Abstract
Introduction
Prone positioning in respiratory failure has been shown to be a useful adjunct in the treatment of severe hypoxia. However, the prone position can result in dislodgment or malfunction of tubes and cannulae. Certain patients receiving extracorporeal membrane oxygenation (ECMO) or continuous renal replacement therapy (CRRT) may also benefit from positional therapy. The impact of cannula-related complications in these patients is potentially disastrous. The safety and efficacy of prone positioning of these patients has not been previously reported.
Materials and methods
A retrospective chart review evaluated ECMO or CRRT cannula location, and displacement or malfunction during positional change or while prone. The study was set in a General Surgery and Trauma Intensive Care Unit. The subjects were all patients at our institution who simultaneously underwent ECMO or CRRT and prone positioning from July 1996 to July 2001. There were no interventions.
Results
Ten patients underwent ECMO and 42 patients underwent CRRT during the study period. Seven patients underwent simultaneous prone positioning and either ECMO (4/10) or CRRT (4/42). A total of 68 turning events (prone to supine or supine to prone) were recorded, with each patient averaging 9.7 (range, 4–16) turning episodes. Turning was performed with sheets and extra nursing personnel; no special mechanical assist devices were used. No patients experienced inadvertent cannula removal during turning. Two patients had poor flow through their cannulae. In one patient, this occurred in the supine position and required repositioning of the cannula. In the second patient, cannulae were changed twice and flow was poor in both the supine and the prone positions. All ECMO and CRRT patients received venous cannulae. Cannula location (seven internal jugular and 11 femoral) did not the affect risk of malfunction.
Discussion and conclusions
Patients with venous cannulae for ECMO or CRRT can be safely placed in the prone position. Flow rates are maintained in this position. Potential cannula complications of ECMO and CRRT are not a contraindication to prone positioning in severely ill patients.
Keywords: continuous renal replacement therapy, extra-corporeal membrane oxygenation, positional therapy, prone positioning, renal replacement therapy, safety
Introduction
Prone positioning for respiratory failure has recently gained popularity as an adjunct for the treatment of respiratory failure and adult respiratory distress syndrome. High-risk patients who may benefit from prone positioning include some patients with large-bore, high-flow-access cannulae. This includes patients on extracorporeal membrane oxygenation (ECMO) and continuous renal replacement therapy (CRRT), such as continuous venovenous hemofiltration and dialysis. Cannula-related complications in these patients are potentially disastrous and the safety of turning patients with these types of cannulae has not been previously demonstrated.
Materials and methods
All patients admitted to the intensive care unit from July 1996 to July 2001 who underwent prone positioning while receiving either ECMO or CRRT were evaluated. Demographic data were recorded as well as the number of turns, the location of the cannulae and cannula displacement or malfunction as related to positioning. The turning technique used for all of these patients requires only sheets and extra personnel (Figs 1,2,3,4,5); no mechanical assist devices are used. Access cannulae and tubing are brought off the ends of the bed to provide coaxial rotation. An intensivist, a respiratory therapist, and multiple nurses are present for all turning events. Vital signs are monitored closely before and after the turn to ensure that the patient is tolerating the position change.
Figure 1.

A typical patient at our institution undergoing prone positioning. The abdomen is open due to a gunshot wound. The patient requires multiple vasopressors, continuous venovenous hemofiltration and inhaled nitric oxide.
Figure 2.
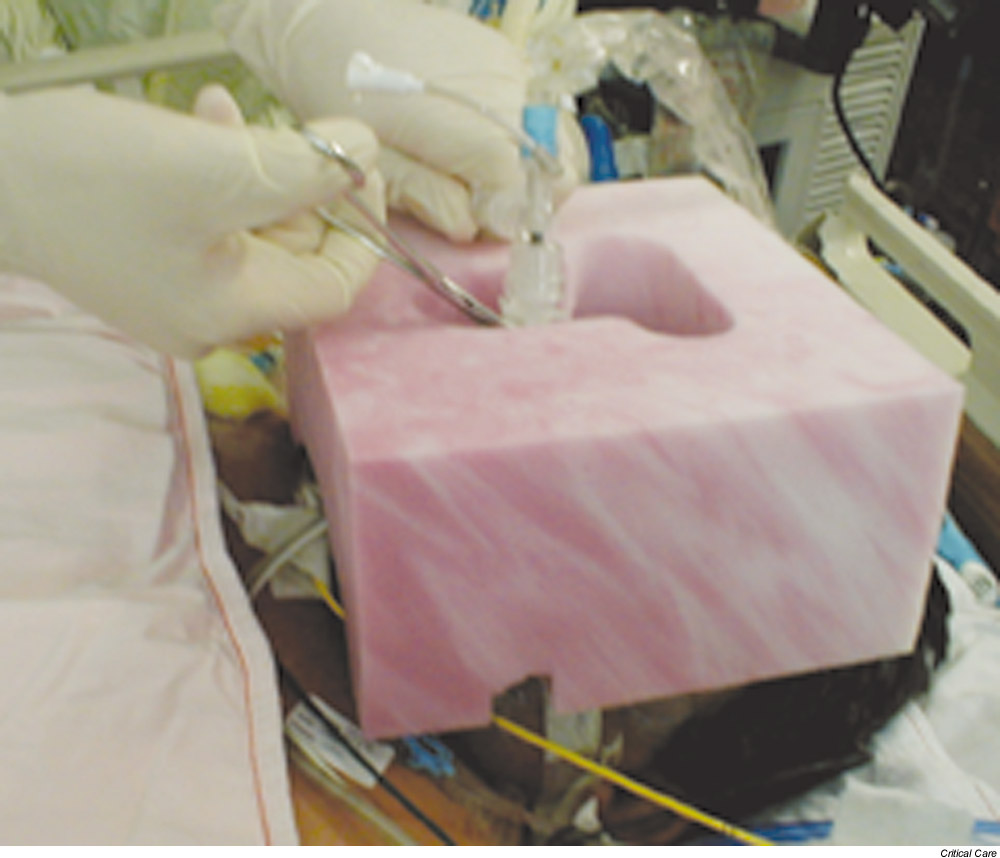
Adequate padding, especially of the face, is mandatory. An operative pillow with a cutout for the endotracheal tube is used. Prior to disconnecting the endotracheal tube, it is clamped to prevent loss of positive end expiratory pressure.
Figure 3.

The patient is tightly rolled in two sheets and is moved to the far side of the bed, away from the ventilator.
Figure 4.

The patient is rolled into an extreme lateral position, facing the ventilator, with close monitoring of the hemodynamics. As the turn is completed, transverse rolls are place under the chest and pelvis to allow free abdominal excursion.
Figure 5.

Positioning is completed with chest and pelvis rolls in place, and the arms flexed at the elbows and in the neutral position at the shoulders. The arm position is changed every 2 hours and automated bed rotation is continued in the prone position. The feet are elevated with ankle rolls to prevent pressure breakdown.
Results
During the study period, 10 patients underwent ECMO and 42 patients underwent CRRT. Seven patients underwent simultaneous prone positioning and either ECMO (n = 3) or CRRT (n = 4). Table 1 demonstrates the demographics, the disease process and the outcome of the patients. A total of 68 turning events (prone to supine or supine to prone) were recorded, with each patient averaging 9.7 (range, 4–16) turning episodes. No patients experienced inadvertent cannula removal during turning. Two patients had poor flow through their cannulae unrelated to prone position or turning. In one patient, this occurred in the supine position and required repositioning of the cannula. In the second patient, cannulae were changed twice and flow was poor in both the supine and the prone positions. All ECMO and CRRT patients in this series received venous cannulae. The cannula location (seven internal jugular and 11 femoral) did not affect the risk of malfunction. One internal jugular cannula was repositioned, and one was replaced for poor flow. One femoral cannula was replaced for poor flow.
Table 1.
Demographics, disease process and outcome of patients
| Patient | Age (years) | Sex | Primary disease | Therapy | Number of turns on therapy | Cannula location | Cannula complication | Outcome |
| 1 | 26 | Male | Inhalation injury, burn | ECMO | 4 | RIJ, RFem | None | Alive |
| 2 | 34 | Male | Pulmonary contusion, polytrauma | ECMO | 6 | RIJ, RFem, LFem | None | Dead |
| 3 | 21 | Female | Viral pneumonia | ECMO | 10 | RIJ, RFem, LFem | None | Dead |
| 4 | 47 | Male | Esophagectomy, anastomotic leak | CVVH | 10 | RIJ × 2, RFem × 2 | Both cannulae changed, poor flow supine and prone | Dead |
| 5 | 37 | Male | Abdominal gunshot | CVVH | 12 | LFem | None | Alive |
| 6 | 23 | Male | Abdominal gunshot | ECMO | 8 | RIJ, RFem × 2 | None | Alive |
| CVVH | 2 | |||||||
| 7 | 59 | Male | Viral pneumonia | ECMO | 16 | RIJ, RFem | RIJ low flow supine, cannula repositioned | Dead |
CVVH, continuous venovenous hemofiltration; ECMO, extracorporeal membrane oxygenation; RIJ, right internal jugular vein; RFem, right femoral vein; LFem, left femoral vein.
Discussion
Prone positioning for respiratory failure has been shown to increase oxygenation when used as adjunctive therapy for respiratory failure and adult respiratory distress syndrome. This has resulted in an increase in the use of prone positioning worldwide, with numerous studies of its effects. Recent studies, however, have not demonstrated a decrease in mortality with this modality [1].
The act of turning patients prone, and the prone position itself, is not without risk. These patients tend to require high levels of ventilatory and hemodynamic support, and are dependent on endotracheal tubes and monitoring cannulae, as well as on intravenous inotropic infusions. In addition, these patients are heavily sedated and often paralyzed, resulting in their inability to shift position to prevent pressure necrosis or neurologic injury from poor positioning. Hence, the choice to use prone positioning as a therapy must be weighed against the potential risks of the turning and the position.
Prone positioning and turning have been reported to result in complications in 32% of prone cycles. Most of these are related to skin pressure necrosis. Inadvertent extubation and central line decannulation are two of the more disastrous complications that have been reported [2,3].
Our group has previously reported the safety of prone positioning in high-risk patients, such as those with open abdomens [4]. Other similarly high-risk patients with large-bore vascular cannulae may not undergo prone positioning due to fear of cannula complications, including patients on ECMO and CRRT. The safety of turning patients with these types of cannulae has not been systematically evaluated. There are reports of individual cases of prone positioning in patients with continuous venovenous hemofiltration therapy [5,6,7,8].
The present results indicate that prone positioning with these cannulae can be carried out safely and does not significantly affect the function of the high-flow systems. This again expands the patient population in which prone positioning is potentially beneficial. The location of high flow catheters is not related to complication or malfunction rate, thus all sites can be safely used for access.
The outcome of the present group of patients was poor, with 57% mortality. This is not surprising given the severity of illness necessitating both prone positioning and therapy with ECMO or CRRT. There were no deaths related to turning, to the prone position or to cannula malfunction. This series is too small to offer any predictions regarding survival with the multimodality therapy used.
Conclusions
Using our technique, prone positioning with large-bore venous access is safe and does not result in cannula complications. Flow rates are maintained in the prone position. Potential cannula complications of ECMO and CRRT are not a contraindication to prone positioning in severely ill patients.
Competing interests
None declared.
Key messages
• Prone positioning is an important adjunct in the treatment of respiratory failure
• Some patients with severe respiratory failure, who are receiving ECMO or CRRT may also benefit from prone positioning
• It is safe to position patients prone with high flow venous catheters if a co-ordinated method of turning is used with care to avoid dislodgment of the access lines
Abbreviations
ECMO = extracorporeal membrane oxygenation; CRRT = continuous renal replacement therapy.
Acknowledgments
Acknowledgements
The work was performed at the Hospital of the University of Pennsylvania. There was no financial support for this study. The original abstract was a poster presentation at the Society of Critical Care Medicine in San Diego, California, USA, 2002.
References
- Gattinoni L, Tognoni G, Pesenti A, Taccone P, Mascheroni D, Labarta V, Malacrida R, Di Giulio P, Fumagalli R, Pelosi P, Brazzi L, Latini R, Prone-Supine Study Group. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001;345:568–573. doi: 10.1056/NEJMoa010043. [DOI] [PubMed] [Google Scholar]
- Offner PJ, Haenel JB, Moore EE, Biffl WL, Francoise RJ, Burch JM. Complications of prone ventilation in patients with multi-system trauma with fulminant acute respiratory distress syndrome. J Trauma. 2000;48:224–228. doi: 10.1097/00005373-200002000-00004. [DOI] [PubMed] [Google Scholar]
- Curley MA. Prone positioning of patients with acute respiratory distress syndrome: a systematic review. Am J Crit Care. 2000;8:392–405. [PubMed] [Google Scholar]
- Schiller HJ, Reilly PM, Anderson HL, Schwab CW. The 'open abdomen' is not a contraindication to prone positioning for severe ARDS [abstract]. Chest. 1996;110:142S. [Google Scholar]
- Mure M, Martling C-R, Lindahl S. Dramatic effect on oxygenation in patients with severe acute lung insufficiency treated in the prone position. Crit Care Med. 1997;25:1539–1544. doi: 10.1097/00003246-199709000-00022. [DOI] [PubMed] [Google Scholar]
- Chatte G, Sab J-M, Dubois J-M, Sirodot M, Gaussorgues P, Robert D. Prone position in mechanically ventilated patients with severe acute respiratory failure. Am J Respir Crit Care Med. 1997;115:473–478. doi: 10.1164/ajrccm.155.2.9032181. [DOI] [PubMed] [Google Scholar]
- Kornecki A, Frndova H, Coates AL, Shemie S. A randomized trail of prolonged prone positioning in children with acute respiratory failure. Chest. 2001;119:211–218. doi: 10.1378/chest.119.1.211. [DOI] [PubMed] [Google Scholar]
- Marik PE, Iglesias J. A 'prone dependent' patient with severe adult respiratory distress syndrome. Crit Care Med. 1997;25:1085–1087. doi: 10.1097/00003246-199706000-00030. [DOI] [PubMed] [Google Scholar]


