The word orthopaedic was coined by Nicolas Andry in 1741 from 2 Greek words: orthos, which means straight, and paedion, which means child. Andry's initial manuscript was entitled “Orthopaedia, or the art of correcting and preventing deformities in children.” Even a century ago, orthopaedics was still primarily involved with fractures, congenital and developmental anomalies, and the aftermath of infectious diseases, such as polio and tuberculosis. Orthopaedics is considered by many to be a spectacular success story, but its success came only after the 3 great discoveries of anesthesia, aseptic surgery, and x-rays.
The practice of orthopaedics in the USA 100 years ago can be gauged by the subjects of papers presented during the first 10 years of the American Orthopaedic Association, which was formed in 1887. Forty percent of the papers were on tuberculosis, 15% on clubfeet, and another 15% on developmental dysplasia of the hip, rickets, and polio combined. Life expectancy was short, and those who survived without infection or trauma might live to reach 60 years of age. Degenerative joint diseases were rare and were never diagnosed or treated.
DALLAS—100 YEARS AGO
The catalytic event leading to the 1903 establishment of the Texas Baptist Memorial Sanitarium, progenitor of Baylor University Medical Center (BUMC), was the spectacular visit of Dr. Adolf Lorenz of Vienna. Dr. Lorenz was known in Europe as “the bloodless surgeon of Vienna” (Figure 1). His specialty was the treatment of congenital dislocation of the hip, clubfoot, and other skeletal deformities with closed methods of treatment (as opposed to open or operative methods). His treatments consisted of manipulation and bracing. Dr. Lorenz (1854–1946) had trained as a general surgeon in Austria but became sensitive to the carbolic acid used as an antiseptic rinse. When he could no longer operate, he took up nonoperative orthopaedics and changed from being an advocate of open reduction of hip dysplasia to closed or bloodless reduction of dislocated hips. In retrospect, the forced and closed abduction of hips caused many cases of avascular necrosis. However, Dr. Lorenz attracted large audiences in his tour of the USA.
Figure 1.
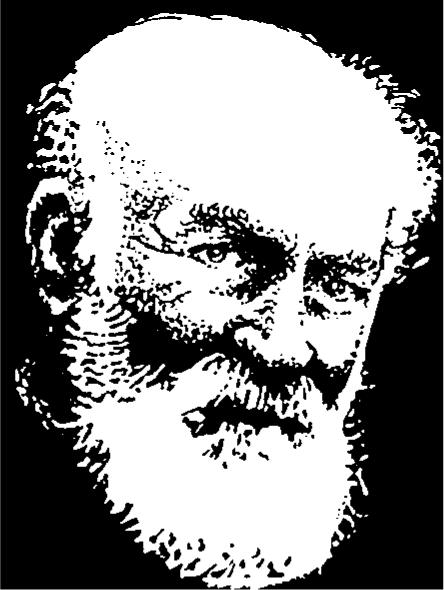
Dr. Adolf Lorenz.
Philip Armour, of the meatpacking family in Chicago, brought Dr. Lorenz to Chicago in 1902 to treat his child who had a congenital dislocation of the hip. Dr. Lorenz' visit was accompanied by a great deal of publicity, and he was invited to the American Medical Association (AMA) meeting in New Orleans in May 1903. Dr. C. M. Rosser, who had met Dr. Lorenz in Chicago, went to the AMA meeting in New Orleans with an invitation for Dr. Lorenz to visit Dallas under the auspices of the faculty of the newly founded University of Dallas Medical School and the Good Samaritan Hospital. His visit received a lot of press attention and stirred interest throughout the medical profession in the Southwest. Drs. E. H. Cary and E. A. Blount also played important roles in welcoming Dr. Lorenz to Dallas. He originally planned to be in Dallas for only 2 days, conducting 2 clinics a day at the Good Samaritan Hospital, also called the “Old Hopkins Place”—a 14-room home located at Junius and Hall streets. However, so many patients with crippling deformities sought Dr. Lorenz' care and so many doctors attended his clinics that he agreed to stay for a full week.
Following Dr. Lorenz' extended visit, Dr. E. H. Cary, who was then dean of the University of Dallas, pressed vigorously for a university affiliation for the medical school. Southern Methodist University, Trinity University, and Southwestern University all rejected his efforts for affiliation. However, with the help of his Baptist friends, the Reverend George Truett, Dr. J. B. Gambrell, Dr. R. C. Buckner, Colonel C. C. Slaughter, and President S. P. Brooks of Baylor University in Waco, he was able to form an affiliation with that institution. The University of Dallas then formally became Baylor University College of Medicine in 1903. The Good Samaritan Hospital and all its supplies and laboratory equipment were sold in October 1903 to the new corporation called the Texas Baptist Memorial Sanitarium. The sanitarium became part of Baylor University and was renamed Baylor University Hospital in 1920. Historically, therefore, the single most important event that led to the foundation of BUMC was the visit of the bloodless surgeon of Vienna, Dr. Adolf Lorenz.
THE EVOLUTION OF ORTHOPAEDIC SURGERY
During the next few years, no one practicing in the Dallas area could be specifically identified as an orthopaedic surgeon. General surgeons looked after fractures, and other orthopaedic problems were generally untreated. The onset of World War I in 1914 introduced new concepts in the treatment of trauma, and gradually orthopaedics emerged from under the shadow of general surgery. The first orthopaedic surgeon to practice in Dallas was Dr. W. B. Carrell, who founded the Carrell Clinic in 1917 and the Scottish Rite Hospital in 1921. From then on Dallas, and particularly Baylor, developed into a major orthopaedic referral center for North Texas.
In the interval between World War I and World War II, many notable achievements occurred in medicine worldwide, all of which affected orthopaedics. In 1928, Dr. Alexander Fleming discovered a mold called “penicillium,” which inhibited bacterial growth. In 1930, Dr. Lorenz Bohler (no relation to Adolf Lorenz) introduced the Kirschner intramedullary nail for the treatment of long bone fractures. This was a significant development in the concept of open reduction and internal fixation of fractures. Until 1931, the common hip fracture in the elderly patient was almost always a precursor of death. In that year, Dr. Smith Peterson developed his nail, and from then on subcapital fractures were stabilized and mobilized quickly. Baylor surgeons were the first to add a sideplate, which extended down the femoral shaft, to stabilize intertrochanteric hip fractures. This soon became the universally accepted way of treating these fractures. In 1937, Dr. Peterson also developed one of the early hip arthroplasties, which he called a “cup arthroplasty.” With the rapidly growing interest in the operative treatment of fractures and the possibility of treating scoliosis and congenital deformities surgically with less risk of infection, the specialty of orthopaedics began to expand rapidly. The American Academy of Orthopaedic Surgeons was formed in 1933, and the Texas Orthopaedic Association began in 1936.
In 1939, the second major world conflict, World War II, engulfed Europe, and in 1941 the USA was brought into the conflict with the war against Japan. In 1942, a large army unit went from Baylor to fight in that war. The unit was composed of nurses and doctors of all specialties, not just orthopaedics. Because of the magnitude of the conflict, many advances were made in the treatment of trauma. Antibiotics, developed in 1940 by Dr. Howard Florey based on the work of Fleming, were a significant factor that led to victory for the Allies. The control of sepsis was now a reality.
Progress was equally rapid in the postwar period. Artificial hips were developed—in 1946 the Judet hips and in 1950 the Moore-Thompson hip prosthesis. In 1951, the first knee replacement (a Waldius) was produced and in 1958, Dr. David Macintosh contributed the “hemiarthroplasty.” Also in 1958, Dr. Paul Harrington developed spinal instrumentation techniques for scoliosis. It was in this immediate postwar era that Dr. Jonas Salk developed a vaccine that eliminated polio; the last major polio epidemic occurred in 1955. Antibiotics and pasteurization of milk virtually eliminated bone and joint tuberculosis.
In 1958, the Association for the Study of Internal Fixation was founded in Switzerland with the purpose of improving the principles and materials used in the open reduction and internal fixation of fractures. A major improvement in artificial hips occurred in 1960 when Sir John Charnley combined metal with plastic to produce his artificial hip joint and introduced the concept of cementing the components in place.
In 1965, Dr. Robert Jackson introduced arthroscopy to North America, which was followed by the development of surgical techniques under endoscopic control. The success of arthroscopic surgery in the knee led to a major revolution in all surgical disciplines, with minimally invasive techniques being developed for a variety of procedures that previously had been accomplished only through large incisions.
In 1965, Medicare effectively changed the face of medicine and surgery in the USA. Numerous orthopaedic subspecialty societies were also founded in the 1960s, dealing with scoliosis research, hip surgery, sports medicine, arthroscopy, and so on— all established to lead to further improvements in their area of interest. This subspecialization of orthopaedics has resulted in fewer orthopaedic generalists but much better care for each specific problem, whether it be in the hip, shoulder, spine, knee, hand, or foot.
The practice of orthopaedics at BUMC reflected all of these changes.
ORTHOPAEDIC SURGEONS ON BUMC STAFF
Every orthopaedic surgeon who has held a staff position at BUMC is listed in the Table. Each one has had some impact on the development of Baylor as a major center for the treatment of musculoskeletal disorders. It is impossible to recognize every contribution, but several orthopaedists who helped elevate BUMC to its current position—whether as a pioneer or through research, administration, teaching, or exemplary patient care—are recognized below. Some of the more recent members of the BUMC family will undoubtedly make their mark in the future.
Table.
Orthopaedic surgeons past and present on BUMC staff
| Aldredge, George | Butters, Kenneth | Driver, Sim* | Hansen, Phillip E. | Luedke, Dennis C. | Schubert, Richard D. |
| Baker, John A. | Bywaters, Theodore, Jr. | Ellis, Paul | Head, William C. | Maale, Gerhard E. | Shirley, Richard A. |
| Beavers, Bruce | Bywaters, Theodore, Sr.* | Evans, J. Pat | Henry, David G. | MacMaster, Benzel | Snoots, Wynne |
| Beckering, Henry H.* | Callewart, Craig | Flatt, Adrian E. | Hopkins, Shelton G. | Mattson, Harold | Sobey, Terry |
| Blum, Jerald L. | Callewart, Robert, Sr. | Frederick, Hugh A. | Jackson, Robert W. | McCaskill, Bernie | Stephenson, Kenneth |
| Bonsell, Shawn | Carrell, Brandon, Jr.* | Freeman, Tandy R. | Jackson, Ruth* | Meyers, Marvin | Sutherland, Dan R. |
| Boswell, George W., Jr. | Carrell, W. B., Sr.* | Freudigman, Paul | Jackson, William K. | Miller, Mark | Tanamachi, Cary |
| Bozone, Richard T.* | Carter, Peter | Gill, John T. | James, George Truett* | Mitchell, Charles Dale | Thompson, Lewis R., Jr. |
| Britton, James | Chapman, D. Robert | Girard, Percy M.* | Jones, Richard E. | Mooney, Vert | Vandermeer, Robert D. |
| Brodsky, James W. | Chapman, Huntly G. | Glass, Kenneth D. | Key, James D. | Moore, Howard A. | Viere, Robert |
| Brooks, James G., Jr. | Cooper, Daniel E. | Glidewell, M. Gayle | Knight, Marvin* | Ough, James* | Ware, F. Leon* |
| Bruck, William A. | Cotton, Stonie R.* | Goldberg, Robert A. | Knight, Walter | Paradies, Louis* | Watkins, Margaret* |
| Buch, Richard G. | Curry, Eugene | Goodfried, M. Paul | Lancaster, J. Mack | Peters, Paul C., Jr. | Webb, David R., Jr. |
| Bucholz, Robert W. | Curtis, Richard Stephen | Gottschalk, Frank | Lang, Frank | Phalen, George* | Webb, Paul C. |
| Buford, Don | Czitrom, Andrei | Graham, Charles E. | Lankford, Lee L. | Prager, Bruce | Wenger, Dennis R. |
| Burandt, David M. | DiBella, Arnold | Graham, William A.* | Lawson, L. Ray | Rathjen, Kurt W. | Wharton, George W. |
| Burkhead, Wayne Z. | Dickhaut, Steven C. | Gunn, John B. | Legg, Eugene P.* | Sackett, James R. | Williams, Paul* |
| Butte, Felix* | Diliberti, Thomas | Halley, B. Clyde, Jr. | Loiselle, Albert O. | Schofield, Gerald W. | Wiltse, Leon L. |
| Dossett, Drew | Loyd, Ralph Daniel | Zehr, David |
*Deceased
OUTSTANDING BUMC ORTHOPAEDISTS
William Beall Carrell, MD (1883–1944)
Dr. W. B. Carrell (Figure 2) was born in Lawrenceburg, Tennessee, on December 21, 1883, the son of Dr. Charles A. and Virginia Carrell. Four years later, the family moved to Cedar Hill, Texas. His early education was therefore in Texas, and he graduated from Southwestern University in 1905. Yearning to follow in his father's footsteps, he enrolled in Southwestern University Medical College (later the Southern Methodist University Medical Department) in Dallas and received his medical degree in 1908. He conducted a general practice in surgery until 1917, when he joined the Medical Corps of the US Army, spending most of the next year and a half in the American Expeditionary Force in France. The experience gained in that conflict helped develop orthopaedics as a separate specialty, as traumatic injuries occurred in huge numbers. “Willie Bell,” as his friends knew him, gained a heightened awareness and a great deal of new knowledge regarding the treatment of trauma.
Figure 2.

Dr. William Beall Carrell.
He returned to Dallas following the war but shortly after that went back to Liverpool, England, for several months of further study with some of the orthopaedic leaders of that time. On his return to Dallas in 1919, Dr. Carrell was the first and only orthopaedic surgeon in the city. His immediate focus, however, was on the charitable care of children. Poliomyelitis or infantile paralysis was a highly contagious viral infection that had devastating aftereffects of paralysis. The disease was often fatal, and children were the prime victims. With the help of Samuel P. Cochran, a prominent Dallas businessman and head of the Freemasons in Texas, a children's aid committee was established to provide treatment for any needy child at Dr. Carrell's Orthopaedic Clinic free of charge. Mr. Cochran also convinced his Masonic colleagues to develop a new hospital for children, and in December 1921 construction of the Scottish Rite Hospital began. Dr. Carrell and subsequent surgeons who worked at Scottish Rite Hospital in the early days did so without any thought of financial recompense. Their surgical procedures were performed at Baylor Hospital and at Parkland Hospital. Dr. Carrell received the Linz Award in 1925 for “greatest service to the community” and “his unselfish, devoted, and humanitarian assistance to crippled children.”
In 1921, a young man named Dr. Sim Driver became the first orthopaedic resident at the Scottish Rite Hospital; his training was subsidized almost entirely by Dr. Carrell's personal pocket. He later became the interim chief of orthopaedics at Baylor University Hospital from 1944 to 1947 (Figure 3).
Figure 3.

Dr. Sim Driver.
The worst polio outbreak in Dallas history occurred in the summer of 1943 (Figure 4). Sister Kenny, well known for her postpolio rehabilitation techniques, came to Dallas during that outbreak. She spent several days making rounds at the Scottish Rite Hospital and gave instruction in her technique of moist heat applied to the affected body segments of the patients. Dr. Carrell was almost 60 years old at that time and suffered from emphysema. The heat and humidity of that summer coupled with stress and long hours of work began to take their toll. Air conditioning was just coming into use, and it is reported that Dr. Carrell would sometimes leave the hospital to be taken by an attendant to a nearby movie theater that had air conditioning. There, in the cool and darkness, he could rest for a few hours before returning to the hospital. Dr. Carrell died on February 23, 1944, naming his son, Dr. Brandon Carrell, and Dr. P. M. (Percy) Girard associate chiefs of staff.
Figure 4.
Polio victims at Scottish Rite Hospital, 1943. Photo courtesy of the Scottish Rite Hospital.
W. Brandon Carrell, MD (1911–1981)
Dr. Brandon Carrell (Figure 5) went to Southern Methodist University and then Northwestern Medical School. He did postgraduate work both at Northwestern Medical School and at Johns Hopkins University and Hospital. He did his orthopaedic training in Dallas, which was the first training program in the USA in which residents rotated through 3 major centers, Parkland Hospital, Texas Scottish Rite Hospital, and Baylor University Hospital. He was married in 1931 and joined the Carrell Clinic on January 31, 1939.
Figure 5.
Dr. Brandon Carrell and friend. Photo courtesy of the Scottish Rite Hospital.
On Dr. W. B. Carrell's death in 1944, Dr. Brandon Carrell was appointed chief surgeon at Texas Scottish Rite Hospital. His surgical skills were well recognized by his colleagues and resulted in a large private practice through the Carrell Clinic. He retired from private practice in 1960 to become the first full-time chief at Texas Scottish Rite. He was obliged to accept a $50,000 annual salary and a car due to Internal Revenue Service regulations. Prior to that, all surgeons at Scottish Rite had donated their time. He remained chief until his death in 1981 and was succeeded by the current chief, Dr. Tony Herring.
Ruth Jackson, MD (1902–1994)
Dr. Ruth Jackson (Figure 6) trained in orthopaedics in Iowa under Dr. Arthur Steindler. She then started her private practice in Dallas in 1932 and continued to work over the next 58 years until her retirement in 1990. She was one of the founders of the Texas Orthopaedic Association in 1936, along with Dr. W. B. Carrell, Dr. Clayton, and Dr. Schondfield. She took the examination of the American Board of Orthopaedic Surgery in 1937, becoming the first female member of the American Academy of Orthopaedic Surgeons. In 1939, she joined the staff of Baylor University Hospital and encouraged Dr. Margaret Watkins to train in orthopaedics. Dr. Watkins became the first resident to be trained at Baylor University Hospital and later became associated with Dr. Jackson in practice. In 1956, Dr. Jackson wrote the book The Cervical Syndrome, which was based on her experience in treating >15,000 patients with neck injuries. She said she had no desire to be famous; instead, she just did her work and “paid attention to the little things.”
Figure 6.

Dr. Ruth Jackson.
Her legacy in orthopaedics has been perpetuated by the formation of the Ruth Jackson Society, a society made up entirely of female orthopaedic surgeons. This society is increasingly active in clinical activities and in promoting research.
Dr. Ruth Jackson's generous contributions to the Department of Orthopaedic Surgery at BUMC enabled a major renovation of the department in late 1986. Although she was tiny in stature, her presence was always felt through her biting wit. She died peacefully at the age of 92, leaving an indelible mark on BUMC and orthopaedics.
George Truett James, MD (1919–1984)
Dr. George Truett James (Figure 7) was born in Dallas on March 5, 1919, and was the grandson of the Reverend Dr. George Truett, one of BUMC's founding fathers. He obtained his bachelor of arts degree at the University of Alabama and trained in medicine at Baylor University College of Medicine. He interned at Baylor University Hospital and did his residency in the Baylor– Scottish Rite–Parkland rotation. He was then invited to join the staff of the Carrell Clinic and remained with the clinic throughout his career. His contributions to BUMC included tours of duty as president of the medical staff and chairman of the medical board. He was a member of many societies and professional associations. He was a solid, kind man who, in the words of one of his colleagues, “was the glue that held the department together.” He was well loved by his colleagues and devoted patients, and it is fitting that in 1988, the service established itself as a true Institute of Orthopaedics, complete with teaching, research, and clinical services, and appropriately named the institute after Dr. James.
Figure 7.
Dr. George Truett James.
George M. Boswell, Jr., MD (1920–)
Dr. Boswell (Figure 8) was born in Dallas in 1920 and received his bachelor's degree in journalism at Texas Tech University, followed by a master's degree in psychology from The University of Texas. His adventurous spirit then led him to join the US Navy in 1940, prior to the onset of war against Japan. He rose to the rank of lieutenant commander and spent most of the war in the Pacific, where he served as the beach-landing officer in charge at Iwo Jima, Okinawa, and most of the other island battles. At the conclusion of the conflict, he made a major career change, entering medical school at the Southwestern Medical School (which subsequently became The University of Texas Southwestern Medical School). He was awarded his medical degree in 1950. While he was doing a general surgical residency, Dr. Marvin Knight encouraged him to enter orthopaedics, and since then he has made many contributions to this specialty.
Figure 8.

Dr. George M. Boswell, Jr.
Dr. Boswell joined the staff of Baylor University Hospital in 1952. In that year he and Dr. Harold Cheek performed the first anterior lumbar fusion done in the South. He also did the first cervical fusion and the first artificial knee at Baylor. For many years, he looked after staff of the Dallas police and fire departments and was commissioned as an officer in both of those organizations. His many outside interests include flying, gardening, and church activities.
In 1997, the Prothro-Perkins Foundation established a chair at BUMC in honor of Dr. Boswell, who dedicated the chair to “the perpetuation of the art and science of medicine in the practice of orthopaedic surgery and to the preservation of the traditional patient physician relationship.” Professor Boswell continues to see patients and even makes house calls.
L. Ray Lawson, MD (1925–)
Dr. Lawson (Figure 9) was born in 1925 and entered the army at the age of 18 years, becoming a medical corpsman. Following the war, he went to college and then to medical school at Baylor University College of Medicine in Houston, graduating in 1953. He had a general practice for 2 years and then entered a general surgical training program in Houston. In 1956, Dr. Charles Gregory came to Dallas as the professor of orthopaedics at The University of Texas Southwestern Medical School. Dr. Lawson was very impressed with Dr. Gregory both as a teacher and as an individual and quickly transferred from general surgery to orthopaedics to become one of the first residents to graduate through the new university program. His obvious talents led to a Fulbright scholarship, which enabled him to obtain further training in the United Kingdom under Lloyd Griffiths and Sir John Charnley.
Figure 9.
Dr. Ray Lawson.
On his return to Dallas, Dr. Lawson joined the Carrell Clinic and spent most of his time at the Texas Scottish Rite Hospital. Many cases of scoliosis were being referred to Scottish Rite, and Dr. Lawson developed a special expertise in treatment of these problems. He started the first clinic in scoliosis and invited Dr. Arthur Hodgson from Hong Kong to help develop the anterior spinal approaches. When spinal instrumentation became common, his work rapidly progressed. He continues to this day as the senior consultant at the Carrell Clinic and was recently awarded the prestigious Walter Blount Lifetime Achievement Award by the National Scoliosis Research Society.
John B. Gunn, MD (1931—)
Born in Columbus, Texas, in 1931, Dr. Gunn (Figure 10) obtained his early education in the Columbus public school system. He was valedictorian of his high school class and studied at Southern Methodist University for 1 year before transferring to complete his undergraduate degree at Stephen F. Austin State University. He then went on to earn his medical degree at The University of Texas Southwestern Medical School and did his residency training at the Baylor–Parkland–Scottish Rite program. Shortly after World War II, Dr. Gunn served in the US Navy as an orthopaedic surgeon for 2 years, attaining the rank of lieutenant commander and becoming chief of orthopaedics at the US Naval Hospital in Charleston, South Carolina.
Figure 10.
Dr. John Gunn.
In 1960, Dr. Gunn entered private practice with Orthopaedic Associates of Dallas, focusing his orthopaedic skills on surgery of the knee. He served as team doctor for the Dallas Cowboys and the Dallas Black Hawk hockey team and has become known as a pioneer in cementless joint replacements, knee ligament reconstructions, and simultaneous bilateral knee replacement surgeries.
Dr. Gunn has served in numerous societies and recently finished his active career with the great honor of being named president of the large and prestigious Southern Orthopaedic Association. On his retirement from active practice, his colleagues, friends, and patients contributed funds to establish the John B. Gunn Library of Orthopaedics at BUMC as a fitting tribute to his significant career.
J. Pat Evans, MD (1930—)
Dr. J. Pat Evans (Figure 11) was born in 1930 and raised in Dallas. He followed a path that eventually led him to become one of the more innovative and highly respected practitioners of sports medicine in the country. His career started with an early knee injury as a football player, which gave him great empathy for athletes with injuries. He graduated as a physical therapist in 1952 and worked for Dr. George Boswell in that capacity until Dr. Boswell encouraged him to study medicine. Following his graduation in medicine from The University of Texas Southwestern Medical School in 1959, he interned at Baylor University Medical Center and was immediately offered a staff position.
Figure 11.
Dr. J. Pat Evans.
Dr. Evans became a practice associate of Dr. Boswell but limited his practice to sports medicine; he was one of the first surgeons in the country to do only sports medicine, even before it was recognized as a subspecialty. He looked after members of the professional Dallas Cowboys football team along with Dr. Marvin Knight from 1970 to 1989 and was the team physician for the professional Mavericks basketball team from 1980 to 1992.
After several years, however, Dr. Evans became somewhat disillusioned with the attitude of the modern professional athlete, who seemed to care more about the financial benefits than the sport itself. He recognized that true athletes, such as the rodeo cowboys, always wanted to participate, no matter how badly they were injured. He therefore arranged with the Justin Boot Corporation to help with the medical care of rodeo participants around the country. Soon, almost every rodeo in the West was covered by either a doctor or a physiotherapist, thus providing for the first time professional care for the serious injuries that some of these athletes sustained. Dr. Evans would treat them free of charge, as most rodeo performers could not afford health insurance.
Dr. J. Pat Evans was responsible for suggesting and promoting the development of the Tom Landry Sports Medicine and Research Center, which opened in 1990. Even today, it is one of the best sports medicine facilities in the world. He retired in 2000 to a new home in Colorado.
Theodore W. Bywaters, MD (1906–1999)
Born in Roxton, Texas, Dr. Bywaters attended The University of Texas and the University of Colorado prior to earning his medical degree in 1933 from the University of Michigan Medical School. He interned at Methodist Hospital in Houston and St. Paul Hospital in Dallas and returned to the University Hospital in Ann Arbor, Michigan, as an instructor in surgery before moving back to Dallas to establish his practice.
Dr. Bywaters practiced for 50 years in Dallas, retiring in 1988. He was a member of the American Medical Association, Central States Clinical Orthopaedics Society, American Academy of Orthopaedic Surgeons, and Texas Orthopaedic Association. He was succeeded by his son, Dr. Theodore Bywaters, Jr., who also was an attending staff surgeon at BUMC until his retirement from active practice in September 2000.
Percy Merritt Girard, MD (1898–1987)
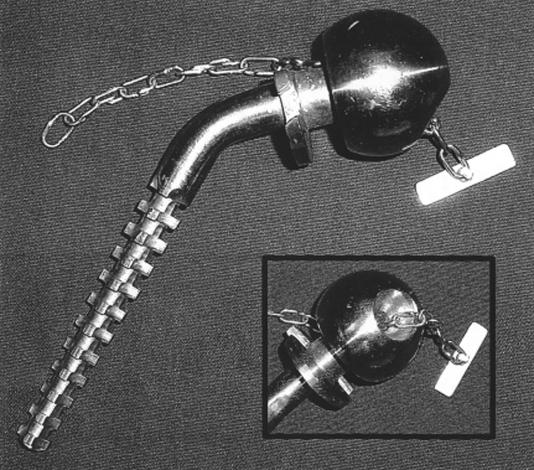
Dr. P. M. Girard's first career was as a mechanical engineer. He then went into medicine and orthopaedics and eventually became associate chief of staff at the Scottish Rite Hospital (along with Dr. Brandon Carrell) and professor of orthopaedic surgery at The University of Texas Southwestern Medical School. For many years, he designed all the equipment used at Scottish Rite Hospital for the treatment of polio patients and other disabled children. Later, he became famous for his prosthesis of the hip, which involved a toggle plate punched through the acetabulum and then tightened into position so that the femoral head could not dislocate (Figure 12). Dr. Girard was an exceptionally good trauma surgeon and also developed the Girard-Carrell screw that was used on occasion in severe compound fractures.
Figure 12.
The Girard hip, approximately 1950. Photo courtesy of Dr. G. M. Boswell.
Dorsey K. Barnes, MD (1911–1961)
Affectionately known as “Corky,” Dr. Barnes arrived in Dallas with a bad hip, presumably due to osteoarthritis. Because of this, he was unable to enter military service during World War II. He was one of the mainstays of the teaching program at BUMC and was very popular with the residents. A fund entitled “The Dorsey K. Barnes Fund” was established by Dr. Clyde Halley to perpetuate the opportunity for residents to attend national meetings.
Henry H. Beckering, MD (1907–1982)
Dr. Beckering was a large man who also was unable to enter military service during World War II. He came to Dallas from Iowa and worked for many years teaching residents at Parkland and in private practice with the Carrell Clinic.
Paul C. Williams, MD (1900–1978)
Dr. Williams came to Dallas from Michigan and entered practice with Dr. Ted Bywaters, Sr. He had an interest in the lumbar spine due to his own significant back pain, and he developed a series of exercises and a brace for victims of low back pain.
Albert O. Loiselle, MD (1915—)
Dr. Loiselle was born in 1915 and arrived in Dallas after military service in World War II. He had known Dr. Percy Girard in San Antonio and went into private practice with him, initially using Baylor as his main hospital. He later did most of his work at Methodist and St. Paul's hospitals. Dr. Loiselle is now enjoying retirement.
THE CHIEFS OF ORTHOPAEDICS AT BUMC
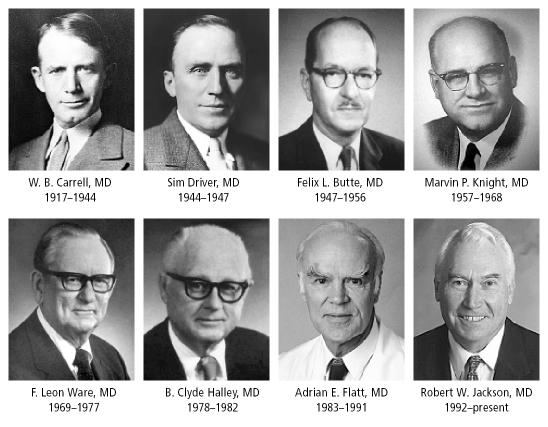
The chiefs of the Department of Orthopaedic Surgery are featured in Figure 13.
Figure 13.
Chiefs of orthopaedics at Baylor University Medical Center.
W. B. Carrell, MD (1883–1944)
Dr. Carrell was a dominant figure as the first chief of the department. He was appointed in 1917 and held this position for 27 years until his death in 1944.
Sim Driver, MD (1890–1949)
Dr. Driver was the first resident to be trained by Dr. Carrell and assumed the position as chief of orthopaedics, on a temporary basis, from 1944 to 1947. Dr. Driver was a strong proponent of the trifin nail developed by Dr. Smith Peterson for the treatment of subcapital fractures and added a sideplate to treat intertrochanteric fractures. Prior to the advent of hip pinning, patients with fractured hips were treated with traction or were placed in a hip spica, and many died of hypostatic pneumonia.
Felix L. Butte, MD (1901–1962)
Dr. Butte was born in Sherman, Texas, and studied medicine at The University of Texas Medical Branch. He graduated in 1926 and became a professor of anatomy at Galveston from 1927 until 1933. His increasing interest in orthopaedics led him to New York to train in that specialty. He returned to practice in Texas, but his career was interrupted by military service from 1942 to 1945. His peers considered him a superb technician, and his main clinical interest was the spine. He is thought to have been the first to use pedicle screw fixation in the stabilization of spines. He became well known for both the operative and conservative treatment of scoliosis. He was chief of the department at Baylor University Hospital from 1947 to 1956.
Marvin P. Knight, MD (1908–2000)
Dr. Knight was born in Texas and trained in orthopaedics in Iowa under Dr. Arthur Steindler. In 1941 he entered the military. He looked after the Dallas Cowboys from 1960 to 1987, a period of 27 years. His major clinical contribution concerned the care of chronic osteomyelitis, and he pioneered the debridement of bony lesions with skin grafting of the defects. His term as chief of the department was from 1957 to 1968.
Dr. Knight was one of the first sports medicine doctors in the USA. He retired to his ranch in 1987 and died on January 24, 2000.
F. Leon Ware, MD (1914—1991)
Born in Arkansas, Dr. Ware obtained his medical degree from Louisiana State University in New Orleans. He then trained in orthopaedics in Dallas, and from 1949 until his retirement he was an associate of Dr. Marvin Knight. It has been said that Dr. Ware contributed more time to the success of BUMC's Department of Orthopaedics than any other single individual. He was a marvelous teacher of surgical anatomy and held regular teaching rounds. At that time 3 to 4 residents from the Parkland program were training at Baylor. He was chief from 1969 to 1977.
B. Clyde Halley, MD (1916—)
Dr. Halley was born in Waco, Texas, in 1916 and graduated from Southwestern Medical College in 1944. He served briefly in the US Navy and at the end of the war established his practice in Dallas. He was associated with Dr. Ted Bywaters, Sr., and Dr. Paul Williams. He practiced primarily at the Gaston Hospital and was very active in the polio epidemics of 1943 and 1953. He was also the first to use penicillin for the treatment of osteomyelitis. In his retirement, Dr. Halley continues to attend orthopaedic functions and to play golf. Dr. Halley was chief at BUMC from 1978 to 1982.
Adrian E. Flatt, MD (1921—)
Dr. Flatt was born in England in 1921 but spent most of his early childhood in India, where his father was in charge of the Indian railway system. From 1934 to 1939, he attended an English public school. Following that, he went to Cambridge University and studied medicine, graduating in 1945. His postdoctoral training was in general surgery, plastic surgery, and orthopaedics. In 1950, he joined the Royal Air Force and spent much of his service time in Ceylon, now Sri Lanka. In 1954, he obtained a Fulbright scholarship and visited the USA. He was obliged to return to England but immigrated the following year, 1956, to the USA, where he was recruited by the University of Iowa to run the nation's first academic hand service. He was on the staff of Iowa for the following 22 years and was elected president of the American Society for Surgery of the Hand in 1976. It was also at Iowa that he developed techniques for modeling hands in order to preserve and display congenital abnormalities. His hand collection later expanded to include the hands of many of the most famous and influential people in the world; it is prominently displayed in the Truett Hospital lobby at BUMC.
Dr. Flatt became the first “full-time” chief of orthopaedics at Baylor in 1982 but maintained a private practice and led the department until 1992. He continues to teach anatomy, to publish, and to see problem cases as the chief emeritus at BUMC.
Robert W. Jackson, MD (1932—)
Dr. Robert Jackson was born in 1932 in Toronto, Canada. His early education took place in Toronto, and he graduated from the University of Toronto in medicine in 1956. He then embarked on 9 years of postgraduate training in Boston, London, Tokyo, and Toronto, with 3 of those years being directed towards orthopaedic research. He was active in sports medicine and traveled to Tokyo in 1964 on a McLaughlin scholarship, where he also provided medical care for the Canadian Olympic Team. In Tokyo, he learned the technique of arthroscopy from Professor Watanabe and brought that technique back to North America and the Western world. The combination of sports medicine and arthroscopic surgery was natural, as many athletes had knee injuries which could now be accurately diagnosed and treated by endoscopic means. His contribution to sports was recognized by the magazine Sports Illustrated, when in its 40th year of publication it chose 40 individuals who had elevated sports to its highest level during the years of publication. Dr. Jackson's contribution to arthroscopic surgery was the only medical event to be recognized. He was also heavily involved in sports for the physically disabled at the Olympic and world level from 1967 until 1984, when he stepped down as president of the International Paralympic Committee.
After 27 years in academic orthopaedics in Toronto, he was recruited by BUMC in 1992 to be chief of a rapidly growing department, bringing with him his interest in research and education.
STRENGTHS OF BAYLOR ORTHOPAEDICS
Sports medicine has long been a major strength of the department. Dallas is a very sports-minded city, and Baylor surgeons have looked after 3 of the 4 major professional teams in the Dallas–Fort Worth area. These include the Dallas Cowboys football team (Drs. Marvin Knight, John Gunn, J. Pat Evans, Robert Vandermeer, and now Daniel Cooper), the Dallas Mavericks basketball team (Drs. J. Pat Evans, Robert Jackson, Tandy Freeman, and Don Buford), and the Dallas Stars hockey team (Dr. Dan Cooper). The Dallas Burn and Dallas Sidekicks soccer teams have been treated by Dr. Howard Moore and the professional rodeo competitors by Drs. J. Pat Evans, Tandy Freeman, and Robert Chapman. Athletes at Southern Methodist University, one of the major universities in Dallas, have for years been treated by Dr. John Baker. The sports medicine group at the Landry Center has always seen high school athletes from North Texas at Saturday morning clinics.
Another strength of the service has been the development of total joints, such as artificial hips and knees. In this respect, Drs. Paul Peters, Richard Schubert, Kurt Rathjen, John Gunn, Robert Jackson, Bill Jackson, Mack Lancaster, and others have performed a great service, operating on >1100 hips and knees a year.
A spine center has been established recently, headed up by Dr. Craig Callewart and staffed by Drs. Robert Viere, Huntly Chapman, William Bruck, and Drew Dossett. Dr. Steve Curtis is well known for his lifelong interest in spinal surgery.
Another area of strength is the hand service, originally developed by Dr. Adrian Flatt and later directed by Dr. Peter Carter, but now managed with great skill by Drs. Arnold DiBella, Paul Ellis, Hugh Frederick, and Thomas Diliberti. Limb and digit replantation is superbly performed by Dr. David Zehr.
In foot and ankle problems, Drs. Jerald Blum, James Brodsky, and Eugene Curry do outstanding work. Dr. Brodsky is well known for his research and teaching efforts in foot and ankle surgery and for his administrative talents on the national executive level of the American Orthopaedic Foot and Ankle Society.
Shoulder and upper limb problems are well treated by Drs. Wayne (Buz) Burkhead, Phillip Hansen, and Don Buford.
BUMC has recently achieved level I trauma status because of the hard work of Dr. Paul Freudigman, assisted by all the staff younger than 55 years, who take call.
Oncology is represented by Dr. Wynne Snoots, who also works with victims of cerebral palsy. He and Dr. James Sackett treat most of the pediatric patients at Baylor.
Every subspecialty is aided by the teaching and diagnostic assistance provided by Dr. Guerdon Greenway of the Department of Radiology, who has specialized in orthopaedic aspects of radiology. He has recently been joined by Dr. Marc Fulmer.
Such subspecialization has produced a department that is becoming increasingly busy. The most recent statistics show that the orthopaedic service performs more operations and treats more patients than any other surgical service in the hospital.
A widely read magazine, U.S. News & World Report, has recognized the department as one of the top 40 orthopaedic departments in the USA.
EDUCATION AND RESEARCH
The original orthopaedic training program in Dallas was established in 1946 on the return of Dr. P. M. Girard from World War II army duty. Dr. Girard established a 3-year training program with junior resident rotations of 6 months each at Parkland, Baylor, and Scottish Rite hospitals, followed by senior resident rotations of 6 months each at the 3 teaching hospitals. The faculty comprised all of the attending staff at the 3 hospitals. Each staff member in turn would take a 3-month rotation, cover the residents in the emergency room and the outpatient clinic, and hold weekly rounds at Parkland. In those early days, therefore, the staff at BUMC contributed significantly to the success of the orthopaedic training program. The chiefs of each of the training centers rotated yearly as chief of the teaching service.
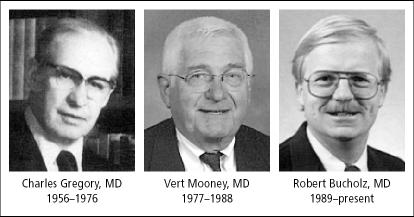
In 1956, Dr. Charles Gregory (1919–1976) was appointed full-time chairman and professor of orthopaedics at The University of Texas Southwestern Medical School (Figure 14). He devoted his life to the education and training of residents, spending hours with them, making rounds late in the afternoon, staying and eating supper and teaching them long into the night. He had the ability to make the residents think in an orderly fashion to solve problems. Later a second full-time staff person, Dr. Louis Paradies, was appointed. During the 1960s and early 1970s, much of the resident training was at Baylor; the rotations were highly successful, as the residents were exposed to the more practical aspects of the private practice of medicine. They would also see the early and often subtle problems involving the foot and ankle, hand, shoulder, and sports injuries that were often overlooked in the hectic services of public hospitals such as Parkland.
Figure 14.
Professors of orthopaedics at The University of Texas Southwestern Medical School.
In 1967, the first postgraduate program sponsored by the Academy of Orthopaedic Surgeons outside of the regular academy meeting was held in Dallas under the direction of Dr. Gregory.
When Dr. Gregory died in 1976, Dr. Vert Mooney was appointed and began to recruit more full-time staff for the training of residents. However, the number of residents rotating through BUMC declined. In 1989, Dr. Robert Bucholz was appointed professor and chairman; he since has developed a firstclass training program for orthopaedics with a strong emphasis on trauma and joint replacements. Basic research activities have also been encouraged at Parkland.
Recognizing the trend toward full training of residents at Parkland and the decreasing need for them to rotate through BUMC, the Department of Orthopaedics is now concentrating on fellowship training, with fellowships being offered in foot and ankle care, shoulder care, sports medicine, arthroscopy, trauma, and basic research.
In the past, research activities at BUMC were largely focused on clinical follow-up studies. Since 1991, with the support of the Robert and Ruby Priddy Foundation, a motion and performance laboratory dedicated to the kinematic analysis of human performance has been developed. Most of the work to date has been directed toward the lower extremity, with knee, hip, and ankle problems being studied at great length. The motion and performance laboratory is now headed by Fabian Pollo, PhD, a bioengineer and an expert in gait analysis.
Basic research is being performed, notably the development of an instrumented spatial linkage device to measure the motion of joints in 6 degrees of freedom. This has been worked out in some detail for the knee joint but can be applied to any moving joint such as shoulder, spine, or wrist. Photodynamic tissue bonding is also being explored as an offshoot of laser technology.
A highlight of the orthopaedic educational activities is the visiting professor program, which brings an internationally recognized speaker to Baylor each spring for an academic session open to all surgeons in North Texas.
An arthroscopy learning center or bioskills teaching laboratory has been active since 1992, where arthroscopic surgical techniques for the knee and shoulder can be taught on cadaver parts.
A closed-circuit television system has been established from the operating rooms to the Ruth Jackson Conference Center so that surgical procedures on patients can be televised directly to the conference center. This is a very powerful teaching tool, which has been well utilized by the foot and ankle service.
FUTURE OF ORTHOPAEDICS AT BAYLOR
While other diseases will eventually be cured or prevented, aging and trauma are problems that will continue forever. Overall, hospital stays will be minimized and more and more surgical cases will be done as outpatient procedures. Minimally invasive surgery will become the norm. With the steadily increasing age of the population, it must be recognized that if the elderly are to remain independent at home or in modified surroundings, with a reasonably good quality of life and without increasing the burden on the health care system, the management of orthopaedic conditions will be a most important factor. Improvement of mobility through the treatment of arthritis, proprioception training to improve balance, and ancillary surgery such as cataract removal to aid vision and vascular reconstruction to preserve limbs will all have a significant impact on the costs and efficacy of our health care system in the future.
Trauma and degenerative diseases together currently provide the greatest volume of work for orthopaedic surgeons at BUMC. It is obvious that the workload involving arthritis, osteoporosis, and fractures from falls will increase in future decades. Also, as people live longer and participate more in recreational activities, sports medicine for the older age group will become an increasingly large part of orthopaedics.
Prevention of injuries is one area that has never been adequately addressed. Orthopaedists must work toward the prevention of problems or, at the very least, the accurate prediction of their occurrence. Chronic disuse types of problems are currently being treated but not prevented (e.g., carpal tunnel syndrome). Primary healing of tissues is also a goal (e.g., tissue welding). However, for this work orthopaedic surgeons will require and welcome help from their allies, including basic researchers, biomechanics researchers, and epidemiologists.
At BUMC, a single building with inpatient and outpatient facilities, specialized radiology, specialized operating rooms, and related services would definitely help achieve this goal. A true Institute of Orthopaedics is something that will be pursued.
SUMMARY
The impact of orthopaedics in this past century has been significant. Many musculoskeletal problems have almost disappeared, such as uncontrollable infections, metabolic diseases, and polio. While arthritis is an increasing problem, it is not an insurmountable challenge. There are now many ways of treating and even preventing arthritic joints.
Orthopaedic surgeons are no longer pure surgical technicians but have evolved into caregivers for disorders of the musculoskeletal system, with surgery as only one of the options of treatment.
Acknowledgments
Historical research relies on information obtained from many sources, and the author gratefully acknowledges the specific contributions of Drs. Ray Lawson, George Boswell, John Gunn, Clyde Halley, and Adrian Flatt. Information regarding BUMC, the Carrell Clinic, and the Scottish Rite Hospital was obtained from the archives of those institutions. Additional information was obtained from the writings of Steven Schmich, the Dallas Times Herald, the Ruth Jackson Society, and Linda Dunagan, who has been the “keeper of the files” for many years. Thanks also to Mary Ann Krajca for collating and typing vast amounts of information.