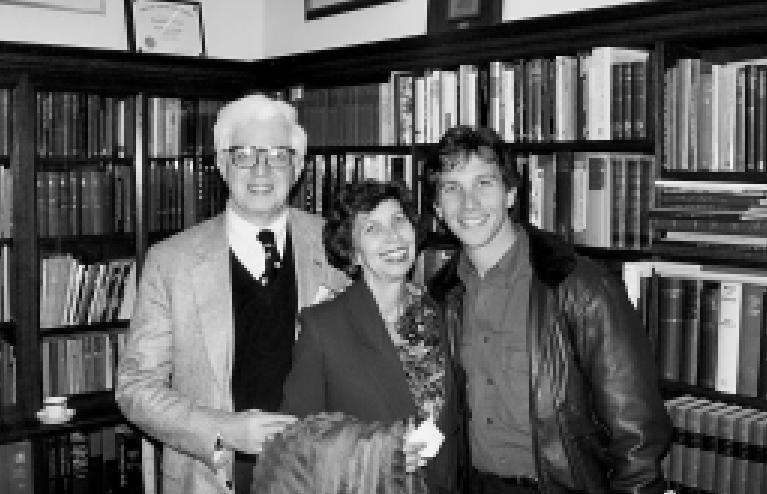
Marvin Stone (Figure 1) was born in Columbus, Ohio, on August 3, 1937. He grew up in Bexley, Ohio, where he attended public schools. After premedical studies at Ohio State University (1955 to 1958), he went to the University of Chicago School of Medicine (1958 to 1963). Following his sophomore year in medical school, he took off a year to do research in the pathology department. In 1962, he received a master of science degree in pathology and the next year the MD with honors. His internship and first-year residency were at Barnes Hospital in St. Louis on the ward medical service. From 1965 to 1968, he was a clinical associate in the Arthritis and Rheumatism Branch of the National Institute of Arthritis and Metabolic Diseases of the National Institutes of Health (NIH) in Bethesda, Maryland. He then came to Dallas, Texas, to be a senior resident in medicine at Parkland Memorial Hospital, and the following year he was a fellow in hematology/oncology there.
Figure 1.

Marvin Stone during the interview.
He remained on the faculty of The University of Texas Southwestern Medical School until 1976, having risen to the rank of associate professor with tenure, when he moved to Baylor University Medical Center to become the first chief of oncology and director of the new Charles A. Sammons Cancer Center. He was also named director of immunology. He continued as a clinical professor in the Department of Internal Medicine at Southwestern Medical School after moving to Baylor.
For the past 25 years, Marvin has directed the Sammons Cancer Center, and it has thrived. He has been an active teacher of the housestaff and oncology/hematology fellows in addition to directing the junior medical students from Southwestern rotating through Baylor. Despite an active private practice and a heavy teaching load, he has continued his research endeavors, which have led to the publication of nearly 150 articles, most in peer-reviewed medical journals. For his many achievements, Dr. Stone has received a number of honors including Phi Beta Kappa; Alpha Omega Alpha; Sigma Xi; Outstanding Full-time Faculty Member, Department of Internal Medicine, Baylor University Medical Center (1977 to 1978 and 1986 to 1987); governor, Texas Northern region (1993 to 1997), laureate, Texas Chapter(2000), and mastership (2001), all in the American College of Physicians; fellowship, Royal Society of Medicine (London)(1998); dedication of the Marvin J. Stone Library, Baylor Institute for Immunology Research, Zelig H. Lieberman Research Building (1999); honoree of the William Solly and Carol Dismukes Carter Endowment Fund for Oncology Education and Research of the Baylor Health Care System Foundation (2000); and the Dr. Judah Folkman Scientist in Residence, Bexley High School, Columbus, Ohio(2001). He will be a recipient of the University of Chicago’s Distinguished Service Award for the year 2002 and is upcoming president of the American Osler Society. Dr. Stone is a beloved physician, a role model and mentor to many physicians, and one who personifies, more than anyone I’ve met, the life of his beloved Sir William Osler. His devoted wife, Jill, and their lovely daughter and son round out this exemplary life.
William Clifford Roberts (hereafter, WCR): I am in my house with Dr. Marvin Stone on May 23, 2001. Marvin, I sincerely appreciate your coming over and permitting me and therefore the readers of BUMC Proceedings to get to know you better. To start, could you address your early upbringing in Columbus, Ohio—your father, mother, and siblings? What was it like growing up in Columbus in the late 1930s and early 1940s?
Marvin Jules Stone (hereafter, MJS): My father was an attorney. Mother took care of my older sister and me (Figure 2). I grew up in Bexley, a suburb on the east side of Columbus (Figure 3). We moved there when I was 2 years old and lived in the same house through high school and my freshman year at Ohio State. Bexley was a wonderful place to grow up. The school system was outstanding. I lived about a block away from the school. I could sleep late in the morning and get up 25 minutes before I had to be there. We had excellent teachers. I grew up with the same group of kids the entire time.
Figure 2.
Parents, Roy J. and Lillian B. Stone.
Figure 3.

At age 1½ years, headed for Texas before he knew it.
WCR: How did your father get to Columbus? Was his family raised there?
MJS: He grew up in Massillon, in northeastern Ohio near Canton and Akron. Massillon was known for its football team. Paul Brown was the high school coach there in his early years and produced perennial state championship teams. My father attended college and law school at Ohio State, where he met my mother, who was from Charleston, West Virginia. She had a year of law school before they were married in 1931 and settled in Columbus.
WCR: When was your father born?
MJS: In 1903.
WCR: Is he still alive?
MJS: No. He died in 1956 when I was a freshman in college.
WCR: Is your mother still alive?
MJS: Yes. She will have her 90th birthday at the end of July and remains a bright and vivacious woman.
WCR: When was she born?
MJS: In 1911.
WCR: There was an 8-year difference between your mother and your father. Was he in law school when they met?
MJS: He was just out of law school and was her coach on a debate team. I believe that’s how they met.
WCR: What was your father like?
MJS: He was a practicing attorney. He did a lot of tax and corporate law. I think he also did some divorce work. He was a scholarly person who loved books. We had a lot of books in our home when I was growing up. My mother used to complain that there was no space to put them. He taught the high school class in our temple for many years. Unfortunately, he died, presumably of a myocardial infarction, at age 52. Both my grandfathers died at about that age.
WCR: Did your father have a major impact on you?
MJS: Yes. He was 34 when I was born. I always looked up to him. He was a role model for me in terms of how he conducted himself and because of his interests in scholarly activities and teaching.
WCR: What kind of books did he acquire? Did he have a particular interest in one area or another?
MJS: I’m not sure I know the answer to that. Aside from books about law, he also read about philosophy, literature, and psychiatry. After he developed cardiac problems, he bought a number of books on heart disease. I first heard of Sir Thomas Lewis because my dad bought one of his books. My father had eclectic interests.
WCR: Would he read every night?
MJS: Perhaps not every night, but many of them.
WCR: What was your mother like?
MJS: My mother was devoted to her family and still is. She raised my older sister and me. She also was active in a number of volunteer and community activities. Her debating experience came in handy from time to time. People used to comment about her knowledge of various subjects and ability to express herself clearly.
WCR: In what way?
MJS: She would often get into in-depth discussions with people over various issues in the community. I remember several of them commenting about her talent in arguing her point. My dad was one of the few people who could win an argument with her—sometimes!
WCR: What was dinner like at home at night? Would you and your parents and sister have discussions around the table?
MJS: Dinner was a special time. We would hear about Mom and Dad’s activities that day and tell them about ours. Current events were also a frequent topic of conversation. World War II began when I was 4 years old. I remember many conversations about what was happening in the war and about trying to help in whatever way we could. I recall collecting newspapers and donating toys for the war effort. We also heard a lot about buying “war bonds.”
WCR: It sounds like it was a very pleasant home.
MJS: It was.
WCR: And there was enough money for you and your sister to do more or less what you wanted to do?
MJS: We were comfortable. My father had an adequate income, but we were never wealthy. My parents had been through the depression from the time they were married. They were very conscious of the importance of being frugal.
WCR: What is your sister like?
MJS: Her name is Jocelyn, but we always called her “Jo.” From as early as I can remember, she liked to read. She attended Miami University in Oxford, Ohio. She got married before she finished, had 3 children, and subsequently was divorced. Later, Jo finished her college degree. She remarried about 10 years ago, but unfortunately, her second husband died about 2 years later. She still lives in Columbus and recently retired from her job with the state government.
WCR: You and she got along very well, I presume.
MJS: I think we got along well. We had our share of sibling rivalries. Overall, I think we did fine.
WCR: Was there a teacher or a person at the temple who had a major influence on you as you were growing up?
MJS: Many of my teachers had an influence on me. I still remember some of my grade school teachers. In junior high, I recall Miss Ogan, one of my English teachers. In high school, I especially remember my math teacher, John Schacht. I took math from him for 3 years. He was one of the best teachers I’ve ever had, and I’ve had a number of excellent ones.
WCR: What were your other activities in junior high school and high school? Were you an athlete? Were you on the debating team?
MJS: We didn’t have a debating team. I loved sports but wasn’t very good. I played football, baseball, basketball, and golf, but not well. I sang in the chorus and was in a number of school plays. In junior high school, I got the role of the stage manager in Our Town, which was my favorite acting experience. I was also in some plays in high school. In our senior play, I had the role of Nels in I Remember Mama.
WCR: Was Bexley a large high school?
MJS: No. There were 150 in my graduating class. I was recently back there, and it’s only a little larger now than in the 1950s.
WCR: Did you and your family go on vacations during the summer? What family activities did you do together?
MJS: Usually we would visit relatives. We would go to Massillon and Canton because my father’s family lived there. And then my mother’s mother and brothers were in Charleston, West Virginia. Most of our travels were to one of those cities. Occasionally, we went elsewhere. In those very early years, it was wartime and hard to take long trips. Later, my father became ill, and it was difficult for us to travel as a family.
WCR: How long was he ill? He had a coronary event sometime before he died?
MJS: He had a heart attack when he was in his mid 40s. He recovered and went back to work but died suddenly at age 52.
WCR: Did you have jobs when you were in high school to earn a little money? What did you do in the summers?
MJS: I had a morning paper route for a while but hated getting up at 4:00 am. One summer, I worked with a schoolmate in his father’s cigar and candy wholesale distributing company. I also worked several summers with my brother-in-law who did heavy manual labor buying and selling used auto parts. We traveled across the Midwest in his truck. That was hard physical work. I think that experience is one reason I appreciate cognitive pursuits!
WCR: How did you select Ohio State for college?
MJS: Practical reasons. Several of my good friends were going East to college. When we were seniors, we visited a number of eastern colleges. They wound up at Williams. I knew I wanted to go to medical school, and it was financially most feasible to stay in Columbus and attend Ohio State.
WCR: There were no physicians in your family?
MJS: Only distant relatives. My father’s cousin was an allergist named Benjamin Feingold. He was the head of allergy at the Kaiser Hospital in San Francisco—the original Kaiser Hospital. He had a large practice there and wrote about allergy. A nephew of his was Morton Grossman, who was a well-known research gastroenterologist in Chicago and later at UCLA.
WCR: Did you see them much?
MJS: I remember seeing Morton Grossman only once as a youngster when I was in Canton and he came there. Shortly after I came to Baylor in the mid 1970s, he came to visit John Fordtran but, unfortunately, I was away. Regrettably, I never did see him again, as he died shortly afterwards. I got to know Cousin Ben because I saw him in San Francisco when I was applying for an internship and several times thereafter. I was in San Francisco last week for a meeting and visited with his widow, who is now 97 years old and still sharp as a tack.
WCR: Benjamin Feingold and Morton Grossman must have been mentioned at your home periodically?
MJS: Rarely. I was aware that they were brilliant physicians, but not much else.
WCR: They really didn’t have a major impact on you. When did you know that you wanted to be a physician?
MJS: When I was in junior high school.
WCR: How did you decide that that was the area you wanted to pursue?
MJS: I visited my mother after she had surgery at University Hospital in Columbus. I remember going there and being struck by the atmosphere of the hospital and the healing mission of the doctors. Watching the physicians interacting with patients, I knew I wanted a medical career. I couldn’t imagine a better way to spend my life. Still can’t.
WCR: You mentioned the influence of a math teacher on you. Was science something you took to in junior high or high school?
MJS: Yes and no. I did fairly well in math. As I mentioned, I had a superb teacher, Mr. Schacht, for 3 years in high school. He exerted a major influence on many Bexley students, not only because of the math per se, but also because he emphasized the importance of being a good citizen. He used to say that he wasn’t as interested in how much math we knew as he was in how we drove a car and that we always exercised our right to vote. I also remember him saying he didn’t know how to accurately grade us and if he could come within one letter of what we really deserved, that was the best he could do. I often think of that viewpoint when I’m in grading sessions for the junior medical students. I liked biology and chemistry a lot but didn’t care much for physics and didn’t do well in physics.
WCR: Did you read a lot in junior high and high school?
MJS: Not enough. When I met Jill, I found she was much more widely read than I was. We had to read for school, but I didn’t do much extra reading back then.
WCR: How did you do in high school? Were you a good student?
MJS: I was erratic. I was about 20th in the class of 150. We had a bright group of students at Bexley. I didn’t apply myself consistently. I kind of messed around.
WCR: Achieving came relatively easy for you?
MJS: I don’t know that I would say it was easy. I just remember that I wouldn’t really work hard except in short spurts. I was more interested in sports.
WCR: How did Ohio State University hit you? Did you live at home when you went to college?
MJS: I lived at home the first year; the next 2 years I lived on campus. Ohio State was a very large university even then. It had nearly 40,000 students. The premed curriculum was highly structured so that during the first 3 years, I had only 2 electives. It was heavily weighted towards science. I was in the “arts-medicine” curriculum, which potentially would allow me to enter medical school after 3 years and receive my undergraduate degree after the first year there. I took chemistry every quarter, the other sciences, and the required liberal arts courses.
WCR: Who had a major influence on you in college at Ohio State?
MJS: Jill.
WCR: You met Jill when you were a sophomore?
MJS: Yes. I met her the first week she was at Ohio State when I was beginning my sophomore year.
WCR: How did that come about?
MJS: As an out-of-state student from Little Rock, Arkansas, she was not allowed to live in the dorms. She was in a rooming house for nonresident girls which was located close to our fraternity house. Several of us went visiting there during orientation week to look over the new crop of freshman girls.
WCR: This young lady from Little Rock, Arkansas, really got to you right off. Is that how it worked?
MJS: Yes, I think so!
WCR: When did you get married?
MJS: About 2 years later, in June 1958. I began medical school at the University of Chicago the following September. We had a marvelous summer as newlyweds. By the way, I had been advised during my Chicago interviews not to get married—that the best students there were never married.
WCR: How old were you when you got married?
MJS: Twenty.
WCR: And Jill was how old?
MJS: Nineteen.
WCR: Did you tell your kids to get married young or to wait awhile?
MJS: I’m not sure we told our kids either one. Back in the 1950s, many people married at a young age. Jill still enjoys telling the story that I had to have my mother’s written permission to get married because in Arkansas men had to be 21, whereas women only had to be 18. To further complicate the situation, my grandmother became ill just before our wedding. When it was time to get the license, I was in Charleston, West Virginia, with my grandmother, so Jill had to take the letter from my mother saying that she gave permission for her son to get married—without me. She went with a girlfriend to get our marriage license!
WCR: It sounds like in college you were relatively active socially as well as academically.
MJS: Remember, it was Ohio State! I was social chairman of our fraternity, so I used to arrange the functions (dances and so forth). Of course, Jill and I dated but I also worked in college, unlike in high school. I applied myself much more consistently in college than ever before.
WCR: What came over you to make you do that?
MJS: Realizing I needed good grades to get into medical school.
WCR: You wanted to be sure you got into medical school. You were a Phi Beta Kappa the third year in college?
MJS: No, I missed it by a hair the third year. Because I left Ohio State after 3 years to attend the University of Chicago Medical School, I lost my bachelor’s degree and eligibility for senior year Phi Beta Kappa. I recall thinking it was a bit ironic that Ohio State wouldn’t accept the University of Chicago as an equal academic institution. When I graduated from Chicago, I was inducted into its Phi Beta Kappa chapter, an unexpected honor.
WCR: How was it that you went to the University of Chicago? You had planned from the time you entered college to go to medical school there in Columbus. What changed your mind?
MJS: Seeing the University of Chicago and meeting the people there, I was struck immediately by the exciting intellectual atmosphere—it was almost palpable. I knew at once that I wanted to go there; it was similar to the decision about becoming a physician. Those were 2 of several events in my life in which the direction was crystal clear.
WCR: How many medical schools did you apply to?
MJS: I applied to 5: Cincinnati, Harvard, Jefferson, Chicago, and Ohio State.
WCR: How many were in your medical school class?
MJS: Seventy-two.
WCR: All of them graduated? Was that at the beginning or the end?
MJS: Nearly all graduated. The first day of medical school, the dean told our class that the selection process had been stringent, that he was glad all of us were there, and that they’d do their best to make sure we graduated.
WCR: You entered medical school what year?
MJS: 1958.
WCR: This was the first time you lived outside of Columbus. Chicago is a big city, much bigger than Columbus. How did this intellectual, big-city atmosphere hit you?
MJS: I was a little overwhelmed. It was not only the big city; it was the south side of Chicago in the late 1950s. We lived in a third-floor walk-up apartment over a grocery store at 57th and Harper. Hyde Park previously had been one of the elite neighborhoods in Chicago, but it had deteriorated greatly. It was almost like a war zone. Many people in our class were robbed or burglarized at one time or another during medical school. It was dangerous. It also was a politically and socially labile neighborhood. Malcolm X lived 10 blocks away. The unrest that occurred in many American cities in the 1960s and 1970s was already happening on Chicago’s south side in the 1950s. Nevertheless, the medical school was fabulous. Being from a “Big 10” school with only 3 years of college, it took me awhile to become acclimated to the pace of medical school. I had some ups and downs the first year, especially in biochemistry and anatomy. Then things improved.
WCR: Jill had gone from Little Rock, Arkansas, to Columbus, Ohio, and then to Chicago, Illinois. That must have been an even greater shock for her.
MJS: Not really. She was much more knowledgeable about social inequities than I was. She had been a volunteer social worker and came to Ohio State planning to become a social worker. Shortly after we had moved into our apartment (called our “magnificent palace”) that first summer, Jill met an elderly lady. Her name was Bertha Parker, and she worked across the street from our building. She was the editor of the Golden Books Encyclopedias for children. She hired Jill to type manuscripts for the Golden Books. Later, Jill worked in the associate dean’s office at the University of Chicago. She acclimated very well— much better than I did. It took me awhile.
WCR: When did your first child come?
MJS: Nancy was born in September 1960, just after my sophomore year. I had decided to take a year off to work in pathology with Dr. Robert W. Wissler, chairman of the pathology department, with whom I had started a research project near the end of my freshman year. I became a predoctoral graduate student for that year off. We moved out of Hyde Park because of the baby, but it was a rather long commute.
WCR: How did you spend that year in pathology?
MJS:I took a number of graduate-level courses and helped as a lab assistant in the pathology course for medical students. Most of the time, I worked on my research project, which had to do with injecting antitumor antibodies and an oncolytic virus into tumor-bearing mice. The tumor immunology work with Dr. Wissler resulted in my first publication and led to the master’s degree. We moved back to Hyde Park for my junior year of medical school.
WCR: How did it come about that you did research in your freshman year? You’d never done research before?
MJS: During the third quarter of the freshman year at Chicago, everyone had an elective that could be spent in research. I asked to work with Dr. Wissler in pathology, got started on a project, and enjoyed it. I decided to take the extra year because of my interest in the tumor immunology study and, in part, because I had had only 3 years of college.
WCR: How did investigation hit you? Did you enjoy it from the beginning?
MJS: Oh yes. It was fun. Pathology at the University of Chicago had been an experimental department with immunology emphasis under Dr. Paul R. Cannon and before him, under Dr. H. Gideon Wells. Dr. Wissler was an MD/PhD who was interested in cancer immunology and the pathogenesis of atherosclerosis. I chose to work on the cancer immunology side.
WCR: That entire year you went to certain classes but for the most part you worked on your research project. Did Robert Wissler have a significant impact on you?
MJS: He sure did. A wonderful mentor who was very supportive of students, he was the type of person who let you grow and develop at your own speed. He was easygoing and very encouraging. He reflected the general atmosphere of the medical school; the faculty at Chicago made you think. I would plan an experiment and then discuss it with Dr. Wissler. He would point out deficiencies in a very kind way or make suggestions about ways of improving the design. He was just a joy to work with and is still at Chicago.
WCR: Who else in medical school had a major influence on you?
MJS: Dean Joseph Ceithaml, PhD.
WCR: How did he influence you?
MJS: He was the first person I met when I was interviewed. A PhD in biochemistry, he was a member of the medical school faculty. He was a fairly young dean—dean of students he was called. He set the pattern for the other interviews and created that excitement in me. After I became a student there, Dean Ceithaml encouraged me a great deal. Toward the end of my freshman year, he awarded me a scholarship, which I was able to keep for the remainder of medical school.
WCR: Were there other teachers or professors who influenced you considerably at medical school?
MJS: Yes, there were a number of them, but none who had the impact of Dr. Wissler and Dean Ceithaml.
WCR: How did it hit you when you entered the wards your junior year?
MJS: I’d come back from the year off. I started on surgery, and my first rotation was neurosurgery. It was a fabulous experience! We had 2 neurosurgeons at the University of Chicago, Drs. John Mullan and Joseph Evans, both marvelous role models. I had a wonderful time on neurosurgery and also enjoyed the rest of the surgery rotation, especially with Dr. George Block, a terrific teacher and a legend at Chicago. I never expected to like surgery, but I did. As I rotated through the remainder of the junior year, I sucked things up like a sponge. I loved it.
WCR: How did the neurosurgeons influence you? You say they were both role models. In what way?
MJS: Both Dr. Mullan and Dr. Evans were excellent clinicians and very caring physicians, kind and encouraging to students and wonderful with patients. Their operating procedure notes were almost like literature. I remember reading their notes after seeing the surgery performed. They would frankly say that they made a decision to do something or other and hoped it would be beneficial for the patient, but they weren’t sure. Such statements would be dictated right into the body of the note. Both men had great integrity and were superb teachers.
WCR: How did you decide to intern in internal medicine? You’d had a good experience with surgery.
MJS: I always thought I would go into internal medicine. I really liked pathology, but I enjoyed clinical work and patient care too much to give them up. I felt internal medicine was a challenging field, one in which clinicopathologic correlation was particularly important. However, I was undecided between general internal medicine and a subspecialty.
WCR: Did you and Jill have enough time to be able to enjoy some of the cultural activities that Chicago afforded?
MJS: We didn’t have much time or money. We’ve always enjoyed theater, and 2 or 3 times a year, we would see whatever touring show was on. The Museum of Science and Industry was within walking distance of our first apartment, and we spent much of the summer of 1958 there.
WCR: Did your classmates have much influence on you?
MJS: Yes. Three other couples were married at the beginning of medical school. We used to get together occasionally with them. In gross anatomy, 4 of us worked on a cadaver, and we became close friends as people tend to do when they share unforgettable experiences. When I changed classes, of course, I inherited a new group of classmates. One was Mark Silverman. We had been friends at Ohio State, and he also knew Jill. Mark came to Chicago, and we ended up in the same medical school class.
WCR: Mark is from Ohio?
MJS: Yes. He’s from Springfield.
WCR: You had made up your mind to be an internist. How did you end up at Barnes Hospital in St. Louis for your internship?
MJS: I was lucky. I interviewed at some of the Boston places, but neither they nor I found each other irresistible. Still, it was a memorable experience, especially the interview/examination at Massachusetts General. One of my classmates ended up at the Brigham. I also interviewed at Barnes, Stanford, and Parkland. Because of my cousin, I interviewed at the Kaiser Hospital in San Francisco. However, I was most impressed by the Barnes atmosphere, much as I had been by the University of Chicago. Dr. Carl V. Moore was chief of medicine. The Barnes ward service was a superb teaching service and highly sought after. I ranked it first and was excited and pleased when I matched there.
WCR: And you were delighted to be at Barnes?
MJS: I think it was the best thing that could have happened. Barnes was great, and I enjoyed my 2 years there (Figure 4). When I arrived at NIH after the second year and was thrown in with a number of other clinical and research associates from Boston and New York programs, I felt my housestaff training had been equal to theirs.
Figure 4.
Barnes ward medicine housestaff, 1964–1965. Carl Moore is fourth from the left on the first row; Marvin Stone is sixth from the left on the first row.
WCR: What did you love about Barnes? This is one of the finest medical centers in the world, obviously.
MJS: Mainly, Dr. Carl Moore and Dr. Sol Sherry. Also my peers. Drs. Moore and Sherry were inspiring role models and had a tremendous impact on those of us on the ward service. There were 12 interns in our class, all first-rate people. Dr. Moore was the kind of person who made you want to do as well as you could. We didn’t want to disappoint him. He commanded enormous respect and engendered a wonderful learning atmosphere. We learned a lot from each other and especially from Dr. Moore, a hematologist, who was a front-rank clinician and teacher. I don’t think I ever made rounds with him without learning something.
WCR: What were his characteristics that made you feel that you just couldn’t disappoint this man?
MJS: He was quiet, very kind, very bright, and very thoughtful. He taught by asking questions rather than by answering them. He made me think, much as Dr. Wissler had. Dr. Moore was an ideal role model. He took care of people who were seriously ill and, to them, he was almost like a minister as well as a physician. It was a marvelous experience watching him interact with people.
WCR: I gather he was the one who got you interested in hematology and oncology.
MJS: He added greatly to my interest. At Chicago, there was a large hematology/oncology service. I liked hematology and, of course, I liked pathology. I was interested in cancer immunology. Barnes was another big hematology/oncology center. Dr. Moore had a major role in further developing my interest, but it was already there.
WCR: You started your internship in 1963. When I was in medical school, there was the hematologist, but nobody spoke of oncologists at that time.
MJS: That’s right. It was principally hematology. Most hematologists also treated cancer patients with solid tumors, however.
WCR: When did oncology, that phase, come to be connected to hematology?
MJS: In the late 1960s, as I was nearing the completion of my training, I remember that a number of people discussed the possibility of establishing oncology as a separate medical specialty. Oncology relating to chemotherapy had been included as part of hematology, but you’re right, the focus was mainly hematology. Those of us who trained in hematology did oncology as well, but it was, at least in an academic sense, certainly not the major part of the field. Finally, in about 1970, the American Board of Internal Medicine (ABIM) decided to create additional subspecialties in internal medicine, one of which was medical oncology. After passing the written examination in 1970, I had the choice of either waiting to take the subspecialty examination 2 or 3 years later or taking the orals right away. I was in the group that took the last internal medicine orals because I didn’t want to wait for ABIM certification. Then I took the first hematology subspecialty exam in 1972 and the first medical oncology exam the following year. From that point on, medical oncology developed as a separate subspecialty. Now things have flipped-flopped: medical oncology has become more popular than hematology. With the recent advances in molecular biology and genetics, medical oncology is one of the most exciting fields in medicine.
WCR: I gather you were a pretty good Ping-Pong player as a houseofficer at Barnes.
MJS: About the same as the other sports—I tried.
WCR: But you got a Ping-Pong award during your housestaff training there. What was that all about?
MJS: At Dr. Moore’s Christmas party, I was awarded a Ping- Pong paddle by one of my fellow interns, Jan Szidon, who was from Sao Paulo, Brazil. He became a pulmonary physiologist. We were on call every other night as interns and there was a Ping- Pong table in the housestaff quarters. Whenever we had the chance, we would play. Somehow or another, I must have triumphed and was awarded the paddle. Jill said, “I thought you were working all of those call nights!” I assured her that Ping- Pong opportunities were rare!
WCR: You and Jill enjoyed St. Louis as a city?
MJS: Very much. We lived in Brentwood in Audubon Park which was sort of a large commune. Virtually everyone was either a houseofficer at Barnes or graduate student at Washington University. Many had little children. It was a great place for the kids and the wives. We really enjoyed St. Louis, especially the people.
WCR: How did it come about that you went from St. Louis, Missouri, to Bethesda, Maryland, as a clinical associate in the Institute of Arthritis and Metabolic Diseases?
MJS: Because of the Vietnam war, many physicians were being drafted. Toward the end of my internship year, I learned that some houseofficers on the ward service at Barnes went either to NIH or the Centers for Disease Control as commissioned officers in the US Public Health Service. I thought the NIH would be a great place to obtain more research experience, so I applied for a position. I interviewed with a number of investigators in the cancer and arthritis institutes. I was accepted and matched with Dr. Joseph Bunim in arthritis and with the laboratory of Dr. Henry Metzger in immunochemistry.
WCR: How many clinical associates were there in the arthritis institute? You went there in 1965.
MJS: Yes. I was there from 1965 to 1968. In the whole institute, my guess is that there were about 15 or 20, including Bill Kelley, Pedro Cuatrecasas, and Sid Wolfe. In our Arthritis and Rheumatism Branch, there were 3—John Johnson, Paul Plotz, and me.
WCR: You initially went for 2 years, but you stayed 3. You stayed 3 years because your research work was going so well that you thought it was the right thing to do, I presume.
MJS: That’s correct. I felt that if I stayed the third year, I’d get a lot more out of it because my lab project on Waldenström’s macroglobulin antibody activity was gaining momentum the second year. I had already decided to come to Dallas to finish my residency, so I wrote and asked Jay Sanford if I could postpone it a year. He said that would be fine.
WCR: Your work at NIH was fundamentally in immunochemistry. That was a relatively new arena at that time. Is that true?
MJS: To some extent. However, immunochemistry has been a recognized discipline since the days of Paul Ehrlich and Karl Landsteiner. Breakthroughs in immunoglobulin structure had occurred during the 5 or 6 years before I arrived at NIH. Antibody molecules could be disassembled and their functional parts characterized. The senior investigator in whose lab I worked, Henry Metzger, was involved in defining the structure of macroglobulin (immunoglobulin M or IgM), using plasma from patients with Waldenström’s macroglobulinemia. I was his second clinical associate and started working in that area. We soon began to investigate IgM function as well because we were studying a Waldenström protein that formed a mixed cryoglobulin with IgG and set about to determine whether the cryoglobulin was an antibody-antigen complex.
WCR: You hit on something that you really enjoyed.
MJS: Yes. One reason was that Henry was an excellent mentor and first-rate scientist. During the course of the next 2 years, we were able to demonstrate that the Waldenström protein (IgMLay) was the antibody and IgG the antigen. The IgM-IgG immune complex formed the cryoglobulin. Because this Waldenström macroglobulin was one of the first human monoclonal antibodies described and because of its clinical relevance, I was interested in pursuing it.
WCR: You did work on the wards there, at least your first year.
MJS: During the first year and a half, I spent about one third of my time on the arthritis service.
WCR: What kind of diseases did most patients have?
MJS: Mainly rheumatoid arthritis, systemic lupus erythematosus, or Sjögren’s syndrome.
WCR: How did Washington, DC, hit you and Jill for those 3 years?
MJS: We enjoyed it immensely. We had more time than ever before. We lived in Rockville, Maryland, and so were a good distance away from the District. Because of our love of the theater, we tried to see as many plays as we could at the Arena Stage and elsewhere in downtown Washington. You may remember that there was also a summer theater in Olney that was fairly close to us. We used to go there as well. The museums in DC, of course, were fabulous. Jill used to take our 2 children (with or without me) to Washington a couple of times a month to the various museums, especially the Smithsonian. We also enjoyed the National Gallery a great deal. Washington is a unique city. It was fun to be there.
WCR: Your first child was born in 1960. When was your second born?
MJS: Rob was born in 1962 when I was a senior medical student. They were both born in Chicago. Rob had a number of health problems his first year but, fortunately, all were corrected. Our last year in Chicago was difficult for Jill.
WCR: You had had 2 children before you interned and before you went to NIH. How did you decide to finish your internal medicine residency in Dallas?
MJS: I had only an internship and one year of residency training in internal medicine before NIH. Unlike some of my colleagues, I felt I needed more residency training. It was really a matter of whether I wanted to return to St. Louis or come to Dallas. I had applied for internship in Dallas but ranked Parkland under Barnes. I was aware of the excellent department at Southwestern because a close friend from Ohio State, Erwin Thal (now professor of surgery at Southwestern), had interned at Parkland. At NIH I kept meeting people who had been in Dallas—for example, Paul Richardson, Bill Kelley, and Stanley Watkins—and they raved about it. It really came down to how I would spend the year. If I had gone back to Barnes as a senior resident, I would essentially have had a repeat of the assistant residency, whereas the senior residency at Parkland offered a number of subspecialty rotations. In addition, I was flirting with the idea of rheumatology because of my NIH experience, and Dr. Morris Ziff was at Southwestern. So there were multiple attractions to Dallas.
WCR: What did the colleagues you mentioned say about Dallas? That it was a fantastic place for training, research, or both?
MJS: Their experiences had been as houseofficers, and they said the teaching in the Department of Medicine was great, mainly because of Dr. Donald Seldin. Others had told me the same thing, which is why I had considered Parkland for internship. Some of my NIH colleagues, especially those who had never been away from the East Coast, thought I was falling off the end of the earth by coming to Dallas.
WCR: When you came here, how did Dallas and Southwestern Medical Center strike you? This was 1968.
MJS: It was perhaps as big a change as Chicago had been. Moving from Montgomery County, Maryland, to Irving, Texas, was somewhat of a shock. It was a presidential election year and all over Irving were signs that said, “Irving is Wallace Country.” Many of the people we met in Irving seemed so different from those we had known in Maryland. This was particularly so for our children’s school experiences. At the medical school, I felt just as much at home as in Chicago, St. Louis, or Bethesda. Some of our neighbors in Irving were very thoughtful, generous, and kind to us that first year when Jill’s parents became seriously ill and died within a few months. Despite differences in political or social views, our new neighbors pitched in and helped us a great deal when Jill was away and I was working at Parkland; they often cared for our children. We quickly became aware of the pioneer spirit and friendliness that characterize people in Texas. We were most grateful, and it really taught us a lesson.
WCR: How did Southwestern strike you? How did the hospital and the staff there in internal medicine strike you? Were you pleased with your decision?
MJS: Yes, I liked it immediately. I had not spent much time in a city/county hospital before. Parkland is a different type of hospital than Barnes or Billings at the University of Chicago. The Department of Medicine at Southwestern was phenomenal. The people on the faculty were talented and enthusiastic teachers. There was, again, this sort of “can-do” pioneer spirit. Academically, Southwestern was still a young school, only about 25 years old then. The atmosphere was different than at Barnes because Parkland is a charity hospital and because Don Seldin has a different kind of teaching style than Carl Moore did. I had extraordinary training experiences at both places.
WCR: Seldin was different in what way?
MJS: Seldin’s approach to teaching was much more proactive than Carl Moore’s was. To some extent, Seldin put more pressure on the housestaff than Moore did. As I mentioned before, Dr. Moore was quiet but commanded enormous respect. He was a marvelous role model. Don Seldin is a great teacher, very supportive, and moderately dogmatic—in some ways a more effective teacher than Carl Moore. Seldin assembled a fantastic department at Southwestern, partly because he has an uncanny ability to identify talented young people.
WCR: After you had been here, you made up your mind to go into hematology/oncology. What tipped the scales there for you to decide on that subspecialty?
MJS: First, I had liked hematology/oncology at Chicago and Barnes. I tried to like rheumatology but it just wasn’t the same. The clinical experience at NIH was first-rate. The new branch chief, John Decker, arrived about the same time we did; he replaced Dr. Bunim, who had died suddenly. John was an excellent clinician and a warm person. I remember thinking during my time on the arthritis service at NIH that here I am, seeing the most interesting patients that exist in this specialty, and yet it seemed so descriptive. I liked immunology a lot, but there appeared to be a significant gap between basic immunology and clinical rheumatology. When I came to Dallas, my first rotation during that residency year was hematology with Gene Frenkel. I’d been in the lab for 15 months and was glad to return to clinical work; I also realized how much I enjoyed hematology and oncology. By the end of my first month in Dallas, I had decided to specialize in hematology/oncology.
WCR: After completion of that senior residency in internal medicine, you did a fellowship in hematology with Frenkel. How did that work out?
MJS: Fine. I spent most of the year almost as a junior staff member. I worked at Parkland and the Veterans Administration Hospital and wrote a number of grant proposals, which I hoped would provide some support the following year when I joined the faculty.
WCR: By the time you started your fellowship in hematology, you had already been more or less offered a faculty position at Southwestern. You knew you were going to be here for a while. By that time, you and Jill were getting used to Dallas. You finished your fellowship in 1970. You were on the faculty at Southwestern full time until 1976. How did you enjoy being a faculty member of this very high-powered medical center?
MJS: It was terrific! I had a great time. I was successful in obtaining some grant support, initially as an established investigator of the American Heart Association and from the Damon Runyon Cancer Research fund. As a junior faculty member, I enjoyed the teaching and tried to expand on some of the research I had done at NIH. By coincidence, a patient with Waldenström’s macroglobulinemia and a mixed cryoglobulin was referred to us during my fellowship. I did a lot of work with his IgM protein (IgMSie) and demonstrated that it was an antibody to IgG and nearly identical to the IgMLay protein we had studied at NIH. These 2 Waldenström macroglobulins were subsequently utilized by several investigators (Don Capra, Dennis Carson, Ralph Williams, and Vincent Agnello) in a number of studies on monoclonal rheumatoid factors over the next 20 years. I spent about half my time on the hematology consulting service at Parkland and also attended on the medicine service. I was busy, but it was stimulating and fun.
WCR: The decision to leave Southwestern in 1976 to come to Baylor University Medical Center must have been a difficult one for you. How did that come about?
MJS: I had never intended to leave Southwestern. I was happy there and had recently received a promotion to associate professor. I had been asked occasionally to come over to Baylor to give conferences or grand rounds and was impressed with the people I met and the quality of the medical staff. When I got a call from Reuben Adams, chairman of the search committee for director of the new cancer center, I interviewed but didn’t think much more about it. I was 38 years old and thought the position would likely go to a more senior physician. I didn’t hear anything for several months and then got another call. Things were much more serious at that point. I met more of the medical staff and administration, including Boone Powell, Sr., who struck me immediately as a brilliant and talented “can-do” person. The close relationship between the administration and the medical staff, not always present at other institutions, was clearly evident. I felt that the opportunity here at Baylor was exciting and that I’d be sorry if I didn’t give it a chance. It was a difficult decision.
WCR: And you’ve never regretted that move?
MJS: Not really. I’ve missed some aspects of academia but managed to maintain my teaching and research activities. And Baylor is a great institution! I’ve had many challenging opportunities and enjoyable experiences that may not have occurred at a medical school.
WCR: Marvin, you seem to be a triple threat. You’re a splendid physician, a devoted teacher, and yet you’ve been able to continue your research work on a very high level since coming to Baylor. Obviously, you didn’t need a university hospital or a medical school environment to continue to be quite productive. Which of your research endeavors have you been most pleased with?
MJS: I’ve enjoyed most of the research activities in which I’ve been involved, starting with the early experience at the University of Chicago that got me interested in cancer immunology. That first project had to do with trying to combine antitumor antibody with a virus in order to localize the antibody in tumor cells. Interestingly, as things tend to happen, just within the past year or two, there has been a rebirth of interest in socalled “oncolytic” viruses. My initial orientation toward cancer immunology then was further developed at NIH with the work on the Waldenström’s protein and the cryoglobulin mechanism. It was a thrill for me, a 29-year-old clinical associate at NIH, to have our work presented at the Cold Spring Harbor Symposium on Antibodies in 1967. About 270 people attended, including James Watson, Francis Crick, Macfarlane Burnet, Niels Jerne, Gerald Edelman, Cesar Milstein, and Baruj Benacerraf—all previous or future Nobel Prize winners. It was an exciting meeting and signaled the arrival and acceptance of immunology as a core science.
In Dallas, first at Southwestern and then at Baylor, I’ve tried to further expand my studies in clinical immunology, principally the investigation of patients with monoclonal gammopathies: Waldenström’s macroglobulinemia, multiple myeloma, and amyloidosis. I also collaborated with Jim Willerson, a friend from NIH who came to Dallas shortly after I did. We developed radioimmunoassays in order to quantify acute myocardial infarction—first with myoglobin and later with a creatine kinase isozyme. Collaborating with Jim was fun and productive. I also felt it was a way for me to further justify my generous grant support from the American Heart Association, which had been given for the monoclonal antibody studies. When I came to Baylor, I was asked by George Race to direct the immunology laboratory. Dr. Joe Newman has worked closely with me in this lab. We’ve always tried to conduct some research along with the service activities. With the generous support of Mr. Max Thomas, we established the Cancer Immunology Research Laboratory at the Sammons Cancer Center in 1982 and recruited Alex Tong to work with us on monoclonal antibodies and myeloma cell biology.
In the mid 1980s, we began our collaboration with Jonathan Uhr and Ellen Vitetta at Southwestern involving the use of B- cell immunotoxin to treat patients with non-Hodgkin’s lymphoma. An NIH program project grant supported these studies for 9 years. Most of the patients were treated at Baylor. The toxin we used, ricin, became well known in the 1970s when the KGB used a drop of it on an umbrella to assassinate a Bulgarian diplomat. In our study, a portion of the ricin was linked to a monoclonal antibody directed to B lymphoma cells. That project gave us clinical experience with monoclonal antibodies which, during the past 3 years, have become widely used therapeutic agents in oncology. The lymphoma project enlarged our scope of interest in hematologic malignancies, i.e., myeloma, macroglobulinemia, lymphoma, and leukemia.
I’ve also been involved in a number of investigative activities with Göran Klintmalm and the liver transplant team at Baylor. Our principal efforts have been in 3 areas: the use of neoadjuvant chemotherapy in transplanted patients with hepatocellular carcinoma (hepatoma), prevention of recurrent thrombosis in patients transplanted for Budd-Chiari syndrome, and graft-vs-host disease in liver transplant patients. The hepatoma study examined the use of preoperative, intraoperative, and postoperative doxorubicin to delay tumor recurrence after transplantation. Our initial results were promising: 50% of the treated patients were tumor free at 4 years, though late recurrences followed. It looked as if the chemotherapy “shifted the curve to the right.” Hepatoma patients transplanted without chemotherapy usually have disease recurrence within 2 years, so we planned to perform further studies using different chemotherapy dose and scheduling designs. However, the waiting time for donor livers has become much longer than previously, thereby precluding this approach. I hope that it can be investigated at some later date, since there is no clearly effective treatment for patients with hepatocellular carcinoma, and the incidence of this malignancy will very likely increase in this country because of its association with hepatitis C.
WCR: When you came to Baylor in 1976 to head the Sammons Cancer Center, how many people were involved in that activity?
MJS: The Cancer Center was created because it was an idea whose time had come. Boone Powell, Sr., was constantly building new facilities and services at Baylor. There was already a large number of cancer patients here. In the early 1970s, President Nixon signed the National Cancer Act. The cancer center concept then became much more visible. The new specialty of medical oncology also was established. Key members of the Baylor medical staff helped Mr. Powell plan the Cancer Center. George Race, Billie Aronoff, Mike Reese, and Dick Collier were leaders in this effort. When the Sammons building opened in May 1976, I became its director and the chief of oncology at Baylor. There were 3 other medical oncologists—Mike Reese, Dick Williams, and John Bagwell. Mike, Dick, John, and I formed the Division of Medical Oncology-Hematology in the Cancer Center; Mike was the first division head. Billie Aronoff was division head of surgical oncology. Dick Collier, who had been at Baylor for many years, was named division head of radiation oncology. Later, we created an oncologic pathology division with Bill Kingsley as head. When Allan Stringer joined Baylor in 1989, the gynecologic oncology division was established.
In addition to the various divisions, programs such as bone marrow transplantation and the patient education/psychosocial support activities were initiated within the Sammons Cancer Center. I recruited Joe Fay to start our marrow program, the first transplant program at Baylor. It has become one of the largest in the USA, performing >200 blood stem cell or marrow transplants annually. The Virginia R. Cvetko Center for Patient Education and Psychosocial Support was started through the leadership and efforts of a devoted and energetic patient. Virginia’s support group was the first of its kind at Baylor. Patient volunteers continue to be key participants. Lloyd Kitchens is the medical director of the Cvetko program, which now includes 12 different support groups serving hundreds of cancer patients and their families each year. All Cvetko services are free. We also have the annual Charlotte Johnson Barrett Lectureship (Figure 5) (see also article by Dr. Christina Puchalski in this issue) and the Deborah Kielman Rodriguez Patient Education Library in the Cvetko Center.
Figure 5.
With Wendy Harpham, MD, Barrett lecturer, 1995.
WCR: How many people are involved in the Cancer Center at Baylor now, including physicians and nonphysicians?
MJS: The Department of Oncology was created in 1976 at the medical staff level in addition to the Cancer Center administrative component. The Department of Oncology is the only multidisciplinary department at Baylor. Every member has a primary appointment in his or her own department (surgery, medicine, pathology, radiology, gynecology, etc.) and a secondary appointment in the Department of Oncology. I believe it is the second largest department at Baylor, with about 140 medical staff members.
Outreach activities began in 1979 and were designed according to the needs of physicians in the various communities. They most often requested medical oncology consultation. Our first such activity was in Odessa, Texas, and later involved other cities. These efforts were well received and led to the concept of multicity practice and subsequent development of Texas Oncology, PA. The visionary leadership of Dr. Mike Reese was responsible for Texas Oncology’s growth into one of the largest oncology practice groups in the country and played a major role in developing the Cancer Center at Baylor. The long-standing relationship between Baylor’s medical oncologists and the institution has been productive and mutually supportive. In 1994, Baylor and Texas Oncology became partners through the Sammons Cancer Center, thus further augmenting the strengths of both organizations. The medical oncologists, originally housed at the Cancer Center, outgrew the available space and moved to outside offices for several years but returned in 1994. Now Sammons Cancer Center is a joint venture between Baylor and Texas Oncology with its new management company, US Oncology. It’s been an interesting evolution during the past 25 years.
WCR: Marvin, you have a number of administrative tasks. You do a great deal of teaching at Baylor. You have a large practice. I know that there is not a day that is absolutely typical, but what is your usual day like? When I come into Baylor your car is usually there. When I leave at night, your car is usually there. What time do you wake up in the morning? What time do you get to the hospital? What time do you leave the hospital as a rule? What time do you go to bed at night?
MJS: As you know, Baylor has a lot of meetings, and the Cancer Center is no exception. I come in most mornings either for a meeting or site tumor conference at 6:30 or 7:00 am. I attend some but not all of these conferences. Generally, I then make inpatient rounds. Four days a week I see outpatients. I do not have a large practice; it is rather modest. I spend time in the immunology laboratory every day, interpreting tests. I have regular teaching conferences with the medical students, residents, and fellows (Figure 6). I meet with the junior students for a case conference every Monday and conduct a microscope conference with the fellows, residents, and others on our service every Tuesday afternoon. I give occasional conferences to the internal medicine housestaff and attend for 1 month on the medicine service. On Thursdays, I try to catch up on administrative duties. It’s sort of chaotic and I’m slow, but I enjoy it.
Figure 6.
With 1999–2001 medical oncology fellows, Drs. J. Melear, H. Jordan, D. Wilder, and C. Stokoe.
WCR: What time do you get up in the morning?
MJS: Usually around 5:00 or 5:30 am.
WCR: What time do you leave the hospital as a general rule?
MJS: It varies, often about 7:00 pm.
WCR: You get home around 7:30 pm. What time do you go to bed?
MJS: In recent years, earlier and earlier. As I told you, when I was growing up I had the luxury of sleeping late because I lived close to school. One thing about coming to Dallas, probably the only thing I haven’t been delighted with, is this urge to begin morning activities before dawn. I’ve never gotten accustomed to getting up so early in the morning, so I usually fall asleep at 10:00 or 11:00 pm.
WCR: After dinner, do you get back to medical activities or do you tend to do something nonprofessional every night after getting home?
MJS: Often I work on a manuscript or put slides together for a talk. It depends on what needs to be done, but often I spend a little time after dinner. We talk to our children frequently over the phone. And Jill and I enjoy watching old movies on TV.
WCR: You received several “best teacher of the year” awards from the medical housestaff at Baylor. Those must have been very gratifying to you.
MJS: Yes, they were.
WCR: Several years ago I understood that you were offered a very nice position somewhere else and the housestaff really were quite upset with the possibility that you might leave Baylor. What did they do to try to keep you from leaving Baylor?
MJS: They wrote me a letter. They urged me to do whatever I thought best but said I was important to the teaching program at Baylor and that I would be sorely missed. It was signed by every member of the internal medicine housestaff and made a very large impact on me.
WCR: Despite doing a lot of teaching at Baylor, you have continued your relationship with Southwestern. You still do a good bit of teaching over there, or at least in the first few years you were at Baylor you did. What’s the situation now?
MJS: I don’t attend at Parkland anymore because I’m involved all year round with the junior medical students who come to Baylor for internal medicine. I actually do more teaching here than when I was a full-time faculty member because it is all the time. I’m also in charge of the internal medicine junior clerkship administratively, so I get to spend a good bit of time with the students.
WCR: How many medical students from Southwestern are generally at Baylor at any one time?
MJS: It varies. Generally I would say 7 to 10 junior students for a 6-week rotation. About 65 students per year.
WCR: Marvin, you were most gracious in getting me into the American Osler Society and you’ve propagated some of Osler’s teachings to housestaff and other staff for many years. You obviously are the number one medical historian at Baylor. How did you get interested initially in medical history and specifically in Sir William Osler?
MJS: I suppose like many people I was vaguely aware of Osler. I remember buying a copy of Aequanimitas in medical school. I had the desire to learn more about him because everyone had considered him such a great physician and teacher and I wanted to know why. I never had the time to really read that book or to learn about him; it was always something that was tucked away as a “to-do” item. Shortly after coming to Baylor, we were at a meeting in San Francisco and wandered into an antiquarian bookstore, where I found a first edition of his textbook. Jill has always encouraged me in everything, and she bought me Osler’s book. That launched my overt effort to learn about him. During the early 1980s, I finally started reading some of his works as well as books and articles about him. Everything I came across just seemed like pure gold. He was such an inspirational person, a great clinician and a remarkable educator. He wrote beautifully, and what he had to say was worth knowing about. His precepts and teachings have timeless relevance and are valuable guideposts (Figures 7 and 8).
Figure 7.
In front of a portrait of his hero, Sir William Osler, at the Royal College of Physicians in London.
Figure 8.
With Jill and Rob in William Osler’s study, 13 Norham Gardens, Oxford.
WCR: I presume your study of Osler has had a considerable impact on you from the standpoint of being a patient physician as well as being a teacher of physicians and medical students. Is that correct?
MJS: Yes. I think that Osler was in many ways the ideal physician-educator. That’s why he has had such an enduring influence on so many people in so many different places. He possessed many qualities worth emulating, but I don’t think there has ever been anyone quite like him. He combined the art and science of medicine perhaps better than anyone else and remains a role model for us all. While reading about Osler, I came across John Fulton’s excellent biography of Harvey Cushing. In the front of the book are the following words: “Live as to die tomorrow, learn as to live for ever” (attributed to Isidore of Seville, fl. 630 AD). I believe this aphorism applied to Osler as well as to Cushing.
WCR: You showed me your beautiful microscope collection. How did you get involved in collecting microscopes?
MJS: I use a microscope every day in practicing hematology/ oncology (Figure 9), and I was becoming ever more interested in medical history. I began looking for an old brass microscope for my office. Jill and I were in London and saw some magnificent instruments but didn’t buy any. After we returned to Dallas, she found a mid-19th century microscope in an antique store in Highland Park and bought it for me. We started learning about antique microscopes together, reading various books and articles. When we visited other cities, we would look for antiquarian books or microscopes, or both. Finding the microscopes has been a large part of the fun. We’ve ended up in instrument shops in England and France, as well as in the home of a retired physician in Toronto. Another time we discovered some antique microscopes in a pawnshop across from New York University Medical School. The employees there didn’t even know what they had buried in a cabinet; Jill found them. Unbeknownst to me until I started reading about Osler, he learned to use a microscope as a schoolboy and introduced clinical microscopy into diagnosis at McGill, the University of Pennsylvania, and Johns Hopkins. Osler’s clinical microscopy laboratory at Hopkins was the place that Max Wintrobe did his work on defining normal blood values and various anemias a generation later. So a number of things have come together to encourage our interest in antiquarian microscopes.
Figure 9.
At the microscope.
WCR: How many microscopes do you have now?
MJS: I think we have about 30. When the library was dedicated a couple of years ago, we gave 12 to Baylor.
WCR:I know you have an interest in bioethics. Tell me about that.
MJS:Al Jonsen has claimed that the bioethical era in medicine began in 1960 with development of the Scribner shunt, allowing patients with chronic renal failure to be kept alive on hemodialysis. I was a medical student then. Later, as a houseofficer at Barnes, I recall sitting in on some of the meetings where it was decided which of our patients would (and wouldn’t) be dialyzed. At NIH, I became concerned that some of our patients were being put on experimental protocols without being told much about the dangers and side effects. At that same time, publicity surfaced about Chester Southam, a well-known cancer investigator at Memorial Sloan-Kettering in New York, who injected live cancer cells into elderly individuals without their knowledge. I knew who Southam was and remember giving a conference about consent in human experimentation to my clinical associate colleagues at NIH. By the time I became a faculty member at Southwestern in 1970, these and other experiences had convinced many people that there was a large gap between some of the technological advances in medicine and protection for patients. I invited Leon Kass, one of my classmates at Chicago who had become well known in bioethical circles, to speak at Southwestern.
By 1975, I found myself chairing an ad hoc bioethics committee at the medical school. We recommended that a bioethics course be incorporated into the curriculum. Nothing happened. Four years later, Kern Wildenthal asked me to organize a course for the Southwestern sophomore medical students. We were given 12 contact hours (four 3-hour sessions) during the Introduction to Disease course during the latter part of the year. After a lecture, we split into small discussion groups using a case conference format. Each group had 2 discussion leaders— one a member of the full-time faculty and the other a practicing physician from the community. The first bioethics course for Southwestern medical students was given in 1980. I served as one of the discussion leaders and enjoyed it; the students seemed to as well. I was glad to see the subject finally get off the ground. By the time Kern requested that I design and implement the course, I was at Baylor and the logistics involved in recruiting 30 faculty discussion leaders were complicated. After the second year, I turned it over to people at the medical school. The present course has a format similar to our original one. I’ve remained interested in bioethics, especially as it relates to oncology and to end-of-life care. Last year, Bob Fine and I gave the AMA EPEC (education for physicians on end-of-life care) course at Baylor. I also give talks on bioethics occasionally. Looking back, it’s amazing to realize how much medicine has changed during our careers!
WCR: Marvin, could you talk a bit about your family? You’ve mentioned Jill numerous times here and your 2 lovely children.
MJS: Nancy is our older child (Figure 10). She is a speech pathologist and works in the school system near Boca Raton, Florida. She was married last year. She enjoys working with young speech-impaired children and really helps them. Rob is 2 years younger and lives in the Los Angeles area (Figure 11). He was married about 3 years ago. He and his wife, Melissa, presented us with our first grandchild last January (Figure 12). Jill and I are thrilled! Rob graduated from the University of Southern California in the fine arts program. He got a part on the Mr. Belvedere TV show when he was a senior. It ran for 5 years. He speaks of Belvedere as his graduate school, and it was. In more recent years he has been producing and directing documentary films. He’s made several aviation documentaries that have been shown on the A&E and History Channels. One of them on the navy’s Blue Angels won a Cable Ace Award. He also did a director’s teaching movie for film schools in conjunction with the Directors Guild of America. Needless to say, I'm very proud of both our children.
Figure 10.

With son, Rob, at the Super Bowl.
Figure 11.

With daughter, Nancy, in New York City.
Figure 12.
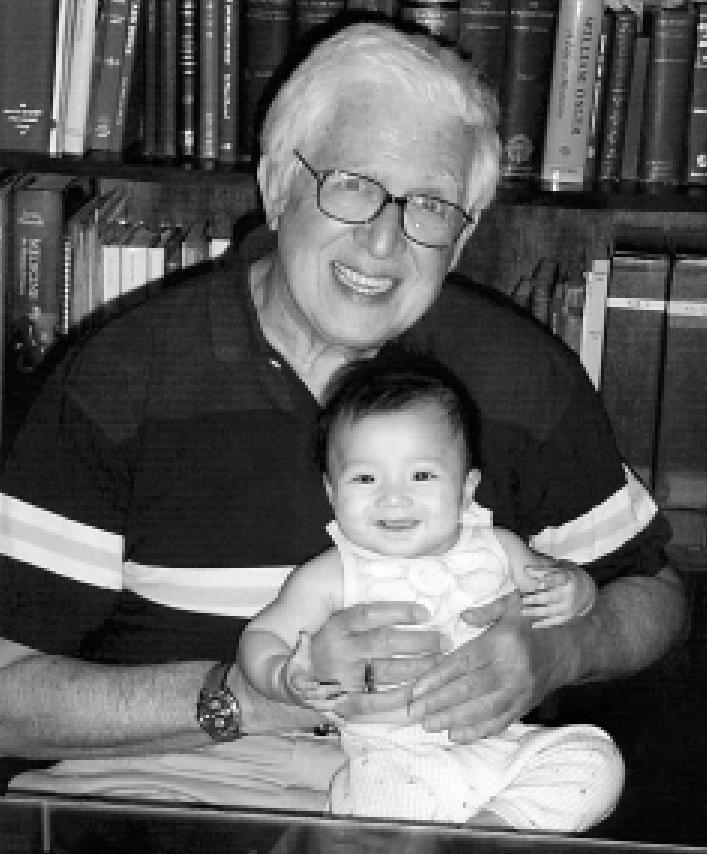
With granddaughter, Sabrina Jillian Stone, age 5 months.
tors Guild of America. Needless to say, I’m very proud of both our children.
WCR: You got him interested in theater and arts and acting from going to the theater in Dallas primarily?
MJS: Rob began to play the drums at age 5 and wrote a short novel when he was 12. He began in the Dallas Theater Center’s children’s program when he was in junior high school. At the theater center, Rob had the opportunity to be in a world premiere of one of Preston Jones’ plays, Santa Fe Sunshine. It was reviewed in Variety, and his name was listed in the cast. He was also in a number of plays at Greenhill, including some lead roles. We didn’t know he was going to major in drama in college until it came time to apply. He had talked previously about premed and was concerned that we might be opposed to drama. Jill and I encouraged him to do it.
WCR: You are a busy man. You’re in demand. You’re on several national committees. You give talks at a number of places. How many trips outside of Dallas do you go on a year? How do you work your travel into your present agenda?
MJS: With difficulty, just like you and many of our colleagues do. Our vacations are often combined with medical meetings. There’s been a particular string of them recently. I would say on average I attend about 6 meetings a year in various places.
WCR: I know you’ve been honored in a number of ways. I gather the Marvin Stone Library is particularly important to you. How did that come about?
MJS: It is. The library was established through the kindness and generosity of Bobbie and Leo Fields and the M. B. and Edna Zale Foundation (Figure 13). Bobbie has been a patient of mine for several years. She and Leo had asked several times about doing something for me. As they got to know me better, it became evident to them that there was nothing I would like more than a library. And they were right; I’m thrilled and very honored. We’ve tried to give it a historical flavor by putting some of my antiquarian medical books and microscopes there, as well as a bust of William Osler. My favorite Osler aphorism is on a plaque in the library: “To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” But it is also the working library for the investigators at the Baylor Institute for Immunology Research (BIIR).
Figure 13.

With Bobbie and Leo Fields at the Stone Library dedication.
Bobbie and Leo made all that possible. I’m very grateful to them. The library dedication was one of the most memorable events of my life (Figure 14). (See Marvin J. Stone, MD: a beloved physician, mentor, and friend. BUMC Proceedings 1999;12:265–266.)
Figure 14.
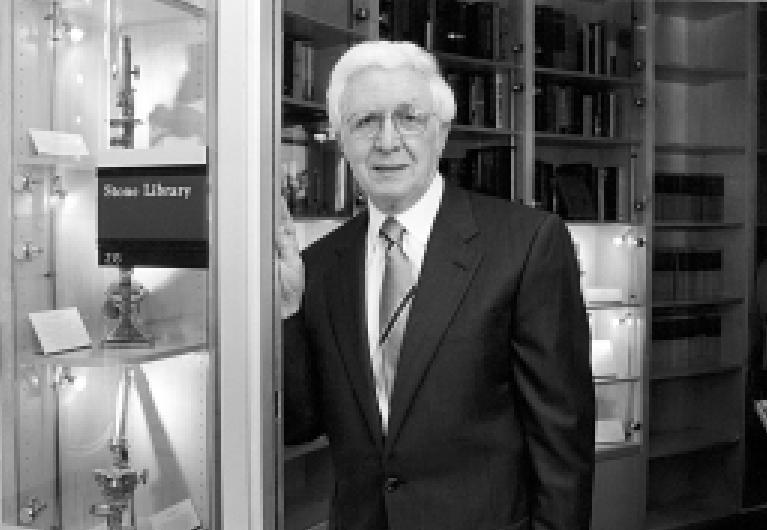
At the entrance to the Marvin J. Stone Library.
WCR: You’ve done a lot of things since you came to Baylor in 1976, which is now 25 years ago, and you’ve had considerable impact at other places before you got to Baylor. As you look back over your sterling career, what are you most proud of professionally?
MJS: I’m not sure. I’ve been very fortunate all the way through and have been lucky to have had exposure to a lot of outstanding individuals, particularly teachers and peers. A supportive family and dedicated teachers are so important. I’ve enjoyed everything I’ve done, whether it involved patient care, teaching, or research. I was pleased to receive my MD degree with honors from the University of Chicago. The experiences at Barnes and NIH were outstanding. Dallas has been fabulous. The opportunity to come to Baylor and see the Cancer Center grow and develop has been particularly gratifying. The same has been true of medical oncology as a specialty. I’ve always enjoyed my teaching activities and am delighted with the library named for me here at Baylor.
WCR: Your day-to-day life is quite varied. You are doing different things throughout the day. The variety makes things quite nice. Is that what you are saying to some extent?
MJS: Yes, but like everything else, it has advantages and disadvantages. The disadvantages of variety are that at times you feel like you’re not doing anything very well and that you are more of a dilettante as opposed to someone who seriously pursues one area. On the other hand, I’ve always felt that teaching and research make me a better physician. My students have taught me a lot more than I’ve taught them. It’s wonderful working with young people who are just beginning their medical careers. Research and the quest for new knowledge are the way medicine advances. In some ways, research is more difficult and provides a different kind of satisfaction. Both teaching and research bring patient care into better focus. And caring for patients is what medicine is all about.
WCR: It seems to me that you and Charles Bryan and maybe Mark Silverman live your lives more like William Osler than about any other people I’ve encountered.
MJS: It’s kind of you to say that.
WCR: You are doing the same thing that Osler did, just 100 years later, in many ways. You say you use the microscope every day. What are you looking at in the microscope?
MJS: Blood smears, bone marrows, biopsies of various sorts. I try to look at the pathological material on every patient I see because it’s the backbone of diagnosis.
WCR: You have an appointment in the pathology department at Baylor now. You’ve had that ever since you’ve been here. I don’t think there are many people who could blend the personalities that you have in a cancer center—the oncologists, the hematologists, the surgeons, the radiation oncologists, the pathologists—as well as you have. Everybody seems to get along. I’m a little disappointed that we haven’t been able to pull that off quite as well in the heart center at Baylor. I’m sure that’s not been an easy thing for you to do for 25 years.
MJS: I’ve always regarded it as an experiment. We really did not have a model to follow. We felt our way along. I’ve always thought that my goal at the Cancer Center has been to facilitate multidisciplinary interaction among the medical staff. It’s important because so much of cancer care, as it has developed over the past 25 or 30 years, is heavily dependent on effective multidisciplinary interaction. Before 1970, cancer care was mainly surgery or surgery and radiation therapy. There was a little chemotherapy. But major advances have been made in diagnosis and therapy during the past quarter century. Now multimodal therapy is essential for best results in patients with many types of cancer. I’m proud of what we have at Baylor and believe that our strengths are due mainly to our talented and dedicated medical staff and administration. Boone Powell, Sr., and Boone Powell, Jr., always were very supportive. The various site tumor conferences, all of which are multidisciplinary, are beneficial educational case-management tools for us all. These conferences help develop the expertise of our staff and thus improve patient care. Paula Holder and Sylvia Coats have provided inestimable assistance in helping me with Cancer Center administrative activities during the past 16 years.
WCR: You’ve been director of the Cancer Center for 25 years. I can tell you that in cardiology divisions in university hospitals across the country, there is not a single director of cardiology who has been in the position for 25 years. The longest survivor as chief of a cardiology division in a university hospital is Bob Myerberg at the University of Miami, and he’s been there 22 years. That’s it.
You’ve received a number of honors in your career—masterships of the American College of Physicians and a number of others. Which ones are you particularly proud of? What does the mastership of the American College of Physicians mean? How many masters are there in this country? You received that award this year. How many others received that award with you?
MJS: The mastership is an honor given each year to a number of physicians by the American College of Physicians-American Society of Internal Medicine. Baylor has had several masters—for example, Ralph Tompsett, our former chief of medicine; John Fordtran, our more recent chief of medicine; and Al Roberts, a Baylor staff member for many years. There may have been others. When I was honored, our colleagues Mike Emmett and Lloyd Kitchens also were made masters. So this year 3 of the 42 physicians awarded new ACP masterships were from our hospital. During the past decade or so, I’ve participated in various roles with the college and have had the opportunity to meet and work with a lot of talented and stimulating people. The college is an outstanding organization, and so I was very honored to receive the mastership.
WCR: You were honored by your high school, Bexley High School, in Columbus recently. What was that about?
MJS: Judah Folkman, who is a well-known cancer researcher at Harvard, graduated from Bexley High School in 1950. I graduated in 1955, so he was gone by the time I arrived in high school, but I heard a lot about him even then. His father was a rabbi and a distinguished scholar in Columbus, and I knew Judah’s younger brother and sister. I have followed his career through the years. Folkman has developed the field of angiogenesis almost singlehandedly. The study of angiogenesis inhibition in cancer and its stimulation in cardiovascular disease has become an exciting area of medical research. Many clinical trials are now in progress. About 2 years ago, Judah’s classmates established a fund in his honor. The purpose of the fund is to bring people to Bexley High School, preferably alumni, who act as visiting scientists and hopefully inspire the students to pursue careers in science or medicine. I was invited last month and had a wonderful time. Another Bexley graduate who was 2 years ahead of me and recently retired as professor of medicine at Ohio State, Earl Metz, participated with me (Figure 15). We spent 2 days with the students and gave a number of talks. I presented the school with a 19th-century microscope from my collection and a copy of Mike Brown’s and Joe Goldstein’s Nobel lecture which they graciously autographed for the students. Going back to Bexley was a tremendous experience; Earl and I really enjoyed it.
Figure 15.
With Dr. Earl Metz, Judah Folkman Visiting Scientist Program, Bexley High School, Columbus, Ohio.
WCR: Are there some goals you want to accomplish before you retire?
MJS: I’d like to develop some new programs and expand others at the Cancer Center, for example, in cancer prevention, genetic counseling, and psychosocial support activities. I’m optimistic about our research endeavors as well; they’re so important. I’d like to continue teaching and hope I’ll be able to do some more writing, especially in medical history, which I really enjoy. During the past few years, I’ve become more interested in ways of reducing medication errors and improving end-of-life care. Both have finally gained considerable attention, and I hope to work with our colleagues at Baylor on these challenging areas in the future. I was surprised and honored to have recently been elected an officer of the American Osler Society (Figure 16). I look forward to participating in those activities, as it’s a terrific organization and one which, as we’ve discussed, is very close to my heart. People are very fortunate if they can spend their days doing what they enjoy. That is truly a gift. I’m one of those people.
Figure 16.

Giving a presentation to the American Osler Society at the Royal College of Physicians.
WCR: It sounds as if you and Jill are best friends. Is that so?
MJS: Not only is she my best friend, we’ve been partners throughout most of our lives (Figure 17). Jill is the most loving, supportive, and considerate person I could ever imagine. I’ve told her she’s made my life like a Renoir portrait. She has provided a wonderful life experience for me and our children. I’m a lucky man indeed! Some years ago, Rob got actor James Stewart to autograph a poster from his film It’s a Wonderful Life for our wedding anniversary. It hangs on the wall in our bedroom.
Figure 17.

With Jill on their 35th wedding anniversary. Photo: Gittings.
WCR: Jill is actually quite a scholarly person. Is that correct?
MJS: She wouldn’t admit to that, but she is. Jill left college after 2 years because we were married and went to Chicago. As we discussed, she worked while I was in medical school. Although she sat in on some classes at Chicago and later at Washington University in St. Louis, she really didn’t pursue her formal education until we came to Dallas and the kids were in school. Then she graduated from Southern Methodist University Phi Beta Kappa and earned a master’s degree in urban studies at SMU. Jill did her master’s thesis in 1976 on the social, economic, and political history of medical care in the USA. Thus, she had a good background when Kenneth Ludmerer’s book, Time to Heal, was published 2 years ago. She enjoyed reading Ken’s splendid book. (See Stone JF. Book review: Time to Heal. BUMC Proceedings 2001;14:312–313.)
WCR: Marvin, not only on my own behalf but of course for the readers of BUMC Proceedings, I want to thank you for pouring out your soul, so to speak, so all of us can get to know you better. Thank you.
MJS: Thank you, Bill. It has been my pleasure.
References
- 1.Stone MJ, Dzoga K, Wissler RW. Combined inhibitory effect of antitumor antibody and an oncolytic virus on the solid Ehrlich tumor. Lab Invest. 1962;11:306–310. [PubMed] [Google Scholar]
- 2.Stone MJ, Metzger H. The valence of a Waldenström macroglobulin antibody and further thoughts on the significance of paraprotein antibodies. Cold Spring Harb Symp Quant Biol. 1967;32:83–88. [Google Scholar]
- 3.Stone MJ, Metzger H. Study of macromolecular interactions by equilibrium molecular sieving. J Biol Chem. 1968;243:5049–5055. [PubMed] [Google Scholar]
- 4.Stone MJ, Metzger H. Binding properties of a Waldenström macroglobulin antibody. J Biol Chem. 1968;243:5977–5984. [PubMed] [Google Scholar]
- 5.Stone MJ, Metzger H. The specificity of a monoclonal macroglobulin (gamma M) antibody: reactivity with primate gamma G immunoglobulins. J Immunol. 1969;102:222–228. [PubMed] [Google Scholar]
- 8.Stone MJ. Studies on monoclonal antibodies. I. The specificity and binding properties of a Waldenström macroglobulin with anti-gamma G activity. J Lab Clin Med. 1973;81:393–409. [PubMed] [Google Scholar]
- 10.Stone MJ, Fedak JE. Studies on monoclonal antibodies. II. Immune complex (IgM-IgG) cryoglobulinemia: the mechanism of cryoprecipitation. J Immunol. 1974;113:1377–1385. [PubMed] [Google Scholar]
- 12.Stone MJ, Frenkel EP. The clinical spectrum of light chain myeloma. A study of 35 patients with special reference to the occurrence of amyloidosis. Am J Med. 1975;58:601–619. doi: 10.1016/0002-9343(75)90496-9. [DOI] [PubMed] [Google Scholar]
- 15.Stone MJ, Willerson JT, Gomez-Sanchez CE, Waterman MR. Radioimmunoassay of myoglobin in human serum. Results in patients with acute myocardial infarction. J Clin Invest. 1975;56:1334–1339. doi: 10.1172/JCI108211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Willerson JT, Stone MJ, Ting R, Mukherjee A, Gomez-Sanchez CE, Lewis P, Hersh LB. Radioimmunoassay of creatine kinase-B isoenzyme in human sera: results in patients with acute myocardial infarction. Proc Natl Acad Sci U S A. 1977;74:1711–1715. doi: 10.1073/pnas.74.4.1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone MJ, Waterman MR, Harimoto D, Murray G, Willson N, Platt MR, Blomqvist G, Willerson JT. Serum myoglobin level as diagnostic test in patients with acute myocardial infarction. Br Heart J. 1977;39:375–380. doi: 10.1136/hrt.39.4.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stone MJ. Plasma cell dyscrasias. In: Berkow R, editor. The Merck Manual. 13th ed. West Point, Pa: Merck Sharp & Dohme Research Laboratories; 1977. 339–344; also 14th ed., 1982; 15th ed., 1987; 16th ed., 1992; home ed., 1997. [Google Scholar]
- 30.Gilkeson G, Stone MJ, Waterman M, Ting R, Gomez-Sanchez CE, Hull A, Willerson JT. Detection of myoglobin by radioimmunoassay in human sera: its usefulness and limitations as an emergency room screening test for acute myocardial infarction. Am Heart J. 1978;95:70–77. doi: 10.1016/0002-8703(78)90398-8. [DOI] [PubMed] [Google Scholar]
- 46.Hirsch VJ, Neubach PA, Parker DM, Reese MH, Stone MJ. Paroxysmal nocturnal hemoglobinuria. Termination in acute myelomonocytic leukemia and reappearance after leukemic remission. Arch Intern Med. 1981;141:525–527. doi: 10.1001/archinte.141.4.525. [DOI] [PubMed] [Google Scholar]
- 48.Stone MJ. A Bibliography of Biomedical Ethics. Austin: Texas Medicine, 1981. See editorial: References offer help with biomedical ethics problems. Texas Med. 1981;77(12):6. [Google Scholar]
- 49.Stone MJ, Lieberman ZH, Chakmakjian ZH, Matthews JL. Coexistent multiple myeloma and primary hyperparathyroidism. JAMA. 1982;247:823–824. [PubMed] [Google Scholar]
- 51.Stone MJ, Willerson JT, Waterman MR. Radioimmunoassay of myoglobin. Methods Enzymol. 1982;84:172–177. doi: 10.1016/0076-6879(82)84014-7. [DOI] [PubMed] [Google Scholar]
- 57.Stone MJ. Monoclonal gammopathies: clinical aspects. In: Ritzmann SE, editor. Protein Abnormalities: Vol. 2, Pathology of Immunoglobulins: Diagnostic and Clinical Aspects. 8. Vol. 2. New York: Alan R Liss; 1982. pp. 161–236. [Google Scholar]
- 61.Stone MJ, Willerson JT. Myoglobinemia in myocardial infarction. Int J Cardiol. 1983;4:49–52. doi: 10.1016/0167-5273(83)90213-9. [DOI] [PubMed] [Google Scholar]
- 65.Tong AW, Lee J, Stone MJ. Characterization of two human small cell lung carcinoma-reactive monoclonal antibodies generated by a novel immunization approach. Cancer Res. 1984;44:4987–4992. [PubMed] [Google Scholar]
- 66.Stone MJ, Hirsch VJ. Splenic function in amyloidosis. In: Glenner GG, Osserman EF, Benditt EP, Calkins E, Cohen AS, Zucker-Franklin D, editors. Amyloidosis. New York: Plenum Press; 1986. pp. 583–590. [Google Scholar]
- 67.Tong AW, Lee JC, Stone MJ. Discrimination of human small cell and nonsmall cell lung tumors by a panel of monoclonal antibodies. J Natl Cancer Inst. 1986;77:1023–1033. [PubMed] [Google Scholar]
- 69.Tong AW, Lee JC, Stone MJ. Characterization of a monoclonal antibody having selective reactivity with normal and neoplastic plasma cells. Blood. 1987;69:238–245. [PubMed] [Google Scholar]
- 73.Tong AW, Lee JC, Fay JW, Stone MJ. Elimination of clonogenic stem cells from human multiple myeloma cell lines by a plasma cell-reactive monoclonal antibody and complement. Blood. 1987;70:1482–1489. [PubMed] [Google Scholar]
- 77.Tong AW, Lee JC, Stone MJ. Expression of plasma cell-associated nonlight chain antigens in patients with plasma cell dyscrasia and amyloidosis. In: Isobe T, Araki S, Uchino F, Kito S, Tsubura E, editors. Amyloid and Amyloidosis. New York: Plenum Press; 1988. pp. 185–190. [Google Scholar]
- 80.Tong AW, Lee JC, Wang RM, Ordonez G, Stone MJ. Augmentation of lymphokine-activated killer cell cytotoxicity by monoclonal antibodies against human small cell lung carcinoma. Cancer Res. 1989;49:4103–4108. [PubMed] [Google Scholar]
- 81.Stone MJ, Klintmalm G, Polter D, Husberg B, Egorin MJ. Neoadjuvant chemotherapy and orthotopic liver transplantation for hepatocellular carcinoma. Transplantation. 1989;48:344–347. doi: 10.1097/00007890-198908000-00031. [DOI] [PubMed] [Google Scholar]
- 82.Tong AW, Lee J, Wang RM, Dalton WS, Tsuruo T, Fay JW, Stone MJ. Elimination of chemoresistant multiple myeloma clonogenic colony-forming cells by combined treatment with a plasma cell-reactive monoclonal antibody and a P-glycoprotein-reactive monoclonal antibody. Cancer Res. 1989;49:4829–4834. [PubMed] [Google Scholar]
- 84.Stone MJ. Amyloidosis: a final common pathway for protein deposition in tissues. Blood. 1990;75:531–545. [PubMed] [Google Scholar]
- 91.Goldstein R, Clark P, Klintmalm G, Husberg B, Gonwa T, Stone M. Prevention of recurrent thrombosis following liver transplantation for BuddChiari syndrome associated with myeloproliferative disorders: treatment with hydroxyurea and aspirin. Transplant Proc. 1991;23(1 Pt 2):1559–1560. [PubMed] [Google Scholar]
- 92.Vitetta ES, Stone M, Amlot P, Fay J, May R, Till M, Newman J, Clark P, Collins R, Cunningham D, Ghetie V, Uhr J, Thorpe PE. Phase I immunotoxin trial in patients with B-cell lymphoma. Cancer Res. 1991;51:4052–4058. [PubMed] [Google Scholar]
- 97.Stone MJ, Klintmalm GB, Polter D, Husberg BS, Mennel RG, Ramsay MA, Flemens ER, Goldstein RM. Neoadjuvant chemotherapy and liver transplantation for hepatocellular carcinoma: a pilot study in 20 patients. Gastroenterology. 1993;104:196–202. doi: 10.1016/0016-5085(93)90852-4. [DOI] [PubMed] [Google Scholar]
- 100.Collins RH, Jr, Anastasi J, Terstappen LW, Nikaein A, Feng J, Fay JW, Klintmalm G, Stone MJ. Brief report: donor-derived long-term multilineage hematopoiesis in a liver-transplant recipient. N Engl J Med. 1993;328:762–765. doi: 10.1056/NEJM199303183281104. [DOI] [PubMed] [Google Scholar]
- 102.Amlot PL, Stone MJ, Cunningham D, Fay J, Newman J, Collins R, May R, McCarthy M, Richardson J, Ghetie V, Ramilo O, Thorpe PE, Uhr JW, Vitetta ES. A phase I study of an anti-CD22-deglycosylated ricin A chain immunotoxin in the treatment of B-cell lymphomas resistant to conventional therapy. Blood. 1993;82:2624–2633. [PubMed] [Google Scholar]
- 108.Tong AW, Zhang BQ, Mues G, Solano M, Hanson T, Stone MJ. AntiCD40 antibody binding modulates human multiple myeloma clonogenicity in vitro. Blood. 1994;84:3026–3033. [PubMed] [Google Scholar]
- 110.Stone MJ. The wisdom of Sir William Osler. Am J Cardiol. 1995;75:269–276. doi: 10.1016/0002-9149(95)80034-p. [DOI] [PubMed] [Google Scholar]
- 115.Stone MJ. Transplantation for primary hepatic malignancy. In: Busuttil RW, Klintmalm GB, editors. Transplantation of the Liver. Vol. 12. Philadelphia: WB Saunders; 1996. pp. 120–129. [Google Scholar]
- 117.Tong AW, Su D, Mues G, Tillery GW, Goldstein R, Klintmalm G, Stone MJ. Chemosensitization of human hepatocellular carcinoma cells with cyclosporin A in post-liver transplant patient plasma. Clin Cancer Res. 1996;2:531–539. [PubMed] [Google Scholar]
- 118.Stone MJ, Sausville EA, Fay JW, Headlee D, Collins RH, Figg WD, StetlerStevenson M, Jain V, Jaffe ES, Solomon D, Lush RM, Senderowicz A, Ghetie V, Schindler J, Uhr JW, Vitetta ES. A phase I study of bolus versus continuous infusion of the anti-CD19 immunotoxin, IgG-HD37-dgA, in patients with B-cell lymphoma. Blood. 1996;88:1188–1197. [PubMed] [Google Scholar]
- 124.Stone MJ. Henry Bence Jones and his protein. J Med Biogr. 1998;6:53–57. doi: 10.1177/096777209800600112. [DOI] [PubMed] [Google Scholar]
- 129.Stone MJ. Immunology near the millennium. BUMC Proceedings. 1998;11:203–206. [Google Scholar]
- 132.Fine KD, Stone MJ. Alpha-heavy chain disease, Mediterranean lymphoma, and immunoproliferative small intestinal disease: a review of clinicopathological features, pathogenesis, and differential diagnosis. Am J Gastroenterol. 1999;94:1139–1152. doi: 10.1111/j.1572-0241.1999.01057.x. [DOI] [PubMed] [Google Scholar]
- 138.Stone MJ. Major contributor. In: Huth EJ, Murray TJ, editors. Medicine in Quotations. Views of Health and Disease Through the Ages. Philadelphia: American College of Physicians; 2000. [Google Scholar]
- 139.Stone MJ. What is Waldenström's macroglobulinemia? Clinical Lymphoma. 2000;1:44–45. [Google Scholar]
- 140.Stone MJ. Book review: William Osler: A Life in Medicine, by Michael Bliss. BUMC Proceedings. 2000;13:260. [Google Scholar]
- 143.Stone MJ. Goals of care at the end of life. BUMC Proceedings. 2001;14:134–137. doi: 10.1080/08998280.2001.11927748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Stone MJ. Polycythaemia vera: Osler-Vaquez disease. J Med Biogr 2001;9:99–103. (Selected for The Persisting Osler III Volume. American Osler Society, in press.) [DOI] [PubMed]



