Abstract
Moraxella catarrhalis is an important human mucosal pathogen. This study investigated the effect of intranasal immunization with a detoxified-lipooligosaccharide-cross-reactive mutant of diphtheria toxin (dLOS-CRM) vaccine candidate on pulmonary clearance following an aerosol challenge of mice with M. catarrhalis. Intranasal immunization with dLOS-CRM plus cholera toxin induced a significantly dose-dependent increase of immunoglobulin A (IgA) and IgG in the nasal wash, lung lavage fluid, saliva, and fecal extract. In addition, serum IgG, IgM, and IgA against LOS of M. catarrhalis were detected. LOS-specific antibody-forming cells were found in the nasal passages, spleens, nasally associated lymphoid tissues, cervical lymph nodes, lungs, and Peyer's patches using an enzyme-linked immunospot assay. The dLOS-CRM vaccine induced a significant bacterial clearance (70 to 90%) of both homologous and heterologous strains in the lungs compared to that observed in the controls (P < 0.01). Intriguingly, intranasal immunization with dLOS-CRM showed a higher level of bacterial clearance compared with subcutaneous injections with dLOS-CRM. These data indicate that dLOS-CRM induces specific mucosal and systemic immunity through intranasal immunization and also provides effective bacterial clearance. On the basis of these results, we believe that dLOS-CRM should undergo continued testing to determine whether it would induce protective immune response in humans.
The mucosal surfaces of the respiratory, genitourinary, and gastrointestinal tracts consist of an efficient physical barrier against environmental pathogens. However, a majority of bacterial and viral infections directly affect or enter the body through mucosal surfaces, and colonization at these sites is the first step in pathogenesis. Moraxella catarrhalis is a gram-negative human mucosal pathogen which causes middle ear infections in children as well as lower respiratory tract infections in adults with chronic pulmonary disease (8, 9, 22, 28). In young children, M. catarrhalis is one of the three major causes of otitis media (OM) along with Streptococcus pneumoniae and nontypeable Haemophilus influenzae. More than 80% of children are likely to experience at least one episode of OM by the age of 2 years. Recurrent or chronic OM can lead to hearing, speech, and/or language problems. The estimated cost from OM in the United States is $5 billion annually (23). In the elderly, especially those with chronic obstructive pulmonary diseases, M. catarrhalis can cause severe lower respiratory tract infections such as pneumonia that can be life threatening (38). Currently, the number of antibiotic-resistant strains of M. catarrhalis has significantly increased (4, 13).
Active immunization with an effective vaccine would be an efficient approach to prevent such infections (27). Efforts have therefore been made to evaluate surface antigens of M. catarrhalis such as outer membrane proteins (6, 11, 29, 30) and lipooligosaccharide (LOS) as candidate vaccines, which may elicit protective antibodies against M. catarrhalis infection. The LOS molecule, which is a major surface-exposed antigen of M. catarrhalis, is not only a possible virulence factor but also an attractive vaccine candidate (10, 14, 15, 17). Serum antibodies to LOS developed in patients with M. catarrhalis infections, and the convalescent-phase immunoglobulin G (IgG) anti-LOS from patients demonstrated bactericidal activity against M. catarrhalis strains (36, 38, 41). Furthermore, a mouse monoclonal antibody was bactericidal and enhanced bacterial clearance in a murine pulmonary challenge model (19). In addition, the serological properties of LOS in humans suggest a less variable structure of LOS. To date, only three major antigenic types of M. catarrhalis LOS can be distinguished, and more than 95% of 302 strains expressed one of three LOS serotypes (A, 61%; B, 29%; C, 5%) (43). Among them, strains of serotype A and C, but not serotype B strains, share the conserved epitopes in LOS molecule (14).
As a vaccine component, LOS is too toxic to be administrated in humans, while detoxified LOS (dLOS or hapten) is not immunogenic. Accordingly, in previous studies, we used the M. catarrhalis strain 25238 as a source of LOS (serotype A) coupled to a carrier protein (10). The resulting dLOS-protein conjugates demonstrated that systemic immunization with the vaccines induced the LOS immune responses and protected against challenges in a mouse pulmonary clearance model (17). Nevertheless, systemic immunization does not initiate mucosal immune responses, which may be important against mucosal infection. Protection at mucosal sites may be obtained by stimulation of the mucosa-associated lymphoid tissue, which elicits a systemic IgG response in addition to secretory IgA. IgA is thought to play an important role in preventing OM in humans (9, 26). Secretory IgA may inhibit the adherence and invasion of mucosal pathogens and neutralize the virulence of enzymes and toxins. Investigators have shown that a mucosal immunization regime of an intra-Peyer's patch (intra-PP) immunization, followed by an intratracheal boost with killed M. catarrhalis whole cells (24, 25) or its outer membrane protein CD (30), resulted in significant enhancement of pulmonary clearance of bacteria after an intratracheal challenge with live bacteria in a rat or mouse model. However, the intra-PP route is not a practical route for humans. In an attempt of using nasally or intranasally (i.n.) associated lymphoid tissue (NALT) immunization with killed M. catarrhalis resulted in an enhanced bacterial clearance in mouse lungs (16). In this study, therefore, we investigated whether i.n. immunization with a dLOS-conjugated vaccine but not whole cells would result in an effective immune response and/or potential protection in a mouse model. Time course and dose-effect studies by i.n. immunization were performed, i.n. and systemic immunizations were compared, and homologous and heterologous protections were examined.
(This work was presented in part at the 101st General Meeting of the American Society for Microbiology, Orlando, Fla., May 2001 [abstract D128].)
MATERIALS AND METHODS
Mice.
Female BALB/c mice (6 to 8 weeks of age) were obtained from Taconic Farms Inc. (Germantown, N.Y.). The mice were housed in an animal facility in accordance with National Institutes of Health guidelines under animal study protocol 1009-01.
Bacterial strains and culture conditions.
Strain 25238 (type A) was purchased from the American Type Culture Collection (Manassas, Va.). Strains 26404 and 26397 (types C and B) were obtained from the Culture Collection of the University of Göteborg, Department of Clinical Bacteriology, Göteborg, Sweden. Strain O35E was provided by E. J. Hansen (42). These strains were grown on chocolate agar at 37°C with 5% CO2 for 16 h. Three to five isolated colonies from each strain were then transferred onto new plates and incubated for 3.5 to 4 h (mid-logarithmic phase). The strains were adjusted in phosphate-buffered saline (PBS) (pH 7.2) containing 0.1% gelatin, 0.15 mM CaCl2, and 0.5 mM MgCl2 to the required CFU as determined from a plot of optical density (or 65% transmission) at 540 nm against viable counts.
Conjugate vaccine.
Purification of LOS from strain 25238, detoxification of the LOS, and conjugation of dLOS to a carrier, cross-reactive mutant (CRM9) of diphtheria toxin (31, 34), were performed (10). The composition of dLOS-CRM was 419 μg of dLOS and 222 μg of CRM per ml, with a molar ratio of dLOS to CRM of 40:1, based on an estimated Mr of 3,000 for dLOS, and Mr of 63,000 for CRM.
Immunizations.
(i) i.n. immunization. Mice were anesthetized (intraperitoneally) with 0.1 ml of 2% ketamine (Fort Dodge Laboratories, Inc., Fort Dodge, Iowa) and 0.2% xylazine (Miles Inc., Shawnee Mission, Kans.) in PBS. The animals were then allowed to inhale 10 μl of vaccine or saline that was slowly instilled by micropipette into both nares. The amount of vaccine preparations inhaled was formulated to contain 5 μg of dLOS-CRM (carbohydrate content) mixed with 1 μg of cholera toxoid (CT) (List Biological Laboratories, Inc, Campbell, Calif.) as an adjuvant. The control mice were also immunized i.n. with a mixture of 5 μg of dLOS, 2 μg of CRM, and 1 μg of CT or with 1 μg of CT in PBS. All mice were given a total of four doses at 1-week intervals, with the last immunization 1 week before bacterial challenge or sample collection.
(ii). s.c. immunization. Mice were immunized subcutaneously (s.c.) with 5 μg of conjugate vaccine in 0.2 ml of normal saline mixed with Ribi-700 adjuvant (containing 50 μg of monophosphoryl lipid A and 50 μg of synthetic trehalose dicorynomycolate; Corixa Corporation, Mamilton, Mont.). All mice were given a total of three injections at 2-week intervals, with the last injection 1 week before bacterial challenge or sample collection.
Collection of secretions and sera.
Saliva (∼100 μl) was collected first, from mice anesthetized with a mixture of ketamine and xylazine and then intraperitoneally. administered with 100 μl of 1-mg/ml pilocarpine (Sigma Chemical Co., St. Louis, Mo.) in PBS to stimulate salivation, using a transfer pipette (Becton Dickinson Labware, Franklin Lakes, N.J.). Then, the mice were euthanized with an overdose of methoxyflurane (Metophane; Mallinckrodt Veterinary Inc., Mundelein, Ill.), the nasal wash was obtained by flushing the nasal cavity from the pharynx through the nostrils 10 times with 200 μl of PBS (44). For the collection of the lung lavage fluid (also called bronchoalveolar lavage fluid), the trachea was exposed through the neck, a cannula was inserted in the trachea, and the lung lavage fluid was collected by instilling and recovering three times via the cannula with 1 ml of PBS (30). Fresh feces from the small intestines was suspended at a ratio of approximately 1:10 in PBS, supplemented with 0.05% NaN3 and protease inhibitor (10 μg/ml; Sigma). After being vigorously vortexed for 15 min and subjected to centrifugation, the extract supernatant was removed and aliquoted. Peripheral blood was obtained via the axillary artery. Blood samples were allowed to clot at 4°C and then centrifuged in a refrigerated centrifuge. Sera were removed and divided into aliquots. All samples were stored at −70°C until assayed.
Preparation of lymphocytes from different organs.
Lymphocytes were prepared from the spleens, the NALT, cervical lymph nodes (CLN), PPs, nasal passages (NP), and lungs (2, 12, 44). Mice were anesthetized and then bled. After exsanguination, the mouse palate with NALT was peeled from the rest of the nasal tissue and pooled into an ice-cold incomplete medium: RPMI 1640 containing l-glutamine, supplemented with 5% fetal bovine serum, 0.5% (vol/vol) antibiotic-antimycotic, gentamicin (20 μg/ml; Life Technologies Inc., Rockville, Md.), 5 × 10−5 M 2-mercaptoethanol, and 0.01 M HEPES (Sigma). Single cells were obtained from the spleens, PPs, CLN, lungs, and NP by pressing the organs through stainless-steel mesh or the frosted ends of two microscope slides in a 24-mm-diameter petri dish containing 5 ml of cold incomplete medium. Cell suspensions from the NALT, spleens, PPs, and CLN were washed twice with incomplete medium by centrifugation (200 × g for 8 min at 4°C). The lung and NP cell suspensions were layered on a Percoll (Sigma) density gradient after lysing the red blood cells. Viable lymphoid cells were recovered from the interface between the 40 and 75% Percoll solutions. Total cell yields were enumerated in a hemacytometer using 0.4% trypan blue to assess viability and kept in complete medium (10% fetal bovine serum).
ELISA.
The titers of LOS-specific antibodies in the nasal washes, saliva, lung lavage fluid, fecal extracts, and sera were determined by enzyme-linked immunosorbent assay (ELISA) (17) with 96-well Nunc-Immuno plates (MaxiSorp surface; Nalge Nunc International, Roskilde, Denmark) coated with strain 25238 LOS (10 μg/ml) in PBS (pH 7.4) containing 10 mM MgCl2 overnight at 4°C. A mouse antiserum against strain 25238 whole cells was used as a reference (10). Negative controls included presera and external secretions from naïve mice, giving optical density readings of less than 0.1. The antibody endpoint titer was defined as the highest dilution of sample giving an A405 twofold greater than that of presera or external secretions from naïve mice.
ELISPOT.
Enumeration of antibody-forming cells (AFCs) was performed by enzyme-linked immunospot assay (ELISPOT) (3, 45). A 96-well membrane-based plate (MultiScreen-HA plate, Millipore Corporation, Bedford, Mass.) was coated with 25238 LOS as described in ELISA. The plate was blocked with complete medium, and lymphocytes from spleens, NALT, CLN, PPs, NP, and lungs at appropriate concentrations were incubated at 37°C in 5% CO2 for 6 h. Isotype-specific biotinylated anti-mouse IgA, -G, or -M reagents (Sigma) were added at 4°C for an overnight incubation, followed by incubation with avidin-peroxidase conjugate (5 μg/ml) diluted in PBS containing 0.05% Tween 20 for 1 h at room temperature. After 4-chloro-1-naphthol-H2O2 (Sigma) was added, the plates were incubated for 5 to 8 min at room temperature, and the reaction was stopped by thoroughly washing plates with tap water. Spots were enumerated using a stereomicroscope equipped with a vertical white light (Zeiss, Jena, Germany).
Bacterial challenge.
Bacterial aerosol challenges were carried out one week after the last immunization in an inhalation exposure system (Glas-col, Terre Haute, Ind.) (18). Mice were challenged with 10-ml aliquots of live bacteria, 108 to 109 CFU/ml, in a nebulizer. At 6 h postchallenge, mouse lungs were removed and homogenized in 5 ml of PBS for 1 min at low speed in a tissue homogenizer (stomacher lab system model 80; Seward, London, United Kingdom). Each homogenate was diluted serially in PBS, and 50-μl aliquots of the homogenate and diluted samples were cultured on chocolate agar plates (Remel, Richmond, Va.). The bacterial colonies were counted after an overnight incubation at 37°C with 5% CO2.
Statistical analysis.
The viable bacteria were expressed as the geometric mean CFU of n independent observations ± the standard deviation (SD). Geometric means of reciprocal antibody titers were determined. Significance was determined by the two-tailed Student's t test.
RESULTS
Antibody responses against LOS of M. catarrhalis.
Significant LOS-specific antibody responses were elicited by i.n. immunization with dLOS-CRM (Table 1). LOS-specific IgA titers in external secretions and in serum were increased in animals immunized with dLOS-CRM. An increase of 56-fold in the nasal wash or 48-fold in the lung lavage fluid compared with PBS controls was detected. LOS-specific IgA titers in the nasal wash were also elevated in animals immunized with dLOS plus CRM (sevenfold), but they were significantly lower than those of animals immunized with dLOS-CRM (P < 0.01). A significant increase in LOS-specific IgG titers was detected in mice immunized with dLOS-CRM compared with the PBS control groups: serum (fivefold), nasal wash (fivefold), and lung lavage fluid (ninefold). LOS-specific IgM titers were significantly increased only in serum from mice immunized with dLOS-CRM (fivefold) or with dLOS plus CRM (threefold).
TABLE 1.
Effect of i.n. immunization with dLOS-CRM conjugate on LOS antibody responses and bacterial clearance of homologous strain 25238 in mice
| Immunization groupa | Antibody class | GMb antibody titers as determined by ELISA
|
Mean CFU of bacteria recovered/mouseb (range) | Bacterial reductionc (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Nasal wash | Lung lavage fluid | Saliva | Fecal extract | Serum | ||||
| dLOS-CRM | IgA | 169 (36-782)**d | 144 (41-501)** | 30 (7-124)** | 21 (3-159)* | 48 (14-167)** | 1,290 (555-2,998)** | 87 |
| IgG | 14 (6-31)** | 26 (8-83)** | 3 | 3 | 56 (8-412)** | |||
| IgM | 3 | 3 | 3 | 3 | 48 (14-167)** | |||
| dLOS+CRM | IgA | 21 (12-37)** | 8 (5-13) | 3 | 3 | 10 | 8,450 (6,804-10,494) | 12 |
| IgG | 3 | 3 | 3 | 3 | 10 | |||
| IgM | 3 | 3 | 3 | 3 | 26 (17-39)** | |||
| PBS | IgA | 3 | 3 | 3 | 3 | 10 | 9,656 (8,130-11,472) | 0 |
| IgG | 3 | 3 | 3 | 3 | 10 | |||
| IgM | 3 | 3 | 3 | 3 | 10 | |||
Mice, 16 per group, were i.n. immunized 4 times at 1-week intervals with either a mixture of 5 μg of dLOS-CRM and 1 μg of CT or a mixture of 5 μg of dLOS, 1 μg of CRM, and 1 μg of CT or with 1 μg of CT in 10 μl of PBS. One week after the last immunization, eight mice from each group were used to collect samples for antibody measurement and ELISPOT assay. The remaining eight mice from each group were challenged with 2 × 108 CFU of the M. catarrhalis strain 25238 per ml in a nebulizer. Mouse lungs were collected 6 h postchallenge.
Geometric mean (± SD range) of data from eight mice.
Compared with PBS group.
Statistical significance for comparison with PBS group: *, P < 0.05; **, P < 0.01.
LOS-specific AFCs in different lymphoid or nonlymphoid tissues.
The dominant isotype of LOS-specific AFCs was IgA, followed by small numbers of IgG and IgM. i.n. immunization with dLOS-CRM resulted in detection of LOS-specific IgA AFCs in all tissues tested, including distant organs such as PPs and spleen (Table 2). The majority of LOS-specific IgA AFCs were located in the NP (203 per 106 cells), followed by a small amount in other tested tissues, including lungs (52 per 106 cells). i.n. immunization with dLOS plus CRM elicited a few LOS-specific IgA AFCs in NP but not in other tissues. LOS-specific IgM AFCs were detected in the spleen and CLN. No LOS-specific AFCs were found in any tissues from mice immunized with PBS.
TABLE 2.
Anti-LOS AFCs elicited in different tissues of mice after dLOS-CRM conjugate immunization
| Immunization groupa | Antibody class | No. of AFCs/106 lymphoid cellsb
|
|||||
|---|---|---|---|---|---|---|---|
| NALT | NP | Spleen | Lung | CLN | PP | ||
| dLOS-CRM | IgA | 31 | 203 | 14 | 52 | 15 | 22 |
| IgG | 16 | 23 | 8 | 15 | 71 | 1 | |
| IgM | 5 | 5 | 21 | 3 | 116 | 7 | |
| dLOS+CRM | IgA | 0 | 4 | 0 | 0 | 0 | 0 |
| IgG | 0 | 0 | 0 | 0 | 0 | 0 | |
| IgM | 0 | 0 | 24 | 0 | 4 | 0 | |
| PBS | IgA | 0 | 0 | 0 | 0 | 0 | 0 |
| IgG | 0 | 0 | 0 | 0 | 0 | 0 | |
| IgM | 0 | 0 | 0 | 0 | 0 | 0 | |
See Table 1, footnote a.
The average number of AFC per 106 lymphoid cells from two experiments. The lymphoid cells were collected from eight mice.
Enhancement of bacterial clearance from murine lungs.
One week after the final immunization, mice were challenged with the homologous strain 25238. The number of bacteria recovered from lungs 6 h postchallenge was significantly reduced in the dLOS-CRM group (87%; P < 0.01) compared with the PBS group (Table 1). Immunization with dLOS plus CRM did not significantly enhance bacterial clearance compared with the PBS group.
The relationship between LOS-specific antibody titers and bacterial counts from mouse lungs was further analyzed in the nasal wash, lung lavage fluid, saliva, fecal extract, and serum from dLOS-CRM-immunized and PBS-immunized mice. A negative correlation was found in the nasal wash IgA (r = −0.85; P < 0.01) or IgG (r = −0.76; P < 0.05), lung lavage fluid IgA (r = −0.912; P < 0.001) or IgG (r = −0.68; P < 0.05), or serum IgA (r = −0.68; P < 0.05) or IgG (r = −0.80; P < 0.01).
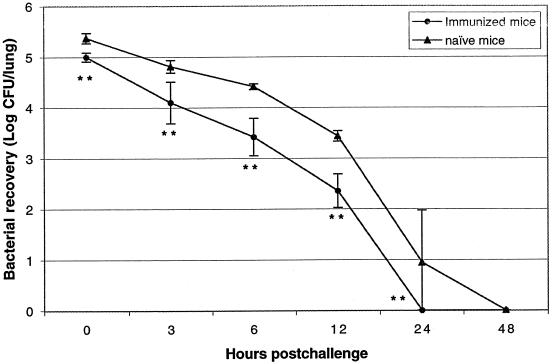
To define the kinetics of bacterial reduction in the immunized mice, the time course of bacterial clearance in the lungs was observed after challenging with strain 25238 (Fig. 1). Immunization with dLOS-CRM enhanced bacterial clearance in the lungs during the whole period and also reduced bacterial duration compared with natural clearance in the lungs of naïve mice (P < 0.01). Bacterial recovery became undetectable within 24 h postchallenge in the immunized mice, whereas naïve mice still carried a small amount of bacteria. The highest bacterial reduction occurred at 6 h (90%) and 12 h (92%) postchallenge, suggesting that 6 h postchallenge in mice retaining more bacteria is an optimal time point to observe the efficacy of immunization.
FIG. 1.
Time course of bacterial recovery from mouse lungs challenged with M. catarrhalis strain 25238 after i.n. immunization with dLOS-CRM. Mice received i.n.-administered 10-μl aliquots of PBS containing a mixture of 5 μg of dLOS-CRM and 1 μg of CT four times at 1-week intervals or were kept as naïve mouse controls. One week after the last immunization, all the mice were challenged (via aerosol) with 10 ml of M. catarrhalis strain 25238 (5 × 108 CFU/ml) in a nebulizer. Lungs were collected, homogenized, and cultured for bacterial counts at 0, 3, 6, 12, 24, and 48 h postchallenge. Bacterial recoveries from lungs are expressed as geometric means ± SD (error bars) from eight mice. **, P < 0.01 (for comparison with naïve mouse controls).
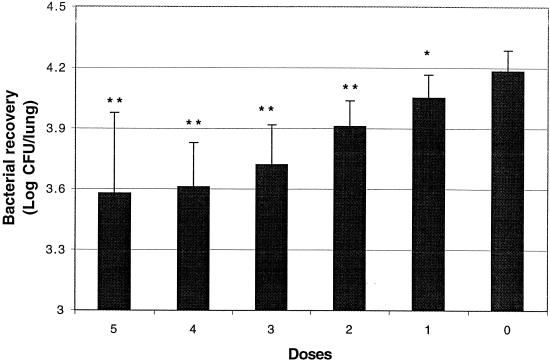
Effect of i.n. immunization with different doses of dLOS-CRM.
To determine what doses would further enhance pulmonary clearance, mice were i.n. immunized with one to five doses of dLOS-CRM plus CT and then challenged with the strain 25238 (Fig. 2). The bacterial counts in the lungs were reduced following the increase of doses, and significant bacterial clearance was found at each dose compared to that observed in naïve mice (P < 0.05 or P < 0.01). There was no significant difference on the bacterial clearance in mice given three, four, or five doses. The number of bacteria in the lungs decreased from 75 to 66% compared with the naïve mice and showed the highest variation of bacterial counts after five doses. In terms of LOS antibody responses, four doses elicited the highest LOS-specific IgA and IgG titers, especially in the nasal wash, lung lavage fluid, and serum (Table 3). Five doses did not result in further enhancement of either antibody responses or pulmonary clearance.
FIG. 2.
Comparison of protective effect induced by different doses of dLOS-CRM conjugate in mouse lungs challenged with the M. catarrhalis strain 25238. Mice were i.n. immunized at 1-week intervals with one to five doses consisting of 10 μl of PBS containing a mixture of 5 μg of dLOS-CRM and 1 μg of CT or were kept as naïve mouse controls. One week after last immunization, all the mice were challenged (via aerosol) with 10 ml of M. catarrhalis strain 25238 (5 × 108 CFU/ml) in a nebulizer, and their lungs were collected 6 h postchallenge. Bacterial recoveries from the lungs are expressed as geometric means + SD (error bars) from eight mice. Statistical significance for comparison with naïve mouse controls: **, P < 0.01; *, P < 0.05.
TABLE 3.
Dose pattern of LOS antibody responses elicited after i.n. immunization with dLOS-CRM conjugate
| No. of immunization dosesa | Antibody class | GMb antibody titers as determined by ELISA
|
||||
|---|---|---|---|---|---|---|
| Nasal wash | Lung lavage fluid | Saliva | Fecal extract | Serum | ||
| 5 | IgA | 140 (52-373)**c | 90 (23-346)** | 6 (2-17) | 15 (5-42)** | 90 (23-346)* |
| IgG | 12 (5-32)* | 19 (3-103)* | 3 | 5 (3-9) | 112 (18-682)* | |
| IgM | 3 | 4 (2-7) | 3 | 3 | 19 (11-35)* | |
| 4 | IgA | 225 (62-812)** | 156 (49-493)** | 12 (4-36)* | 25 (7-92)** | 130 (42-404)** |
| IgG | 43 (9-198)** | 36 (8-155)** | 8 (3-25) | 8 (3-25) | 324 (64-1,634)** | |
| IgM | 3 | 4 (2-6) | 3 | 3 | 17 (7-43) | |
| 3 | IgA | 43 (10-194)** | 43 (10-194)** | 7 (3-17) | 9 (2-54) | 36 (10-130) |
| IgG | 11 (2-60) | 16 (2-120) | 3 | 7 (3-17) | 130 (13-1,256)* | |
| IgM | 3 | 3 | 3 | 3 | 14 (8-25) | |
| 2 | IgA | 14 (4-45)* | 12 (8-19)** | 5 (3-11) | 7 (4-12)* | 17 (9-32) |
| IgG | 4 (2-6) | 4 (2-6) | 4 (2-6) | 8 (3-19)∗ | 30 (15-60)* | |
| IgM | 3 | 3 | 3 | 4 (2-8) | 21 (12-37)* | |
| 1 (or 0) | IgA | 3 | 3 | 3 | 3 | 10 |
| IgG | 3 | 3 | 3 | 3 | 10 | |
| IgM | 3 | 3 | 3 | 3 | 10 | |
Mice were i.n. immunized with one to five doses at 1-week intervals with 10 μl of PBS containing a mixture of 5 μg of dLOS-CRM and 1 μg of CT or were kept as naïve mouse controls.
Geometric mean (± SD range) of data from six mice.
Statistical significance for comparison with naïve mouse group: *, P < 0.05; **, P < 0.01.
Comparison of the effects of i.n. immunization and systemic immunization.
Previous work showed that systemic immunization with dLOS-protein conjugates could enhance pulmonary clearance of M. catarrhalis (17). Therefore, groups of mice were immunized with dLOS-CRM by either the s.c. or i.n. route. Ribi was used as an optimal adjuvant for the s.c. route, while CT was used for the i.n. route. As shown in Table 4, i.n. immunization achieved an 80% bacterial clearance in the lungs compared to that observed in naïve mice (P < 0.01) following an aerosol challenge with strain 25238, while s.c. application showed a 58% bacterial reduction (P < 0.05). The i.n. route showed a higher level of bacterial clearance compared to s.c. application, although there was no statistical difference between the two groups. However, when the same adjuvant CT was used for both routes, i.n. immunization showed significantly higher levels of bacterial clearance compared to s.c. injection (80 versus 40%; P < 0.05, data not shown). In terms of LOS antibody responses, different patterns of AFC responses were elicited in tissues by the two routes of application (Table 5). LOS-specific IgA AFCs were detected in all tissues from the i.n. immunization group, but not in the s.c. injection group. s.c. injections with dLOS-CRM plus Ribi adjuvant elicited higher levels of LOS-specific IgG AFCs in the spleen and CLN compared to that elicited by i.n. immunization with dLOS-CRM plus CT. Significant differences between the two groups were observed (P < 0.05 or P < 0.01) in IgA titers of the nasal wash, lung lavage, and serum (higher with i.n.); in IgG titers of the lung lavage fluid and serum; and in IgM titers of serum (higher with s.c.).
TABLE 4.
Effects of different immunizations routes with dLOS-CRM conjugate on LOS antibody responses and bacterial clearance in mice
| Routea | Antibody class | GMb titers of antibody against LOS of strain 25238 as determined by ELISA
|
Mean CFU of bacteria recovered/mouseb (range) | Bacterial reductionc (%) | ||||
|---|---|---|---|---|---|---|---|---|
| Nasal wash | Lung lavage fluid | Saliva | Fecal extract | Serum | ||||
| i.n. | IgA | 140 (77-225)**d | 111 (23-530)** | 14 (4-55) | 15 (5-42) | 37 (15-94)* | 4,192 (2,360-7,447)¶¶e | 80 |
| IgG | 37 (23-61) | 73 (13-396)* | 3 | 3 | 47 (17-124)** | |||
| IgM | 3 | 3 | 3 | 3 | 12 (8-20)** | |||
| s.c. | IgA | 3 | 3 | 3 | 3 | 10 | 9,095 (5,403-15,311)¶ | 58 |
| IgG | 12 (4-42) | 217 (36-1,318) | 3 | 6 (2-17) | 5,851 (962-35,587) | |||
| IgM | 3 | 3 | 3 | 3 | 522 (149-1,810) | |||
| Naïve control | IgA | 3 | 3 | 3 | 3 | 10 | 21,437 (16,000-28,723) | 0 |
| IgG | 3 | 3 | 3 | 3 | 10 | |||
| IgM | 3 | 3 | 3 | 3 | 10 | |||
Mice, 16 per group, were i.n. immunized four times at 1-week intervals with 10 μl of PBS containing a mixture of 5 μg of dLOS-CRM and 1 μg of CT or received s.c. injections three times at 2-week intervals with 200 μl of PBS containing 5 μg of dLOS-CRM mixed with Ribi adjuvant or were kept as naïve mouse controls. One week after the last immunization, eight mice from each group were used to collect samples for antibody measurement and ELISPOT assay. The remaining eight mice from each group were challenged with 5.0 × 108 CFU of the M. catarrhalis strain 25238 per ml in a nebulizer. Mouse lungs were collected 6 h postchallenge.
Geometric mean (± SD range) of data from eight mice.
Compared with naïve group.
Statistical significance for comparison with s.c. group: *, P < 0.05; **, P < 0.01.
Statistical significance for comparison with naïve mice: ¶, P < 0.05; ¶¶, P < 0.01.
TABLE 5.
Anti-LOS AFCs elicited in different tissues of mice by dLOS-CRM conjugate
| Routea | Antibody class | No. of AFCs/106 lymphoid cellsb
|
|||||
|---|---|---|---|---|---|---|---|
| NALT | NP | Spleen | Lung | CLN | PP | ||
| i.n. | IgA | 32b | 204 | 12 | 57 | 8 | 20 |
| IgG | 12 | 12 | 10 | 8 | 58 | 0 | |
| IgM | 2 | 2 | 28 | 0 | 117 | 8 | |
| s.c. | IgA | 0 | 0 | 0 | 0 | 0 | 0 |
| IgG | 0 | 4 | 218 | 4 | 184 | 0 | |
| IgM | 0 | 0 | 24 | 0 | 8 | 0 | |
| Naïve control | IgA | 0 | 0 | 0 | 0 | 0 | 0 |
| IgG | 0 | 0 | 0 | 0 | 0 | 0 | |
| IgM | 0 | 0 | 0 | 0 | 0 | 0 | |
See Table 4, footnote a.
The average number of AFCs per 106 lymphoid cells from two experiments. The lymphoid cells were collected from eight mice.
Heterologous bacterial clearance from the lungs.
To evaluate the heterologous protection of i.n. immunization on pulmonary clearance of M. catarrhalis, strain O35E (type A), 26397 (type B), or 26404 (type C) was used to challenge the animals (Tables 6 to 8). The protective effect of i.n. immunization was significant against strains O35E and 26404, with bacterial reduction of the strains in the lungs at 81 and 71%, respectively, compared to the PBS group (P < 0.01), but it was not significant against type B strain 26397, with bacterial reduction in the lungs at 38% (P > 0.05). The cross-reactivity of antibodies elicited by the dLOS-CRM from strain 25238 against the LOS of strain O35E (Table 6) or 26404 (Table 7) in the lung lavage fluid and serum was also analyzed. There was no significant difference between the titers of antibody against LOS of the serotype A or C strains. However, the titer of the cross-reactive antibody against LOS of the type B strain 26397 was significantly lower (Table 8).
TABLE 6.
Effect of i.n. immunization with dLOS-CRM conjugate on LOS antibody responses and bacterial clearance of the heterologous strain O35E (serotype A) in mice
| Immunization groupa | Antibody class | Anti-LOSb of:
|
Mean CFU of bacteria recovered/lungb (range) | Bacterial reduction (%)c | |||
|---|---|---|---|---|---|---|---|
| O35E
|
25238
|
||||||
| Lung lavage fluid | Serum | Lung lavage fluid | Serum | ||||
| dLOS-CRM | IgA | 210 (30-1,355)**d | 33 (8-138)* | 210 (30-1,355)** | 42 (11-165)** | 1,674 (900-3,115)** | 81 |
| IgG | 40 (10-215)** | 72 (14-366)** | 45 (10-295)** | 90 (12-669)** | |||
| IgM | 30 (10-80)** | 24 (10-57)** | 35 (15-90)** | 24 (10-57)** | |||
| PBS | IgA | 3 | 10 | 3 | 10 | 8,651 (6,374-11,740) | 0 |
| IgG | 3 | 10 | 3 | 10 | |||
| IgM | 3 | 10 | 3 | 10 | |||
Mice, 20 per group, were i.n. immunized four times at 1-week intervals with 10 μl of PBS containing a mixture of 5 μg of dLOS-CRM and 1 μg of CT or with 10 μl of PBS containing 1 μg of CT, respectively. One week after the last immunization, 10 mice from each group were used to collect samples for antibody measurement. The remaining 10 mice from each group mice were challenged with 2 × 108 CFU of the M. catarrhalis strain O35E per ml in a nebulizer, and mouse lungs were collected 6 h postchallenge.
Geometric mean (± SD range) of antibody ELISA titers of 10 mice.
Compared with PBS group.
Statistical significance for comparison with PBS group: *, P < 0.05; **, P < 0.01.
TABLE 8.
Effect of i.n. immunization with dLOS-CRM conjugate on LOS antibody responses and bacterial clearance of the heterologous strain 26397 (serotype B) in micea
| Immunization groupa | Antibody class | Anti-LOSb of:
|
Mean CFU of bacteria recovered/lungb (range) | Bacterial reduction (%)c | |||
|---|---|---|---|---|---|---|---|
| 26397
|
25238
|
||||||
| Lung lavage fluid | Serum | Lung lavage fluid | Serum | ||||
| dLOS-CRM | IgA | 30 (20-80)**d | 19 (11-34)* | 235 (35-1,530)** | 100 (20-494)** | 12,297 (5,926-25,518) | 38 |
| IgG | 20 (10-30)** | 14 (8-24) | 35 (20-60)** | 58 (10-328)** | |||
| IgM | 3 | 10 | 20 (10-49) | 17 (7-44) | |||
| PBS | IgA | 3 | 10 | 3 | 10 | 19,767 (16,169-24,166) | 0 |
| IgG | 3 | 10 | 3 | 10 | |||
| IgM | 3 | 10 | 3 | 10 | |||
See footnotes to Table 6. Here, the M. catarrhalis strain 26397 was used as a challenge organism, with 4.9 × 108 CFU per ml in a nebulizer.
TABLE 7.
Effect of i.n. immunization with dLOS-CRM conjugate on LOS antibody responses and bacterial clearance of the heterologous strain 26404 (serotype C) in mice
| Immunization groupa | Antibody class | Anti-LOSb of:
|
Mean CFU of bacteria recovered/lungb (range) | Bacterial reduction (%)c | |||
|---|---|---|---|---|---|---|---|
| 26404
|
25238
|
||||||
| Lung lavage fluid | Serum | Lung lavage fluid | Serum | ||||
| dLOS-CRM | IgA | 95 (25-390)**d | 24 (6-102)* | 130 (15-1,030)** | 52 (9-295)** | 1,990 (870-4,552)** | 71 |
| IgG | 30 (5-125)** | 47 (7-306)** | 40 (10-235)** | 125 (13-1,200)** | |||
| IgM | 20 (10-30)** | 17 (8-38)** | 20 (10-30)** | 19 (9-42)** | |||
| PBS | IgA | 3 | 10 | 3 | 10 | 6,878 (4,313-10,970) | 0 |
| IgG | 3 | 10 | 3 | 10 | |||
| IgM | 3 | 10 | 3 | 10 | |||
See footnotes to Table 6. Here, the M. catarrhalis strain 26404 was used as a challenge organism, with 2 × 108 CFU per ml in a nebulizer.
DISCUSSION
i.n. immunization of mice with dLOS-CRM conjugate vaccine elicited LOS-specific mucosal and systemic immune responses and resulted in significant clearance of M. catarrhalis from the mouse lungs. Our unpublished data also revealed that i.n. immunization with another conjugate, dLOS-tetanus toxoid, generated similar data to that of dLOS-CRM. This is the first report on the characteristics of mucosal immunity of M. catarrhalis LOS-based conjugate vaccines; however, other studies have shown similar results by capsular polysaccharide conjugates from S. pneumoniae, group B streptococci, or H. influenzae type b (Hib) (5, 20, 39).
To verify if the specific LOS immunity contributes to M. catarrhalis clearance from the mouse lungs, the correlation between LOS antibody levels and bacterial recoveries was analyzed. The results revealed a negative correlation between the nasal wash IgA or IgG levels, the lung lavage fluid IgA or IgG levels, the serum IgA or IgG levels, and the bacterial counts. These data indicate that these local and/or systemic specific LOS antibodies are associated with the bacterial clearance. We believe that secretory IgA in the lung lavage fluid and the nasal wash may play an important role in antibacterial immunity since high levels of IgA were detected and local IgA is thought to contribute in preventing OM in humans, perhaps by inhibiting the adherence of mucosal pathogens and neutralizing the virulence of enzymes and toxins (9, 26). i.n. immunization can deliver antigens directly to NALT, and thereby induce specific IgA antibodies in other mucosal secretions, including saliva, fecal extract, and the lung lavage fluid (2, 3, 12, 44, 45). Furthermore, T cells in NALT primed after i.n. immunization could migrate to mucosal effector sites to help IgA B cells to differentiate and mature into plasma cells (1, 31). Better understanding of the full mechanisms involved in this process still awaits the clarification of the functional role of the secretory IgA in the enhancement of M. catarrhalis clearance from the lungs after the application of the conjugate vaccines. It would be interesting to quantify and normalize mucosal IgA to compensate for differences in total IgA content and to determine the dominant IgG isotype that was stimulated with the dLOS-CRM conjugate. In addition, it will be important to observe if dLOS-CRM can elicit memory responses through i.n. immunization since an effective memory response was developed with an Hib polysaccharide-CRM conjugate through s.c. injection (21). The Hib-CRM induced a rapid increase in CRM-specific memory T cells and mixed Th1/Th2 cytokines, which may regulate the isotype and quantity of polysaccharide antibody.
It is worth noting that i.n. immunization with dLOS-CRM showed a tendency toward rapid bacterial clearance compared to s.c. injections. The following observations might lead to some explanations. Firstly, i.n. immunization induced both mucosal and systemic immune responses, especially when the IgA levels of the lung lavage fluid and the nasal wash were 37- to 47-fold higher than those of the s.c. injections. In contrast, s.c. injections only induced high levels of IgG in the lung lavage fluid, which was threefold higher than that induced by i.n. immunization. Secondly, LOS-specific IgA AFCs were found in the NP, lungs, spleens, NALT, CLN, and PPs from i.n. immunized mice but not in those from the s.c. immunized ones. The latter just showed high levels of LOS-specific IgG AFCs in the spleen and CLN. Thirdly, our data on s.c. injections with dLOS-CRM plus CT (the same adjuvant used in i.n. immunization) resulted in 40% bacterial reduction in the lungs compared to naïve mice, which was significantly lower than that of the i.n. immunization (80%). In addition, the i.n. route is simple and noninvasive, and administration devices are available (33, 40). Further investigations are, however, necessary to determine whether i.n. immunization with the conjugates will induce protective immune responses in humans.
Since strain 25238 LOS used for dLOS-CRM shares the common epitopes on all serotype A strains and has the mutual epitopes shared with serotype C strains (14), it was postulated that the dLOS-CRM would induce protective immunity against not only serotype A strains but also serotype C strains. The results of heterologous protection against the strain O35E (serotype A) or 26404 (serotype C) confirmed this hypothesis, indicating that a vaccine candidate including two types of LOSs (A and B) would have the potential of being able to produce protective immunity against majority of the pathogenic strains of M. catarrhalis.
Our study suggests that with an appropriate mucosal adjuvant and/or delivery system (32, 37), such conjugate vaccines and vaccination regimens may be effective at preventing OM and lower respiratory tract infections caused by M. catarrhalis in humans. At present, few adjuvants have yet been used in humans at mucosal surfaces, as many of the adjuvants are traditionally used in animal models. Although CT is one of the most potent mucosal adjuvants, it is too toxic to be administered in humans (32, 33). Future studies should be undertaken to compare different adjuvants such as monophosphoryl lipid A, CpG oligodeoxynucleotide, B subunit of CT, heat-labile enterotoxin mutants, proteasome, and cytokine (7, 33, 35, 40) and to identify a safe and effective mucosal adjuvant for human applications.
Acknowledgments
We are grateful to E. J. Hansen and J. C. McMichael for providing M. catarrhalis strains.
Editor: J. D. Clements
REFERENCES
- 1.Allen, J. S., G. Dougan, R. A. Strugnell. 2000. Kinetics of the mucosal antibody secreting cell response and evidence of specific lymphocyte migration to the lung after oral immunisation with attenuated S. typhimurium. FEMS Immunol. Med. Microbiol. 27:275-281. [DOI] [PubMed] [Google Scholar]
- 2.Asanuma, H., A. H. Thompson, T. Iwasaki, Y. Sato, Y. Inaba, C. Aizawa, T. Kurata, and S.-I. Tamura. 1997. Isolation and characterization of mouse nasal-associated lymphoid tissue. J. Immunol. Methods 202:123-131. [DOI] [PubMed] [Google Scholar]
- 3.Asanuma, H., C. Aizawa, T. Kurata, and S.-I. Tamura. 1998. IgA antibody-forming cell responses in the nasal-associated lymphoid tissue of mice vaccinated by intranasal, intravenous and/or subcutaneous administration. Vaccine 16:1257-1262. [DOI] [PubMed] [Google Scholar]
- 4.Bandak, S. I., M. R. Turnak, B. S. Allen, L. D. Bolzon, D. A. Preston, S. K. Bouchillon, and D. J. Hoban. 2001. Antibiotic susceptibilities among recent clinical isolates of Haemophilus influenza and Moraxella catarrhalis from fifteen countries. Eur. J. Clin. Microbiol. Infect. Dis. 20:55-60. [DOI] [PubMed] [Google Scholar]
- 5.Bergquist, C., T. Lagergard, and J. Holmgren. 1998. Antibody responses in serum and lung to intranasal immunization with Haemophilus influenzae type b polysaccharide conjugated to cholera toxin B subunit and tetanus toxoid. APMIS 106:800-806. [DOI] [PubMed] [Google Scholar]
- 6.Chen, D., J. C. McMichael, K. R. VanDerMeid, D. Hahn, T. Mininni, J. Cowell, and J. Eldridge. 1996. Evaluation of purified UspA from Moraxella catarrhalis as a vaccine in a murine model after active immunization. Infect. Immun. 64:1900-1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Del Giudice, G., M. Pizza, and R. Rappuoli. 1999. Mucosal delivery of vaccines. Methods 19:148-155. [DOI] [PubMed] [Google Scholar]
- 8.Enright, M. C., and H. McKenzie. 1997. Moraxella (Branhamella) catarrhalis: clinical and molecular aspects of a rediscovered pathogen. J. Med. Microbiol. 46:360-371. [DOI] [PubMed] [Google Scholar]
- 9.Faden, H. 2001. The microbiologic and immunologic basis for recurrent otitis media in children. Eur. J. Pediatr. 160:407-413. [DOI] [PubMed] [Google Scholar]
- 10.Gu, X.-X., J. Chen, S. J. Barenkamp, J. B. Robbins, C. M. Tsai, D. J. Lim, and J. Battey. 1998. Synthesis and characterization of lipooligosaccharide-based conjugates as vaccine candidates for Moraxella (Branhamella) catarrhalis. Infect. Immun. 66:1891-1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Helminen, M. E., I. Maciver, J. L. Latimer, L. D. Cope, G. H. McCracken, and E. J. Hansen. 1993. A major outer membrane protein of Moraxella catarrhalis is a target for antibodies that enhance pulmonary clearance of the pathogen in an animal model. Infect. Immun. 61:2003-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heritage, P. L., B. J. Underdown, A. L. Arsenault, D. P. Snider, and M. R. McDermott. 1997. Comparison of murine nasal-associated lymphoid tissue and Peyer's patches. Am. J. Respir. Crit. Care Med. 156:1256-1262. [DOI] [PubMed] [Google Scholar]
- 13.Hoban, D. J., G. V. Doern, A. C. Fluit, M. Roussel-Delvallez, and R. N. Jones. 2001. Worldwide prevalence of antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenza, and Moraxella catarrhalis in the SENTRY antimicrobial surveillance program, 1997-1999. Clin. Infect. Dis. 32:S81-S93. [DOI] [PubMed] [Google Scholar]
- 14.Holme, T., M. Rahman, P.-E. Jansson, and G. Widmalm. 1999. The lipooligosaccharide of Moraxella catarrhalis: structural relationships and antigenic properties. Eur. J. Biochem. 265:524-529. [DOI] [PubMed] [Google Scholar]
- 15.Holst, O., A. J. Ulmer, H. Brade, H.-D. Flad, E. T. Rietschel. 1996. Biochemistry and cell biology of bacterial endotoxins. FEMS Immunol. Med. Microbiol. 16:83-104. [DOI] [PubMed] [Google Scholar]
- 16.Hou, Y., W. G. Hu, T. Hirano, X.-X. Gu. 2002. A new intra-NALT route elicits mucosal and systemic immunity against Moraxella catarrhalis in a mouse challenge model. Vaccine 20:2375-2381. [DOI] [PubMed] [Google Scholar]
- 17.Hu, W.-G., J. Chen, J. F. Battey, and X.-X. Gu. 2000. Enhancement of clearance of bacteria from murine lungs by immunization with detoxified lipooligosaccharide from Moraxella catarrhalis conjugated to proteins. Infect. Immun. 68:4980-4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hu, W.-G., J. Chen, F. M. Collins, and X.-X. Gu. 2000. An aerosol challenge mouse model for Moraxella catarrhalis. Vaccine 18:799-804. [DOI] [PubMed] [Google Scholar]
- 19.Hu, W.-G., J. Chen, J. C. McMichael, and X.-X. Gu. 2001. Functional characteristics of a protective monoclonal antibody against serotype A and C lipooligosaccharides from Moraxella catarrhalis. Infect. Immun. 69:1358-1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jakobsen, H., D. Schulz, M. Pizza, R. Rappuoli, and I. Jónsdóttir. 1999. Intranasal immunization with pneumococcal polysaccharide conjugate vaccines with nontoxic mutants of Escherichia coli heat-labile enterotoxins as adjuvants protects mice against invasive pneumococcal infections. Infect. Immun. 67:5892-5897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kamboj, K. K., C. L. King, N. S. Greenspan, H. L. Kirchner, and J. R. Schreiber. 2001. Immunization with Haemophilus influenzae type b-CRM (197) conjugate vaccine elicits a mixed Th1 and Th2 CD4+ T cell cytokine response that correlates with the isotype of antipolysaccharide antibody. J. Infect. Dis. 184:931-935. [DOI] [PubMed] [Google Scholar]
- 22.Karalus, R., and A. Campagnari. 2000. Moraxella catarrhalis: a review of an important human mucosal pathogen. Microb. Infect. 2:547-559. [DOI] [PubMed] [Google Scholar]
- 23.Klein, J. O. 2001. The burden of otitis media. Vaccine 19:S2-S8. [DOI] [PubMed] [Google Scholar]
- 24.Kyd, J. M., and A. W. Cripps. 1999. Killed whole bacterial cells, a mucosal delivery system for the induction of immunity in the respiratory tract and middle ear: an overview. Vaccine 17:1775-1781. [DOI] [PubMed] [Google Scholar]
- 25.Kyd, J., A. John, A. Cripps, T. F. Murphy. 2000. Investigation of mucosal immunization in pulmonary clearance of Moraxella (Branhamella) catarrhalis. Vaccine 18:398-406. [DOI] [PubMed] [Google Scholar]
- 26.McMichael, J. C. 2000. Progress toward the development of a vaccine to prevent Moraxella (Branhamella) catarrhalis infections. Microb. Infect. 2:561-568. [DOI] [PubMed] [Google Scholar]
- 27.McMichael, J. C. 2001. Vaccines for Moraxella catarrhalis. Vaccine 19:S101-S107. [DOI] [PubMed] [Google Scholar]
- 28.Murphy, T. F. 1996. Branhamella catarrhalis: epidemiology, surface antigenic structure, and immune response. Microbiol. Rev. 60:267-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy, T. F., A. L. Brauer, N. Yuskiw, E. R. McNamara, and C. Kirkham. 2001. Conservation of outer membrane protein E among strains of Moraxella catarrhalis. Infect. Immun. 69:3576-3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murphy, T. F., J. M. Kyd, A. John, C. Kirkham, and A. W. Cripps. 1998. Enhancement of pulmonary clearance of Moraxella (Branhamella) catarrhalis following immunization with outer membrane protein CD in a mouse model. J. Infect. Dis. 178:1667-1675. [DOI] [PubMed] [Google Scholar]
- 31.Neville, D. M., J. Scharff, and K. Srinivasachar. 1992. In vivo T-cell ablation by a holo-immunotoxin directed at human CD3. Proc. Natl. Acad. Sci. USA 89:2585-2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogra, P. L., H. Faden, and R. C. Welliver. 2001. Vaccination strategies for mucosal immune responses. Clin. Microbiol. Rev. 14:430-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O'Hagan, D. T., M. L. MacKichan, and M. Singh. 2001. Recent developments in adjuvants for vaccines against infectious diseases. Biomol. Eng. 18:69-85. [DOI] [PubMed] [Google Scholar]
- 34.Pavliakova, D., C. Chu, S. Bystricky, N. W. Tolson, J. Shiloach, J. B. Kaufman, D. A. Bryla, J. B. Robbins, and R. Schneerson. 1999. Treatment with succinic anhydride improves the immunogenicity of Shigella flexneri type 2a O-specific polysaccharide-protein conjugates in mice. Infect. Immun. 67:5526-5529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pizza, M., M. M. Giuliani, M. R. Fontana, E. Monaci, G. Douce, G. Gougan, K. H. Mills, R. Rappuoli, G. Del Giudice. 2001. Mucosal vaccine: non toxic derivatives of LT and CT as mucosal adjuvants. Vaccine 19:2534-2541. [DOI] [PubMed] [Google Scholar]
- 36.Rahman, M., T. Holme, I. Jonsson, and A. Krook. 1995. Lack of serotype-specific antibody response to lipopolysaccharide antigens of Moraxella catarrhalis during lower respiratory tract. Eur. J. Clin. Microbiol. Infect. Dis. 14:297-304. [DOI] [PubMed] [Google Scholar]
- 37.Ryan, E. J., L. M. Daly, and K. H. G. Mills. 2001. Immunomodulators and delivery systems for vaccination by mucosal routes. Trends Biotechnol. 19:293-304. [DOI] [PubMed] [Google Scholar]
- 38.Sethi, S., and T. F. Murphy. 2001. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-the-art review. Clin. Microbiol. Rev. 14:336-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shen, X., T. Lagergård, Y. Yang, M. Lindblad, M. Fredriksson, and J. Holmgren. 2000. Systemic and mucosal immune responses in mice after mucosal immunization with group B Streptococcus type III capsular polysaccharide-cholera toxin B subunit conjugate vaccine. Infect. Immun. 68:5749-5755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh, M., and D. O'Hagan. 1999. Advances in vaccine adjuvants. Nat. Biotechnol. 17:1075-1081. [DOI] [PubMed] [Google Scholar]
- 41.Tanaka, H., K. Oishi, F. Sonoda, A. Iwagaki, T. Nagatake, and K. Matsumoto. 1992. Biochemical analysis of lipopolysaccharides from respiratory pathogenic Branhamella catarrhalis strains and the role of anti-LPS antibodies in Branhamella respiratory infections. J. Jpn. Assoc. Infect. Dis. 66:709-715. [DOI] [PubMed] [Google Scholar]
- 42.Unhanand, M., I. Maciver, O. Ramilo, O. Arencibia-Mireles, J. C. Argyle, G. H. McCracken, and E. J. Hansen. 1992. Pulmonary clearance of Moraxella catarrhalis in an animal model. J. Infect. Dis. 165:644-650. [DOI] [PubMed] [Google Scholar]
- 43.Vaneechoutte, M., G. Verschraegen, G. Claeys, and A.-M. van den Abeele. 1990. Serological typing of Branhamella catarrhalis strains on the basis of lipooligosaccharide antigens. J. Clin. Microbiol. 28:182-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu, H.-Y., and M. W. Russell. 1997. Induction of mucosal and systemic immune responses by intranasal immunization using recombinant cholera toxin B subunit as an adjuvant. Vaccine 16:286-292. [DOI] [PubMed] [Google Scholar]
- 45.Wu, H.-Y., and M. W. Russell. 1997. Nasal lymphoid tissue, intranasal immunization, and compartmentalization of the common mucosal immune system. Immunol. Res. 16:187-201. [DOI] [PubMed] [Google Scholar]