Idiopathic condylar resorption (ICR) is a specific condition that affects the jaw joints (temporomandibular joints or TMJs) and most commonly occurs in teenage girls. It sometimes has been referred to as “cheerleaders syndrome,” because it frequently occurs in teenage girls participating in sports activities which, through minor or major trauma to the jaws, can initiate or exacerbate the condition. ICR is also known as idiopathic condylysis, condylar atrophy, and progressive condylar resorption. This is a well-documented but poorly understood disease process that occurs with a 9:1 female-to-male frequency ratio and rarely develops after the age of 20 years.
A number of local and systemic pathologies or diseases can cause mandibular condylar resorption. Local factors include osteoarthritis, reactive arthritis, avascular necrosis, infection, and traumatic injuries. Systemic connective tissue or autoimmune diseases that can cause condylar resorption include rheumatoid arthritis, psoriatic arthritis, scleroderma, systemic lupus erythematosus, Sjögren syndrome, ankylosing spondylitis, and others. ICR is a specific disease entity different from these other disease processes. Therefore, it has a specific diagnostic presentation and treatment protocol. ICR causes mandibular condylar resorption and, with loss of vertical dimension of the condyle, it can create occlusal (bite relationship) and musculoskeletal instability, resulting in the development of dentofacial deformities, TMJ dysfunction, and pain.
The occurrence of ICR has been identified by many authors as being associated with orthodontic treatment and orthognathic (i.e., corrective jaw) surgery (1–10). This association may, in fact, be coincidental and not reflect a specific cause-and-effect relationship. Recommended treatment for ICR at one time included splint therapy to minimize joint loading, nonloading orthodontic and orthognathic surgical procedures after the disease had been in remission 6 to 12 months, arthroscopic lysis and lavage, condylar replacement with a costochondral graft if the ICR could not be controlled or recurred, and maxillary surgery only to correct the occlusal deformity (5, 6, 11–14). None of these management strategies for ICR provides predictable, stable outcomes for the TMJ, optimizes function and aesthetic results, or eliminates pain. Wolford and Cardenas recently published a treatment protocol that effectively stops the disease process, provides reliable functional and aesthetic results, and eliminates or significantly reduces pain levels (15). This article presents the diagnostic factors for ICR, the specific treatment protocol, and the expected outcomes.
ICR PREDISPOSITION
Specific factors and preexisting facial morphologic characteristics significantly increase susceptibility to ICR. These factors include female sex; age range from 10 to 20 years, with a strong predilection for teenagers in their pubertal growth phase; high occlusal plane angle and mandibular plane angle (i.e., dolicocephalic) facial morphology (Figure 1a, 1b); and predominance of class II skeletal (retruded lower jaw) and occlusal relationships with or without open bite (Figure 1c). ICR rarely occurs in patients with low occlusal and mandibular plane angles (i.e., brachyocephalic) facial types or class III (lower jaw forward of the upper jaw) skeletal relationships.
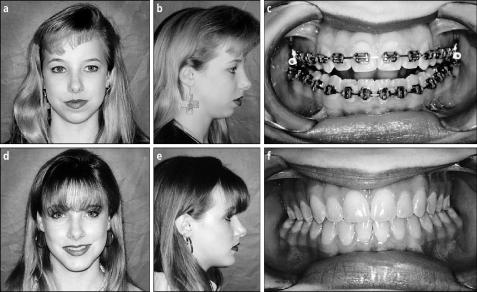
Figure 1.
Case 1. (a–c) This 15-year-old girl has active idiopathic condylar resorption. Notice the significantly retruded position of the mandible, high mandibular plane angle, and associated facial morphology. The presurgical occlusion demonstrates anterior open bite and a class II end-on cuspid occlusal relationship. (d–f) The same patient 3 years after surgical treatment of idiopathic condylar resorption with removal of hyperplastic synovial tissues, articular disc repositioning, and simultaneous double-jaw orthognathic surgery, demonstrating excellent stability.
PATHOGENESIS OF ICR
Although the specific cause of ICR has not been clearly identified, its strong predilection for teenage girls in their pubertal growth phase supports a theory of hormonal mediation. Estrogen receptors have been identified in the TMJs of female primates (16, 17); in human TMJ tissues of patients affected by TMJ symptoms such as TMJ pain, headache, myofascial pain, clicking and popping, and crepitation (18); and in arthritic knee joints (19). Estrogen is known to mediate cartilage and bone metabolism in the female TMJ. An increase in receptors may predispose to an exaggerated response to joint loading from parafunctional activity, trauma, orthodontics, or orthognathic surgery. I believe that progression of this disease is as follows: Hormones mediate biochemical changes within the TMJ, causing hyperplasia of the synovial tissues; this stimulates production of destructive substrates that initiate breakdown of the ligamentous structures that normally support and stabilize the articular disc in position. This breakdown allows the disc to become anteriorly displaced. The hyperplastic synovial tissue then assumes a position around the head of the condyle, further exposing the condyle to the substrates that create the resorptive phenomenon (Figure 2). The condyle shrinks in size in all 3 planes of space as a result of resorption occurring in the subcondylar bone without clinically apparent destruction of the fibrocartilage on the condylar head and roof of the fossa; this is unlike the arthritides, which destroy fibrocartilage by an inflammatory disease process. ICR can progress for a while and then go into remission or progress until the entire condylar head has been resorbed. In cases that go into remission, excessive joint loading (i.e., parafunctional habits, trauma, orthodontics, or orthognathic surgery) can reinitiate the resorption process later in life.
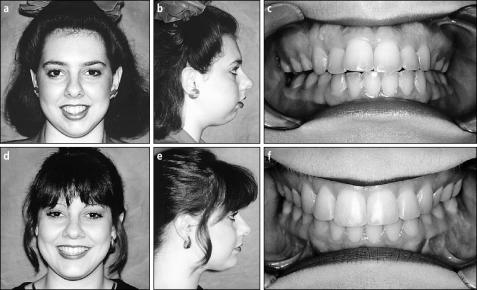
Figure 2.
Magnetic resonance imaging sagittal view of the left temporomandibular joint of the patient described in case 1 shows an anteriorly displaced articular disc (D) and an increased thickness of amorphous tissue composed of hyperplastic synovial tissue (hst) overlying the condyle (C). Notice the diminutive size of the condyle, which has some anterior beaking and loss of definition of the cortical bone over the head of the condyle.
CLINICAL EVALUATION AND DIAGNOSIS
A diagnosis of ICR can usually be made on the basis of patient history, clinical examination, and imaging. Patients may report progressive worsening of their occlusion and aesthetics, with or without TMJ symptoms and associated pain. When the disease process occurs bilaterally, it is usually accompanied by a relatively symmetric posterior shift of the mandible, development or worsening of the class II occlusal relationship (the lower teeth positioned excessively posteriorly relative to the upper teeth), and development of an anterior open bite (Figure 1c). In unilateral cases, or in bilateral cases with different rates of resorption, the following occurs: 1) the mandibular dental midline and chin shift toward the affected side; 2) an ipsilateral class II occlusion, crossbite, and posterior occlusal prematurities develop; and 3) an open bite develops on the contralateral side of the jaws. Although TMJ symptoms can be present, oftentimes they are mild or nonexistent. In fact, 25% of the patients in our study had no TMJ symptoms (15). Clicking and popping may be absent because the hyperplastic synovial tissue increases the joint space thickness, which provides a smooth transition onto the displaced disc during condylar translation. Rarely are other body joints involved in ICR of the TMJ. Laboratory studies may be indicated, particularly if other joints are involved, to evaluate for connective tissue or autoimmune diseases, which can also cause condylar resorption. No laboratory tests are specific for ICR.
Another common pathological TMJ development causing condylar resorption is reactive arthritis. Factors characteristic of reactive arthritis that help distinguish it from ICR include the following: 1) emergence generally in the late teens or after the age of 20 years; 2) decreased joint space between condyle and fossa; 3) erosion of the condyle and fossa with loss of fibrocartilage; 4) osteophyte formation; 5) anterior condylar beaking; 6) involvement of other joints; and 7) other systemic problems (e.g., problems of the female reproductive system, urinary tract, gastrointestinal tract, or chronic upper and lower respiratory infections). Reactive arthritis may be related to bacterial infections (i.e., Chlamydia, Mycoplasma) (20, 21) and requires different treatment considerations than ICR.
IMAGING FINDINGS
Four imaging studies are particularly helpful in diagnosis and treatment planning for ICR: lateral cephalometric radiographs, lateral cephalometric TMJ tomograms, panographic radiographs, and magnetic resonance imaging (MRI). Findings on lateral cephalometric radiographic films include skeletal and occlusal class II deformity (Figure 1a), anterior open bite, high occlusal plane angle, high mandibular plane angle, decreased vertical height of the ramus, possible overangulation of the lower incisors, and significant narrowing of the oropharyngeal airway in more severe cases, which may result in the development of sleep apnea symptoms (22). Serial lateral cephalometric radiographs demonstrate slow but progressive retrusion of the mandible during the active resorption phase of the disease. If the condition occurs unilaterally, then findings on lateral cephalometric radiographic images include unilateral skeletal and occlusal class II deformity; vertical height difference at the mandibular inferior borders, ramus, and occlusal plane; and open bite on the unaffected jaw.
Cephalometric tomographic evaluation of the TMJs usually shows relatively normal or excessive joint space because of the hyperplasia of the synovial tissues within the joint. The involved condylar head will appear smaller in size; the degree of this size difference depends on the length of time since onset and the aggressiveness of the disease. The cortical bone on the head of the condyle may lose some integrity. Superimposition of serial cephalometric tomograms helps document the presence of active condylar resorption. Bone scans may be of no significant diagnostic benefit in ICR.
MRI is very helpful in the diagnostic process. Expected findings include decreased condylar size and volume; anterior disc displacement, with or without reduction on opening; extreme thinness or loss of continuity of cortical bone on the head of the condyle; and often thick, amorphous-appearing soft tissue occupying the space between the condyle and fossa (Figure 2). The degree of deformation and degenerative changes of the disc will depend on the length of time that the disc has been displaced. The surgeon must determine if the disc is salvageable and if the remaining condyle is adequate to withstand normal functional loading and stress forces.
SURGICAL FINDINGS
Surgery usually reveals an anterior or anteromedial displacement of the articular disc. The hyperplastic synovial tissue covers the condylar head. This tissue may appear amorphous in nature, with little vascular component and usually no inflammation. Examination of the condylar head and glenoid fossa usually reveals what appears to be intact fibrocartilage covering the structures, without evidence of erosion or osteophytic formation. The articular disc may or may not demonstrate significant deformation and degenerative changes, depending on the length of time that the disc has been displaced. Histological examination of the retrodiscal tissues demonstrates synovial hyperplasia. If the fibrocartilage is absent and erosion is present on the condyle and fossa, then the disease process is not ICR.
NEW SURGICAL TREATMENT PROTOCOL
Wolford and Cardenas developed the most effective and reliable method of treating ICR (15). The hyperplastic synovial tissue is removed from the joint, and the articular disc is repositioned and stabilized to the condyle by using a Mitek mini anchor (Mitek Products, Inc., Westwood, Mass) placed in the posterior aspect of the condylar head with two 0-Ethibond sutures (Ethicon Inc., Somerville, NJ) attached, functioning as artificial ligaments (23, 24) (Figure 4). Orthognathic surgery (i.e., surgical repositioning of the upper and lower jaws) is then done to correct the associated jaw and occlusal deformities. This treatment protocol effectively eliminates the TMJ pathology and corrects the functional and aesthetic dentofacial deformity with one surgical procedure. If surgeons prefer, the TMJ surgery can be done as a separate procedure from the orthognathic surgery, but the TMJ surgery must be done first. Attempting to treat ICR cases with orthognathic surgery alone strongly encourages further condylar resorption, redevelopment of functional and aesthetic deformities, worsening TMJ symptoms and dysfunction, and worsening pain and increases the patient's chance of requiring extensive additional surgery. Because most of these patients have retruded jaw structures and those with more severe disease are likely to have significant sleep apnea symptoms, the optimal functional and aesthetic results are often best achieved by a counterclockwise rotation of the maxilla and mandible. We previously described the facial characteristics of individuals with high occlusal plane angle facial morphology (25, 26). These facial characteristics are commonly seen in patients with ICR. Chemello et al demonstrated that counterclockwise rotation of the maxillomandibular complex is a very stable procedure in patients with healthy jaw joints (27). In our treatment protocol for ICR, the TMJ discs are surgically repositioned and stabilized, eliminating the disease process. With an adequate remaining condyle, the TMJ can withstand the loading of the counterclockwise rotation of the maxillomandibular complex.
Figure 4.
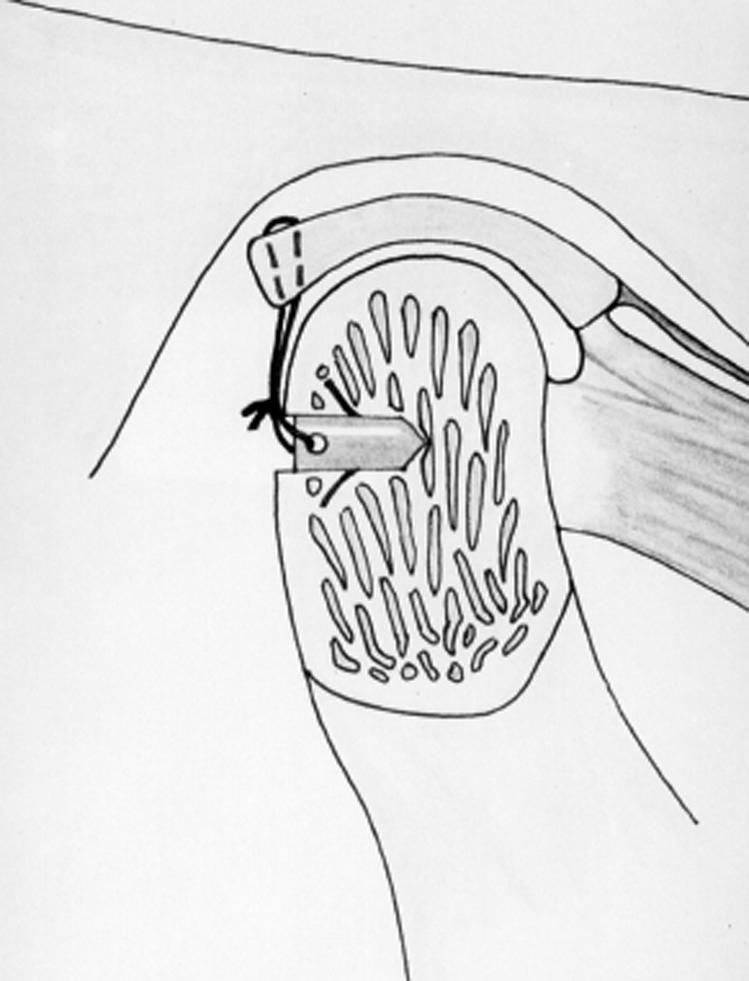
A sagittal cross-section through a right temporomandibular joint. A Mitek anchor with two 0-Ethibond sutures placed through the eyelet is inserted into the posterior head of the condyle. The 2 sutures are then attached to the posterior band of the articular disc and tied to secure the disc to the condylar head.
Arthroscopy and arthrocentesis techniques do not remove the hyperplastic synovial tissues of ICR, nor do they reposition the articular disc into a normal functional position. These techniques are predictably unsuccessful in treating this disease process. In ICR cases in which the disc is nonsalvageable but adequate condyle remains, the hyperplastic synovial tissue should be removed and the disc replaced with autogenous tissues. However, treatment results in such cases are far less predictable. A meniscectomy alone is not recommended, as this introduces other arthritic conditions. In more severe cases in which the condyle is nonsalvageable, condylar replacement may be necessary; appropriate techniques include a sternoclavicular joint graft, costochondral graft, or, my preference, the TMJ Concepts total joint prosthesis (TMJ Concepts Inc., Camarillo, Calif) (28, 29).
STABILITY OF RESULTS
Only one study in the literature shows highly reliable results for the management of patients with ICR. Wolford and Cardenas reported on 12 patients with ICR who had documented active condylar resorption at surgery and were treated by the same protocol presented here (15). The average age at surgery was 21 years (range, 14 to 36 years). In the older patients, the condition began in their teenage years, went into remission, and was reinitiated later on. The average presurgical rate of condylar resorption was 1.5 mm per year, indicating a slow but progressive disease process that caused the mandible to become more retruded at a rate of approximately 2.5 mm per year. The occlusal plane angle increased at a rate of 2° per year. Surgical intervention included removal of the hyperplastic synovial tissue, repositioning of the articular discs with Mitek anchors, and orthognathic surgery in which the mandible was advanced an average of 10.9 mm (range, 2 to 18 mm) and the occlusal plane angle decreased an average of –7.8° (range, –5° to –12°).
The postsurgical follow-up average was 33.2 months (range, 18 to 68 months). The average postsurgical condylar length change was +0.2 mm (range, –0.5 to +1.5 mm). During the postsurgery period, the mandible moved slightly forward, an average of +0.3 mm (range, –0.5 mm to +2 mm), and the average occlusal plane angle change was +0.04° (range, 0° to 0.5°). These changes from immediately after surgery to the longest follow-up were not statistically significant.
Five patients were younger than 16 years at the time of surgery, and these patients exhibited a modest amount of postsurgical condylar growth, with an average increase in condylar height of +0.43 mm (range, –0.1 to 1.5 mm). In all 12 patients, jaw function remained unchanged with no statistically significant difference between presurgical and postsurgical incisal openings (47 mm) or excursive movements (>7 mm). Decrease in pain after surgery, as measured on the visual analog pain scale (0 = no pain to 10 = worst pain) was statistically significant; the average presurgical pain score was 3.5 (range, 0 to 9), and the average postsurgical pain score was 0.7 (range, 0 to 4).
DISCUSSION
Patients predisposed to ICR are usually teenage girls in their pubertal growth phase; they typically have high occlusal plane angle facial types and class II skeletal and occlusal relationships. They are often candidates for orthodontics and orthognathic surgery even before the onset of the disease. Since ICR usually develops during pubertal growth, some patients are in orthodontic treatment at the onset of the disease. In most cases, ICR develops regardless of orthodontic or orthognathic surgical intervention. However, these procedures can increase loading or stress on the TMJ and can initiate or accelerate the rate of condylar resorption. In some ICR cases the pathology is self-limiting, with only moderate amounts of bone resorption, whereas in other cases the entire head and neck of the condyle can be resorbed. If the disease does go into remission, it can be easily reactivated by parafunctional habits, trauma, orthodontics, orthognathic surgery, or other factors that load or stress the joint.
In ICR, the ligaments that normally stabilize the articular disc in position are severely degenerated. Use of the Mitek anchor with artificial ligaments (22, 23) has significantly improved the stability of results in disc-repositioning procedures, particularly in treating ICR. A Mitek anchor supports 2 artificial ligaments (0-Ethibond sutures) threaded through the eyelet of the anchor and secured to the articular disc. The Mitek anchors are extremely stable and osseointegrate with the bone in the condylar head (30, 31). An important finding in our ICR study was that 5 of the 6 patients who were 16 years old or younger at the time of surgery demonstrated some modest postsurgical growth (15). This indicates a reversal of the disease process from resorption and progressive lower jaw retrusion to subsequent return of growth.
The best results in the management of ICR involve early detection of the disease process and early surgical management. The earlier ICR is treated, the more likely the following will occur: reduction of resorption of the condyle, thus maintaining a greater condylar dimension; reduction of distortion and degeneration of the articular disc; and improvement of postsurgical distribution of loading forces on the joint structures. The high predictability of treatment outcomes with this protocol for ICR substantiates the suggestion that early diagnosis and initiation of this specific treatment protocol yield the best functional, occlusal, and aesthetic success, with long-term stability and elimination of or significant reduction in pain.
Case 1
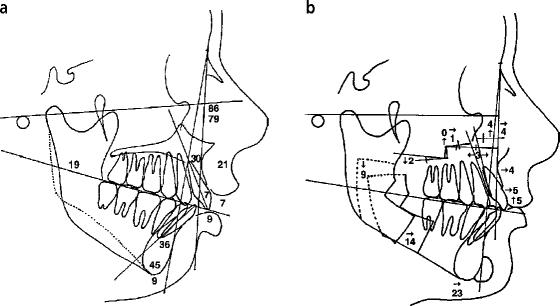
This 15-year-old girl, who was undergoing orthodontic treatment, was referred by her orthodontist because she was developing a significant jaw deformity; her mandible was becoming more retruded, and she was having difficulty chewing because her teeth didn't fit together (Figure 1a–1c). She had no pain, headaches, TMJ noises, or dysfunction. Her diagnoses included bilateral ICR of the TMJs, anteroposterior mandibular hypoplasia, maxillary posterior vertical hypoplasia, anteroposterior microgenia, high occlusal and mandibular plane angles, and class II occlusion with an open bite (Figure 3a). MRI showed significant loss of condylar volume bilaterally and anterior displacement of the articular discs (Figure 2). Serial cephalometric and tomographic analysis confirmed active condylar resorption. Her treatment included 1) presurgical orthodontics to continue to align and level the dental arches; 2) surgery (Figure 3b), including a) bilateral repositioning of the TMJ articular disc, ligament repair with Mitek anchors, and removal of hyperplastic synovial tissue; b) bilateral mandibular ramus osteotomies to advance the man dible in a counterclockwise direction; c) multiple maxillary osteotomies to advance, expand, and decrease the occlusal plane angulation by downgrafting the posterior aspect of the maxilla; and d) augmentation genioplasty; and 3) postsurgical orthodontics to finish and retain. The chin advanced 19 mm with the surgical treatment.
Figure 3.
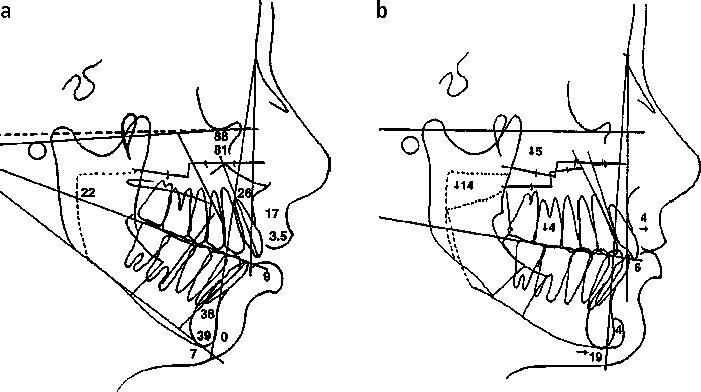
Case 1. (a) The common cephalometric appearance of idiopathic condylar resorption includes class II skeletal and occlusal relationships, anterior open bite, steep occlusal and mandibular plane angles, and overangulated lower incisors. (b) The surgical treatment objective (prediction tracing) demonstrates the orthognathic procedures required to achieve a good functional and aesthetic result, including maxillary and mandibular osteotomies with counterclockwise rotation of the occlusal plane and augmentation genioplasty.
Figure 1 shows the patient before and 3 years after surgery; the photographs reveal excellent stability and significant improvement in her functional and aesthetic facial balance. She has no pain or headache problems. Postsurgical condylar growth was 1 mm. (Orthodontics by Dr. Fred Spradley, Fort Worth, Tex.)
Case 2
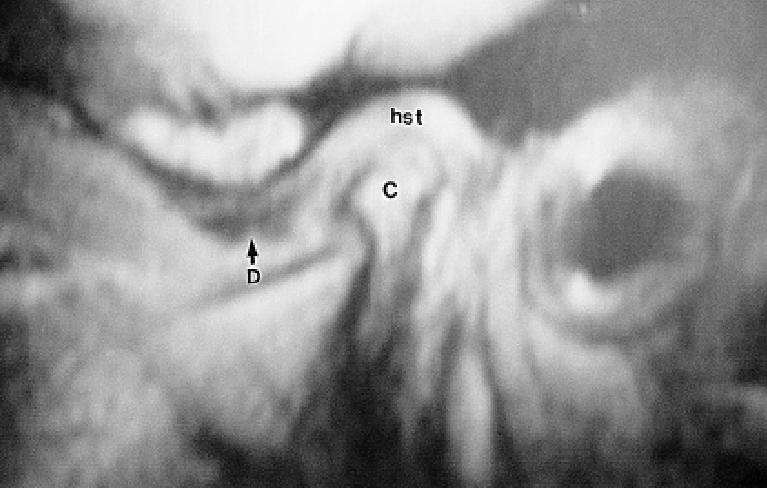
This 16-year-old girl was referred because her lower jaw began shifting to the left, developing a class II occlusion and an anterior open bite tendency (Figure 5a–c). She also complained of severe headaches, jaw and neck pain, and difficulty chewing. Her diagnosis included bilateral ICR of the TMJs, with the left side worse than the right side; mandibular anteroposterior deficiency; maxillary anterior vertical hyperplasia (Figure 6a); anteroposterior microgenia; and myofascial pain, TMJ pain, and headaches. MRI revealed bilateral anterior displacement of the articular discs and diminutive condylar size. Serial TMJ tomograms revealed progressive condylar resorption. Her visual analog pain scale score was 9 (0 = no pain, 10 = most severe pain). Treatment included 1) presurgical orthodontics to align and level the dental arches; 2) surgery (Figure 6b), including a) bilateral TMJ articular disc repositioning, ligament repair with Mitek anchors, and removal of hyperplastic synovial tissues; b) bilateral mandibular ramus osteotomies to advance the mandible in a counterclockwise direction; c) multiple maxillary osteotomies to move the anterior aspect superiorly and expand and level the occlusal plane; and d) augmentation genioplasty; and 3) postsurgical orthodontics to refine occlusion.
Figure 5.
Case 2. (a–c) This 16-year-old girl developed a worsening class II end-on occlusion, anterior open bite, and retruded mandible. She was diagnosed as having progressive idiopathic condylar resorption. (d–f) The same patient 6 years after surgical repair, showing good stability of the functional and aesthetic outcome; the idiopathic condylar resorption was eliminated.
Figure 6.
Case 2. (a) The cephalometric tracing shows the class II skeletal and occlusal relationship, with an open bite tendency and high occlusal and mandibular plane angles. (b) The surgical treatment objective demonstrates the proposed double-jaw orthognathic surgery, with counterclockwise rotation of the maxillomandibular complex, and genioplasty.
Figure 5 shows the patient before and 6 years after surgery, demonstrating excellent stability of results. The patient had a mansignificant decrease in her headache pain levels (visual analog pain score decreased from 9 before surgery to 3 after surgery) and no TMJ pain. The residual headaches are consistent with vascular or stress-related pain. At long-term follow-up, her right condyle had grown 1 mm, and her left condyle had grown 1.5 mm.
CONCLUSION
ICR can be treated very effectively with the specific treatment protocol described here, provided the articular discs and condyles are still salvageable. Other pathological conditions must be ruled out, because they may require different treatment protocols.
References
- 1.Worms FW, Speidel TM, Bevis RR, Waite DE. Posttreatment stability and esthetics of orthognathic surgery. Angle Orthod. 1980;50:251–273. doi: 10.1043/0003-3219(1980)050<0251:PSAEOO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Kerstens HC, Tuinzing DB, Golding RP, van der Kwast WA. Condylar atrophy and osteoarthrosis after bimaxillary surgery. Oral Surg Oral Med Oral Pathol. 1990;69:274–280. doi: 10.1016/0030-4220(90)90286-2. [DOI] [PubMed] [Google Scholar]
- 3.Moore KE, Gooris PJ, Stoelinga PJ. The contributing role of condylar resorption to skeletal relapse following mandibular advancement surgery: report of five cases. J Oral Maxillofac Surg. 1991;49:448–460. doi: 10.1016/0278-2391(91)90166-j. [DOI] [PubMed] [Google Scholar]
- 4.De Clercq CA, Neyt LF, Mommaerts MY, Abeloos JV, De Mot BM. Condylar resorption in orthognathic surgery: a retrospective study. Int J Adult Orthod Orthognath Surg. 1994;9:233–240. [PubMed] [Google Scholar]
- 5.Arnett GW, Tamborello JA. Progressive class II development: female idiopathic condylar resorption. Oral Maxillofac Surg Clin North Am. 1990;2:699–716. [Google Scholar]
- 6.Crawford JG, Stoelinga PJ, Blijdorp PA, Brouns JJ. Stability after reoperation for progressive condylar resorption after orthognathic surgery: report of seven cases. J Oral Maxillofac Surg. 1994;52:460–466. doi: 10.1016/0278-2391(94)90341-7. [DOI] [PubMed] [Google Scholar]
- 7.Schellhas KP, Wilkes CH, Fritts HM, Omlie MR, Lagrotteria LB. MR of osteochondritis dissecans and avascular necrosis of the mandibular condyle. AJR Am J Roentgenol. 1989;152:551–560. doi: 10.2214/ajr.152.3.551. [DOI] [PubMed] [Google Scholar]
- 8.Copray JCVM, Jansen HWB, Duterloo HS. The role of biomechanical factors in mandibular condylar cartilage growth and remodeling in vitro. In: McNamara JA Jr, editor. Craniofacial Growth Series, Center for Human Growth and Development. Ann Arbor, Mich: University of Michigan; 1984. [Google Scholar]
- 9.Will LA, West RA. Factors influencing the stability of the sagittal split osteotomy for mandibular advancement. J Oral Maxillofac Surg. 1989;47:813–818. doi: 10.1016/s0278-2391(89)80039-4. [DOI] [PubMed] [Google Scholar]
- 10.Huang CS, Ross RB. Surgical advancement of the retrognathic mandible in growing children. Am J Orthod. 1982;82:89–103. doi: 10.1016/0002-9416(82)90488-2. [DOI] [PubMed] [Google Scholar]
- 11.Merkx MA, Van Damme PA. Condylar resorption after orthognathic surgery. Evaluation of treatment in 8 patients. J Craniomaxillofac Surg. 1994;22:53–58. doi: 10.1016/s1010-5182(05)80297-5. [DOI] [PubMed] [Google Scholar]
- 12.Huang YL, Pogrel MA, Kaban LB. Diagnosis and management of condylar resorption. J Oral Maxillofac Surg. 1997;55:114–119. doi: 10.1016/s0278-2391(97)90222-6. [DOI] [PubMed] [Google Scholar]
- 13.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion— idiopathic condylar resorption. Part I. Am J Orthod Dentofacial Orthop. 1996;110:8–15. doi: 10.1016/s0889-5406(96)70081-1. [DOI] [PubMed] [Google Scholar]
- 14.Arnett GW, Milam SB, Gottesman L. Progressive mandibular retrusion— idiopathic condylar resorption. Part II. Am J Orthod Dentofacial Orthop. 1996;110:117–127. doi: 10.1016/s0889-5406(96)70099-9. [DOI] [PubMed] [Google Scholar]
- 15.Wolford LM, Cardenas L. Idiopathic condylar resorption: diagnosis, treatment protocol, and outcomes. Am J Orthod Dentofacial Orthop. 1999;116:667–677. doi: 10.1016/s0889-5406(99)70203-9. [DOI] [PubMed] [Google Scholar]
- 16.Aufdemorte TB, Van Sickels JE, Dolwick MF, Sheridan PJ, Holt GR, Aragon SB, Gates GA. Estrogen receptors in the temporomandibular joint of the baboon (Papio cynocephalus): an autoradiographic study. Oral Surg Oral Med Oral Pathol. 1986;61:307–314. doi: 10.1016/0030-4220(86)90407-x. [DOI] [PubMed] [Google Scholar]
- 17.Milam SB, Aufdemorte TB, Sheridan PJ, Triplett RG, Van Sickels JE, Holt GR. Sexual dimorphism in the distribution of estrogen receptors in the temporomandibular joint complex of the baboon. Oral Surg Oral Med Oral Pathol. 1987;64:527–532. doi: 10.1016/0030-4220(87)90025-9. [DOI] [PubMed] [Google Scholar]
- 18.Abubaker AO, Raslan WF, Sotereanos GC. Estrogen and progesterone receptors in temporomandibular joint discs of symptomatic and asymptomatic persons: a preliminary study. J Oral Maxillofac Surg. 1993;51:1096–1100. doi: 10.1016/s0278-2391(10)80448-3. [DOI] [PubMed] [Google Scholar]
- 19.Tsai CL, Liu TK, Chen TJ. Estrogen and osteoarthritis: a study of synovial estradiol and estradiol receptor binding in human osteoarthritic knees. Biochem Biophys Res Commun. 1992;183:1287–1291. doi: 10.1016/s0006-291x(05)80330-4. [DOI] [PubMed] [Google Scholar]
- 20.Henry CH, Hudson AP, Gerard HC, Franco PF, Wolford LM. Identification of Chlamydia trachomatis in the human temporomandibular joint. J Oral Maxillofac Surg. 1999;57:683–688. doi: 10.1016/s0278-2391(99)90432-9. [DOI] [PubMed] [Google Scholar]
- 21.Henry CH, Hughes CV, Gerard HC, Hudson AP, Wolford LM. Reactive arthritis: preliminary microbiologic analysis of the human temporomandibular joint. J Oral Maxillofac Surg. 2000;58:1137–1142. doi: 10.1053/joms.2000.9575. [DOI] [PubMed] [Google Scholar]
- 22.Mehra P, Wolford LM. Surgical management of obstructive sleep apnea. BUMC Proceedings. 2000;13:338–342. doi: 10.1080/08998280.2000.11927701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolford LM, Cottrell DA, Karras SC. Mitek Mini Anchor in maxillofacial surgery. In: Pelton AR, Hodgson D, Duerig T, editors. Proceedings of the First International Conference on Shape Memory and Superelastic Technologies. Monterey, Calif: MIAS; 1994. pp. 477–482. [Google Scholar]
- 24.Mehra P, Wolford LM. Use of the Mitek anchor in temporomandibular joint disc-repositioning surgery. BUMC Proceedings. 2001;14:22–26. doi: 10.1080/08998280.2001.11927726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolford LM, Chemello PD, Hilliard FW. Occlusal plane alteration in orthognathic surgery. J Oral Maxillofac Surg. 1993;51:730–740. doi: 10.1016/s0278-2391(10)80410-0. [DOI] [PubMed] [Google Scholar]
- 26.Wolford LM, Chemello PD, Hilliard F. Occlusal plane alteration in orthognathic surgery—Part I: Effects on function and esthetics. Am J Orthod Dentofacial Orthop. 1994;106:304–316. doi: 10.1016/S0889-5406(94)70051-6. [DOI] [PubMed] [Google Scholar]
- 27.Chemello PD, Wolford LM, Buschang PH. Occlusal plane alteration in orthognathic surgery—Part II: Long-term stability of results. Am J Orthod Dentofacial Orthop. 1994;106:434–440. doi: 10.1016/S0889-5406(94)70066-4. [DOI] [PubMed] [Google Scholar]
- 28.Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg. 1994;52:2–10. doi: 10.1016/0278-2391(94)90003-5. [DOI] [PubMed] [Google Scholar]
- 29.Wolford LM, Mehra P. Custom-made total joint prostheses for temporomandibular joint reconstruction. BUMC Proceedings. 2000;13:135–138. doi: 10.1080/08998280.2000.11927656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fields RT, Jr, Cardenas LE, Wolford LM. The pullout force for Mitek mini and micro suture anchor systems in human mandibular condyles. J Oral Maxillofac Surg. 1997;55:483–487. doi: 10.1016/s0278-2391(97)90697-2. [DOI] [PubMed] [Google Scholar]
- 31.Fields RT, Jr, Franco PF, Wolford LM. The osseointegration of Mitek mini suture anchors in the mandibular condyle. AAOMS 78th Annual Meeting and Scientific Sessions. J Oral Maxillofac Surg. 1997;55:92–93. [Google Scholar]