Abstract
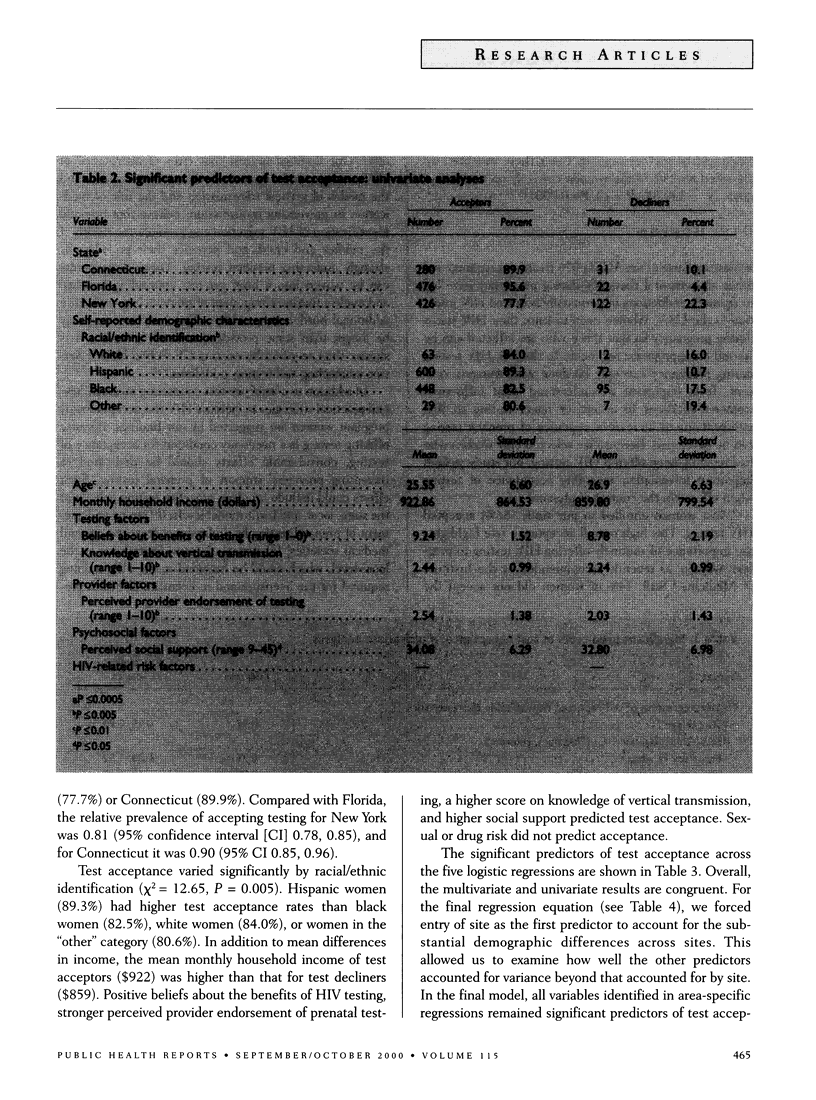
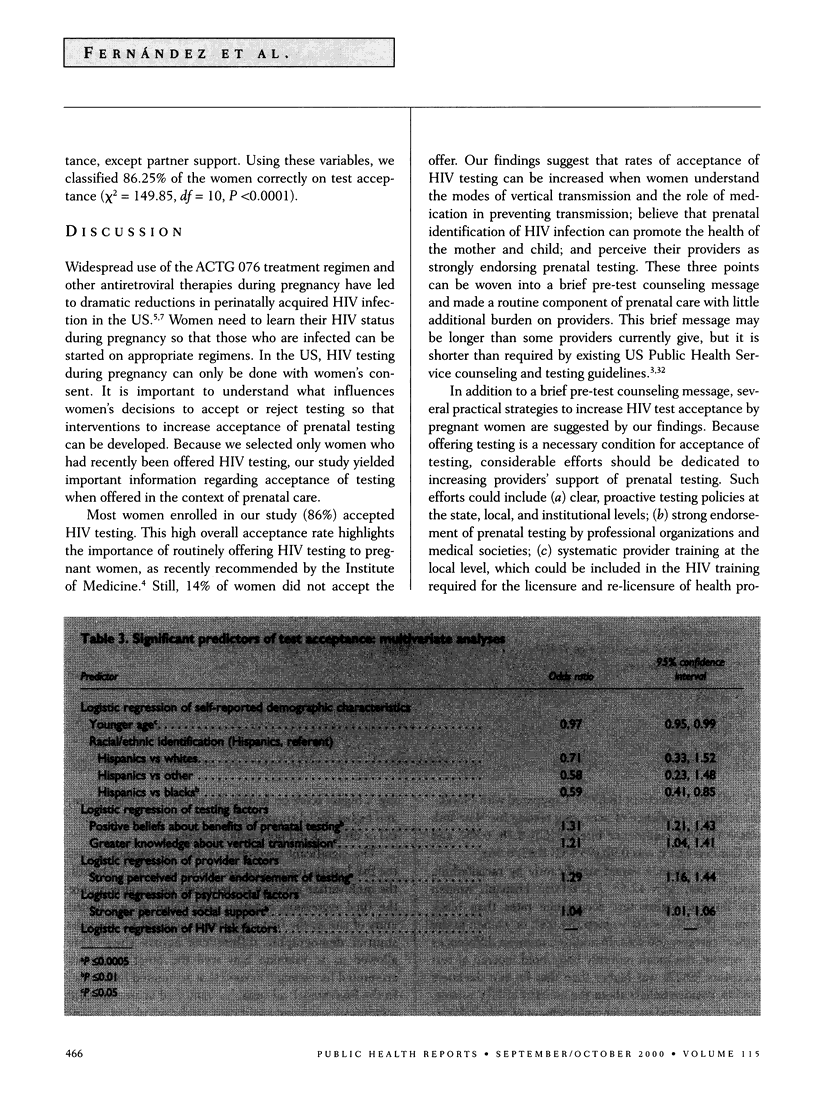
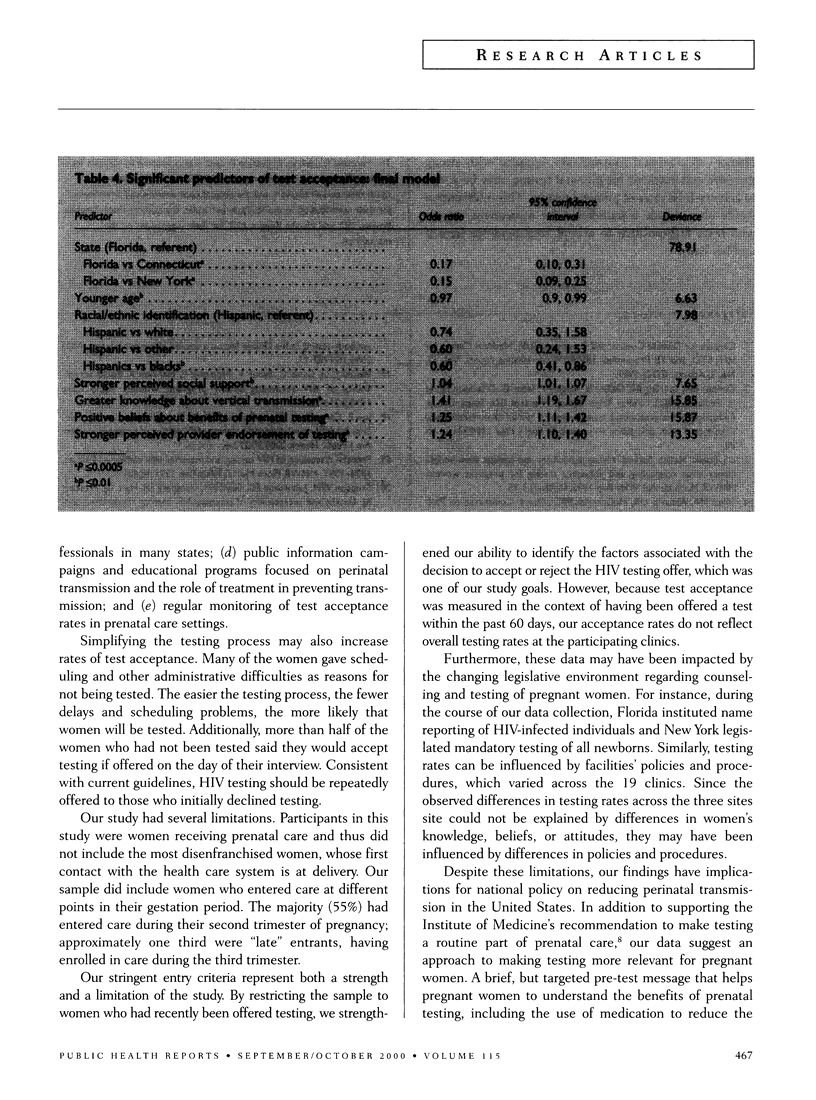
OBJECTIVE: The purpose of this study was to assess the factors associated with acceptance of HIV testing during pregnancy on the part of women receiving prenatal care at public clinics. METHODS: Trained interviewers recruited and interviewed 1,357 women receiving prenatal care at clinics in Florida, Connecticut, and New York City. RESULTS: Eighty-six percent of participants reported having been tested or having signed a consent form to be tested. Acceptance of testing was found to be related to strong beliefs about the benefits of testing, knowledge about vertical transmission, perceived provider endorsement of testing, and social support. Women who declined testing said they did so because they did not perceive themselves to be at risk for HIV (21%) or they faced administrative difficulties (16%) with some aspect of the testing process (for example, scheduling, limited availability of pre-test counselors). CONCLUSIONS: Acceptance rates can be increased when women understand the modes of vertical transmission and the role of medication regimens in preventing transmission; believe that prenatal identification of HIV can promote the health of mother and child; and perceive their providers as strongly endorsing testing. These points can be woven into a brief pre-test counseling message and made a routine component of prenatal care.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beevor A. S., Catalan J. Women's experience of HIV testing: the views of HIV positive and HIV negative women. AIDS Care. 1993;5(2):177–186. doi: 10.1080/09540129308258598. [DOI] [PubMed] [Google Scholar]
- Connor E. M., Sperling R. S., Gelber R., Kiselev P., Scott G., O'Sullivan M. J., VanDyke R., Bey M., Shearer W., Jacobson R. L. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. N Engl J Med. 1994 Nov 3;331(18):1173–1180. doi: 10.1056/NEJM199411033311801. [DOI] [PubMed] [Google Scholar]
- Irwin K. L., Valdiserri R. O., Holmberg S. D. The acceptability of voluntary HIV antibody testing in the United States: a decade of lessons learned. AIDS. 1996 Dec;10(14):1707–1717. doi: 10.1097/00002030-199612000-00016. [DOI] [PubMed] [Google Scholar]
- Joo E., Carmack A., Garcia-Buñuel E., Kelly C. J. Implementation of guidelines for HIV counseling and voluntary HIV testing of pregnant women. Am J Public Health. 2000 Feb;90(2):273–276. doi: 10.2105/ajph.90.2.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limata C., Schoen E. J., Cohen D., Black S. B., Quesenberry C. P., Jr Compliance with voluntary prenatal HIV testing in a large health maintenance organization (HMO). J Acquir Immune Defic Syndr Hum Retrovirol. 1997 Jun 1;15(2):126–130. doi: 10.1097/00042560-199706010-00005. [DOI] [PubMed] [Google Scholar]
- Lindegren M. L., Byers R. H., Jr, Thomas P., Davis S. F., Caldwell B., Rogers M., Gwinn M., Ward J. W., Fleming P. L. Trends in perinatal transmission of HIV/AIDS in the United States. JAMA. 1999 Aug 11;282(6):531–538. doi: 10.1001/jama.282.6.531. [DOI] [PubMed] [Google Scholar]
- Lindsay M. K., Adefris W., Peterson H. B., Williams H., Johnson J., Klein L. Determinants of acceptance of routine voluntary human immunodeficiency virus testing in an inner-city prenatal population. Obstet Gynecol. 1991 Oct;78(4):678–680. [PubMed] [Google Scholar]
- Meadows J., Catalan J., Gazzard B. "I plan to have the HIV test"--predictors of testing intention in women attending a London antenatal clinic. AIDS Care. 1993;5(2):141–148. doi: 10.1080/09540129308258594. [DOI] [PubMed] [Google Scholar]
- Meadows J., Catalan J., Gazzard B. HIV antibody testing in the antenatal clinic. Midwifery. 1993 Mar;9(1):17–27. doi: 10.1016/0266-6138(93)90038-t. [DOI] [PubMed] [Google Scholar]
- Meadows J., Catalan J., Gazzard B. HIV antibody testing in the antenatal clinic: the views of the consumers. Midwifery. 1993 Jun;9(2):63–69. doi: 10.1016/0266-6138(93)90048-w. [DOI] [PubMed] [Google Scholar]
- Ruiz J. D., Molitor F. Knowledge of treatment to reduce perinatal human immunodeficiency virus (HIV) transmission and likelihood of testing for HIV: results from two surveys of women of childbearing age. Matern Child Health J. 1998 Jun;2(2):117–122. doi: 10.1023/a:1022944907256. [DOI] [PubMed] [Google Scholar]
- Simonds R. J., Steketee R., Nesheim S., Matheson P., Palumbo P., Alger L., Abrams E. J., Orloff S., Lindsay M., Bardeguez A. D. Impact of zidovudine use on risk and risk factors for perinatal transmission of HIV. Perinatal AIDS Collaborative Transmission Studies. AIDS. 1998 Feb 12;12(3):301–308. doi: 10.1097/00002030-199803000-00008. [DOI] [PubMed] [Google Scholar]
- Sobo E. J. Attitudes toward HIV testing among impoverished inner-city African-American women. Med Anthropol. 1994 Nov;16(1):17–38. doi: 10.1080/01459740.1994.9966107. [DOI] [PubMed] [Google Scholar]
- Sorin M. D., Tesoriero J. M., LaChance-McCullough M. L. Correlates of acceptance of HIV testing and post-test counseling in the obstetrical setting. AIDS Educ Prev. 1996 Feb;8(1):72–85. [PubMed] [Google Scholar]
- Wade N. A., Birkhead G. S., Warren B. L., Charbonneau T. T., French P. T., Wang L., Baum J. B., Tesoriero J. M., Savicki R. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. N Engl J Med. 1998 Nov 12;339(20):1409–1414. doi: 10.1056/NEJM199811123392001. [DOI] [PubMed] [Google Scholar]
- Weber J. T., Frey R. L., Jr, Horsley R., Gwinn M. L. Publicly funded HIV counseling and testing in the United States, 1992-1995. AIDS Educ Prev. 1997 Jun;9(3 Suppl):79–91. [PubMed] [Google Scholar]


