Abstract
In order to identify Rickettsia prowazekii in lice, we developed a panel of 29 representative monoclonal antibodies selected from 187 positive hybridomas made by fusing splenocytes of immunized mice with SP2/0-Ag14 myeloma cells. Immunoblotting revealed that 15 monoclonal antibodies reacted with the lipopolysaccharide-like (LPS-L) antigen and 14 reacted with the epitopes of a 120-kDa protein. Only typhus group rickettsiae reacted with the monoclonal antibodies against LPS-L. R. felis, a recently identified rickettsial species, did not react with these monoclonal antibodies, confirming that it is not antigenically related to the typhus group. Monoclonal antibodies against the 120-kDa protein were highly specific for R. prowazekii. We successfully applied a selected monoclonal antibody against the 120-kDa protein to detect by immunofluorescence assay R. prowazekii in smears from 56 wild and laboratory lice, as well as in 10 samples of louse feces infected or not infected with the organism. We have developed a simple, practical, and specific diagnostic assay for clinical specimens and large-scale epidemiological surveys with a sensitivity of 91%. These monoclonal antibodies could be added to the rickettsial diagnostic panel and be used to differentiate R. prowazekii from other rickettsial species.
Rickettsia prowazekii is the causative agent of epidemic typhus, a severe reemerging disease (31, 32). It is transmitted to humans by the body louse, Pediculus hominis corporis (23), and has the most serious epidemic potential among all rickettsiae. Epidemic typhus frequently occurs in areas where poverty, lack of hygiene, and cold weather favor the proliferation of lice. Its prevalence reflects the socioeconomic level of a society (43). Sporadic cases of epidemic typhus have reemerged in areas of North Africa (22), North America (20), and western South America (28); and outbreak cases have been reported in Russia (37) and Burundi (31), where the biggest outbreak since World War II was observed in 1997.
R. prowazekii and R. typhi, the agent of murine typhus, which is transmitted by fleas, are grouped together on the basis of comparisons of phylogenetic references, antigenic components, and other pathogenic characteristics (24, 32). Epidemic and endemic typhus can be observed as sporadic cases; therefore, it is critical to differentiate between these two types of typhus since their epidemic potentials differ greatly. Compared with the high rate of mortality from typhus, which can reach 10 to 30% for epidemic typhus, murine typhus usually runs a mild course. Moreover, a sporadic case of epidemic typhus could elicit an outbreak in a louse-infested population (34). Although molecular biological tests have been applied to detect R. prowazekii in lice and blood (4, 33), so far the diagnosis of typhus is essentially based on serological assays, which include immunofluorescence analysis (18, 24-26), the Weil-Felix test (7), the latex agglutination assay (10), dot blot assay (13), the slide immunoperoxidase assay (14), and Western blotting (18). Due to intensive serological cross-reactions between these two typhus species (1, 11), their differentiation is difficult by serology. Recently, Western blotting and/or cross-adsorption studies have been shown to be definitive techniques (18); however, the high costs of such studies limit their use.
In an effort to circumvent the problem of diagnosis of epidemic typhus economically, we produced species-specific monoclonal antibodies (MAbs) against R. prowazekii to detect this pathogen from infected body lice by immunofluorescence assay. Although MAbs against R. prowazekii have been described in previous studies (2, 5, 6, 38), to the best of our knowledge, these MAbs have not been used in practice and their use in a diagnostic assay has never been tested.
MATERIALS AND METHODS
Preparation of antigens.
The Breinl strain of R. prowazekii and 27 other reference rickettsial strains (listed in Table 1) were cultivated in confluent monolayers of L929 cells (ATCC CCL 1 NCTC clone 929), as described previously (40-42). R. felis was grown in XTC2 cells (9, 29). When the cells were heavily infected and estimated to be at a concentration of 104 PFU/ml, as determined by Gimenez staining (35), they were harvested and stored at −70°C. These unpurified antigens were used in the indirect immunofluorescence assay to screen MAbs. For immunization, they were sonicated, centrifuged at 100 × g (CR4, 12 refrigerated Bank-Top centrifuge; Jouan, Winchester, Va.) for 10 min, and concentrated 20 times to an estimated density of 2 × 105 PFU/ml. For sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE), the antigens of R. prowazekii, R. typhi, or R. felis were purified by centrifugation in Renografin density gradients as described previously (39). The final pellets were suspended in distilled water, adjusted to a concentration of 1 mg/ml (19), and stored at −80°C.
TABLE 1.
Rickettsial strains studied
| Rickettsia | Groupa | Strain | Source | Geographic origin | Pathogenicity | Standard strain no.b |
|---|---|---|---|---|---|---|
| Rickettsia rickettsii | SFG | Sheila Smith | Human | Montana | Rocky Mountain SE:c | ATCC VR149 |
| Rickettsia sibirica | SFG | 246 | Dermacentor nuttalii | Former USSR | North Asian tick typhus | ATCC VR151 |
| Rickettsia conorii | SFG | 7(Malish) | Human | South Africa | Mediterranean SF | ATCC VR613 |
| Rickettsia conorii | SFG | Moroccan | Unknown | Morocco | Mediterranean SF | ATCC VR141 |
| Rickettsia australis | SFG | Philips | Human | Australia | Queensland tick typhus | |
| Rickettsia akari | SFG | MK (Kaplan) | Human | New York | Rickettsialpox | ATCC VR 148 |
| Rickettsia montanensis | SFG | Tick strain | Dermacentor andersoni | Montana | ATCC VR611 | |
| Rickettsia rhipicephali | SFG | 3-7-6 | Rhipicephalus sanguineus | Mississippi | ||
| Rickettsia parkeri | SFG | Maculatum 20 | Amblyomma maculatum | Mississippi | ||
| Rickettsia africae | SFG | Z9-Hu | Human | Zimbabwe | African tick bite fever | |
| Rickettsia helvetica | SFG | C9P9 | Ixodes ricinus | Switzerland | ? | ATCC VR1375 |
| Rickettsia massiliae | SFG | Mtu1 | Rhipicephalus turanicus | France | ATCC VR 1376 | |
| Rickettsia mongolotimonae | SFG | HA-91 | Hyalomma asiaticum kozlovi | China | SF | |
| Astrakhan fever rickettsia | SFG | Human isolate | Human | Russia | Astrakhan fever | |
| Bar 29 | SFG | Bar 29 | Rhipicephalus sanguineus | Spain | ||
| Rickettsia conorii Israel | SFG | ISTT CDC1 | Human | Israel | Israeli SF | |
| Rickettsia slovaca | SFG | 13-B | Dermacentor marginatus | Slovakia | Tick-borne lymphadenopathy | |
| Thai tick typhus rickettsia | SFG | TT-118 | Ixodes and Rhipicephalus spp. | Spain | ||
| Rickettsia honei | SFG | RB | Human | Australia | Flinders Island SF | |
| Rickettsia conorii Indian | SFG | Rhipicephalus sanguineus | India | |||
| SFG | 369L42-1 | Dermacentor andersonii | Ohio | |||
| Rickettsia felis | SFG | Marseille | Ctenocephalides felis | United States | Flea borne SF | |
| Rickettsia japonica | SFG | YH | Human | Japan | Japanese SF | ATCC VR1363 |
| Rickettsia aeschlimannii | SFG | MC16 | Hyalomma marginatum | Morocoo | ||
| Strain S | SFG | S | Rhipicephalus sanguineus | Former USSR | ||
| Rickettsia typhi | TG | Wilmington | Human | North Carolina | Murine typhus | ATCC VR 144 |
| Rickettsia canadensis | TG | 2678 | Haema physalis leporispalustris | Canada | ATCC VR610 | |
| Rickettsia prowazekii | TG | Breinl | Human | Poland | Epidemic typhus | ATCC VR142 |
SFG, spotted fever group; TG, typhus group.
ATCC, American Type Culture Collection.
SF, spotted fever.
Six bacterial human isolates from different phyla (Pseudomonas aeruginosa, Haemophilus influenzae, Streptococcus pneumoniae, Escherichia coli, Klebsiella oxytoca, Staphylococcus aureus) and three other louse-associated bacteria (Bartonella quintana, Borrelia recurrentis, Acinetobacter baumannii) (17) were used to determine the specificities of the MAbs.
Production of MAbs.
Six-week-old female BALB/c mice were inoculated intraperitoneally with 106 R. prowazekii organisms in 4% formalin (Sigma Chemical Co., St. Louis, Mo). After three injections at 7-day intervals, the mice were given two boosters 7 and 14 days later by intravenous injection of 4 × 103 organisms in 0.1 ml of phosphate-buffered saline (PBS) into the tail vein. The splenocytes from antibody-positive mice were fused with SP2/0-Ag14 myeloma cells by using 50% (wt/vol) polyethylene glycol (molecular weight, 1,300 to 1,600; Sigma Chemical Co.) by the procedure described by Xu et al. (40). The fused cells were then grown in hybridoma selective medium (Gibco BRL, Paisley, Scotland) containing 20% fetal bovine serum (Gibco BRL) and hypoxanthine-aminopterin-thymidine selective medium (Gibco BRL) for 2 weeks and successively in hypoxanthine-thymidine medium (Sigma Chemical Co.) for 5 days. The supernatants from viable hybridoma clones were screened for antibodies against R. prowazekii by immunofluorescence assay. Positive hybridoma cells were spread and subcloned two to three times by limiting dilution. The immunoglobulin classes and subclasses of the MAbs were determined with an ImmunoType mouse MAb isotyping kit (Sigma Chemical Co.).
Immunofluorescence assay.
An indirect immunofluorescence assay was used to screen hybridoma clones and determine the specificities of the MAbs. Unpurified antigens of R. prowazekii and other reference bacteria (Table 1) were deposited on slides with a pen nib. The slides were air dried and then fixed in acetone for 20 min at room temperature. The assay was modified from a previously described procedure (42). Briefly, the wells were overlaid with 30 μl of supernatants from hybridoma clones, and then the plates were incubated in a moist chamber at 37°C for 30 min before they were washed three times in PBS for 3 min each time. After the slides were dried, bound antibody was detected with dichlorotriazinyl amino fluorescein-conjugated goat anti-mouse immunoglobulin G (IgG) plus IgM (Jackson ImmunoResearch Laboratories, Inc., West Grove, Pa.) diluted 1:200 in PBS containing 3% nonfat dry milk and 0.2% Evans blue (BioMerieux, Marcy 1′Etoile, France). The slides were washed as described above and mounted with Fluoprep (BioMerieux) and were then examined under a Zeiss epifluorescence microscope at ×400 magnification. Sera of immunized and healthy mice were used as positive and negative serum controls, respectively, in each assay.
SDS-PAGE and Western immunoblotting.
The whole antigen of R. prowazekii was dissolved in Laemmli buffer (16) (0.625 M Tris [pH 8.0], 2% [wt/vol] SDS, 5% [vol/vol] 2-mercaptoethanol, 10% [vol/vol] glycerol, 0.002% [wt/vol] bromophenol blue) for 2 h at room temperature and used as native antigen or was boiled for 10 min and used as heated antigen, or the proteins were digested with proteinase K (2 mg/ml) at 37°C for 1 h.
The antigens of R. typhi and R. felis were only used as native antigen. Electrophoresis was performed at 16 mA for 2 h on a 10% polyacrylamide separating gel with 5% polyacrylamide stacking gel in a Mini Protein II cell apparatus (Bio-Rad, Richmond, Calif.). A mixture of high-range molecular mass standards (Bio-Rad) was used as a marker to estimate the molecular weight of the separated antigen.
The resolved polypeptides were transferred onto a nitrocellulose membrane (pore size, 0.45 μm; Trans-Blot Transfer Medium; Bio-Rad) by electrophoresis at 100 V for 1 h in an electrophoretic transfer cell (Mini Trans-Blot; Bio-Rad) with transfer buffer (2.5 mM Tris base, 192 mM glycine, 20% methanol). Then the nitrocellulose sheet was blocked at 4°C overnight with Tampon Saturation buffer (0.121% [wt/vol] Tris base, 150 mM NaCl, 0.05% [vol/vol] Tween 20) containing 5% nonfat powdered milk. After three 10-min washes in Tampon Saturation buffer, the membrane was cut into strips. The supernatants of different hybridoma clones were diluted 1:6 in Tampon Saturation buffer with 0.5% nonfat dry milk and were then applied to the strips, and the strips were incubated at 4°C overnight on a rocker. The strips were washed as described above and were then incubated for 2 h at room temperature with peroxidase-conjugated F(ab′)2 fragment goat anti-mouse IgG (heavy and light chains; AffiniPure; Jackson ImmunoResearch) diluted 1:400 in Tampon Saturation buffer containing 3% nonfat dry milk. After three washes with Tampon Saturation buffer, the bound conjugate was detected by incubation with a solution which contained 0.015% 4-chloro-1-naphthol (Sigma Chemical Co.) in 16.7% methanol in Tampon Saturation buffer containing 0.015% hydrogen peroxide. The sera of the immunized and naive mice were collected, diluted 1:100, and used as the positive and negative controls, respectively, in each test.
Detection of R. prowazekii.
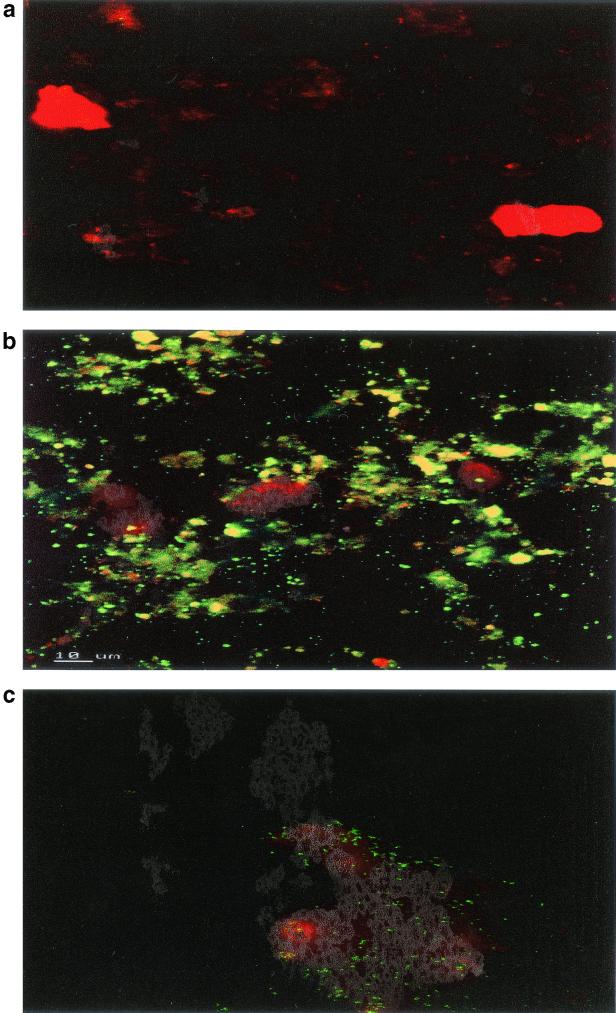
For clinical use we selected an MAb specific for R. prowazekii (MAb P11A12). Twenty-two lice from Rwanda and Burundi sampled during typhus outbreaks were tested by PCR as reported previously (15). We also used 17 lice experimentally infected with R. prowazekii and 17 noninfected lice. These lice were also tested by PCR, as reported previously (36). The gut lumens of the lice were dissected as reported previously (8), and their intestines were crushed and smeared on 18-well microscope slides under an enlarge-scope (Stermi 2000; Zeiss) at ×2.5 magnification. We also tested feces from two lice infected in the laboratory and eight noninfected lice. Feces were directly smeared onto the slides. The immunofluorescence test was performed by using a blind method. After fixation in methanol for 15 min at room temperature, the rickettsiae were detected by immmunofluorescence assay by using supernatants of MAb P11A12 (an R. prowazekii-specific MAb) diluted (1/100 and 1/1,000) with distilled water. Following performance of the immunofluorescence assay as described above, the intracellular position of visible R. prowazekii in lice was determined with a laser scanning confocal microscope as described previously to determine infection (30).
RESULTS
Production of MAbs.
Initially, we obtained 254 viable hybridoma clones 14 to 18 days after the fusion. Through screening by immunofluorescence assay, 187 clones were found to secrete antibodies against R. prowazekii, and 40 were selected for subcloning by limiting dilution two to three times. Finally, 29 MAbs were selected.
SDS-PAGE and Western blotting.
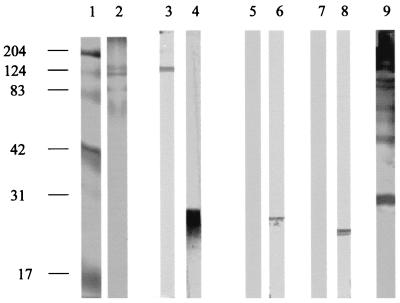
By SDS-PAGE with Coomassie brilliant blue staining of the polyacrylamide gels, the native protein profiles of R. prowazekii showed three major groups of polypeptide bands: bands at 120 and 60 kDa and low-molecular-mass bands at about 17 to 40 kDa, as reported previously (Fig. 1) (7). By Western immunoblotting the polyclonal antiserum of mice against R. prowazekii showed several major reactive bands that comigrated to positions that corresponded to the major polypeptides bands seen by SDS-PAGE. Of the 29 hybridoma clones that produced MAbs, 14 recognized a 120-kDa protein. They belonged to the IgG2b and IgG3 subclasses. This reactivity was completely destroyed after antigen treatment by heating and proteinase K digestion (Fig. 1). Fifteen other MAbs directed against a lipopolysaccharide (LPS)-like (LPS-L) antigen (7) produced multiple bands (17 to 40 kDa), and the antigen resisted destruction by heating and proteinase K digestion (Fig. 1). The MAbs belonged to the IgG3 and IgG1 subclasses.
FIG. 1.
Western blotting profiles of MAbs against R. prowazekii. Lane 1, molecular size markers (numbers on the left are in kilodaltons); lane 2, Coomassie brilliant blue-stained, native R. prowazekii antigen (SDS-PAGE); lanes 3, 5, and 7, MAb P11A12; lanes 4, 6, and 8, MAb P9G1; lane 9, polyclonal antisera against native antigen (lanes 3, 4, and 9), heated antigen (lanes 5 and 6), and proteinase K-digested antigen (lanes 7 and 8).
Specificities of MAbs.
Twenty-nine MAbs against R. prowazekii were tested with 27 other strains of rickettsiae. Among the 14 MAbs against the 120-kDa protein, 8 reacted only with R. prowazekii and 6 had weak cross-reactivity with R. typhi and/or R. canadensis. Fifteen MAbs against the LPS-L antigen strongly reacted with R. typhi and R. canadensis but not with R. felis and were classified as group specific. No MAb was found to have cross-reactivity with any strain of the spotted fever group rickettsiae or the other nine nonrickettsial bacteria including the three louse-associated bacteria.
We selected MAb P11A12, an anti-120-kDa protein MAb that reacts only with R. prowazekii, to test the lice. PCR analysis indicated that 4 of 22 wild lice were infected, as were all lice infected in the laboratory (16). Among the 21 infected (naturally or experimentally) lice, the MAb detected infection in 19 lice by detection of several foci of fluorescent bacteria (Fig. 2). The feces from the two infected lice were found to be positive. Both dilutions of the MAb (1/100 and 1/1,000) gave the same results. The sensitivity of this assay was estimated to be 91%. A weak positive reaction was found with three other lice, including one louse that was PCR positive. None of the noninfected feces were positive. The negative predictive value of our test was 100%.
FIG. 2.
Fluorescent antibody-stained isolate of R. prowazekii. (a) Feces from an uninfected louse; (b) feces of an experimentally infected louse; (c) cell smear prepared from intestines of an experimentally infected louse.
DISCUSSION
In the present work we first applied species-specific MAbs against R. prowazekii to detect this pathogen in infected lice by immunofluorescence assay. MAbs against R. prowazekii have been described in previous studies that have investigated common cross-reactivity with R. typhi (2) and that have studied the surface antigen (21). MAbs against the LPS of typhus group rickettsiae have also been used to establish a timely diagnosis of typhus group rickettsiosis by immunohistochemical examination (38). An investigation of the antigenic specificities of MAbs against R. prowazekii in a large panel of rickettsial species including R. felis has never been reported. In the present study, more than 90 MAbs were produced. Through two to three limiting dilutions, expansions, and determinations, 29 representative MAbs were finally selected. They were shown to be reactive with the epitopes on an LPS-L antigen that may be LPS and a high-molecular-mass protein of 120 kDa that may be rOmpB, an outer membrane protein. Both were found to be predominant immunogens of R. prowazekii by immunoblotting with mouse polyclonal antiserum (Fig. 1).
Further analysis of cross-reactivity with 27 different rickettsial species showed that MAbs against LPS-L of R. prowazekii reacted by immunofluorescence assay with each member of the typhus group rickettsiae, R. typhi and R. canadensis, but not with members of the spotted fever group rickettsiae. It indicated that this antigen, shared by every member of the typhus group rickettsiae, was group specific and may be the LPS. R. felis (29, 32), the agent of flea-borne spotted fever, was first observed in cat fleas (Ctenocephalides felis) by electron microscopy and was originally included in the typhus group rickettsiae (3, 12, 27). More recently, a wealth of genetic studies have discriminated R. felis from the typhus group and have placed it into the spotted fever group (29). The MAbs against LPS-L obtained in the present work did not react with R. felis, confirming this classification.
By Western blotting, 14 MAbs directed against the 120-kDa protein, which may be on the predominant immunogenic surface protein antigen, rOmpB, were considered species-specific MAbs, none of which was found to recognize the heat-denatured form of this antigen. These MAbs were found not to react with other rickettsial species; however, six of the MAbs showed weak cross-reactivity with R. typhi.
Finally, one species-specific MAb against R. prowazekii, directed against the 120-kDa protein, detected the organism in samples of both naturally and experimentally infected lice or their feces by immunofluorescence assay. Other louse-associated bacteria were not detected by these antibodies, which further demonstrated their specificities. This report describes a specific, convenient, and reliable diagnostic assay with a sensitivity of 91%. It especially appears to be of practical value when it is required to identify R. prowazekii in lice in a given area, when typhus cases are suspected, or for epidemiological surveys of lice.
Acknowledgments
We thank Armand Tasmadjian for technical assistance, P. E. Fournier for photographing the Western blotting result, J. M. Rolain for assistance in taking the picture of infected lice, J. Bosco Ndihokubwayo for the naturally infected lice, and Donald Bouyer for correction of the English.
REFERENCES
- 1.Amano, K. I., J. C. Williams, and G. A. Dasch. 1998. Structural properties of lipopolysaccharides from Rickettsia typhi and Rickettsia prowazekii and their chemical similarity to the lipopolysaccharide from Proteus vulgaris OX19 used in the Weil-Felix test. Infect. Immun. 66:923-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black, C. M., T. Tzianabos, L. F. Roumillat, M. A. Redus, J. E. McDade, and C. B. Reimer. 1983. Detection and characterization of mouse monoclonal antibodies to epidemic typhus rickettsiae. J. Clin. Microbiol. 18:561-568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bouyer, D. H., J. Stenos, P. Crocquet-Valdes, C. Moron, P. Vsevolod, J. E. Zavala-Velasquez, L. Foil, D. Stothard, A. Azad, and D. Walker. 2001. Rickettsia felis: molecular characterization of a new member of the spotted fever group. Int. J. Syst. E vol. Microbiol. 51:339-347. [DOI] [PubMed] [Google Scholar]
- 4.Carl, M., C. W. Tibbs, M. E. Dobson, S. Paparello, and G. A. Dasch. 1990. Diagnosis of acute typhus infection using the polymerase chain reaction. J. Infect. Dis. 161:791-793. [DOI] [PubMed] [Google Scholar]
- 5.Drobyshevskaia, E. I., I. A. Nedialkov, S. V. Spitsyn, V. Makarova, I. Tarasevich, and V. Nesterenko. 1989. Characteristics of monoclonal antibodies directed to species specific and group specific antigens of Rickettsia prowazekii. Tr. Inst. Im. Pastera 66:160-165. [PubMed] [Google Scholar]
- 6.Drobyshevskaia, E. I., S. V. Spitsyn, I. U. Nedialkov, I. U. Shchekotikhina, and I. V. Tarasevich. 1989. Monoclonal autoantibodies to the epithelial basement membrane cells of human skin and thymus obtained through immunization with Rickettsia prowazekii antigens. Zh. Mikrobiol. Epidemiol. Immunobiol. 5:73-77. (In Russian.) [PubMed] [Google Scholar]
- 7.Eremeeva, M. E., N. M. Balayeva, and D. Raoult. 1994. Serological response of patients suffering from primary and recrudescent typhus: comparison of complement fixation reaction, Weil-Felix test, microimmunofluorescence, and immunoblotting. Clin. Diagn. Lab. Immunol. 1:318-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fournier, P. E., M. F. Minnick, H. Lepidi, E. Salvo, and D. Raoult. 2001. Experimental model of human body louse infection using green fluorescent protein-expressing Bartonella quintana. Infect. Immun. 69:1876-1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gimenez, D. F. 1964. Staining rickettsiae in yolk-sac cultures. Stain Technol. 39:135-140. [DOI] [PubMed] [Google Scholar]
- 10.Hechemy, K. E., J. V. Osterman, C. S. Eisemann, L. B. Elliott, and S. J. Sasowski. 1981. Detection of typhus antibodies by latex agglutination. J. Clin. Microbiol. 13:214-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hechemy, K. E., D. Raoult, J. Fox, Y. Han, L. B. Elliott, and J. Rawlings. 1989. Cross-reaction of immune sera from patients with rickettsial diseases. J. Med. Microbiol. 29:199-202. [DOI] [PubMed] [Google Scholar]
- 12.Higgins, J. A., S. Radulovic, M. E. Schriefer, and A. F. Azad. 1996. Rickettsia felis: a new species of pathogenic rickettsia isolated from cat fleas. J. Clin. Microbiol. 34:671-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly, D. J., C. T. Chan, H. Paxton, K. Thompson, R. Howard, and G. A. Dasch. 1995. Comparative evaluation of a commercial enzyme immunoassay for the detection of human antibody to Rickettsia typhi. Clin. Diagn. Lab. Immunol. 2:356-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly, D. J., P. W. Wong, E. Gan, and G. E. Lewis, Jr. 1988. Comparative evaluation of the indirect immunoperoxidase test for the serodiagnosis of rickettsial disease. Am. J. Trop. Med. Hyg. 38:400-406. [DOI] [PubMed] [Google Scholar]
- 15.Knobloch, J. 1988. Analysis and preparation of Bartonella bacilliformis antigens. Am. J. Trop. Med. Hyg. 39:173-178. [DOI] [PubMed] [Google Scholar]
- 16.Laemmli, U. K. 1970. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature 227:680-685. [DOI] [PubMed] [Google Scholar]
- 17.La Scola, B., P. E. Fournier, P. Brouqui, and D. Raoult. 2001. Detection and culture of Bartonella quintana, Serratia marcescens, and Acinetobacter spp. from decontaminated human body lice. J. Clin. Microbiol. 39:1707-1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.La Scola, B., L. Rydkina, J. B. Ndihokubwayo, S. Vene, and D. Raoult. 2000. Serological differentiation of murine typhus and epidemic typhus using cross-adsorption and Western blotting. Clin. Diagn. Lab. Immunol. 7:612-616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lowry, O. H., N. J. Rosebrough, A. L. Farr, and R. J. Randall. 1951. Protein measurement with the Folin phenol reagent. J. Biol. Chem. 193:265-275. [PubMed] [Google Scholar]
- 20.Massung, R. F., L. Davis, K. Slater, D. McKechnie, and M. Puerzer. 2001. Epidemic typhus meningitis in the southwestern United States. Clin. Infect. Dis. 32:979-982. [DOI] [PubMed] [Google Scholar]
- 21.Nedialkov, I. A., S. V. Spitsyn, E. I. Drobyshevskaia, V. V. Gosteva, N. V. Klitsunova, N. S. Smirnova, I. V. Tarasevich, and V. G. Nesterenko. 1990. The surface antigens of Rickettsia prowazekii studied with monoclonal antibodies. Zh. Mikrobiol. Epidemiol. Immunobiol. 5:94-97. [PubMed] [Google Scholar]
- 22.Niang, M., P. Brouqui, and D. Raoult. 1999. Epidemic typhus imported from Algeria. Emerg. Infect. Dis. 5:716-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nicolle, C. 1934. Destin des maladies infectieuses, p. 1-215. France Lafayette, Paris, France. (In French.)
- 24.Ormsbee, R., M. Peacock, R. Philip, E. Casper, J. Plorde, T. Gabre-Kidan, and L. Wright. 1977. Serologic diagnosis of epidemic typhus fever. Am. J. Epidemiol. 105:261-271. [DOI] [PubMed] [Google Scholar]
- 25.Philip, R. N., E. A. Casper, W. Burgdorfer, R. K. Gerloff, L. E. Hugues, and E. J. Bell. 1978. Serologic typing of rickettsiae of the spotted fever group by microimmunofluorescence. J. Immunol. 121:1961-1968. [PubMed] [Google Scholar]
- 26.Philip, R. N., E. A. Casper, R. A. Ormsbee, M. G. Peacock, and W. Burgdorfer. 1976. Microimmunofluorescence test for the serological study of Rocky Mountain spotted fever and typhus. J. Clin. Microbiol. 3:51-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radulovic, S., J. A. Higgins, D. C. Jaworski, G. A. Dasch, and A. F. Azad. 1995. Isolation, cultivation, and partial characterization of the ELB agent associated with cat fleas. Infect. Immun. 63:4826-4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raoult, D., R. J. Birtles, M. Montoya, E. Perez, H. Tissot-Dupont, and H. Guerra. 1999. Survey of louse-associated diseases among rural Andean communities in Peru: prevalence of epidemic typhus, trench fever, and relapsing fever. Clin. Infect. Dis. 29:434-436. [DOI] [PubMed] [Google Scholar]
- 29.Raoult, D., B. La Scola, M. Enea, P. E. Fournier, V. Roux, F. Fenollar, M. A. M. Galvao, and X. De Lamballerie. 2001. A flea associated Rickettsia pathogenic for humans. Emerg. Infect. Dis. 7:73-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raoult, D., P. Lecocq, H. Lepidi, B. La Scola, and P. E. Fournier. 2001. Culture and immunological detection of Tropheryma whipplei from the duodenum of a patient with Whipple's disease. JAMA 285:1039-1043. [DOI] [PubMed] [Google Scholar]
- 31.Raoult, D., J. B. Ndihokubwayo, H. Tissot-Dupont, V. Roux, B. Faugere, R. Abegbinni, and R. J. Birtles. 1998. Outbreak of epidemic typhus associated with trench fever in Burundi. Lancet 352:353-358. [DOI] [PubMed] [Google Scholar]
- 32.Raoult, D., and V. Roux. 1997. Rickettsioses as paradigms of new or emerging infectious diseases. Clin. Microbiol. Rev. 10:694-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Raoult, D., and V. Roux. 1999. The body louse as a vector of reemerging human diseases. Clin. Infect. Dis. 29:888-911. [DOI] [PubMed] [Google Scholar]
- 34.Raoult, D., V. Roux, J. B. Ndihokubwaho, G. Bise, D. Baudon, G. Martet, and R. J. Birtles. 1997. Jail fever (epidemic typhus) outbreak in Burundi. Emerg. Infect. Dis. 3:357-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rolain, J. M., M. Maurin, G. Vestris, and D. Raoult. 1998. In vitro susceptibilities of 27 rickettsiae to 13 antimicrobials. Antimicrob. Agents Chemother. 42:1537-1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roux, V. 1999. Phylogenetic analysis and taxonomic relationships among the genus Rickettsia, p. 52-66. In D. Raoult and P. Brouqui (ed.), Rickettsiae and rickettsial diseases at the turn of the third millennium. Elsevier, Marseille, France.
- 37.Tarasevich, I., E. Rydkina, and D. Raoult. 1998. Epidemic typhus in Russia. Lancet 352:1151. [DOI] [PubMed] [Google Scholar]
- 38.Walker, D. H., H.-M. Feng, S. Ladner, A. N. Billings, S. R. Zaki, D. J. Wear, and B. Hightower. 1997. Immunohistochemical diagnosis of typhus rickettsioses using an anti-lipopolysaccharide monoclonal antibody. Mod. Pathol. 10:1038-1042. [PubMed] [Google Scholar]
- 39.Weiss, E., J. C. Coolbaugh, and J. C. Williams. 1975. Separation of viable Rickettsia typhi from yolk sac and L cell host components by Renografin density gradient centrifugation. Appl. Microbiol. 30:456-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Xu, W., L. Beati, and D. Raoult. 1997. Characterization of and application of monoclonal antibodies against Rickettsia africae, a newly recognized species of spotted fever group rickettsia. J. Clin. Microbiol. 35:64-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu, W., and D. Raoult. 1997. Distribution of immunogenic epitopes on the two major immunodominant proteins (rOmpA and rOmpB) of Rickettsia conorii among the other rickettsiae of the spotted fever group. Clin. Diagn. Lab. Immunol. 4:753-763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu, W., and D. Raoult. 1997. Production of monoclonal antibodies against Rickettsia massiliae and their use in antigenic and epidemiological studies. J. Clin. Microbiol. 35:1715-1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zinsser, H. 1935. Rats, lice, and history, p. 1-301. Broadway House, London, United Kingdom.