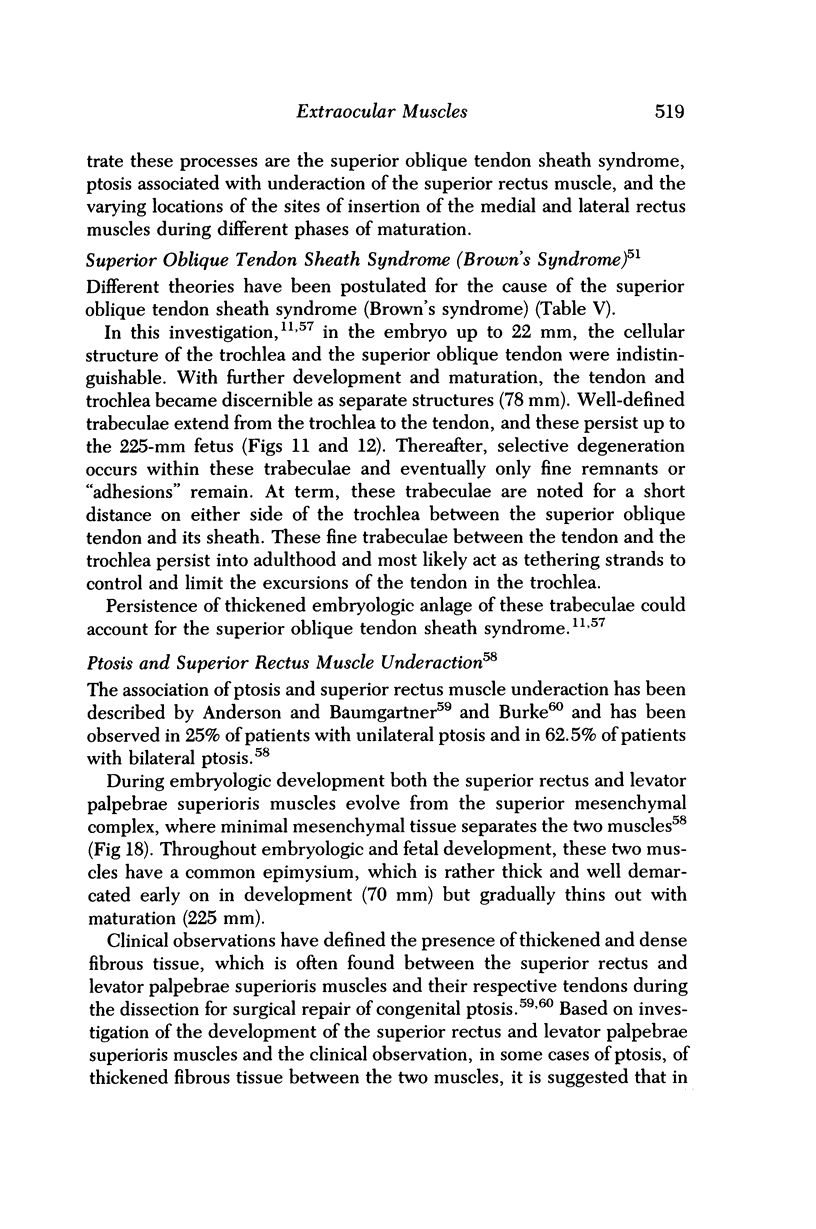
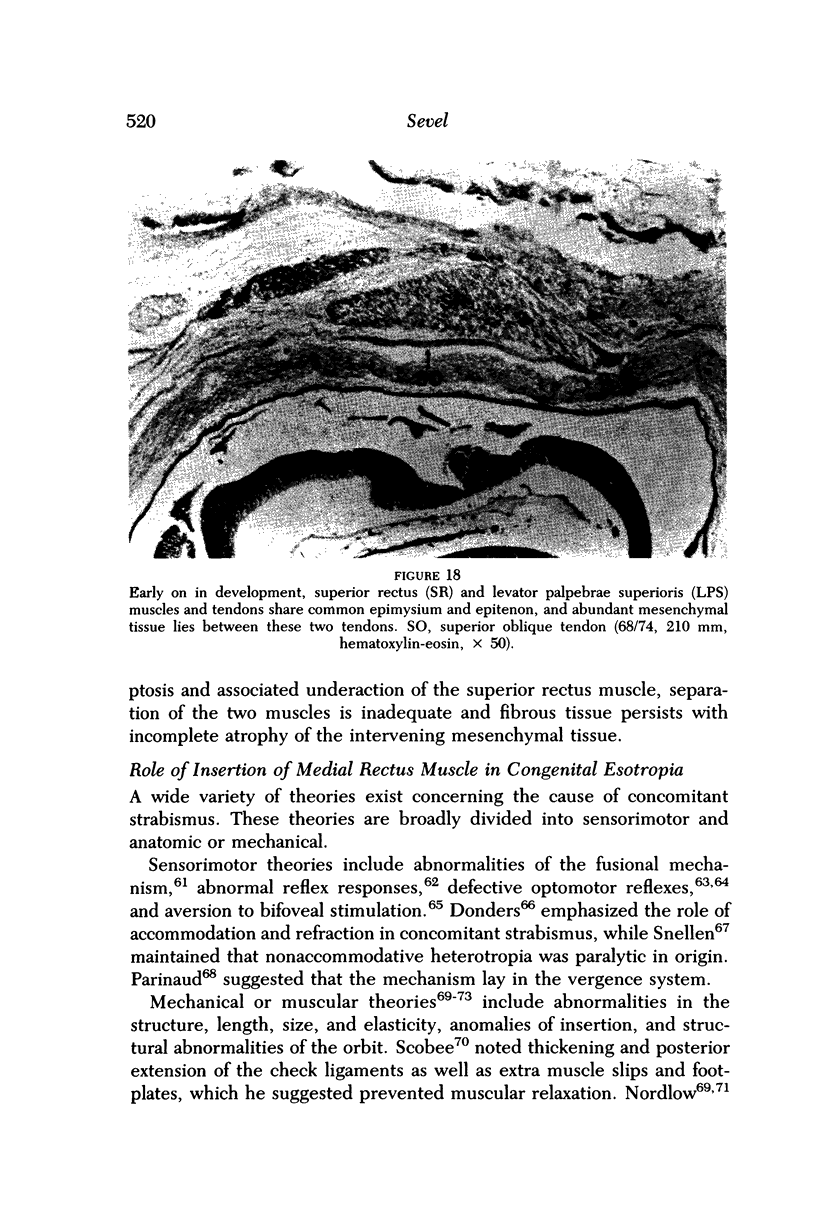
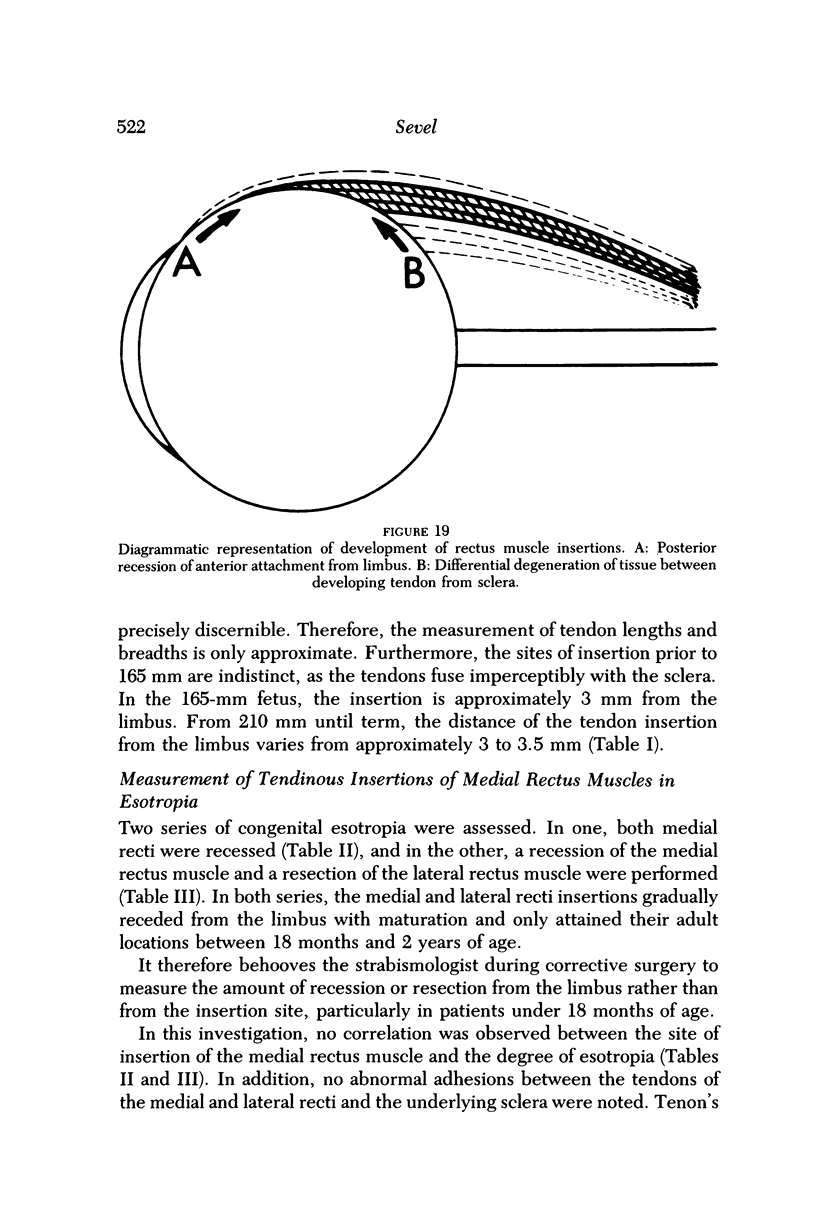
The tendinous origins and insertions of the extraocular muscles were studied embryologically by macroscopic and microscopic methods. It is concluded from this investigation that these tendons of origin and insertion arise from mesenchymal tissue similar to that of their respective muscles. These tendon-muscle groups have developed from superior and inferior mesenchymal complexes. The origins of the extraocular muscles are attached to the periorbita by an interlocking of the tendinous and muscular fibers, which allows for mobility of the extraocular muscles in all extreme directions of gaze and also results in a strong mechanical mooring for these muscles. Avulsion at the origins of the extraocular muscles following severe traction or trauma is rare. The additional origin of the superior and medial rectus muscles to the dura of the optic nerve explains the pain that may occur on movement of the eye in optic neuritis. Optic nerve compression and thyroid myopathy is explained by mucopolysaccharide and inflammatory cell infiltration of the muscular interdigitations that extend up to the site of origin of the rectus muscles. Findings of this investigation suggest that the association of ptosis and superior rectus muscle underaction may be due to a persistence of fibrous tissue that has endured from embryologic development between the superior rectus and levator palpebrae superioris muscles. Superior oblique tendon sheath syndrome is explained by embryologic strands remaining between the tendon of the superior oblique muscle and the trochlea. The insertions of the rectus muscles extend from the equator of the eye to the limbus early on in development. By processes of differential degeneration between the sclera and the rectus tendon, posterior recession of the tendon from the limbus, and contemporaneous growth of the anterior segment of the eye, these tendons reach their adult location only between the ages of 18 months and 2 years. In strabismus surgery, measurements for muscle adjustments should be assessed from the limbus rather than from the sites of insertion of these tendons. In the series of patients with esotropia, no mechanical abnormalities were noted in relationship to the insertions of the medial or lateral recti muscles. Furthermore, no correlation was found between the site of insertion of the medial rectus muscle and the degree of esotropia.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson R. L., Baumgartner S. A. Strabismus in ptosis. Arch Ophthalmol. 1980 Jun;98(6):1062–1067. doi: 10.1001/archopht.1980.01020031052008. [DOI] [PubMed] [Google Scholar]
- Crawford J. S. True Brown syndrome: surgical treatment. Am Orthopt J. 1977;27:15–20. [PubMed] [Google Scholar]
- FINK W. H. The development of the extrinsic muscles of the eye. Am J Ophthalmol. 1953 Jun;36(6 2):10–23. doi: 10.1016/0002-9394(53)90149-4. [DOI] [PubMed] [Google Scholar]
- Goldstein J. H. Strabismus and insertion of horizontal rectus muscles. Am J Ophthalmol. 1969 Oct;68(4):695–698. doi: 10.1016/0002-9394(69)91255-0. [DOI] [PubMed] [Google Scholar]
- HENNEMAN E., OLSON C. B. RELATIONS BETWEEN STRUCTURE AND FUNCTION IN THE DESIGN OF SKELETAL MUSCLES. J Neurophysiol. 1965 May;28:581–598. doi: 10.1152/jn.1965.28.3.581. [DOI] [PubMed] [Google Scholar]
- Hewer E. E. The Development of Muscle in the Human Foetus. J Anat. 1927 Oct;62(Pt 1):72–78. [PMC free article] [PubMed] [Google Scholar]
- Kennerdell J. S., Rosenbaum A. E., El-Hoshy M. H. Apical optic nerve compression of dysthyroid optic neuropathy on computed tomography. Arch Ophthalmol. 1981 May;99(5):807–809. doi: 10.1001/archopht.1981.03930010807002. [DOI] [PubMed] [Google Scholar]
- Le Lièvre C. S., Le Douarin N. M. Mesenchymal derivatives of the neural crest: analysis of chimaeric quail and chick embryos. J Embryol Exp Morphol. 1975 Aug;34(1):125–154. [PubMed] [Google Scholar]
- Mühlendyck H. Wachstum und Länge der äusseren Augenmuskeln. Ber Zusammenkunft Dtsch Ophthalmol Ges. 1978;(75):449–452. [PubMed] [Google Scholar]
- NORDLOW W. Age distribution of the onset of esotropia. Br J Ophthalmol. 1953 Oct;37(10):593–600. doi: 10.1136/bjo.37.10.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks M. M., Brown M. Superior oblique tendon sheath syndrome of Brown. Am J Ophthalmol. 1975 Jan;79(1):82–86. doi: 10.1016/0002-9394(75)90460-2. [DOI] [PubMed] [Google Scholar]
- Reinecke R. D. Superior oblique surgery. Am Orthopt J. 1974;24:23–26. [PubMed] [Google Scholar]
- Sandford-Smith J. H. Intermittent superior oblique tendon sheath syndrome. A case report. Br J Ophthalmol. 1969 Jun;53(6):412–417. doi: 10.1136/bjo.53.6.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevel D. A reappraisal of the origin of human extraocular muscles. Ophthalmology. 1981 Dec;88(12):1330–1338. doi: 10.1016/s0161-6420(81)34856-8. [DOI] [PubMed] [Google Scholar]
- Sevel D. Brown's syndrome - a possible etiology explained embryologically. J Pediatr Ophthalmol Strabismus. 1981 Sep-Oct;18(5):26–31. doi: 10.3928/0191-3913-19810901-09. [DOI] [PubMed] [Google Scholar]
- Stein H. J., Papst W. Elektromyographische Untersuchungen zur Pathogenese und Therapie des Musculus obliquus superior-Sehnenscheidensyndroms (Brown-Syndrom) Ber Zusammenkunft Dtsch Ophthalmol Ges. 1969;69:618–624. [PubMed] [Google Scholar]
- Trobe J. D., Glaser J. S., Laflamme P. Dysthyroid optic neuropathy. Clinical profile and rationale for management. Arch Ophthalmol. 1978 Jul;96(7):1199–1209. doi: 10.1001/archopht.1978.03910060033007. [DOI] [PubMed] [Google Scholar]
- Trobe J. D. Optic nerve involvement in dysthyroidism. Ophthalmology. 1981 Jun;88(6):488–492. doi: 10.1016/s0161-6420(81)34997-5. [DOI] [PubMed] [Google Scholar]
- Trokel S. L., Jakobiec F. A. Correlation of CT scanning and pathologic features of ophthalmic Graves' disease. Ophthalmology. 1981 Jun;88(6):553–564. doi: 10.1016/s0161-6420(81)34993-8. [DOI] [PubMed] [Google Scholar]
- ZEEMAN W. P. Conservative treatment of strabismus. Doc Ophthalmol. 1954;7-8:527–578. doi: 10.1007/BF00238147. [DOI] [PubMed] [Google Scholar]