Abstract
Public health is a complex discipline that has contributed substantially to improving the health of the population. Public health action involves a variety of interventions and methods, many of which are now taken for granted by the general public. The specific focus and nature of public health interventions continue to evolve, but the fundamental principles of public health remain stable. These principles include a focus on the health of the population rather than of individuals; an emphasis on disease prevention rather than treatment; a goal of intervention at all vulnerable points in the causal pathway of disease, injury, or disability; and operation in a governmental rather than a private context. Public health practice occurs at local, state, and federal levels and involves various professional disciplines. Public health principles and practice are illustrated by a case study example of neural tube defects and folic acid. The application of information science and technology in public health practice provides previously unfathomed opportunities to improve the health of the population. Clinical informaticians and others in the health care system are crucial partners in addressing the challenges and opportunities offered by public health informatics.
In this paper, we explain public health as a professional discipline to clinical informaticians. Defining public health presents a challenge, for two different but key reasons. First, public health as a discipline can be difficult to fathom because of the diverse range of problems it addresses and, consequently, the broad scope of activities. Second, many clinicians and other caregivers already have an idea of what public health is about, but that idea is typically limited in scope and is sometimes quite mistaken. At a minimum, it reflects and is constrained by the perspective that is inherent in the nature of clinical work. Yet understanding the discipline of public health is critical for informaticians. Through an understanding of public health and the developing specialty of public health informatics,1 their training, talents, creativity, and experience can be applied in new ways to the fundamental mission of public health—to promote physical and mental health and prevent disease, injury, and disability to realize the vision of healthy people in healthy communities.2
In this paper, we explain the unique perspectives of public health as a discipline, broadly outline and discuss the fundamental nature of public health, present a case study to illustrate and amplify that discussion, and articulate several “grand challenges” for the new and evolving field of public health informatics.
Definition of Public Health
Tip of the Iceberg
Although the public health sector has protected and kept U.S. residents healthy, the majority of Americans have had limited direct exposure to the ways in which public health is practiced. Exposure to the public health system is typically confined to limited activities undertaken by local or state health departments. These activities might include the vaccination of children and the provision of official copies of birth certificates, among others. For years, public health hospitals have been counted among the most visible manifestations of the public health system, serving as “clinical care provider of last resort.” Indeed, many people equate public health solely with providing care to indigent populations. For others, public health involves routine restaurant inspections and investigations of food-borne epidemics in the community. For many clinicians, their primary (and generally one-way) interaction with public health involves submitting notifiable disease reports when they diagnose communicable diseases among their patients.
Certainly, public health agencies are involved in all of these activities. But to understand public health only in these terms is similar to understanding marine biology in terms of shells on the shore. It misses the broader, often invisible aspects of the discipline that have had and continue to have profound salutary effects on human health. For example, the majority of Americans take for granted certain aspects of daily life that exist because of the historical and continuing efforts of the public health sector, such as clean water, safe roads, a protected food supply, and proper disposal of solid and liquid waste.3,4 In addition, many of the fundamental processes of public health (e.g., ongoing disease surveillance, environmental monitoring, and prevention research) generally take place outside the public consciousness, although they are no less important for being invisible.
Shifting Priorities, Multiple Disciplines, Various Roles
Apart from limited exposure to the public health system, the discipline of public health can be difficult to grasp, in part because the focus of public health action has evolved over the past two centuries. This is because the activities of public health are primarily driven by its goal—to improve health and prevent disease, injury, and disability. Thus, as threats to human health vary with time and geography, so too do specific public health projects and efforts. For example, during the 18th and 19th centuries, yellow fever was a great scourge in America. In Philadelphia in 1793, for example, yellow fever killed 5,000 people in only three months—roughly 10 percent of the population.5 Today, this disease is essentially unknown in the United States, and it is not a current focus of public health action.
As progress was made against infectious diseases in the 20th century, the public health community expanded its focus to include other threats to human health (e.g., occupational illnesses, motor vehicle injuries, chronic diseases, exposures to toxic waste and other environmental hazards, interpersonal violence, and suicide).3,4 Of course, new or reemerging infectious disease threats (e.g., AIDS, hantavirus, and drug-resistant tuberculosis) continue to command the attention of public health officials.
Another aspect of public health that makes the concept hard to grasp derives from its varying interventions, which have involved diverse professional disciplines. Many activities—like road and building design, toxic waste disposal, water treatment, school safety, immigrant health, protection of the food supply, even municipal design to promote healthy lifestyles—have been key to promoting health and preventing disease and injury. In addition to nurses, physicians, epidemiologists, and statisticians, the public health system also relies on engineers, social workers, outreach workers, laboratory workers, health communication specialists, sanitarians, environmental specialists, nutritionists, lawyers, legislators, and others to apply efforts that promote health and prevent disease. The public health system comprises allied government, community, professional, voluntary, and academic institutions and organizations that might not be officially termed (or consider themselves) public health agencies. In this paper, we focus on governmental public health agencies.
Finally, public health as a discipline encompasses an amalgam of science, action, research, policy, advocacy, and government. Public health practitioners play each of these roles at different times, but as a professional discipline, public health is not adequately described by any one of them. If public health were simply a scientific enterprise, government function, or any one of the elements listed previously, the concept would be easier to grasp. But public health professionals do wear distinct hats according to the nature of the various threats to community health, the political and social context of the community, and the often incomplete scientific knowledge regarding available preventive interventions. This also makes understanding the extent and nature of public health as a discipline difficult.
Defining Principles and Core Functions of Public Health
Although the focus of public health action and the nature of public health interventions continue to evolve, the fundamental principles of public health remain clear and stable. We previously stated four principles that define, guide, and provide the context for the types of activities and challenges that are undertaken in furtherance of public health.1 These principles derive from the scope and nature of public health itself and tend to distinguish public health from medicine and health care. These four principles can be useful as a guide to those attempting to understand public health.
The primary focus of public health is to promote the health of populations and not the health of specific individuals.
The primary strategy of public health is prevention of disease and injury by altering the conditions or the environment that put populations at risk.
Public health professionals explore the potential for prevention at all vulnerable points in the causal chains leading to disease, injury, or disability; public health activities are not restricted to particular social, behavioral, or environmental contexts.
Public health interventions must reflect the governmental context in which public health is practiced.
With these four principles as guides, public health can be further defined and understood in terms of its core functions. In 1988, the Institute of Medicine (IOM) published The Future of Public Health,6 in which it articulated three activities that ideally comprise the core functions of an effective public health system—assessment, policy development, and assurance. The first core function refers to the assessment and monitoring of the health of communities and populations at risk, to identify health problems and priorities. Policy development involves formulating public policies, in collaboration with community and government leaders, that are designed to solve identified health problems. Assurance refers to the responsibility of the public health system to ensure that all populations have access to appropriate and cost-effective care, including health promotion and disease prevention services, and evaluation of the effectiveness of that care.
Information is central to each of these core functions. For example, the essence of community health assessment is the collection, analysis, interpretation, and communication of data and information. Timely and authoritative information is also central to the informed development of public health policy. Finally, the assurance function described in the IOM report moves public health away from “clinical care provider of last resort” toward the role of monitor and communicator of information about community access to critical health services. Thus, each of these core functions accentuates the importance of public health as information broker, directly underscoring the need for public health officials to be effective planners, developers, and users of health information systems.
People and Facilities
People
The governmental portion of the public health workforce embodies approximately 500,000 professionals, divided among federal, state, and local departments of health.7 As described previously, they practice many professions, including informatics. These public health practitioners operate within the political realities of government organizations and are constrained by limited budgets and inadequate information system resources. Despite these limitations, they are highly committed and dedicated, and their shared motivation is their belief in the power of prevention to ensure community health.
Public health professionals at the federal level frequently specialize or subspecialize in a narrow field, whereas those working on the front lines of public health (e.g., in local health departments) tend to be generalists with more diverse responsibilities. Depending on funding or need, state public health staff fall somewhere between. For example, an epidemiologist working at the Centers for Disease Control and Prevention (CDC) might focus on asthma or on monitoring the incidence and prevalence of asthma. A CDC health educator might develop training materials pertaining to influenza. In contrast, a state health department epidemiologist might focus on prevention of environmental illnesses, or a state health educator might concentrate on all diseases preventable by vaccine. In smaller cities or counties, a single local health department staff person may cover a wide range of programs; the same person might investigate infectious diseases, disseminate information about chronic diseases, manage the Women, Infants, and Children (WIC) and other direct-service programs, and communicate public health concerns to elected officials.
State and local public health staff and others in the health-care system rely on federal experts as a national resource, whereas federal and state public health departments produce much of the research, guidelines, and recommendations that local public health departments implement.
At all levels of public health, staff must build strong community collaboration, solicit and respond to the concerns of the public, and represent public health programs to elected officials.
Public health professionals adopt this challenging work despite liabilities—lack of academic preparation in public health, barriers to ongoing training, and low pay. As of 1997, 78 percent of local health department executives did not have graduate degrees in public health.8 Many state and federal public health executives are appointed by elected officials and are subject to political tides. Nationwide, a state's chief public health executive stays in the job an average of two years.7
Ongoing training is essential in a field as broad and dynamic as public health, but the barriers to accessing needed training are formidable. For professionals practicing in a rural area, travel time to centralized training can be substantial. For instance, a public health professional from Kittson County in Minnesota, who attends a four-hour training session in Minneapolis, will spend approximately 12 hours commuting. Although public health personnel are taking increasing advantage of distance-learning technologies, for a professional to take the time away from daily work for training in the many areas for which highly technical expertise is required might be impossible.
Recruiting and retaining public health staff are also becoming increasingly difficult. The public health agency for Nobles-Rock counties in Minnesota offers a beginning registered nurse $12.54 per hour,9 while the regional hospital in the same town offers registered nurses $16.74 per hour as a starting wage.10 This disparity, more than $8,000 per nurse per year, is exacerbated for information technology professionals and is impossible for even the most fervent believer in the value of public health to ignore. Many agencies report positions that remain unfilled for months or years.
Facilities
Among the 59 U.S. state and territorial health departments and approximately 3,000 county and city health departments, facilities vary widely in size and resources, from new, state-of-the-art buildings to substandard portable trailers. Many outdated, crowded health department buildings are geographically separate from other government offices that have fast Internet connections and technical support.
Public health professionals are challenged to execute their broad responsibilities with limited electronic communication capacity, data systems, and other informatics tools. Examples include the following:
In 1999, an e-mail test message sent to local health departments showed that only 35 percent of the test e-mails were received.
Only 45 percent of the local agencies had the capacity to issue a broadcast facsimile.
Less than 50 percent had continuous high-speed (>56 KB) access to the Internet.7
In March 2001, 41 percent of Minnesota's local public health agencies reported that all managers had desktop access to the Internet; 31 percent reported that all support staff had desktop access; and only 19 percent reported that all professional staff (e.g., nurses, epidemiologists, sanitarians, and health educators) had desktop access to the Internet.11
Public health staff recognize that integrated, computerized information systems and the World Wide Web are critical tools, but these key components of public health infrastructure traditionally have not been funded by grants or new appropriations. Historically, the U. S. Congress has funded public health programs for disease prevention and control (e.g., cancer, tuberculosis, and sexually transmitted diseases), but such program-specific funding provides no incentives for developing integrated systems that would benefit multiple programs. Personnel at local and state health departments, therefore, are required to use distinct, incompatible applications to enter and analyze data; data cannot be easily exchanged, linked, or merged by different programs, or used to evaluate problems by person, across time or geographic area. (Additional discussion of public health informatics challenges appears below.)
Case Study: Neural Tube Defects
Epidemiology, the basic science of public health, is the study of the distribution and determinants of health-related states or events in specified populations and the application of this study to control health problems.12 An analogy heard in a medical school epidemiology course is that a clinician tries to decide what kind of disease a person has, whereas a public health practitioner tries to determine what kind of person has a disease or condition (i.e., what factors can be influenced to prevent that disease or condition). Through this case study, the clinical informatician will understand more about the practice of public health, where the patient is the population.
Public Health Approach to a Problem
The public health approach to a problem is illustrated in Figure 1▶. Public health surveillance is defined generally as the ongoing systematic collection, analysis, and interpretation of health-related data for use in planning, implementing, and evaluating public health practice.13,14 Surveillance is a key data-driven activity of public health and is crucial for the detection and description of problems. After a potential problem is recognized through surveillance, we identify risk factors to determine the cause of the problem. After risk factors have been characterized, we evaluate interventions to decide which ones work most effectively to prevent disease or illness. Subsequently, we implement programs that include such interventions. We then loop back to the beginning, to ongoing surveillance, to determine whether our programs have affected disease incidence.
Figure 1 .
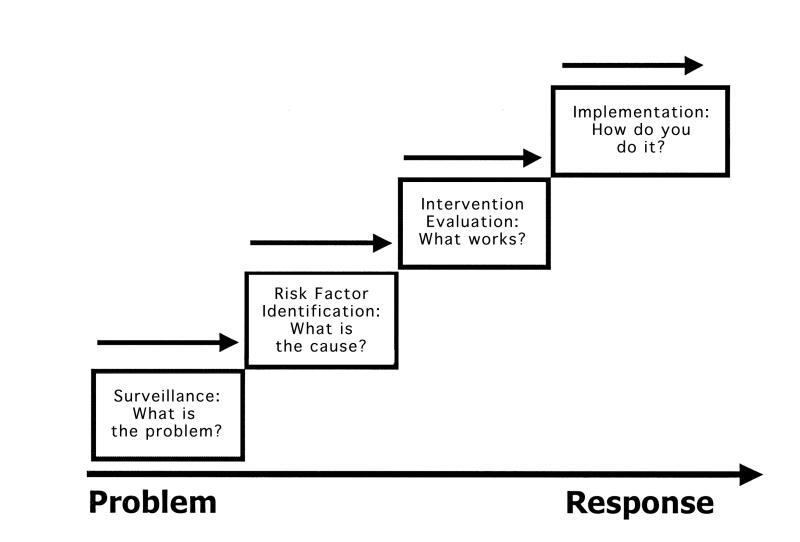
Public health approach. Reproduced from materials used by the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, Atlanta, Georgia.
Not all conditions of interest are under public health surveillance, partly because no single source of data or system contains information for all diseases or conditions of interest. Public health surveillance information systems, like other distributed information systems, are resource-intensive. They use data from various sources, some of which are collected from health care providers, laboratories, or individuals or directly from medical records and birth and death certificates explicitly for surveillance purposes. Decisions about what conditions to monitor are made not by CDC but rather by the state health departments or state legislatures, who might also manage or appropriate specified funds for conducting surveillance activities. Thus, the conditions that are under public health surveillance vary by state.15,16
Factors that influence what conditions are under surveillance in each state include the frequency of disease (i.e., incidence, prevalence, and mortality), the severity (i.e., hospitalization rate, case-fatality rate, years of potential life lost, and disability- and quality-adjusted life-years), the cost of caring for those with the condition, its preventability, its communicability, and the public interest in the condition.14 These criteria for surveillance show why public health officials monitor the occurrence of neural tube defects (NTDs). Neural tube defects affect 1 in every 1,000 pregnancies in the United States, or approximately 4,000 fetuses annually.17 Anencephalic infants are stillborn or die shortly after birth, and although many infants with spina bifida survive, they often suffer from severe lifelong disabilities. The total monetary cost of spina bifida over a lifetime has been calculated as $294,000 per infant (in 1992 dollars).17 It is now known that approximately 50 percent of NTDs can be prevented.18–23
Surveillance: What is the Problem?
A universally available source of data regarding the incidence of NTDs is the birth certificate, which is completed for all live births in the United States. A standardized format is used for birth certificates, the U.S. Standard Certificate of Birth (Figure 2▶), which includes information about the parents, the month prenatal care began, the gestational age and Apgar scores of the infant, the mother's relevant medical and reproductive history, details about the labor and delivery, and check-boxes to indicate whether the newborn has certain congenital anomalies. This latter revision, introduced in 1989,24,25 lists anencephaly and spina bifida first and second, respectively.
Figure 2 .
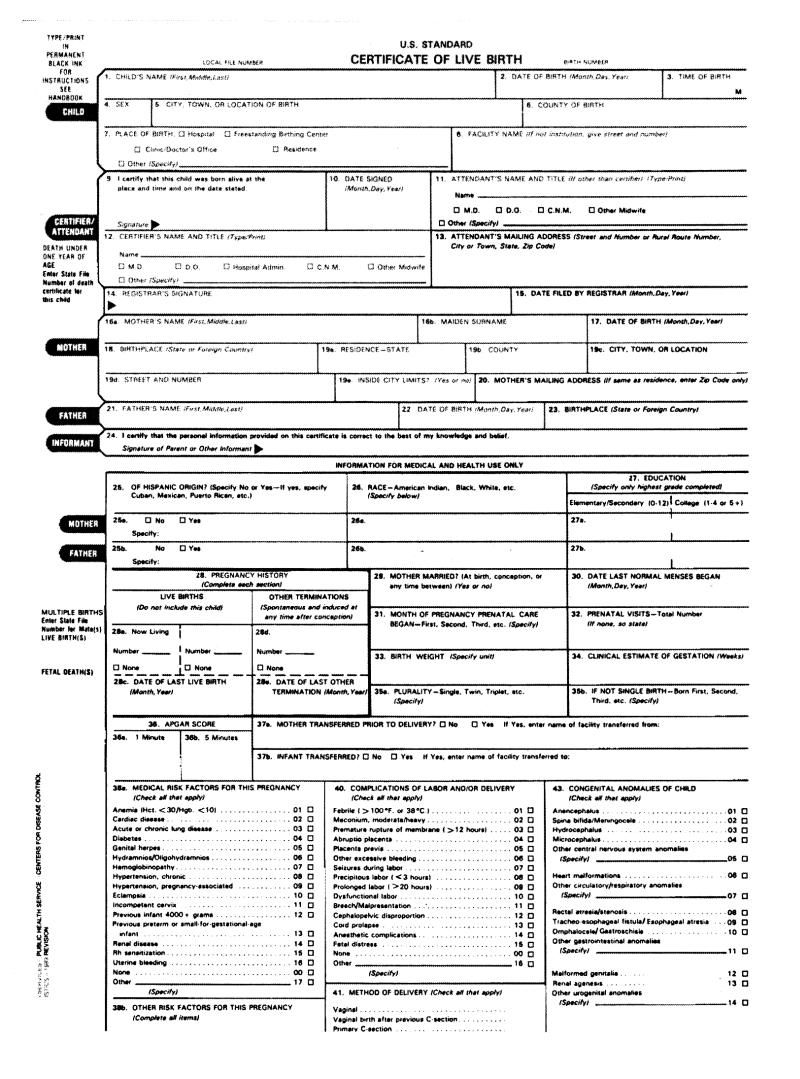
U.S. Standard Certificate of Birth.
As with any other information system, however, birth certificate data have certain limitations. First, timeliness is an issue. A birth certificate generally must be completed, usually by a clerk at the hospital, and filed within five to ten days of birth. The local registrar forwards the information to the state department of health within one to four weeks and states send birth certificate data to the National Center for Health Statistics (NCHS) of CDC anytime, from daily to weekly to monthly. Most states send the data to NCHS within 60 days of birth. Finally, nationwide data are not usually available until a year after the calendar year in which birth occurred.
Second, although the checkboxes for anencephaly and spina bifida appear on the birth certificate, a few states have not consistently required that congenital anomalies be reported.26 Third, even if congenital anomalies are supposed to be reported, they might not be recorded on the birth certificate. The sensitivity of the birth certificate for anencephaly has been documented at approximately 60 percent and for spina bifida at only 40 percent.27,28 Fortunately, given the relative clarity and ease of the diagnosis at birth, the positive predictive value or accuracy of the birth certificate for NTDs approaches 100 percent.27,28
Finally, however, a key limitation of using birth certificates for complete ascertainment or determination of NTDs is that they do not include fetuses that have been miscarried or terminated. Approximately 50 percent of fetuses with NTDs are diagnosed prenatally and aborted.29,30 Thus, in states where detection of all birth defects is a priority, additional resources are invested in gathering data from other sources in addition to the birth certificate.
Approximately 21 states or localities conduct active surveillance for birth defects.31 Active surveillance refers to the increased effort and resources invested by the health department to seek information on a regular basis from sources. Active surveillance, which is initiated primarily by a health department, differs from passive surveillance, which relies on providers to report to the health department.
These birth defects monitoring programs cover various fractions of their population and use various combinations of data sources, which include obstetric offices, prenatal diagnostic centers and laboratories, fetal and neonatal autopsy programs, outpatient perinatal centers, genetic service and other specialty clinics, hospital discharge data and medical records, vital records, ultrasonography records, and neonatal intensive care units; certain ones include passive reports from schools and community agencies. Data from each of these systems are useful for decision making and planning within a jurisdiction, providing information that facilitates understanding the incidence of a problem, the population affected, their rates of prenatal diagnosis and termination and, thus, the most useful points for and types of public health interventions.
Risk Factor Identification: What is the Cause?
Diverse scientific investigations might prove useful to public health officials attempting to identify the etiology or cause of a problem or, at minimum, risk factors that influence the occurrence of a condition. For NTDs, such studies include basic or molecular research into the genetic and biochemical bases of NTDs. They also include clinical research such as that conducted among family planning clinic or prenatal care patients (e.g., case-control or cohort studies to evaluate risk factors and clinical trials to study patient interventions). Naturally, population-based research regarding diet or risk behaviors (e.g., ecologic studies of cultures or nations, state- or communitywide surveys, or case-control studies using cases identified through surveillance) also play a role in the public health understanding of the problem.
Public health officials might also learn more about the cause of a problem during the course of outbreak or cluster investigations. When a cluster of anencephaly occurred along the Texas–Mexico border several years ago,32 public health officials conducted an investigation because of concerns that the outbreak was related to environmental contamination either from the industrial plants along the Mexican border or from pesticide use and that the number of cases was not a statistical anomaly. However, they were unable to identify an etiologic association for this cluster.
Folic Acid and Neural Tube Defects
In July 1991, the British Medical Research Council reported that daily consumption of dietary supplements containing 4 mg of folic acid produced a 72 percent reduction in the recurrence of NTDs.19 The results were so striking that the study was stopped early. This randomized trial supported earlier results by Smithells et al.18 that showed a similar effect with multivitamin supplements containing 0.36 mg of folic acid in a non-randomized intervention among women at high risk (i.e., women with a prior pregnancy resulting in an NTD18).
Officials at CDC determined that this information could prevent NTDs and published a special report in August 199133 that included interim recommendations that women with a history of an infant or fetus with an NTD take 4 mg/day of folic acid, starting when they planned to become pregnant. This amount was 10 times the current recommended daily allowance of folic acid for pregnant women. Given the compelling data from these studies and a sense of urgency about informing the public, this recommendation did not involve CDC's other partner federal agencies, particularly the Food and Drug Administration (FDA). The FDA was apprehensive about safety, about the possibility that taking this amount of folic acid would mask the ability to diagnose vitamin B12 deficiency through blood smears.
Soon after, however, another randomized clinical trial was also stopped early in Hungary after a protective effect was shown for women with no prior history of a pregnancy resulting in an NTD. In the Hungarian study, the women took a multivitamin containing only 0.8mg of folic acid.20 At this point, several studies documented a protective effect of taking folic acid in amounts ranging from 0.1 to 5.0mg.21–23,34 This time, CDC—working with the Office of the Assistant Secretary for Health, FDA, the Health Resources and Services Administration (HRSA), and the National Institutes of Health—developed a statement regarding folic acid for all women.
Thus, in 1992, the U.S. Public Health Service (PHS) recommended that all women consume 0.4 mg folic acid daily.34 The recommended daily consumption was directed at all women, not just women planning to become pregnant, because development and closure of the neural tube takes place within 28 days after conception, before the majority of women know they are pregnant; in addition, approximately 50 per cent of pregnancies in the United States are unplanned.35 The recommendation did not specify how the population might obtain the appropriate amount of folic acid, although it did describe three potential approaches—improvement of dietary habits, fortification of the U.S. food supply, and use of dietary supplements. The report stated that FDA would explore the issue of fortification of the food supply, balancing the goal of increasing folic acid intake with concerns about safety. This process required FDA to participate in federal rule making, which involved obstetric and other medical professionals, the scientific community, consumers, and industry as well as other PHS agencies, underscoring the governmental context of public health actions.
Evaluate Intervention: What Works?
Although science indicated that folic acid was effective in preventing certain NTDs, the question of how to implement effective programs to produce this outcome remained. First was the issue of ensuring that health care providers and consumers were aware of the recommendation, especially the need of women to take folic acid before becoming pregnant. Second, dietary changes are widely acknowledged as difficult to implement, even for a motivated, knowledgeable persons. And above all, the fact that half of pregnancies in this country are unplanned augmented the public health challenge. Clearly, the approach to this problem would have to be multi-pronged.
Implement Program: How Do You Do It?
As in the 1992 recommendation, FDA pursued the option of fortification of the food supply. They published a proposed rule in the Federal Register in 1993 and a final rule in March 1996.36 At that time, fortification was optional; however, the rule required fortification of enriched grain products (e.g., flours and pastas) with 140μg folic acid/100g grain beginning Jan 1, 1998. This action was expected to add 0.1mg of folate to the average person's daily diet and was intended to result in 50 percent of women of reproductive age receiving 0.4mg folate from all sources.37,38 Questions regarding whether more birth defects could be prevented with a larger dose of folic acid remain,39 but FDA wanted to balance this theoretic benefit with concerns about safety and masking vitamin B12 deficiency.
Public health partners working together to disseminate information about folic acid included CDC, FDA, HRSA, and state health agencies, along with obstetric associations and other provider groups, health plans, maternal and child health advocacy groups, public school educators, and community organizations. A CDC publication, “Preventing Neural Tube Birth Defects: A Prevention Model and Resource Guide,” outlines ways to design, develop, deliver, and evaluate an NTD prevention program in a community by using folic acid promotion as a model.40 It includes informational materials targeted at the media, physician's offices, clinics, schools, and even health clubs. In addition, in 1999, CDC, the March of Dimes Birth Defects Foundation, and the National Council on Folic Acid began a national education campaign with materials targeted to women who are thinking about pregnancy, the contemplators, and women who are able to get pregnant even if not planning to in the near future, the non-contemplators. The “Before You Know It” and “Ready, Not” brochures produced for these two groups, respectively, along with other materials, were developed after focus groups were conducted with women who were contemplators and non-contemplators, including Spanish-speaking women from various countries of origin. These materials are readily available in English and Spanish from the CDC Web site and the CDC facsimile information service.
Surveillance: How to Measure Impact?
As with any public health program, continual surveillance to determine whether these programs are having an effect on the incidence of NTDs is essential. However, with delays in the availability of birth certificate data and the utility of assessing more immediately the effects of these programs, evaluation also involves conducting surveillance for outcomes earlier in the causal pathway of disease (▶). Thus, by analyzing the levels of folate in fortified grains, we can measure the effects of the fortification rule on the amount of folic acid in the environment.412
Figure 3 .
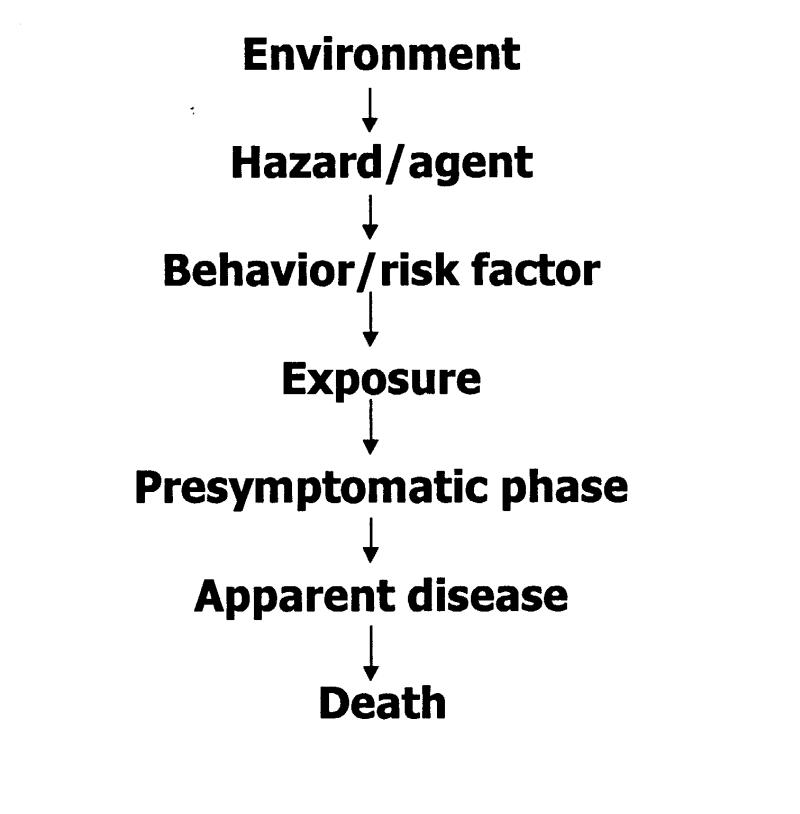
Causal pathway of disease.
To estimate the effects of education campaigns, CDC partnered with the March of Dimes to survey women about their awareness of folic acid and its role in preventing birth defects. Folic acid awareness increased from 52 percent in 1995 to 75 percent in 2000, and the women surveyed also reported an increase in consumption of vitamins containing folic acid, from 28 percent in 1995 to 34 percent in 2000.42,43
We might also enumerate sales of folic acid–containing vitamins to discern whether behavior has changed. Results from the National Health and Nutrition Examination Survey (NHANES), conducted periodically by NCHS, provide another gauge of the increase in folic acid intake among women. Analysis of blood samples from NHANES 1999 demonstrated a substantial increase in serum and red blood cell folate concentrations among women between 1 and 44 years of age after folic acid fortification (Figure 4▶).44 A similar increase in serum folate levels among clinical specimens from men and women supports the hypothesis that folic acid fortification and not dietary supplements might be contributing to this trend.45,46
Figure 4 .
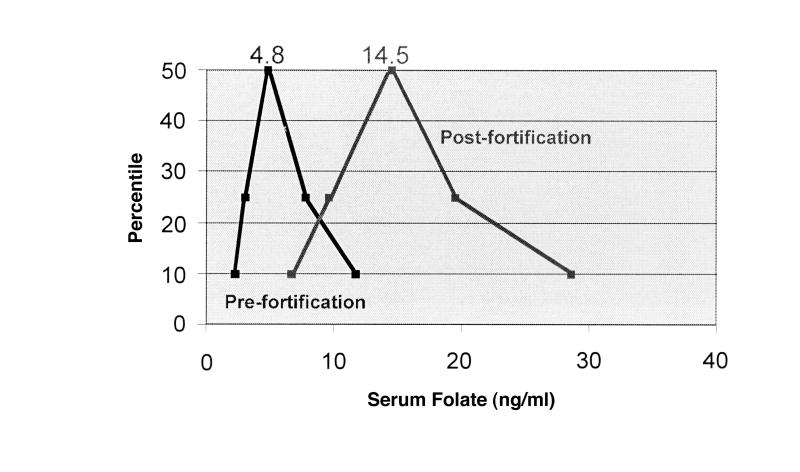
Median serum folate concentrations among non-pregnant women between 15 and 44 years of age, from the National Health and Nutrition Examination Survey (NHANES) III, conducted 1988 to 1994.
Folic acid fortification might be having its intended effect on the incidence of NTDs. An analysis of birth certificate data through 1999 shows that the birth prevalence of NTDs decreased from 37.8 per 100,000 live births before fortification to 30.5 per 100,000 live births after fortification, a 19 percent decline (Figure 5▶).26Analysis of data regarding births to women who received only third-trimester or no prenatal care, and thus could not have terminated a pregnancy with an NTD, demonstrates a similar decline (Figure 6▶).26Data from the Metropolitan Atlanta Congenital Defects Program, which includes prenatally diagnosed cases, also exhibit a decline (Figure 7▶). Factors other than folic acid fortification (e.g., increased vitamin supplementation) may also have contributed to this decline; public health officials will continue to monitor the occurrence of NTDs to further evaluate the effects of these public health interventions.
Figure 5 .
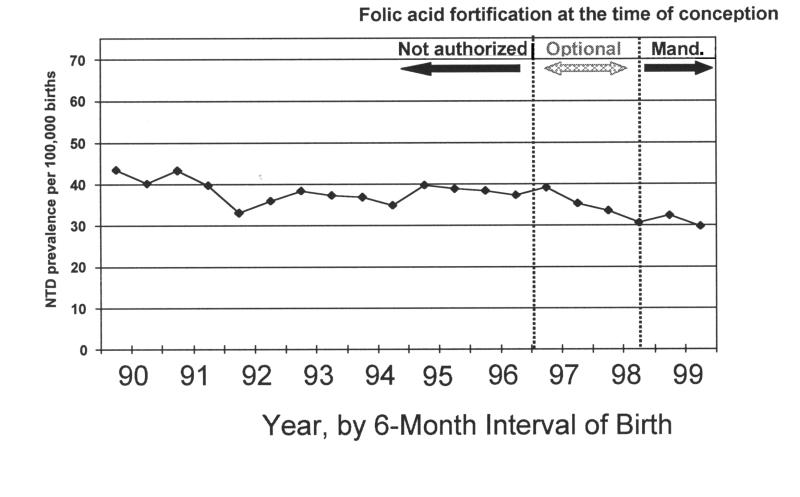
Trends in total neural tube defects (anencephaly and spina bifida) among all births, 1990–1999, for 45 U.S. states and Washington, DC. source: National Center for Health Statistics Vital Statistics Data. Adapted from Honein et al.26
Figure 6 .
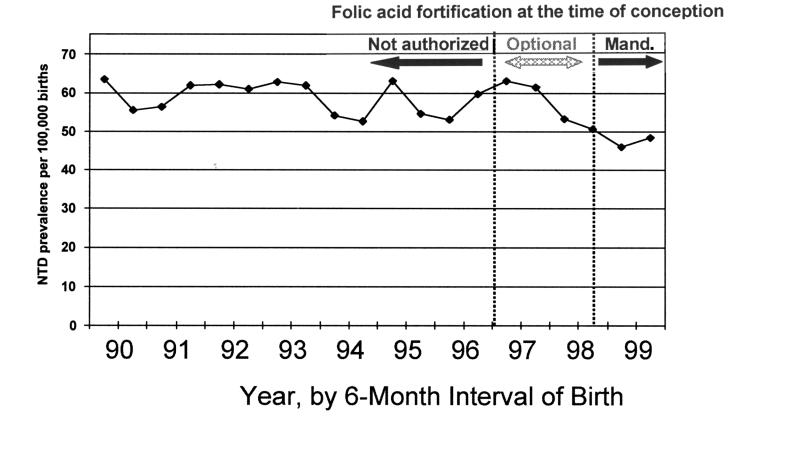
Trends in total neural tube defects (anencephaly and spina bifida) among births to women who received no prenatal care or prenatal care in the third trimester only, 1990–1999, for 45 U.S. states and Washington, DC. source: National Center for Health Statistics, Vital Statistics Data. Adapted from Honein et al.26
Figure 7 .
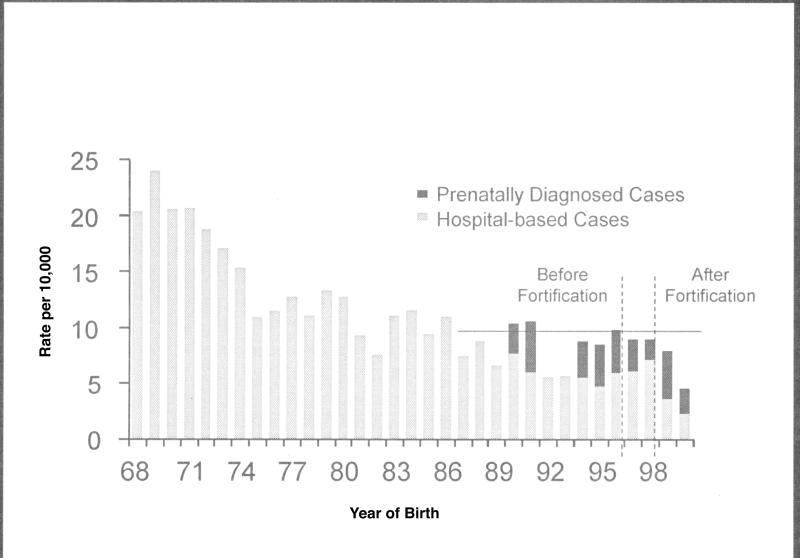
Prevalence of anencephaly and spina bifida, Metropolitan Atlanta Congenital Defects Program, 1968– 2000. Dark bars indicate prenatally diagnosed cases; light bars, hospital-based cases, which include both liveborn and stillborn infants.
Grand Challenges of Public Health Informatics
As might be expected from the public health principles described above and illustrated by the case study, the nature of public health also defines a special set of informatics application challenges. For example, to assess the health and risk status of a a population, data must be obtained from multiple disparate sources (e.g., hospitals, social service agencies, police, departments of labor and industry, population surveys, and on-site inspections). Data about particular individuals from these sources must be accurately combined, then individual-level data must be compiled into usable, aggregate forms at the population level. This information must be presented in clear and compelling ways to legislators and other policymakers, scientists, advocacy groups, and the public while ensuring the confidentiality of the health information of specific individuals.
Although information science and technology can improve public health practice in various ways, three areas represent grand challenges for public health informatics—developing coherent, integrated national public health information systems, developing closer integration of public health and clinical care, and addressing pervasive concerns about the effects of information technology on confidentiality and privacy.
One goal of public health informatics is ensuring the capacity to assess community problems in a comprehensive manner through the development of integrated nationwide public health data systems. This will require a clear definition of public health data needs and the sources of these data, consensus on data and communication standards—to facilitate data quality, comparability, and exchange—with policies to support data sharing and mechanisms and tools for accessing and disseminating data and information in a useful manner. Because electronic reporting will increasingly form the basis for surveillance systems, developmental efforts must also address such concerns as unambiguously defining the specific medical conditions that trigger automated data transmissions, working with reporting organizations to ensure that they have appropriate software and electronic communication capabilities, and ensuring that adequate capacity exists for analysis of the increased volumes of public health data that are anticipated.
A second challenge for public health informatics is facilitating the improved exchange of information between public health and clinical care. Much of the data in public health information systems comes from forms that are filled out by hand and later computer-coded. Even where reporting is electronic, initial data entry is typically manual. This results in serious under-reporting of many reportable diseases and conditions.49–52
Data should flow automatically to public health from clinical and laboratory information systems. When these data are appropriately compiled by public health information systems, they should allow rapid and accurate assessments and disease control responses, as well as the formulation of improved clinical guidelines and interventions. Conversely, automated presentation to clinicians of prevention guidelines has been shown to improve clinical care, and there are other ways in which the skills and activities of the public health community (e.g., community outreach) could benefit clinical care. Electronic information sharing and data exchange provide the means by which we can better integrate public health and clinical care activities, but creativity and hard work are needed to take full advantage of these opportunities.
Finally, privacy, confidentiality, and security are pervasive and persistent challenges to progress in public health informatics. Information systems are correctly perceived by the public as being a double-edged sword: Whatever is done to make integrated, comprehensive information more easily available for laudable and worthwhile purposes must of necessity create new opportunities for misuse. Public health often collects extremely sensitive personal medical information that has the potential for tremendous harm if improperly disclosed. Federal legislation that provides a fair and workable balance between individual privacy and the common good is needed to reassure the public and establish legal guidelines for handling sensitive information.
The Health Insurance Portability and Accountability Act (HIPAA) of 1996 will result in both privacy and security standards for all health plans (including Medicare and Medicaid), clearinghouses, and providers who use electronic data. Public health has had an excellent record of information protection in the past; the recently published HIPAA Privacy Rule continues to permit disclosure of protected health information to public health authorities for public health activities.53 Public health agencies should adopt and enforce confidentiality policies that incorporate fair information practices and use state-of-the-art security measures to implement those policies.
To these three specific challenges for public health informatics,1 we can add another challenge, potentially more important (if less concrete) than the rest— to apply information technology in unanticipated ways to reengineer public health and invent new ways to protect and promote community health. If, as we have said, the goal of public health is to promote health and prevent unnecessary disease, injury, and disability and the means are open-ended, we suggest that unexplored and unimagined ways to promote and protect community health using the power of modern information technology still exist. We have briefly outlined and illustrated the complex, multidimensional nature of public health as a discipline; we anticipate working with our clinical informatics colleagues as critical partners in addressing these major public health informatics challenges.
Acknowledgments
The authors thank Dr. Dave Erickson and Dr. Joseph Mulinare, of the National Center on Birth Defects and Developmental Disabilities, CDC, for their insights and help with the folic acid case study (including the provision of Figures 4 through 7▶▶▶▶), and Ms. Mary Anne Freedman, of the National Center for Health Statistics, CDC, for information about the vital statistics system.
This manuscript is based in part on presentations made by the authors at an orientation session entitled “Public Health for Informaticians” at the AMIA 2001 Spring Congress, May 15-17, 2001, in Atlanta, Georgia,
References
- 1.Yasnoff WA, O'Carroll PW, Koo D, Linkins RW, Kilbourne E. Public health informatics: improving and transforming public health in the information age. J Public Health Manage Pract. 2000;6:67–75. [DOI] [PubMed] [Google Scholar]
- 2.Public Health Functions Steering Committee. Public health in America. Statement adopted Fall 1994. Public Health Functions Web site. Available at: http://www.health.gov/phfunctions/public.htm. Accessed Jul 10, 2001.
- 3.Centers for Disease Control and Prevention. Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48:241–3. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Changes in the public health system. MMWR Morb Mortal Wkly Rep. 1999;48:1141–6. [Google Scholar]
- 5.Foster KR, Jenkins MF, Toogood AC. The Philadelphia yellow fever epidemic of 1793. Sci Am. 1998;279(2):88–93. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine, Committee for the Study of the Future of Public Health, Division of Health Care Services. The Future of Public Health. Washington, DC: National Academy Press, 1988.
- 7.Centers for Disease Control and Prevention. Public Health Infrastructure: A Status Report. Prepared for the Appropriations Committee of the United States Senate, March 2001. Public Health Practice Program Office Web site. Available at: http://www.phppo.cdc.gov/documents/phireport2_16.pdf. Accessed Jun 6, 2001.
- 8.Gerzoff RB, Richards TB. The education of local health department top executives. J Public Health Manage Pract. 1997;3: 50–6. [DOI] [PubMed] [Google Scholar]
- 9.Minnesota Department of Health. Selected Rural Public Health Agencies 2001 Wage and Benefit Survey. June 2001. Available at: http://www.health.state.mn.us/divs/chs/wagesurvey.doc. Accessed Jul 13, 2001.
- 10.Contract Agreement between Worthington Regional Hospital and the Minnesota Nurses Association, Jan 1, 2000–Dec 31, 2001. St. Paul, Minn.: Minnesota Nurses Association, 2001.
- 11.Minnesota Department of Health. Health Alert Network Year 2 Survey of Local Public Health Agencies [unpublished report]. Minneapolis, Minn.: MDH, March 2001.
- 12.Last JM (ed). A Dictionary of Epidemiology. New York: Oxford, 1995.
- 13.Thacker SB, Berkelman RL. Public health surveillance in the United States. Epidemiol Rev. 1988:10:164–90. [DOI] [PubMed] [Google Scholar]
- 14.Teutsch SM, Churchill RE (eds). Principles and Practice of Public Health Surveillance. New York: Oxford, 2000.
- 15.Koo D, Wetterhall SF. History and current status of the National Notifiable Diseases Surveillance System. J Public Health Manage Pract. 1996;2:4–10. [DOI] [PubMed] [Google Scholar]
- 16.Roush S, Birkhead G, Koo D, Cobb A, Fleming D. Mandatory reporting of diseases and conditions by health care professionals and laboratories. JAMA. 1999;282:164–70. [DOI] [PubMed] [Google Scholar]
- 17.Botto LD, Moore CA, Khoury MJ, Erickson JD. Neural-tube defects. N Engl J Med. 1999;341:1509–19. [DOI] [PubMed] [Google Scholar]
- 18.Smithells RW, Nevin NC, Seller MJ, et al. Further experience of vitamin supplementation for the prevention of neural tube defect recurrences. Lancet. 1983;1:1027–31. [DOI] [PubMed] [Google Scholar]
- 19.Medical Research Council. Vitamin Study Research Group. Prevention of neural tube defects: results of the Medical Research Council vitamin study. Lancet. 1991;338;131–7. [PubMed] [Google Scholar]
- 20.Czeizel AE, Dudas I. Prevention of the first occurrence of neural tube defects by periconceptional vitamin supplementation. N Engl J Med. 1992;327:1832–5. [DOI] [PubMed] [Google Scholar]
- 21.Laurence KM, James N, Miller MH, Tennant GB, Campbell H. Double-blind randomised controlled trial of folate treatment before conception to prevent recurrence of neural-tube defects. BMJ. 1981;282:1509–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mulinare J, Cordero JF, Erickson JD, Berry RJ. Periconceptional use of multivitamins and the occurrence of neural tube defects. JAMA. 1988;260:3141–5. [PubMed] [Google Scholar]
- 23.Milunsky A, Jick H, Jick SS, et al. Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence of neural tube defects. JAMA. 1989;262:2847–52. [DOI] [PubMed] [Google Scholar]
- 24.Tolson GC, Barnes JM, Gay GA, Kowaleski JL. The 1989 revision of the US standard certificates and reports. Vital Health Stat [4], June 1991, no. 28:1–34. Washington, DC: Department of Health and Human Services, 1991. Publication PHS 91-1465. [PubMed]
- 25.Freedman MA, Gay GA, Brockert JE, Potrzebowski PW, Rothwell CJ. The 1989 revisions of the U.S. standard certificates of live birth and death and the U.S. standard report of fetal death. Am J Public Health. 1988;78:168–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Honein MA, Paulozzi LJ, Mathews TJ, Erickson JD, Wong LYC. Impact of folic acid fortification of the U.S. food supply on the occurrence of neural tube defects. JAMA. 2001;285: 2981–6. [DOI] [PubMed] [Google Scholar]
- 27.Watkins ML, Edmonds L, McClearn A, Mullins L, Mulinare J, Khoury M. The surveillance of birth defects: the usefulness of the revised US standard birth certificates. Am J Public Health. 1996;86:731–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piper JM, Mitchel EF, Snowden M, Hall C, Adams M, Taylor P. Validation of the 1989 Tennessee birth certificates using maternal and newborn hospital records. Am J Epidemiol. 1993;137:758–68. [DOI] [PubMed] [Google Scholar]
- 29.Yen IH, Khoury MJ, Erickson JD, et al. The changing epidemiology of neural tube defects: United States, 1968–1989. Am J Dis Child. 1992;146:857–61. [DOI] [PubMed] [Google Scholar]
- 30.Limb CJ, Homes LB. Anencephaly: changes in prenatal detection and birth status, 1972 through 1990. Am J Obstet Gynecol. 1994;170:1333–8. [DOI] [PubMed] [Google Scholar]
- 31.National Birth Defects Prevention Network. Congenital malformations surveillance report: a report from the National Birth Defects Prevention Network. Teratology. 2000;61:33–85. [DOI] [PubMed] [Google Scholar]
- 32.Hendricks KA, Simpson JS, Larsen RD. Neural tube defects along the Texas–Mexico border, 1993–1995. Am J Epidemiol. 1999;149:1119–27. [DOI] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. Use of folic acid for prevention of spina bifida and other neural tube defects — 1983–1991: effectiveness in disease and injury prevention. MMWR Morb Mortal Wkly Rep. 1991;40:513–6. [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR. 1992;41 (RR–14):1–7. [PubMed] [Google Scholar]
- 35.Henshaw SK. Unintended pregnancy in the United States. Fam Plann Perspect. 1998;30:24–9. [PubMed] [Google Scholar]
- 36.U.S. Food and Drug Administration. 21 CFR Parts 136, 137, and 139. Food standards: amendment of standards of identity for enriched grain products to require addition of folic acid. Federal Register. 1996;61:8781–97. [Google Scholar]
- 37.Gregory JF III. Bioavailability of folate. Eur J Clin Nutr. 1997; 51(suppl):554–559. [PubMed] [Google Scholar]
- 38.Romano PS, Waitzman NJ, Scheffler RM, Pi RD. Folic acid fortification of grain: an economic analysis. Am J Public Health. 1995;85:667–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mills JL. Fortification of foods with folic acid: How much is enough? N Engl J Med. 2000;342:1442–5. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Preventing Neural Tube Birth Defects: A Prevention Model and Resource Guide. Atlanta, GA: U.S. Department of Health and Human Services, CDC, National Center for Environmental Health, Division of Birth Defects and Pediatric Genetics, 1998. Available at: http://www.cdc.gov/ncbddd/folicacid/ntd/cover.htm
- 41.Rader JI, Weaver CM, Angyal G. Total folate in enriched cereal-grain products in the United States following fortification. Food Chem. 2000;70:275–89. [Google Scholar]
- 42.Centers for Disease Control and Prevention. Knowledge and use of folic acid by women of childbearing age—United States, 1995 and 1998. MMWR. 1999;48:325–7. [PubMed] [Google Scholar]
- 43.March of Dimes/Gallup Organization. Folic acid and the prevention of birth defects: a national survey of pre-pregnancy awareness and behavior among women of childbearing age, 1995–2000 [survey]. White Plains, NY: March of Dimes, June 2000. Publication 31-1404-00.
- 44.Centers for Disease Control and Prevention. Folate status in women of childbearing age—United States, 1999. MMWR. 2000;49:962–5. [PubMed] [Google Scholar]
- 45.Jacques PF, Selhub J, Bostom AG, Wilson PWF, Rosenberg IH. The effect of folic acid fortification on plasma folate and total homocysteine concentrations. N Engl J Med 1999;340:1449–54. [DOI] [PubMed] [Google Scholar]
- 46.Lawrence JM, Petitti DB, Watkins M, Umekubo MA. Trends in serum folate after food fortification [letter]. Lancet. 1999;354: 915–6. [DOI] [PubMed] [Google Scholar]
- 47.Marier R. The reporting of communicable diseases. Am J Epidemiol. 1977;105:587–90. [DOI] [PubMed] [Google Scholar]
- 48.Alter MJ, Mares A, Hadler SC, et al. The effect of under reporting on the apparent incidence and epidemiology of acute viral hepatitis. Am J Epidemiol. 1987;125:133–9. [DOI] [PubMed] [Google Scholar]
- 49.Kirsch T, Shesser R. A survey of emergency department communicable disease reporting practices. J Emerg Med. 1991;9: 211–4. [DOI] [PubMed] [Google Scholar]
- 50.Konowitz PM, Petrossian GA, Rose DN. The underreporting of disease and physicians' knowledge of reporting requirements. Public Health Rep. 1984;99:31–5. [PMC free article] [PubMed] [Google Scholar]
- 51.Simpson DM. Improving the reporting of notifiable diseases in Texas: suggestions from an ad hoc committee of providers. J Public Health Manage Pract. 1996;2:37–9. [DOI] [PubMed] [Google Scholar]
- 52.Campos-Outcalt D, England R, Porter B. Reporting of communicable diseases by university physicians. Public Health Rep. 1991;106:579–83. [PMC free article] [PubMed] [Google Scholar]
- 53.U.S. Department of Health and Human Services. 45 CFR parts 160 and 164. Standards for privacy of individually identifiable health information: final rule. Federal Register. 2000;65: 82798–829. [Google Scholar]


