Abstract
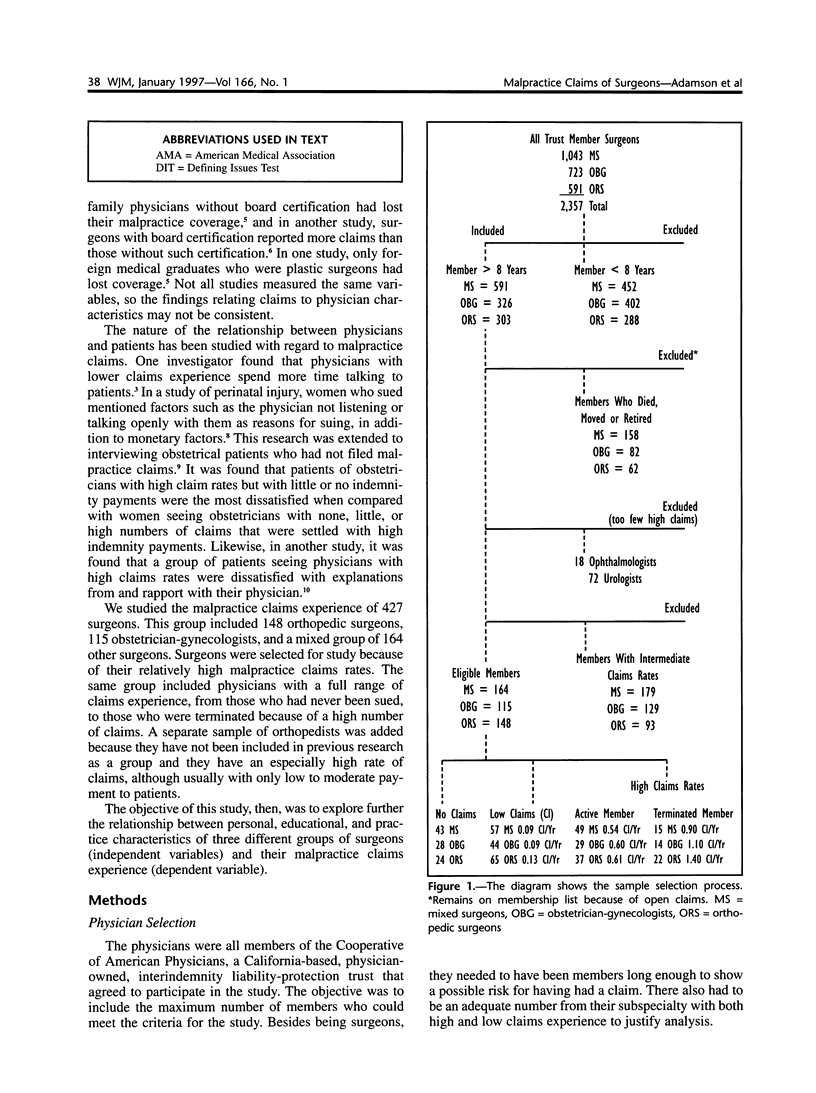
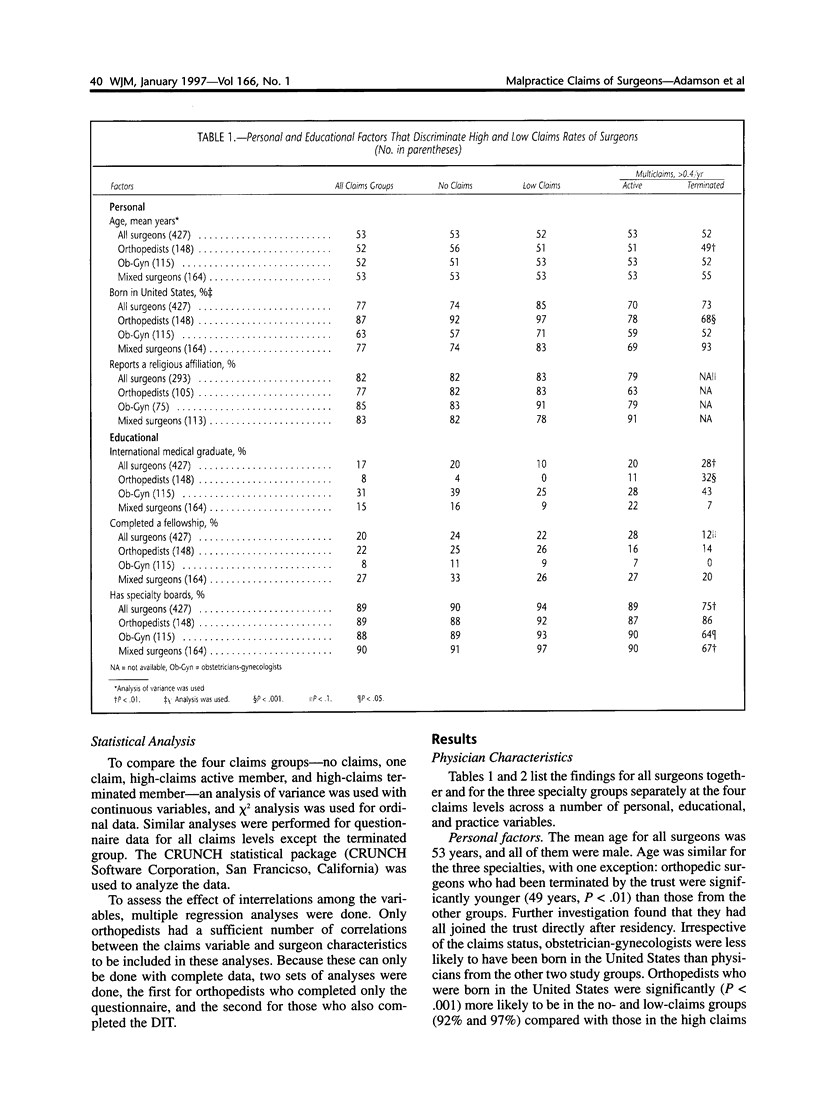
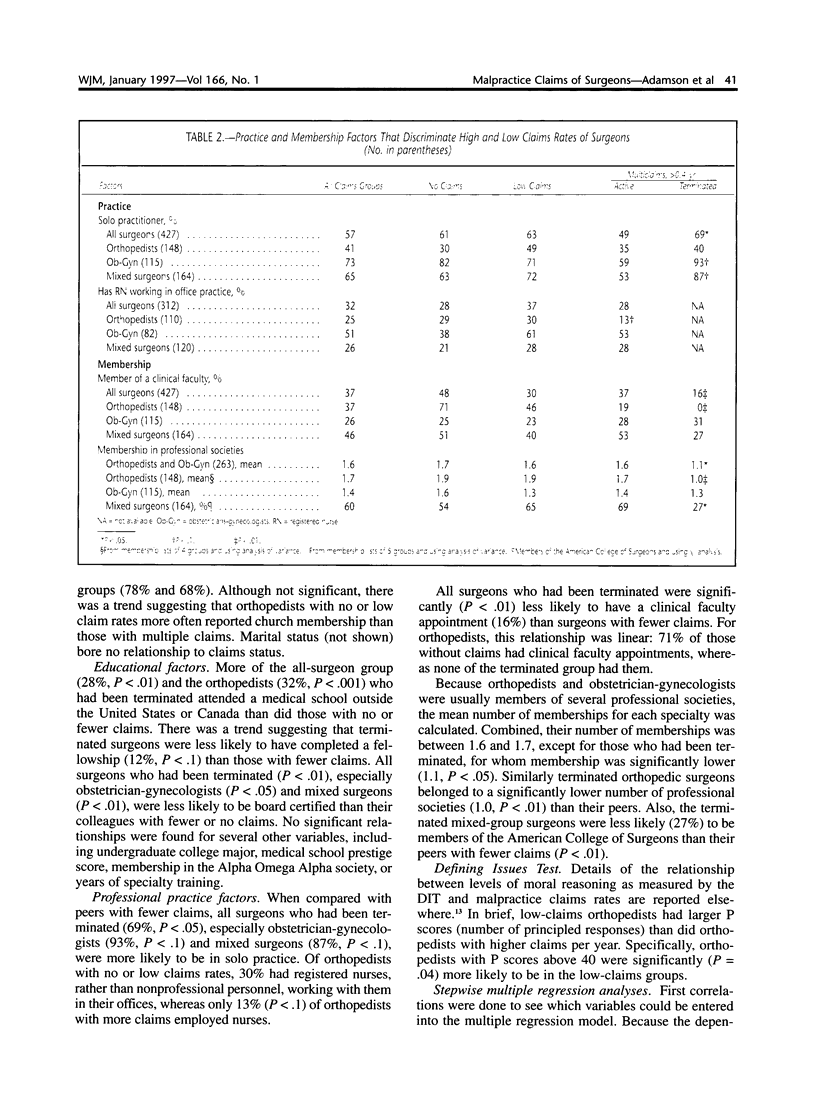
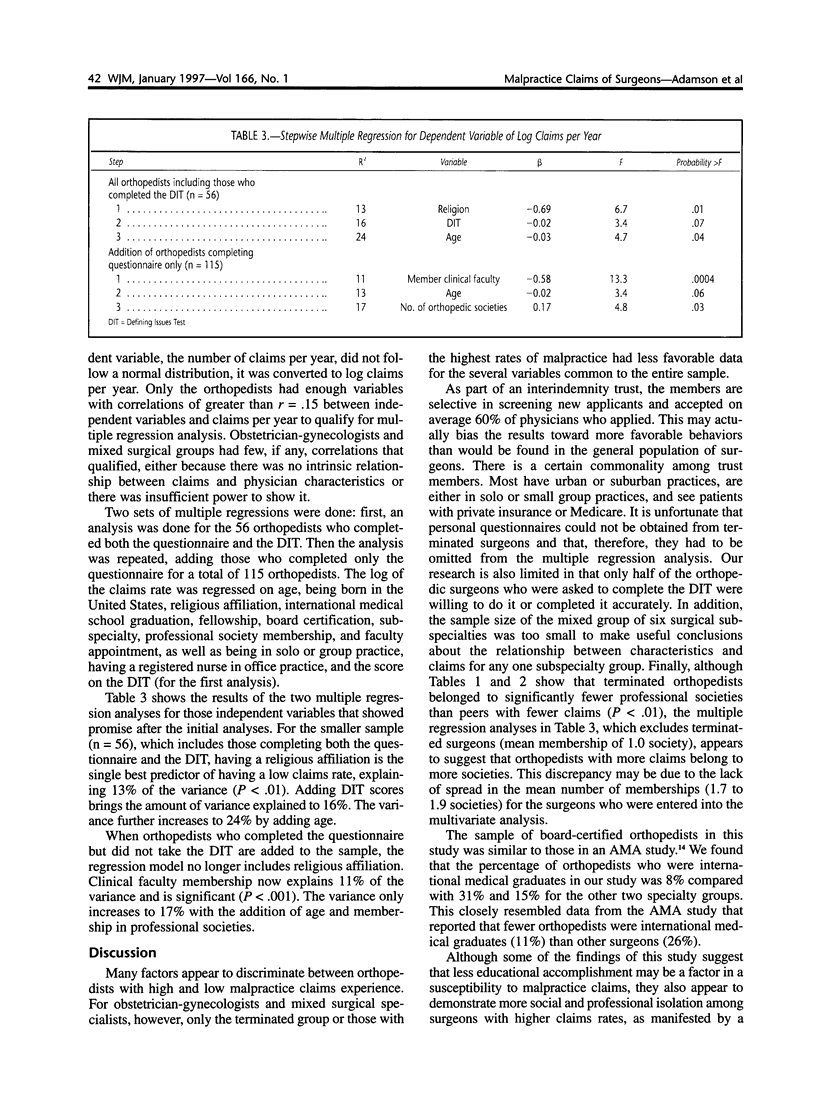
We studied the relationship of malpractice claims and the personal, educational, and practice characteristics of a sample of surgeons (n = 427). The surgeons were members of a physician-owned malpractice trust and represented all those who had fewer than 0.13 malpractice claims per year and those with more than 0.54 claims per year. Data are reported separately for orthopedic surgeons (148), obstetrician-gynecologists (115), and a mixed group of other surgeons (164). The last group included otolaryngologists, neurosurgeons, and general, vascular, thoracic, and plastic surgeons. We studied the relationship between the number of malpractice claims (ranging from no history of claims to those terminated from the trust because of high rates of claims) and the surgeon's personal, educational, and practice characteristics. The major differences were between the surgeons who were terminated because of a high number of claims and those with few or no claims. Terminated surgeons were less likely to have completed a fellowship, belong to a clinical faculty, be members of professional societies, be graduates of an American or Canadian medical school, have specialty board certification, or be in a group practice. The data also suggest that orthopedists with high numbers of claims may be less likely to have a religious affiliation or to have a registered nurse working in their office practice. These findings suggest that surgeons with lower claim rates may be more likely to manifest exemplary modes of professional peer relationships and responsible clinical behavior.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adamson T. E., Tschann J. M., Gullion D. S., Oppenberg A. A. Physician communication skills and malpractice claims. A complex relationship. West J Med. 1989 Mar;150(3):356–360. [PMC free article] [PubMed] [Google Scholar]
- Baldwin D. C., Jr, Adamson T. E., Self D. J., Sheehan T. J., Oppenberg A. A. Moral reasoning and malpractice. A pilot study of orthopedic surgeons. Am J Orthop (Belle Mead NJ) 1996 Jul;25(7):481–484. [PubMed] [Google Scholar]
- Baldwin L. M., Larson E. H., Hart L. G., Greer T., Lloyd M., Rosenblatt R. A. Characteristics of physicians with obstetric malpractice claims experience. Obstet Gynecol. 1991 Dec;78(6):1050–1054. [PubMed] [Google Scholar]
- Charles S. C., Gibbons R. D., Frisch P. R., Pyskoty C. E., Hedeker D., Singha N. K. Predicting risk for medical malpractice claims using quality-of-care characteristics. West J Med. 1992 Oct;157(4):433–439. [PMC free article] [PubMed] [Google Scholar]
- Charles S. C., Pyskoty C. E., Nelson A. Physicians on trial--self-reported reactions to malpractice trials. West J Med. 1988 Mar;148(3):358–360. [PMC free article] [PubMed] [Google Scholar]
- Charles S. C., Wilbert J. R., Kennedy E. C. Physicians' self-reports of reactions to malpractice litigation. Am J Psychiatry. 1984 Apr;141(4):563–565. doi: 10.1176/ajp.141.4.563. [DOI] [PubMed] [Google Scholar]
- Emanuel E. J., Emanuel L. L. Four models of the physician-patient relationship. JAMA. 1992 Apr 22;267(16):2221–2226. [PubMed] [Google Scholar]
- Hickson G. B., Clayton E. W., Entman S. S., Miller C. S., Githens P. B., Whetten-Goldstein K., Sloan F. A. Obstetricians' prior malpractice experience and patients' satisfaction with care. JAMA. 1994 Nov 23;272(20):1583–1587. [PubMed] [Google Scholar]
- Hickson G. B., Clayton E. W., Githens P. B., Sloan F. A. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992 Mar 11;267(10):1359–1363. [PubMed] [Google Scholar]
- Hutson M. M., Blaha J. D. Patients' recall of preoperative instruction for informed consent for an operation. J Bone Joint Surg Am. 1991 Feb;73(2):160–162. [PubMed] [Google Scholar]
- Kettelkamp D. B. Achilles' heel. J Bone Joint Surg Am. 1989 Aug;71(7):959–964. [PubMed] [Google Scholar]
- Kravitz R. L., Rolph J. E., McGuigan K. Malpractice claims data as a quality improvement tool. I. Epidemiology of error in four specialties. JAMA. 1991 Oct 16;266(15):2087–2092. [PubMed] [Google Scholar]
- Oppenberg A. A. A mandatory physician loss prevention seminar. J Healthc Risk Manag. 1993 Spring;13(2):7–14. doi: 10.1002/jhrm.5600130204. [DOI] [PubMed] [Google Scholar]
- Rockwell D. A., Peitone-Rockwell F. The emotional impact of surgery and the value of informed consent. Med Clin North Am. 1979 Nov;63(6):1341–1351. doi: 10.1016/s0025-7125(16)31646-7. [DOI] [PubMed] [Google Scholar]
- Schwartz W. B., Mendelson D. N. Physicians who have lost their malpractice insurance. Their demographic characteristics and the surplus-lines companies that insure them. JAMA. 1989 Sep 8;262(10):1335–1341. [PubMed] [Google Scholar]
- Shapiro R. S., Simpson D. E., Lawrence S. L., Talsky A. M., Sobocinski K. A., Schiedermayer D. L. A survey of sued and nonsued physicians and suing patients. Arch Intern Med. 1989 Oct;149(10):2190–2196. [PubMed] [Google Scholar]
- Stanton R. P. Making a complete orthopod. JAMA. 1990 Dec 5;264(21):2742–2742. [PubMed] [Google Scholar]


