Abstract
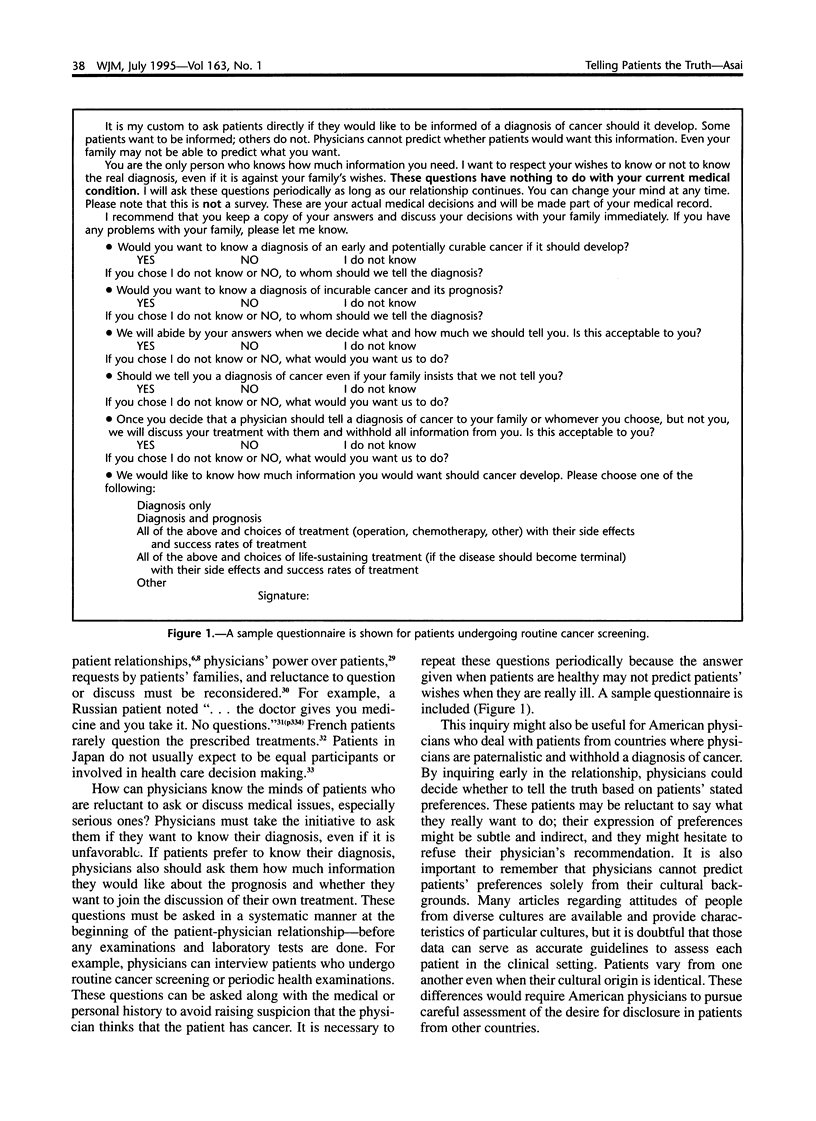
The medical literature suggests that most patients want to be told the truth about a diagnosis of cancer. Despite this evidence of their patients' wishes, physicians in many countries still hesitate to disclose this and other diagnoses. Physicians frequently ignore their patients' wishes when they consider the appropriateness of truth telling. A complete shift from nondisclosure to mandatory disclosure without considering patients' preferences may lead to serious harm to patients who do not want to be told the truth. Because physicians cannot satisfactorily treat patients without knowing their preferences toward disclosure of a diagnosis, I propose a simple strategy to break this long-standing ethical dilemma--physicians must develop the habit of inquiring about their patients' preferences.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beyene Y. Medical disclosure and refugees. Telling bad news to Ethiopian patients. West J Med. 1992 Sep;157(3):328–332. [PMC free article] [PubMed] [Google Scholar]
- Brod M., Heurtin-Roberts S. Older Russian emigrés and medical care. West J Med. 1992 Sep;157(3):333–336. [PMC free article] [PubMed] [Google Scholar]
- Dalla-Vorgia P., Katsouyanni K., Garanis T. N., Touloumi G., Drogari P., Koutselinis A. Attitudes of a Mediterranean population to the truth-telling issue. J Med Ethics. 1992 Jun;18(2):67–74. doi: 10.1136/jme.18.2.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estapé J., Palombo H., Hernández E., Daniels M., Estapé T., Grau J. J., Viñolas N., Mañ J. M. Cancer diagnosis disclosure in a Spanish hospital. Ann Oncol. 1992 Jun;3(6):451–454. doi: 10.1093/oxfordjournals.annonc.a058233. [DOI] [PubMed] [Google Scholar]
- Feldman E. Medical ethics the Japanese way. Hastings Cent Rep. 1985 Oct;15(5):21–24. [PubMed] [Google Scholar]
- Feldman J. The French are different. French and American medicine in the context of AIDS. West J Med. 1992 Sep;157(3):345–349. [PMC free article] [PubMed] [Google Scholar]
- Freedman B. Offering truth. One ethical approach to the uninformed cancer patient. Arch Intern Med. 1993 Mar 8;153(5):572–576. doi: 10.1001/archinte.153.5.572. [DOI] [PubMed] [Google Scholar]
- Hadfield P. Informed consent. Lancet. 1993 May 1;341(8853):1141–1141. doi: 10.1016/0140-6736(93)93144-p. [DOI] [PubMed] [Google Scholar]
- Hattori H., Salzberg S. M., Kiang W. P., Fujimiya T., Tejima Y., Furuno J. The patient's right to information in Japan--legal rules and doctor's opinions. Soc Sci Med. 1991;32(9):1007–1016. doi: 10.1016/0277-9536(91)90158-9. [DOI] [PubMed] [Google Scholar]
- Haug M. R., Akiyama H., Tryban G., Sonoda K., Wykle M. Self care: Japan and the U.S. compared. Soc Sci Med. 1991;33(9):1011–1022. doi: 10.1016/0277-9536(91)90006-x. [DOI] [PubMed] [Google Scholar]
- Holland J. C., Geary N., Marchini A., Tross S. An international survey of physician attitudes and practice in regard to revealing the diagnosis of cancer. Cancer Invest. 1987;5(2):151–154. doi: 10.3109/07357908709018468. [DOI] [PubMed] [Google Scholar]
- Kai I., Ohi G., Yano E., Kobayashi Y., Miyama T., Niino N., Naka K. Communication between patients and physicians about terminal care: a survey in Japan. Soc Sci Med. 1993 May;36(9):1151–1159. doi: 10.1016/0277-9536(93)90235-v. [DOI] [PubMed] [Google Scholar]
- Kojima D. [A survey on informed consent. Approach to cancer treatment]. Nihon Ika Daigaku Zasshi. 1991 Feb;58(1):39–49. doi: 10.1272/jnms1923.58.39. [DOI] [PubMed] [Google Scholar]
- Morioka Y. Informed consent and truth telling to cancer patients. Gastroenterol Jpn. 1991 Dec;26(6):789–792. doi: 10.1007/BF02782871. [DOI] [PubMed] [Google Scholar]
- Mosconi P., Meyerowitz B. E., Liberati M. C., Liberati A. Disclosure of breast cancer diagnosis: patient and physician reports. GIVIO (Interdisciplinary Group for Cancer Care Evaluation, Italy) Ann Oncol. 1991 Apr;2(4):273–280. doi: 10.1093/oxfordjournals.annonc.a057936. [DOI] [PubMed] [Google Scholar]
- Muller J. H., Desmond B. Ethical dilemmas in a cross-cultural context. A Chinese example. West J Med. 1992 Sep;157(3):323–327. [PMC free article] [PubMed] [Google Scholar]
- Nilchaikovit T., Hill J. M., Holland J. C. The effects of culture on illness behavior and medical care. Asian and American differences. Gen Hosp Psychiatry. 1993 Jan;15(1):41–50. doi: 10.1016/0163-8343(93)90090-b. [DOI] [PubMed] [Google Scholar]
- Pfeffer M. R. Ethics and the oncologist. Med Law. 1993;12(3-5):235–240. [PubMed] [Google Scholar]
- Rothchild E. Family dynamics in end-of-life treatment decisions. Gen Hosp Psychiatry. 1994 Jul;16(4):251–258. doi: 10.1016/0163-8343(94)90004-3. [DOI] [PubMed] [Google Scholar]
- Sell L., Devlin B., Bourke S. J., Munro N. C., Corris P. A., Gibson G. J. Communicating the diagnosis of lung cancer. Respir Med. 1993 Jan;87(1):61–63. doi: 10.1016/s0954-6111(05)80315-4. [DOI] [PubMed] [Google Scholar]
- Shimozuma K., Tominaga T., Hayashi K., Kondo J., Kosaki G. [Notification of cancer in breast cancer patients]. Gan To Kagaku Ryoho. 1991 Sep;18(12):2147–2153. [PubMed] [Google Scholar]
- Surbone A. Truth telling to the patient. JAMA. 1992 Oct 7;268(13):1661–1662. [PubMed] [Google Scholar]
- Teshima H., Kihara H., Ago Y., Kawamura H., Inoue T., Nagano H. [Terminal care in patients with lung cancer]. Nihon Kyobu Shikkan Gakkai Zasshi. 1987 Mar;25(3):305–311. [PubMed] [Google Scholar]
- Thomsen O. O., Wulff H. R., Martin A., Singer P. A. What do gastroenterologists in Europe tell cancer patients? Lancet. 1993 Feb 20;341(8843):473–476. doi: 10.1016/0140-6736(93)90218-6. [DOI] [PubMed] [Google Scholar]


