Abstract
•Objective
To investigate how sociocultural factors influence the management of pain from sickle cell disease by comparing the experiences of those who usually manage their pain at home with the experiences of those who are more frequently admitted to hospital for management of their pain.
•Design
Qualitative analysis of semistructured individual interviews and focus group discussions.
•Participants
57 participants with genotype SS or S/β-thal (44 participants) or SC (9 participants); the status of 4 participants was unknown. 40 participants took part in focus groups, 6 took part in both focus groups and interviews, and 9 were interviewed only. Participants were allocated to focus groups according to ethnic origin, sex, and the number of times that they had been admitted to the hospital for the management of painful crises during the previous year.
•Results
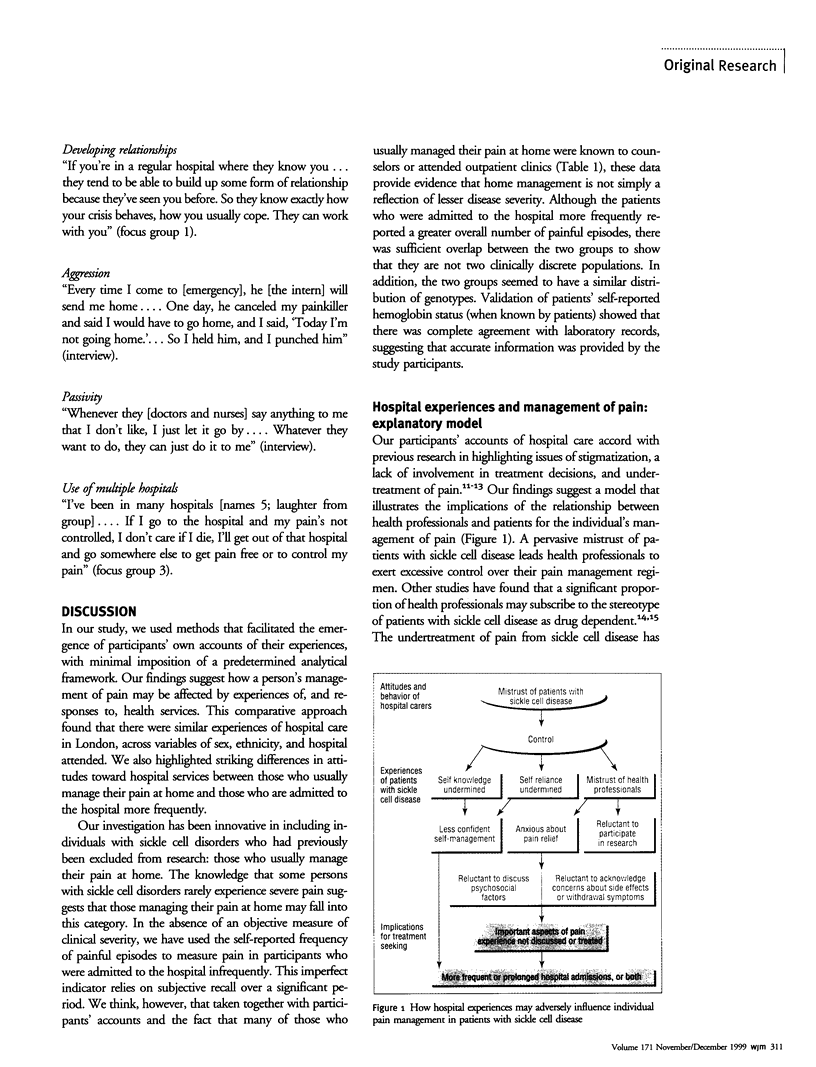
The relation between patients with sickle cell disease and hospital services is one of several major, nonclinical dimensions that shape experiences of pain management and behavior for seeking health care. Participants' experiences of hospital care show a range of interrelated themes that are common to most participants across variables of sex, ethnicity, and which hospital was attended. Themes identified included the mistrust of patients with sickle cell disease, stigmatization, excessive control (including both overtreatment and undertreatment of pain) and neglect. Individuals responded to the challenge of negotiating care with various strategies. Patients with sickle cell disease who are frequently admitted to hospital may try to develop long-term relationships with their caregivers, become passive or aggressive in their interactions with health professionals, or regularly attend different hospitals. Those who usually manage their pain at home expressed a strong sense of responsibility for the management of their pain and advocated self-education, assertiveness, and resistance as strategies toward hospital services.
•Conclusions
The organization and delivery of management for the pain of a sickle cell crisis discourages self-reliance and encourages hospital dependence. Models of care should recognize the chronic nature of sickle cell disorders and give priority to patients' involvement in their care.
Full text
PDF






Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alleyne J., Thomas V. J. The management of sickle cell crisis pain as experienced by patients and their carers. J Adv Nurs. 1994 Apr;19(4):725–732. doi: 10.1111/j.1365-2648.1994.tb01144.x. [DOI] [PubMed] [Google Scholar]
- Brozović M., Davies S. C., Brownell A. I. Acute admissions of patients with sickle cell disease who live in Britain. Br Med J (Clin Res Ed) 1987 May 9;294(6581):1206–1208. doi: 10.1136/bmj.294.6581.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gignac M. A., Cott C. A conceptual model of independence and dependence for adults with chronic physical illness and disability. Soc Sci Med. 1998 Sep;47(6):739–753. doi: 10.1016/s0277-9536(98)00149-x. [DOI] [PubMed] [Google Scholar]
- Konotey-Ahulu F. I. Opiates for sickle-cell crisis? Lancet. 1998 May 9;351(9113):1438–1438. doi: 10.1016/S0140-6736(05)79487-3. [DOI] [PubMed] [Google Scholar]
- Layton D. M., Mufti G. J. Opiates for sickle-cell crisis? Lancet. 1998 Jun 27;351(9120):1964–1965. doi: 10.1016/s0140-6736(05)78656-6. [DOI] [PubMed] [Google Scholar]
- Layzell S., McCarthy M. Community-based health services for people with HIV/AIDS: a review from a health service perspective. AIDS Care. 1992;4(2):203–215. doi: 10.1080/09540129208253091. [DOI] [PubMed] [Google Scholar]
- Murray N., May A. Painful crises in sickle cell disease--patients' perspectives. BMJ. 1988 Aug 13;297(6646):452–454. doi: 10.1136/bmj.297.6646.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olujohungbe A., Cinkotai K. I., Yardumian A. Hydroxyurea therapy for sickle cell disease in Britain. Disappointing recruitment despite promising results. BMJ. 1998 Jun 6;316(7146):1689–1689. doi: 10.1136/bmj.316.7146.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt O. S., Thorington B. D., Brambilla D. J., Milner P. F., Rosse W. F., Vichinsky E., Kinney T. R. Pain in sickle cell disease. Rates and risk factors. N Engl J Med. 1991 Jul 4;325(1):11–16. doi: 10.1056/NEJM199107043250103. [DOI] [PubMed] [Google Scholar]
- Pope C., Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995 Jul 1;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serjeant G. R. Natural history and determinants of clinical severity of sickle cell disease. Curr Opin Hematol. 1995 Mar;2(2):103–108. doi: 10.1097/00062752-199502020-00001. [DOI] [PubMed] [Google Scholar]
- Shapiro B. S., Benjamin L. J., Payne R., Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manage. 1997 Sep;14(3):168–174. doi: 10.1016/S0885-3924(97)00019-5. [DOI] [PubMed] [Google Scholar]
- Streetly A., Dick M., Layton M. Sickle cell disease: the case for coordinated information. BMJ. 1993 Jun 5;306(6891):1491–1492. doi: 10.1136/bmj.306.6891.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldrop R. D., Mandry C. Health professional perceptions of opioid dependence among patients with pain. Am J Emerg Med. 1995 Sep;13(5):529–531. doi: 10.1016/0735-6757(95)90163-9. [DOI] [PubMed] [Google Scholar]
- Westerman M. P., Bailey K., Freels S., Schlegel R., Williamson P. Assessment of painful episode frequency in sickle-cell disease. Am J Hematol. 1997 Mar;54(3):183–188. doi: 10.1002/(sici)1096-8652(199703)54:3<183::aid-ajh2>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]


