Research shows that general practitioners fail to diagnose up to half of cases of depression or anxiety.1 Many studies are cross sectional and have been criticised because, unlike primary care itself, they contain no longitudinal element. They do not always indicate whether undetected depression is important clinically or whether it is diagnosed at a later date, persists undetected, or causes disability.
We aimed to determine whether depression or anxiety not diagnosed during one general practice consultation is diagnosed during follow up or is self limiting and of no clinical importance.
Participants, methods, and results
We followed up consecutive attenders at a general practice in north Bristol in 1997.2 The original sample represented patients attending morning and evening surgeries and all doctors in the practice.
We interviewed 179 patients with the 12 item general health questionnaire and 12 item short form health survey.3,4 We followed up 71% (160/227) of patients still in the practice and 43% (28/65) of those who had moved. Patients who scored 3 or more on the general health questionnaire received a more detailed psychiatric assessment with the clinical interview schedule.5 We analysed the general practitioners' records for psychological diagnoses, treatments, and referrals during the follow up period.
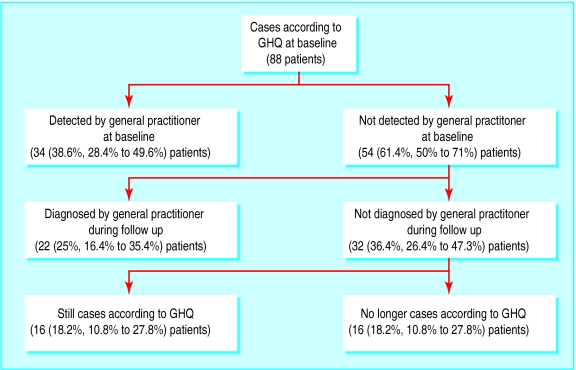
Patients who were followed up were older (48.5 v 43.3 years), were more likely to be female (76% v 68%), and had lower mean scores on the general health questionnaire (3.6, 95% confidence interval 3 to 4.1, v 4.2, 3.5 to 4.9) than those we did not follow up (67 declined, 37 were untraceable, and nine questionnaires were incomplete). None of these differences was statistically significant. Overall, the results of the questionnaire showed that 88/179 (49%, 42% to 57%) patients had depression or anxiety in the original study, but only 34 (39%, 28% to 50%) of these had received a diagnosis of depression or anxiety at that time. Of the 54 who had not received a diagnosis during the original study, 22 received a diagnosis during the three years of follow up (figure).
Of the 56 patients who received a diagnosis, 38 (68%, 54% to 80%) were treated with antidepressants. Twelve (21%, 12% to 34%) were referred to psychiatric services.
Psychological diagnoses had never been made in 32 of the 88 patients; 16/88 (18%; 11% to 28%) patients had depression or anxiety according to the general health questionnaire and had never received a diagnosis from their general practitioner. These 16 patients had severe symptoms (mean score on general health questionnaire 6.4, 4.8 to 7.9). Twelve (14%, 7% to 23%) of the 88 patients without a diagnosis were cases according to the clinical interview schedule or had daily activities adversely affected by anxiety or depression according to the short form health survey.4,5
Comment
Although many patients with depression did not receive a diagnosis at a single consultation, most were given a diagnosis at subsequent consultations or recovered without a general practitioner's diagnosis. Three years later, 14% of patients with depression still had a clinically severe condition, had not received a diagnosis, and might have benefited from treatment.
The prevalence of anxiety and depression (49%) was in line with the high prevalence often found in primary care studies.1 We did not follow up 43 undiagnosed cases (of a total of 153 cases in the original study)—we do not know the outcome of these cases, but the patients were more likely to have changed practice than those we did follow up. This mobility means that those we did not follow up may have been less likely to have received appropriate diagnosis and treatment than those we did follow up. We may have underestimated the proportion of undetected cases.
This small study estimates hidden psychiatric morbidity more realistically than cross sectional studies. General practitioners feel they have been criticised unfairly for missing up to half of the patients with depression that present to them. This study supports their view. Undiagnosed depression may lead to long term disability, but the problem may not be as large as has been thought. Evidence that general practitioners fail to detect one in seven patients with treatable depression are more in tune with clinical impression than estimates of one in two, but the outcome for patients with undetected depression still needs attention.
Figure.
Diagnosis of patients with depression and anxiety in a cross sectional study and three year follow up period. GHQ = general health questionnaire
Footnotes
Funding: Small project grant from NHS South and West Research and Development. DK is an MIA/RCGP research fellow.
Competing interests: DS and DK received honorariums for attending two meetings sponsored by GlaxoSmithKline. GL has received payment from a number of pharmaceutical companies.
References
- 1.Goldberg D, Huxley P. Common mental disorders. London: Routledge; 1992. [Google Scholar]
- 2.Kessler D, Lloyd K, Lewis G, Gray DPG, Heath I. Cross sectional study of symptom attribution and recognition of depression and anxiety in primary care. BMJ. 1999;318:436–440. doi: 10.1136/bmj.318.7181.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg D, Williams P. A user's guide to the general health questionnaire. Windsor: NEFR Nelson; 1991. [Google Scholar]
- 4.Jenkinson C, Layte R. Development and testing of the UK SF-12. J Health Serv Res Policy. 1997;1:14–18. doi: 10.1177/135581969700200105. [DOI] [PubMed] [Google Scholar]
- 5.Lewis G, Pelosi A, Glover E. The development of a computerised assessment for minor psychiatric disorder. Psychol Med. 1988;18:737–745. doi: 10.1017/s0033291700008448. [DOI] [PubMed] [Google Scholar]