Abstract
The core protein of hepatitis C virus (HCV) has been implicated in hepatocarcinogenesis. In order to determine whether there is a correlation between mutations of the core protein and the development of hepatocellular carcinoma (HCC), the core protein-coding sequence of the viral genome of HCV subtype 1b (HCV-1b) obtained from patients with and without HCC was analyzed. We found that 12 (40.0%) of 30 HCV-1b isolates from patients with HCC but none of 29 isolates from patients without HCC had a point mutation(s) in an N-terminal region of 20 residues. Similarly, 10 (33.3%) of 30 isolates from patients with HCC had mutations in a limited region between residues 141 and 160, whereas only 2 (6.9%) of 29 isolates from patients without HCC did. The differences between the two groups were statistically significant. The mutations were found in isolates from both cancerous and adjacent noncancerous tissues of patients with HCC, suggesting that the mutations were present before the development of HCC. The other regions of the core protein of some isolates also had mutations, but no significant difference was observed between isolates from patients with HCC and those from patients without HCC. The F protein, a frameshift product that is still hypothetical for HCV-1b strains, showed more sequence diversity than the core protein among the isolates analyzed, but there were no significant differences in the mutation rates or positions between isolates from patients with HCC and isolates from patients without HCC, except for a short N-terminal sequence of ∼11 residues that is shared with the core protein.
Hepatitis C virus (HCV) is a major etiologic agent of chronic hepatitis worldwide, with the estimated number of infected individuals being more than 170 million. It is estimated that 15 to 20% of chronically infected individuals undergo liver cirrhosis in a decade or so after infection, with hepatocellular carcinoma (HCC) arising from cirrhosis at an estimated rate of 1 to 4% per year (14). Although the precise mechanism is yet to be clarified at the molecular level, the HCV core protein is implicated in the hepatocarcinogenesis. For example, it was reported that the HCV core protein rendered cells more resistant to apoptosis (16, 21) and promoted ras oncogene-mediated transformation of cultured rodent cells (4, 22, 31). Moreover, transgenic mice expressing the HCV core protein in the liver developed HCC (18).
The HCV genome exhibits a considerable degree of sequence variation, and on the basis of these variations, HCV is classified into at least six genotypes and more than 60 subtypes (5, 17, 24). HCV subtype 1b (HCV-1b) is the most prevalent subtype in most parts of Asia including Japan (5, 8, 12) and is likely more frequently associated than the other HCV subtypes with poor responsiveness to interferon treatment, rapid disease progression, and development of HCC (3, 20, 29). In addition to the differences at the genotype and subtype levels, other important sequence diversities have been postulated even among isolates of a given subtype, such as mutations in the interferon sensitivity-determining region of nonstructural protein 5A of HCV-1b, HCV-1c, and HCV-2a (6, 15, 19, 30).
Recently, two research groups independently reported on HCC-associated mutations of the core protein, suggesting a possible role for the mutations in the development of HCC (10, 11, 25, 26, 28). There are, however, some discrepancies between their observations; one group identified point mutations in a hydrophilic region between amino acids (aa) 39 and 76 (28), while the other group found deletion mutations near the N terminus of the core protein that caused a frame shift, giving rise to forms truncated at the C terminus (26). On the other hand, another research group found no significant difference in the N-terminal 80 residues of the core protein between HCV isolates from patients with HCC and HCV isolates from patients without HCC (7). Aside from the HCC-associated mutations in the core protein, Xu et al. (32) recently identified a novel HCV protein, the F protein, that was synthesized from the initiation codon of the core protein followed by a ribosomal frame shift into the +2/−1 reading frame at or near codon 11. Whether or not a particular mutation(s) of the F protein is associated with HCC is another interesting subject to study. In order to clarify the issues outlined above, in the present study we analyzed the core and F proteins of HCV isolates obtained from patients with and without HCC. We report here that about half of the HCV isolates from patients with HCC exhibited point mutations in an N-terminal portion of the core protein, especially a limited region between aa 1 and 20 and another region between aa 141 and 160, both of which were highly conserved among HCV isolates from patients without HCC. Such mutations were found in isolates from both cancerous and surrounding noncancerous tissues of the HCC patients. We also report that although a considerably high degree of sequence variation was observed in the hypothetical F protein, except for a short N-terminal sequence of ∼11 residues that is shared with the core protein, no significant correlation was observed between the mutations and the development of HCC.
MATERIALS AND METHODS
Serum and tissue samples.
Sera were collected from anti-HCV antibody-positive, HBsAg-negative Japanese patients with and without HCC. The sera were tested for anti-HCV antibodies and HBsAg with commercial kits (Ortho HCV Ab ELISA Test III [Ortho Diagnostics, Tokyo, Japan] and AUSAB EIA [Abbott Diagnostics], respectively). The diagnosis of HCC was made on the basis of both clinical and histopathological criteria. A total of 59 serum samples were further analyzed. Thirty serum samples were from patients with HCC (26 men and 4 women; mean age, 63.7 ± 6.4 years; age range, 52 to 76 years), and the remaining 29 serum samples were from age-matched, HCV-infected patients without HCC (18 men and 11 women; mean age, 59.6 ± 10.3 years; age range, 45 to 72 years).
Liver tissues were obtained by surgical resection from 12 patients with HCC who were positive for HCV-1b RNA and negative for HBsAg (11 men and 1 woman; mean age, 65.4 years). After being resected, cancerous and surrounding noncancerous tissues were separated macroscopically, immediately frozen in liquid nitrogen, and stored at −80°C until ready for analysis. The sizes of the tumors ranged from 1.2 to 11.5 cm in diameter, with the average being 4.2 cm.
Sequence analysis of HCV core and F proteins.
RNA was extracted from 50 μl of serum and 30 mg of tissue with an RNeasy Mini kit (Qiagen). To amplify the entire core protein-coding region of the HCV genome, reverse transcription (RT) and the first-round PCR were successively performed in a tube by the Superscript One-Step RT-PCR with Platinum Taq (Gibco BRL) and a set of primers, primers Core-1A (5′-GCGAAAGGCCTTGTGGTACTG-3′, sense, positions 259 to 279) and E1-2 (5′-CCGCTGCCTCATACACAAT-3′, antisense, positions 981 to 963). The reaction was carried out initially at 45°C for 30 min for RT and 94°C for 2 min, followed by PCR over 40 cycles, with each cycle consisting of 1 min each at 94, 52, and 72°C. The second-round PCR was performed over 35 cycles, with each cycle consisting of 1 min at 94°C, 1.5 min at 52°C, and 3 min at 72°C. An inner set of primers, primers Core-3 (5′-ACTGCCTGATAGGGTGCTTG-3′, sense, positions 276 to 295) and E1-1 (5′-GAGCAGTCGTTCGTGACATGGTA-3′, antisense, positions 952 to 930), was used for the second-round PCR. Anti-HCV-negative sera or saline served as a negative control in the RT-PCR analysis to monitor the procedure for possible cross-contamination between the samples. Also, other standard precautions were taken to minimize possible cross-contamination. The amplified fragments were purified with a QIAquick PCR purification kit (Qiagen) and directly sequenced, without being subcloned, in both directions with a dRhodamine Terminator Cycle Sequencing Ready Reaction kit and an ABI 377 sequencer (PE Applied Biosystems). The amino acid sequences of the isolates were then deduced and aligned with each other along with a standard sequence for HCV-1b (HCV-J; DDBJ accession number D90208) (13).
HCV subtype analysis.
HCV subtypes were determined as described previously (2, 5, 29). In brief, RNA extracted from the anti-HCV antibody-positive sera was reverse transcribed into cDNA by using Rous-associated virus type 2 reverse transcriptase (Takara Shuzo, Co., Ltd., Kyoto, Japan) and a primer specific for a portion of the NS5B region of the HCV genome (167R). The resultant cDNA was then amplified by nested PCR with Tth DNA polymerase (Toyobo Co., Ltd., Osaka, Japan) and an outer set of primers (primers 166 and 167R) and an appropriate inner set of primers (primers HC-23, HC-24, and HC-26). The nucleotide sequences of the amplified fragments were determined, based on which HCV subtypes of the isolates were assigned.
Statistical analysis.
The data obtained were statistically analyzed by Student's t test and Welch's t test, the Mann-Whitney U test, and the χ2 test for independence with a two-by-two contingency table. A P value of <0.05 was considered significant.
Nucleotide sequence accession numbers.
The nucleotide sequence data reported in this paper appear in the DDBJ/EMBL/GenBank nucleotide sequence databases under accession numbers AB077701 through AB077747.
RESULTS
Analysis of the core protein sequence of HCV-1b isolates obtained from patients with and without HCC.
The entire 573-base sequence coding for the core protein was determined for HCV isolates obtained from patients with and without HCC, and the sequences were compared with each other. For a detailed comparison, the sequence was divided into three portions, nucleotides 330 to 509 (according to the numbering of HCV-J [13]), 510 to 689, and 690 to 902, each encoding aa 1 to 60, 61 to 120, and 121 to 191 of the core protein, respectively. HCV isolates from patients with HCC had significantly more nucleotide mutations in the N-terminal one-third compared with the number of mutations in isolates from patients without HCC (Table 1). It should also be noted that the N-terminal one-third was more conserved than the other two regions of the core protein-coding sequence, regardless of HCC development. No deletion or insertion was found in the core protein-coding regions of the isolates tested.
TABLE 1.
Nucleotide diversity of the core protein-coding sequence of the HCV genome obtained from patients with and without HCC
| Patient | No. of nucleotide mutations at positionsa:
|
No. of amino acid mutations at positionsb:
|
||||
|---|---|---|---|---|---|---|
| 330 to 509 | 510 to 689 | 690 to 902 | 1 to 60 | 61 to 120 | 121 to 191 | |
| Without HCC | 2.1 ± 1.4 | 7.3 ± 2.4 | 9.8 ± 3.4 | 0.1 ± 0.3 | 1.8 ± 1.0 | 0.7 ± 1.1 |
| With HCC | 3.1 ± 2.0c | 7.7 ± 1.9 | 11.0 ± 3.6 | 0.6 ± 1.0d | 2.0 ± 1.3 | 1.4 ± 1.6 |
Nucleotide positions in the HCV genome. The numbering is as described previously (13).
Amino acid positions in the core protein of HCV.
P < 0.05 compared with the results for isolates from patients without HCC (Student's t test).
P < 0.01 compared with the results for isolates from patients without HCC (Student's t test).
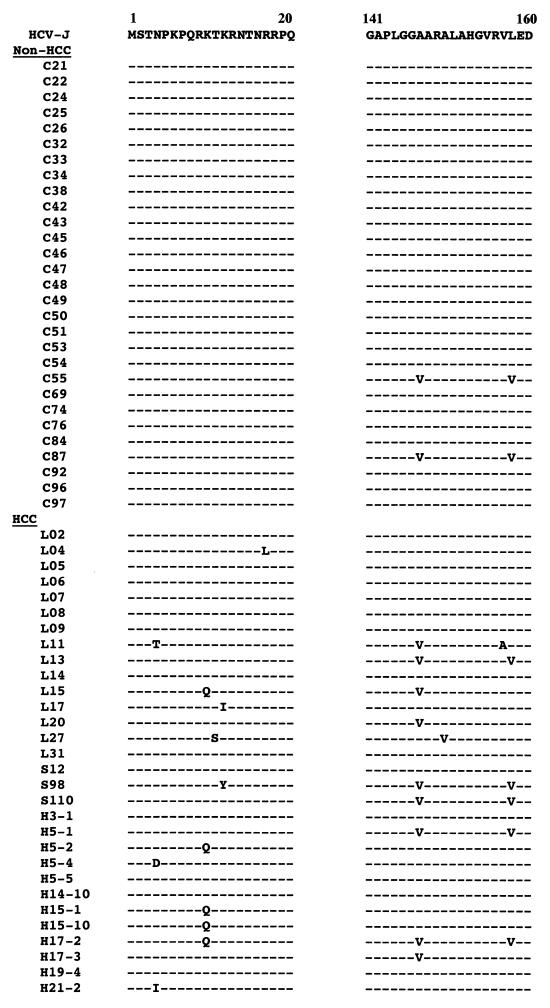
The entire amino acid sequences of the core proteins were likewise compared. HCV isolates from patients with HCC had significantly more amino acid mutations in the N-terminal one-third compared with the number of mutations in the isolates from patients without HCC (Table 1). Further analysis revealed that more than half of the mutations in the N-terminal one-third were localized in a limited region between aa 1 and 20. Whereas the N-terminal 20 residues were completely conserved among isolates from 29 patients without HCC, single point mutations were found in 12 (40.0%) of 30 isolates from patients with HCC (Fig. 1), with the difference between the two groups being statistically significant (P < 0.001). As for the C-terminal one-third, there was no significant difference between isolates from patients with HCC and those from patients without HCC. We found, however, a limited region in the C-terminal one-third (aa 141 to 160) where there were more mutations in isolates from patients with HCC than in those from patients without HCC (Fig. 1). While only 2 (6.9%) of 29 isolates from patients without HCC had a mutation(s), 10 (33.3%) of 30 isolates from patients with HCC had mutations, with the difference being statistically significant (P < 0.05). It should be noted that for the two limited regions combined (aa 1 to 20 and aa 141 to 160), 17 (56.7%) of 30 isolates from patients with HCC had a mutation(s).
FIG. 1.
Sequence alignment of the core proteins of HCV isolates from patients with and without HCC. A reference amino acid sequence (from strain HCV-J [13]; DDBJ accession number D90208) of the regions between aa 1 and 20 and between aa 141 and 160 is shown at the top. Dashes indicate residues identical to those in the reference sequence.
Comparison of the core protein sequences of HCV-1b isolates obtained from cancerous and adjacent noncancerous tissues of patients with HCC.
To see whether the mutations in the core protein were present before the development of HCC or whether they emerged thereafter, isolates from cancerous and adjacent noncancerous tissues of each patient were analyzed. Of 12 pairs of the core protein sequences obtained from cancerous and surrounding noncancerous tissues, each pair of 7 of the pairs had identical amino acid sequences, although there were a number of mutations at the nucleotide level (Table 2). The remaining five pairs showed pairwise differences of one or two residues. Only one pair (from patient L09) showed a pairwise amino acid mutation (A148V) in the limited region between aa 141 and 160. It should also be noted that the degrees of mutations between isolates from cancerous tissues and those from surrounding noncancerous tissues of given patients, both at the nucleotide level and the amino acid level, were smaller than those observed between isolates from different patients (Table 1).
TABLE 2.
Comparison of the core protein sequences between HCV isolates obtained from cancerous and adjacent noncancerous tissues of patients with HCC
| Patient | No. (%) of mutated nucleotides | No. (%) of mutated amino acids | Amino acid mutation |
|---|---|---|---|
| L02 | 5 (0.9) | 0 | |
| L05 | 8 (1.4) | 2 (1.0) | I187T, A189V |
| L06 | 3 (0.5) | 0 | |
| L07 | 1 (0.2) | 1 (0.5) | T110M |
| L08 | 1 (0.2) | 0 | |
| L09 | 3 (0.5) | 1 (0.5) | A148V |
| L11 | 0 | 0 | |
| L13 | 1 (0.2) | 1 (0.5) | K23Q |
| L14 | 9 (1.6) | 2 (1.0) | Q70R, I187M |
| L15 | 2 (0.3) | 0 | |
| L17 | 2 (0.3) | 0 | |
| L20 | 5 (0.9) | 0 | |
| Mean ± SD | 3.3 ± 2.9 (0.6 ± 0.5) | 0.6 ± 0.8 (0.3 ± 0.4) |
Analysis of F-protein sequences of HCV-1b isolates from patients with and without HCC.
It has been reported that the core protein-coding region of the viral genome of HCV-1a strains contains an adenine-rich region where a ribosomal frame shift into the +2/−1 reading frame takes place to generate a novel HCV protein of 162 aa residues, the F protein (32). Although such a frame shift is still a matter of debate for HCV-1b strains, we predicted the amino acid sequences of the hypothetical F proteins of the HCV-1b isolates from patients with and without HCC. Introduction of an additional adenine after the 31st nucleotide (codon 11) resulted in the generation of hypothetical products consisting of 91, 144, and 162 aa residues in 9 (15%), 42 (71%), and 8 isolates (14%), respectively (data not shown). Since the hypothetical protein of 144 residues was most common among the isolates analyzed, including the standard strain, strain HCV-J, we provisionally considered the 144-residue product to be the F protein of the HCV-1b subtype.
The F protein was divided into three regions (aa 1 to 50, 51 to 100, and 101 to 144), and the sequences were compared with that of HCV-J. The F-protein sequence showed higher degrees of sequence diversity than the core protein sequence. When the mutation rates between isolates from patients with HCC and those from patients without HCC were compared, no significant difference was observed in any of the three regions (Table 3).
TABLE 3.
Amino acid diversity of the HCV F protein from patients with and without HCC
| Patient | No. of amino acid mutations at positiona:
|
||
|---|---|---|---|
| 1 to 50 | 51 to 100 | 101 to 144 | |
| Without HCC | 1.4 ± 1.2 | 3.8 ± 1.5 | 4.5 ± 1.3 |
| With HCC | 2.0 ± 1.4 | 3.8 ± 1.4 | 4.7 ± 1.1 |
Amino acid positions in the HCV F protein.
DISCUSSION
The core protein of HCV, which is cleaved from the precursor polyprotein by the signal peptidase of the host cell, forms the nucleocapsid of the virion (23). In HCV-infected cells, the core protein is localized predominantly in the cytoplasm, with a minor fraction with a different higher-order structure being localized in the nucleus (33), exerting versatile functions including inhibition of apoptosis (16, 21) and malignant transformation of the cell (4, 22, 31). Whether some function(s) of the core protein varies with the different sequences of the core protein is an interesting subject to study. Along this line, we have been studying the possible correlation between mutations in the core protein and the development of HCV-associated HCC. In the present study we found two short stretches in the core protein sequence, one between aa 1 and 20 and the other between aa 141 and 160, where a point mutation(s) was found in nearly 60% of the isolates from patients with HCC but was only rarely found in isolates from patients without HCC (Fig. 1). The mutations in these limited regions were found in isolates from both cancerous and adjacent noncancerous tissues of given HCC patients (Table 2). These results suggest that most, if not all, of the mutations in these regions were already present before the development of HCC, implying the possibility that the mutations were not a result of HCC but, rather, were a possible causative factor for the development of HCC. It would be intriguing to test whether an HCV core protein with such a mutation has a greater capacity to transform cells in culture and/or in transgenic mice. In this connection, the remaining 40% of the isolates obtained from patients with HCC did not have such a mutation in the regions concerned, with the result implying the possible presence of another mutation(s) in the HCV polyprotein that is involved in the development of HCC. On the other hand, Hayashi et al. (9) reported on a different aspect of HCV core protein mutation. They found that patients with consistently abnormal levels of alanine aminotransferase (ALT) were more likely to develop HCC than those with consistently normal ALT levels and that the core proteins of HCV isolates from the patients with abnormal ALT levels exhibited a quasispecies nature. The same investigators speculated that mutations in the core protein were a result of viral escape from the immune responses of the host and that strong immune responses would cause a series of hepatocytic injuries followed by regeneration, which might trigger malignant transformation of the cell.
It was previously reported that mutations were clustered in a region between aa 39 and 76 of the core proteins of HCV isolates from patients with HCC, and therefore, the region was referred to as a clustering variable region (10, 28). The same research group also reported that the number of mutations in the clustering variable region was larger in isolates from cancerous tissues than in those from noncancerous tissues and sera of HCC patients (11). However, the present study shows that there were 0.9 ± 0.8 and 1.3 ± 1.1 mutations in the region from aa 39 to 76 in isolates from patients with and without HCC, respectively, with the difference being not statistically significant (P = 0.13). Consistent with our observation, Giménez-Barcons et al. (7) recently reported that there was no significant difference in the number of mutations in the N-terminal sequence of 85 aa residues between isolates from patients with and without HCC. We also observed that codon 45 (Gly) was completely conserved among all 59 isolates analyzed (data not shown). Our observation disagrees with the information in previous reports by Horie et al. (10, 11), who showed that codon 45 was Gly in isolates from cancerous tissues of patients with HCC, while it was Ser in isolates from noncancerous tissues and sera of patients with and without HCC. In this connection, it should be noted that we used the direct sequencing method without subcloning and that only a representative sequence was detected in our study, with a minor group(s) of quasispecies sequences having been overlooked in our study. As for the other types of mutations, Rüster et al. (26) reported that HCV isolates from cancerous tissues of a patient with HCC had deletion mutations near the N terminus of the core protein that led to a frame shift that generated proteins with truncated C termini. However, we did not find deletions or insertions in the core protein-coding sequences of the isolates tested. The average diameter of HCC in our study was 4.2 cm, with most of them being less than 4 cm. It is possible that in the later stages of tumor progression HCV replication in cancerous tissues is impaired due to certain changes in the cellular environment, which may cause more drastic mutations of the viral genome, such as deletions.
Despite a considerable degree of sequence diversity in the entire HCV core protein (Table 1), Ser-53, Ser-99, and Ser-116 were completely conserved in all 59 isolates analyzed in the present study (data not shown). Shih et al. (27) reported that Ser-53 and Ser-116 are potential phosphorylation sites for protein kinase A, that Ser-53 and Ser-99 are potential phosphorylation sites for protein kinase C, and that the phosphorylation of Ser-99 and Ser-116 but not that of Ser-53 is essential for the suppressive activity of the core protein on hepatitis B virus gene expression and replication. On the other hand, the phosphorylation of Ser-53 was shown to be essential for interaction of the core protein with an epsilon isoform of the 14-3-3 protein, which activated the kinase Raf-1 (1). The results of the present study thus support the idea that these three Ser residues are important for the proper functioning of the HCV core protein.
Xu et al. (32) recently identified a novel HCV protein, the F protein, generated by a ribosomal frame shift into the +2/−1 reading frame of the core protein-coding region of the viral genomes of HCV-1a strains. The sequences around the initiation site of the frame shift differ between HCV-1a and HCV-1b isolates, and therefore, the occurrence of such a frame shift in HCV-1b isolates has yet to be proven. With this possibility in mind, we predicted the amino acid sequences of the hypothetical F protein of the HCV-1b isolates from patients with and without HCC. Consistent with the observation by Xu et al. (32), the length of the F protein differed for different isolates of HCV-1b, but a 144-residue product was most common, being detected in 71% of all isolates analyzed. Among the HCV-1b isolates analyzed, the hypothetical F protein showed more sequence diversity than the core protein, but there were no significant differences in mutation rates and sites between isolates from patients with HCC and those from patients without HCC.
Acknowledgments
This work was supported in part by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (JSPS) and a research grant from the Research Foundation of Viral Hepatitis of Japan. This work was also part of a collaborative research project between Southeast Asian countries and Japan conducted by JSPS.
REFERENCES
- 1.Aoki, H., J. Hayashi, M. Moriyama, Y. Arakawa, and O. Hino. 2000. Hepatitis C virus core protein interacts with 14-3-3 protein and activates the kinase Raf-1. J. Virol. 74:1736-1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Apichartpiyakul, C., C. Chittivudikarn, H. Miyajima, M. Homma, and H. Hotta. 1994. Analysis of hepatitis C virus isolates among healthy blood donors and drug addicts in Chiang Mai, Thailand. J. Clin. Microbiol. 32:2276-2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruno, S., E. Silini, A. Crosignani, F. Borzio, G. Leandro, F. Bono, M. Asti, S. Rossi, A. Larghi, A. Cerino, M. Podda, and M. U. Mondelli. 1997. Hepatitis C virus genotypes and risk of hepatocellular carcinoma in cirrhosis: a prospective study. Hepatology 25:754-758. [DOI] [PubMed] [Google Scholar]
- 4.Chang, J., S.-H. Yang, Y.-G. Cho, S. B. Hwang, Y. S. Hahn, and Y. C. Sung. 1998. Hepatitis C virus core from two different genotypes has an oncogenic potential but is not sufficient for transforming primary rat embryo fibroblasts in cooperation with the H-ras oncogene. J. Virol. 72:3060-3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doi, H., C. Apichartpiyakul, K. Ohba, M. Mizokami, and H. Hotta. 1996. Hepatitis C virus (HCV) subtype prevalence in Chiang Mai, Thailand, and identification of novel subtypes of HCV major type 6. J. Clin. Microbiol. 34:569-574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Enomoto, N., I. Sakuma, Y. Asahina, M. Kurosaki, T. Murakami, C. Yamamoto, Y. Ogura, N. Izumi, F. Marumo, and C. Sato. 1996. Mutations in the nonstructural protein 5A gene and response to interferon in patients with chronic hepatitis C virus 1b infection. N. Engl. J. Med. 334:77-81. [DOI] [PubMed] [Google Scholar]
- 7.Giménez-Barcons, M., S. Franco, Y. Suárez, X. Forns, S. Ampurdanes, F. Puig-Basagoiti, A. Sánchez-Fueyo, J.-M. Barrera, J.-M. Llovet, J. Bruix, J.-M. Sánchez-Tapias, J. Rodés, and J.-C. Saiz. 2001. High amino acid variability within the NS5A of hepatitis C virus (HCV) is associated with hepatocellular carcinoma in patients with HCV-1b-related cirrhosis. Hepatology 34:158-167. [DOI] [PubMed] [Google Scholar]
- 8.Greene, W. K., M. K. Cheong, V. Ng, and K. W. Yap. 1995. Prevalence of hepatitis C virus sequence variants in South-East Asia. J. Gen. Virol. 76:211-215. [DOI] [PubMed] [Google Scholar]
- 9.Hayashi, J., N. Furusyo, I. Ariyama, Y. Sawayama, Y. Etoh, and S. Kashiwagi. 2000. A relationship between the evolution of hepatitis C virus variants, liver damage, and hepatocellular carcinoma in patients with hepatitis C viremia. J. Infect. Dis. 181:1523-1527. [DOI] [PubMed] [Google Scholar]
- 10.Horie, C., H. Iwahana, T. Horie, I. Shimizu, K. Yoshimoto, S. Yogita, S. Tashiro, S. Ito, and M. Itakura. 1996. Detection of different quasispecies of hepatitis C virus core region in cancerous and noncancerous lesions. Biochem. Biophys. Res. Commun. 218:674-681. [DOI] [PubMed] [Google Scholar]
- 11.Horie, T., I. Shimizu, C. Horie, M. Yasuda, S. Yogita, S. Tashiro, and S. Ito. 1999. Mutations of the core gene sequence of hepatitis C virus isolated from liver tissues with hepatocellular carcinoma. Hepatol. Res. 13:240-251. [Google Scholar]
- 12.Hotta, H., M. Kemapunmanus, C. Apichartpiyakul, Soetjipto, R. Handajani, and N. G. Barzaga. 1997. Differential distribution of hepatitis C virus subtypes in Asia: comparative study among Thailand, Indonesia, the Philippines and Japan. Southeast Asian J. Trop. Med. Public Health 28(Suppl.):323-331. [PubMed] [Google Scholar]
- 13.Kato, N., M. Hijikata, Y. Ootsuyama, M. Nakagawa, S. Ohkoshi, T. Sugimura, and K. Shimotohno. 1990. Molecular cloning of the human hepatitis C virus genome from Japanese patients with non-A, non-B hepatitis. Proc. Natl. Acad. Sci. USA 87:9524-9528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lauer, G. M., and B. D. Walker. 2001. Hepatitis C virus infection. N. Engl. J. Med. 345:41-52. [DOI] [PubMed] [Google Scholar]
- 15.Lusida, M. I., M. Nagano-Fujii, C. A. Nidom, Soetjipto, R. Handajani, T. Fujita, K. Oka, and H. Hotta. 2001. Correlation between mutations in the interferon sensitivity-determining region of NS5A protein and viral load of hepatitis C virus subtypes 1b, 1c, and 2a. J. Clin. Microbiol. 39:3858-3864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marusawa, H., M. Hijikata, T. Chiba, and K. Shimotohno. 1999. Hepatitis C virus core protein inhibits Fas- and tumor necrosis factor alpha-mediated apoptosis via NF-κB activation. J. Virol. 73:4713-4720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mellor, J., E. C. Holmes, L. M. Jarvis, P. L. Yap, P. Simmonds, and the International HCV Collaborative Study Group. 1995. Investigation of the pattern of hepatitis C virus sequence diversity in different geographical regions: implications for virus classification. J. Gen. Virol. 76:2493-2507. [DOI] [PubMed] [Google Scholar]
- 18.Moriya, K., H. Fujie, Y. Shintani, H. Yotsuyanagi, T. Tsutsumi, K. Ishibashi, Y. Matsuura, S. Kimura, T. Miyamura, and K. Koike. 1998. The core protein of hepatitis C virus induces hepatocellular carcinoma in transgenic mice. Nat. Med. 4:1065-1067. [DOI] [PubMed] [Google Scholar]
- 19.Murakami, T., N. Enomoto, M. Kurosaki, N. Izumi, F. Marumo, and C. Sato. 1999. Mutations in nonstructural protein 5A gene and response to interferon in hepatitis C virus genotype 2 infection. Hepatology 30:1045-1053. [DOI] [PubMed] [Google Scholar]
- 20.Nousbaum, J. B., S. Pol, B. Nalpas, P. Landais, P. Berthelot, and C. Brechot. 1995. Hepatitis C virus type 1b (II) infection in France and Italy. Ann. Intern. Med. 122:161-168. [DOI] [PubMed] [Google Scholar]
- 21.Ray, R. B., K. Meyer, and R. Ray. 1996. Suppression of apoptotic cell death by hepatitis C virus core protein. Virology 226:176-182. [DOI] [PubMed] [Google Scholar]
- 22.Ray, R. B., L. M. Lagging, K. Meyer, and R. Ray. 1996. Hepatitis C virus core protein cooperates with ras and transforms primary rat embryo fibroblasts to tumorigenic phenotype. J. Virol. 70:4438-4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reed, K. E., and C. M. Rice. 2000. Overview of hepatitis C virus genome structure, polyprotein processing, and protein properties. Curr. Top. Microbiol. Immunol. 242:55-84. [DOI] [PubMed] [Google Scholar]
- 24.Robertson, B., G. Myers, C. Howard, T. Brettin, J. Bukh, B. Gaschen, T. Gojobori, G. Maertens, M. Mizokami, O. Nainan, S. Netesov, K. Nishioka, T. Shin-i, P. Simmonds, D. Smith, L. Stuyver, and A. Weiner. 1998. Classification, nomenclature, and database development for hepatitis C virus (HCV) and related virus: proposals for standardization. Arch. Virol. 143:2493-2503. [DOI] [PubMed] [Google Scholar]
- 25.Rüster, B., S. Zeuzem, V. Krump-Konvalinkova, T. Berg, S. Jonas, K. Severin, and W. K. Roth. 2001. Comparative sequence analysis of the core- and NS5-region of hepatitis C virus from tumor and adjacent non-tumor tissue. J. Med. Virol. 63:128-134. [PubMed] [Google Scholar]
- 26.Rüster, B., S. Zeuzem, and W. K. Roth. 1996. Hepatitis C virus sequences encoding truncated core proteins detected in a hepatocellular carcinoma. Biochem. Biophys. Res. Commun. 219:911-915. [DOI] [PubMed] [Google Scholar]
- 27.Shih, C.-M., C.-M. Chen, S.-Y. Chen, and Y.-H. W. Lee. 1995. Modulation of the trans-suppression activity of hepatitis C virus core protein by phosphorylation. J. Virol. 69:1160-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shimizu, I., D.-F. Yao, C. Horie, M. Yasuda, M. Shiba, T. Horie, T. Nishikado, X.-Y. Meng, and S. Ito. 1997. Mutations in a hydrophilic part of the core gene of hepatitis C virus in patients with hepatocellular carcinoma in China. J. Gastroenterol. 32:47-55. [DOI] [PubMed] [Google Scholar]
- 29.Soetjipto, R. Handajani, M. I. Lusida, S. Darmadi, P. Adi, Soemarto, S. Ishido, Y. Katayama, and H. Hotta. 1996. Differential prevalence of hepatitis C virus subtypes in healthy blood donors, patients on maintenance hemodialysis, and patients with hepatocellular carcinoma in Surabaya, Indonesia. J. Clin. Microbiol. 34:2875-2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song, J., M. Fujii, F. Wang, M. Itoh, and H. Hotta. 1999. The NS5A protein of hepatitis C virus partially inhibits the antiviral activity of interferon. J. Gen. Virol. 80:879-886. [DOI] [PubMed] [Google Scholar]
- 31.Tsuchihara, K., M. Hijikata, K. Fukuda, T. Kuroki, N. Yamamoto, and K. Shimotohno. 1999. Hepatitis C virus core protein regulates cell growth and signal transduction pathway transmitting growth stimuli. Virology 258:100-107. [DOI] [PubMed] [Google Scholar]
- 32.Xu, Z., J. Choi, T. S. B. Yen, W. Lu, A. Strohecker, S. Govindarajan, D. Chien, M. J. Selby, and J.-H. Ou. 2001. Synthesis of a novel hepatitis C virus protein by ribosomal frameshift. EMBO J. 20:3840-3848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yasui, K., T. Wakita, K. Tsukiyama-Kohara, S.-I. Funahashi, M. Ichikawa, T. Kajita, D. Moradpour, J. R. Wands, and M. Kohara. 1998. The native form and maturation process of hepatitis C virus core protein. J. Virol. 72:6048-6055. [DOI] [PMC free article] [PubMed] [Google Scholar]