Abstract
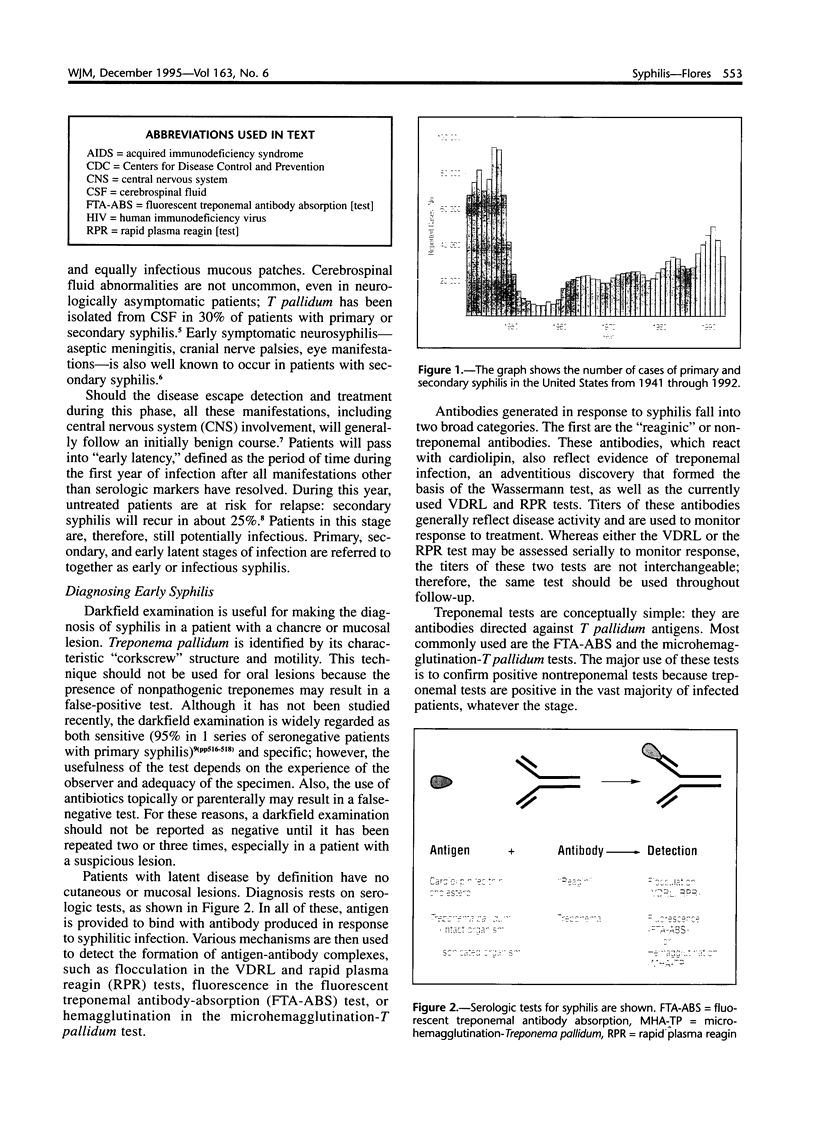
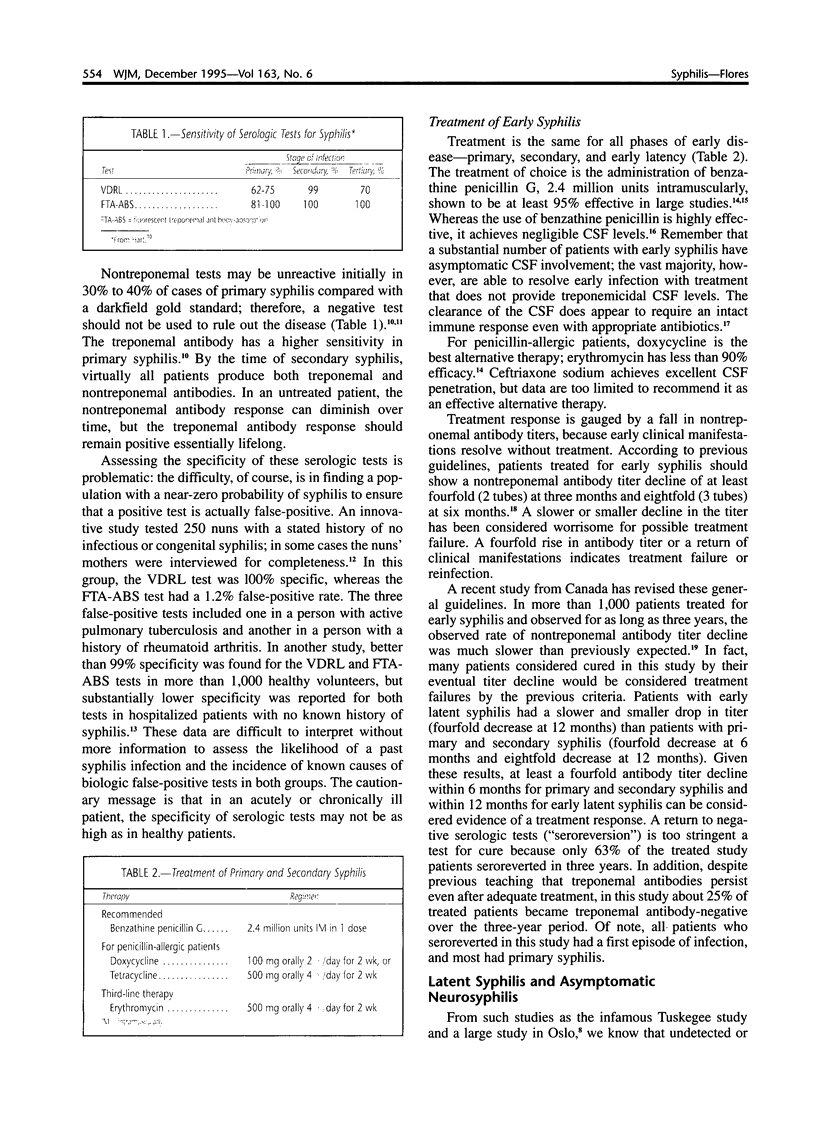
Despite the widespread availability of effective treatment, the incidence of primary and secondary syphilis in the United States is on the rise. In addition, syphilis is occurring in a substantial number of patients infected with the human immunodeficiency virus (HIV), thus adding to the complexities of diagnosis and treatment. Primary syphilis represents a disseminated infection, often accompanied by abnormalities of the cerebrospinal fluid, that may pass unrecognized and progress to the myriad manifestations of secondary syphilis. The diagnosis of syphilis in patients with mucosal or skin lesions may be made by darkfield examination; once lesions have resolved, serologic tests are required. Patients with latent syphilis may have asymptomatic neurosyphilis and risk progression to tertiary disease. The diagnosis of asymptomatic neurosyphilis is necessary to determine the optimal treatment of patients with latent disease. The diagnosis of active neurosyphilis generally requires an inflammatory cerebrospinal fluid profile and a reactive cerebrospinal fluid VDRL test. Syphilis is common in HIV-infected patients, who may have an altered antibody response to infection and an apparent increased incidence of neurologic complications. The preferred treatment at all stages is penicillin, which is also the only recommended therapy for neurosyphilis. The optimal treatment of syphilis in HIV-infected patients is unknown.
Full text
PDF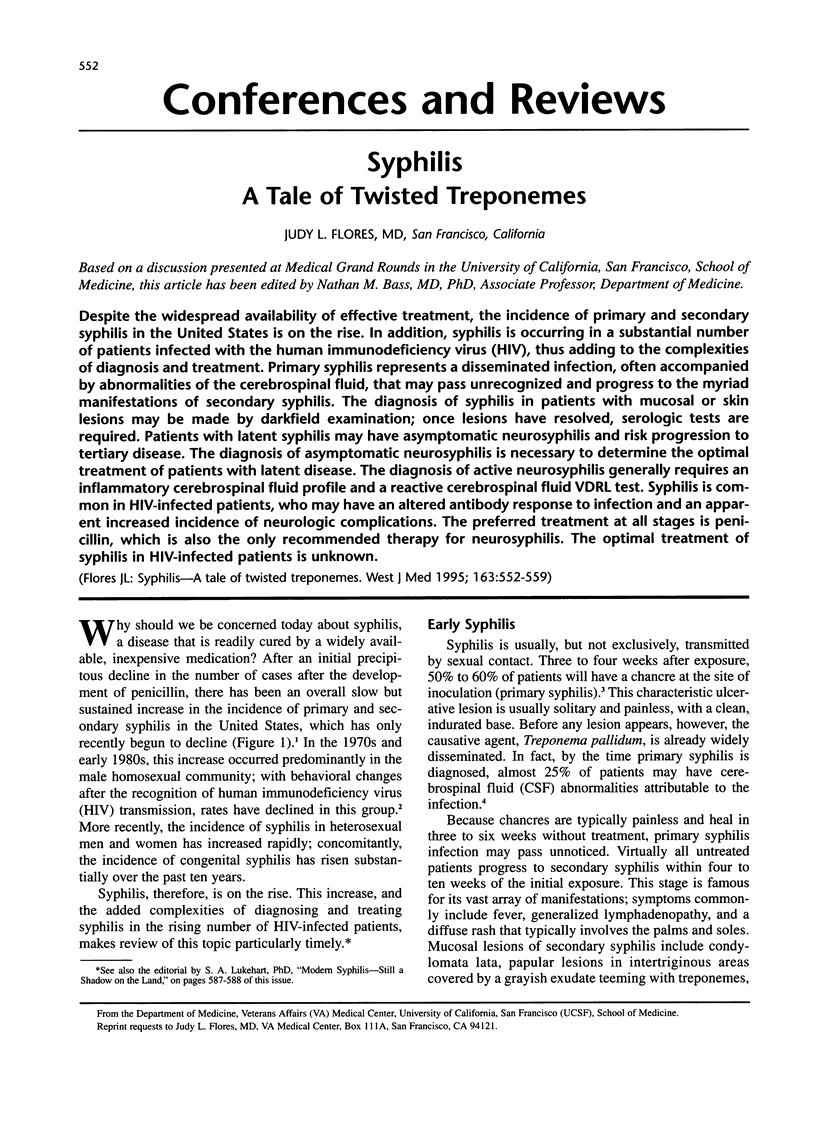


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berger J. R. Neurosyphilis in human immunodeficiency virus type 1-seropositive individuals. A prospective study. Arch Neurol. 1991 Jul;48(7):700–702. doi: 10.1001/archneur.1991.00530190046014. [DOI] [PubMed] [Google Scholar]
- Berinstein D., DeHertogh D. Recently acquired syphilis in the elderly population. Arch Intern Med. 1992 Feb;152(2):330–332. [PubMed] [Google Scholar]
- Berry C. D., Hooton T. M., Collier A. C., Lukehart S. A. Neurologic relapse after benzathine penicillin therapy for secondary syphilis in a patient with HIV infection. N Engl J Med. 1987 Jun 18;316(25):1587–1589. doi: 10.1056/NEJM198706183162507. [DOI] [PubMed] [Google Scholar]
- Brown S. T., Zaidi A., Larsen S. A., Reynolds G. H. Serological response to syphilis treatment. A new analysis of old data. JAMA. 1985 Mar 1;253(9):1296–1299. [PubMed] [Google Scholar]
- DATTNER B., THOMAS E. W., DE MELLO L. Criteria for the management of neurosyphilis. Am J Med. 1951 Apr;10(4):463–467. doi: 10.1016/0002-9343(51)90292-6. [DOI] [PubMed] [Google Scholar]
- Dans P. E., Cafferty L., Otter S. E., Johnson R. J. Inappropriate use of the cerebrospinal fluid Venereal Disease Research Laboratory (VDRL) test to exclude neurosyphilis. Ann Intern Med. 1986 Jan;104(1):86–89. doi: 10.7326/0003-4819-104-1-86. [DOI] [PubMed] [Google Scholar]
- Doskocil M., Med M., Vimmer T. Musculus rectus femoris--zacátecní slacha, její funkcní význam. Acta Chir Orthop Traumatol Cech. 1987 Apr;54(2):99–107. [PubMed] [Google Scholar]
- Dowell M. E., Ross P. G., Musher D. M., Cate T. R., Baughn R. E. Response of latent syphilis or neurosyphilis to ceftriaxone therapy in persons infected with human immunodeficiency virus. Am J Med. 1992 Nov;93(5):481–488. doi: 10.1016/0002-9343(92)90574-u. [DOI] [PubMed] [Google Scholar]
- Faber W. R., Bos J. D., Rietra P. J., Fass H., Van Eijk R. V. Treponemicidal levels of amoxicillin in cerebrospinal fluid after oral administration. Sex Transm Dis. 1983 Jul-Sep;10(3):148–150. doi: 10.1097/00007435-198307000-00011. [DOI] [PubMed] [Google Scholar]
- Feraru E. R., Aronow H. A., Lipton R. B. Neurosyphilis in AIDS patients: initial CSF VDRL may be negative. Neurology. 1990 Mar;40(3 Pt 1):541–543. doi: 10.1212/wnl.40.3_part_1.541. [DOI] [PubMed] [Google Scholar]
- Goldman J. N., Lantz M. A. FTA-ABS and VDRL slide test reactivity in a population of nuns. JAMA. 1971 Jul 5;217(1):53–55. [PubMed] [Google Scholar]
- Gordon S. M., Eaton M. E., George R., Larsen S., Lukehart S. A., Kuypers J., Marra C. M., Thompson S. The response of symptomatic neurosyphilis to high-dose intravenous penicillin G in patients with human immunodeficiency virus infection. N Engl J Med. 1994 Dec 1;331(22):1469–1473. doi: 10.1056/NEJM199412013312201. [DOI] [PubMed] [Google Scholar]
- Gourevitch M. N., Selwyn P. A., Davenny K., Buono D., Schoenbaum E. E., Klein R. S., Friedland G. H. Effects of HIV infection on the serologic manifestations and response to treatment of syphilis in intravenous drug users. Ann Intern Med. 1993 Mar 1;118(5):350–355. doi: 10.7326/0003-4819-118-5-199303010-00005. [DOI] [PubMed] [Google Scholar]
- Haas J. S., Bolan G., Larsen S. A., Clement M. J., Bacchetti P., Moss A. R. Sensitivity of treponemal tests for detecting prior treated syphilis during human immunodeficiency virus infection. J Infect Dis. 1990 Oct;162(4):862–866. doi: 10.1093/infdis/162.4.862. [DOI] [PubMed] [Google Scholar]
- Hart G. Syphilis tests in diagnostic and therapeutic decision making. Ann Intern Med. 1986 Mar;104(3):368–376. doi: 10.7326/0003-4819-104-3-368. [DOI] [PubMed] [Google Scholar]
- Hicks C. B., Benson P. M., Lupton G. P., Tramont E. C. Seronegative secondary syphilis in a patient infected with the human immunodeficiency virus (HIV) with Kaposi sarcoma. A diagnostic dilemma. Ann Intern Med. 1987 Oct;107(4):492–495. doi: 10.7326/0003-4819-107-4-492. [DOI] [PubMed] [Google Scholar]
- Hollander H. Cerebrospinal fluid normalities and abnormalities in individuals infected with human immunodeficiency virus. J Infect Dis. 1988 Oct;158(4):855–858. doi: 10.1093/infdis/158.4.855. [DOI] [PubMed] [Google Scholar]
- Holtom P. D., Larsen R. A., Leal M. E., Leedom J. M. Prevalence of neurosyphilis in human immunodeficiency virus-infected patients with latent syphilis. Am J Med. 1992 Jul;93(1):9–12. doi: 10.1016/0002-9343(92)90673-y. [DOI] [PubMed] [Google Scholar]
- Horowitz H. W., Valsamis M. P., Wicher V., Abbruscato F., Larsen S. A., Wormser G. P., Wicher K. Brief report: cerebral syphilitic gumma confirmed by the polymerase chain reaction in a man with human immunodeficiency virus infection. N Engl J Med. 1994 Dec 1;331(22):1488–1491. doi: 10.1056/NEJM199412013312204. [DOI] [PubMed] [Google Scholar]
- Hutchinson C. M., Rompalo A. M., Reichart C. A., Hook E. W., 3rd Characteristics of patients with syphilis attending Baltimore STD clinics. Multiple high-risk subgroups and interactions with human immunodeficiency virus infection. Arch Intern Med. 1991 Mar;151(3):511–516. [PubMed] [Google Scholar]
- Johns D. R., Tierney M., Felsenstein D. Alteration in the natural history of neurosyphilis by concurrent infection with the human immunodeficiency virus. N Engl J Med. 1987 Jun 18;316(25):1569–1572. doi: 10.1056/NEJM198706183162503. [DOI] [PubMed] [Google Scholar]
- Jordan K. G. Modern neurosyphilis--a critical analysis. West J Med. 1988 Jul;149(1):47–57. [PMC free article] [PubMed] [Google Scholar]
- Katz D. A., Berger J. R. Neurosyphilis in acquired immunodeficiency syndrome. Arch Neurol. 1989 Aug;46(8):895–898. doi: 10.1001/archneur.1989.00520440085024. [DOI] [PubMed] [Google Scholar]
- Lukehart S. A., Hook E. W., 3rd, Baker-Zander S. A., Collier A. C., Critchlow C. W., Handsfield H. H. Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment. Ann Intern Med. 1988 Dec 1;109(11):855–862. doi: 10.7326/0003-4819-109-11-855. [DOI] [PubMed] [Google Scholar]
- Mohr J. A., Griffiths W., Jackson R., Saadah H., Bird P., Riddle J. Neurosyphilis and penicillin levels in cerebrospinal fluid. JAMA. 1976 Nov 8;236(19):2208–2209. [PubMed] [Google Scholar]
- Musher D. M., Hamill R. J., Baughn R. E. Effect of human immunodeficiency virus (HIV) infection on the course of syphilis and on the response to treatment. Ann Intern Med. 1990 Dec 1;113(11):872–881. doi: 10.7326/0003-4819-113-11-872. [DOI] [PubMed] [Google Scholar]
- Musher D. M. Syphilis, neurosyphilis, penicillin, and AIDS. J Infect Dis. 1991 Jun;163(6):1201–1206. doi: 10.1093/infdis/163.6.1201. [DOI] [PubMed] [Google Scholar]
- Quinn T. C., Cannon R. O., Glasser D., Groseclose S. L., Brathwaite W. S., Fauci A. S., Hook E. W., 3rd The association of syphilis with risk of human immunodeficiency virus infection in patients attending sexually transmitted disease clinics. Arch Intern Med. 1990 Jun;150(6):1297–1302. [PubMed] [Google Scholar]
- Rolfs R. T., Nakashima A. K. Epidemiology of primary and secondary syphilis in the United States, 1981 through 1989. JAMA. 1990 Sep 19;264(11):1432–1437. [PubMed] [Google Scholar]
- Romanowski B., Sutherland R., Fick G. H., Mooney D., Love E. J. Serologic response to treatment of infectious syphilis. Ann Intern Med. 1991 Jun 15;114(12):1005–1009. doi: 10.7326/0003-4819-114-12-1005. [DOI] [PubMed] [Google Scholar]
- Rompalo A. M., Cannon R. O., Quinn T. C., Hook E. W., 3rd Association of biologic false-positive reactions for syphilis with human immunodeficiency virus infection. J Infect Dis. 1992 Jun;165(6):1124–1126. doi: 10.1093/infdis/165.6.1124. [DOI] [PubMed] [Google Scholar]
- SMITH C. A., KAMP M., OLANSKY S., PRICE E. V. Benzathine penicillin G in the treatment of syphilis. Bull World Health Organ. 1956;15(6):1087–1096. [PMC free article] [PubMed] [Google Scholar]
- Schober P. C., Gabriel G., White P., Felton W. F., Thin R. N. How infectious is syphilis? Br J Vener Dis. 1983 Aug;59(4):217–219. doi: 10.1136/sti.59.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeter A. L., Lucas J. B., Price E. V., Falcone V. H. Treatment for early syphilis and reactivity of serologic tests. JAMA. 1972 Jul 31;221(5):471–476. [PubMed] [Google Scholar]
- Simon R. P. Neurosyphilis. Arch Neurol. 1985 Jun;42(6):606–613. doi: 10.1001/archneur.1985.04060060112021. [DOI] [PubMed] [Google Scholar]
- Traviesa D. C., Prystowsky S. D., Nelson B. J., Johnson K. P. Cerebrospinal fluid findings in asymptomatic patients with reactive serum fluorescent treponemal antibody absorption tests. Ann Neurol. 1978 Dec;4(6):524–530. doi: 10.1002/ana.410040608. [DOI] [PubMed] [Google Scholar]
- Wentworth B. B., Thompson M. A., Peter C. R., Bawdon R. E., Wilson D. L. Comparison of a hemagglutination treponemal test for syphilis (HATTS) with other serologic methods for the diagnosis of syphilis. Sex Transm Dis. 1978 Jul-Sep;5(3):103–114. doi: 10.1097/00007435-197807000-00005. [DOI] [PubMed] [Google Scholar]
- Wiesel J., Rose D. N., Silver A. L., Sacks H. S., Bernstein R. H. Lumbar puncture in asymptomatic late syphilis. An analysis of the benefits and risks. Arch Intern Med. 1985 Mar;145(3):465–468. [PubMed] [Google Scholar]