Abstract
More than 30 years of experience in developing a computer-based patient record system, The Medical Record (TMR), in multiple settings, in multiple specialty groups, and at multiple sites has taught us many lessons. Lessons related to computer-based patient records include the importance of a data model in which input, storage, and planned use are independent; separation of patient-specific data from metadata; a modular design to localize the program code that deals with a set of data; redundant storage to optimize tasks and response time; and integration of decision support into work process. Lessons related to medical informatics include the importance of a clinical–technical partnership, control of tools at the leading edge, and rapid prototyping in the real world. Finally, changes in technology move the challenges but do not eliminate them.
Much of my professional career has dealt with the creation, implementation, and support of a computer-based patient record system that became known as The Medical Record, or TMR. In this lecture, I would like to discuss with you some of those experiences—what we did, what the driving factors were, what worked and what didn't, what lessons we learned, and what implications for medical informatics might be drawn.
TMR Context
Over its existence, TMR has been implemented in over 40 different sites. It has been implemented in 14 different medical specialties. It has operated in outpatient settings, inpatient settings, intensive care settings, and combinations of these settings. The smallest application was a solo practitioner, and the largest site supported more than 350 providers. The maximum number of patients supported by TMR in one system was approximately 750,000. The Medical Record provides an integrated clinical and accounting functionality. At its peak, it was operational in 15 different sites. At present, TMR is operational in four sites. It is still a character-based system, uses DEC's VMS operating system, and runs on the Alpha computer.
The Medical Record was developed in an environment with limited resources—we were pushing the envelope of the technologies and the tools that were available to us. Over the past 30 years, the evolution of TMR has been driven primarily by the requirements of the myriad users. The advances in our work were a direct consequence of solving problems, and we were particularly fortunate to have selected a design architecture that provided freedom in evolving the system. We never faced a problem that we were ultimately unable to solve. In all our applications, we involved a clinical expert in the domain of implementation, and all our systems were tested in real-world environments, often removed from our physical setting.
Development and Evolution of The Medical Record
Our early work began with the development of a 19-page, mark-sense screening medical history. Around this time, the minicomputer was beginning to appear on the scene. The history-taking project was first initiated on a large mainframe but failed because of cost and the inability to get program, mark-sense output tape and the punched cards containing the free-text data together at the same time. By interfacing the reader directly to the minicomputer and entering the free-text data directly, we solved both the cost and timeliness problems.1
The screening history was followed immediately by the development of a real-time, interactive headache questionnaire by Bill Stead (William W. Stead, MD, Vanderbilt University), a first-year medical student, working with the Division of Neurology. Patients completed the history directly on the minicomputer.2 This project also provided our first experience with decision support, with the program identifying the type of headache. The diagnostic accuracy matched that of the neurologist. Unfortunately, the neurologist did not need a program for help, and the cost of the hardware was too great for primary care sites, which had a need but only a small number of relevant patients. Other history-taking programs developed over time included a pediatric well-baby questionnaire3 and work with an audio version of the screening history.4
In passing, I mention that we proposed a hospital information system for Duke Hospital based on a group of minicomputers connected together. We almost convinced Duke to make the commitment, but instead Duke supplied funding to begin the development of a computer-based medical record. We selected the Division of Obstetrics as the focus of that project, for several reasons. First, the Division was willing. Second, the obstetrics clinic was in a different location from the delivery suite, and records had to be in two places at once—difficult in paper form. Obstetrics also used a number of forms, and the people were accustomed to controlled data capture. Data were reasonably well defined, and the report requirements were known.
The obstetric medical record was developed on a Digital Computer Corporation PDP-12, shown in Figure 1▶. Each DEC tape would accommodate the records for only one month's pregnancies. Patients' records were stored on the tape by the month of expected delivery, and Bill Stead slept in the computer room to change the tapes as required as we crossed each month's boundary.
Figure 1.

The PDP-12 minicomputer, manufactured by the Digital Equipment Corporation. This minicomputer had 4 KB of 12-bit words as main memory, a 20-character by 12-line cathode ray tube display screen, and a 300-KB DEC tape for secondary storage.
We computerized what was done manually. Although external “tables” were used to define display screens, the application was primarily hard coded. We began with mark-sense forms to collect the prenatal history and another mark-sense form for the obstetric examination. The output was in narrative form and often exceeded eight pages. We were not popular, and we quickly learned the definition of information overload.
Fortunately, Bill Stead, as a second-year medical student now, was on obstetric rotation. He saw firsthand what was actually needed and overnight rewrote the output program to create Junior Resident admit note. Figure 2▶ shows the outline for an admit note taken from the 1971 student orientation manual and the computerized version of this note. He extracted the appropriate data from the previously scanned data and reformatted the output to match what had previously been written by hand, leaving space for the five additional items required but not in the database. The users were now happy, because the computer made life easier by meeting a need and reducing their task load. Part of this output was a half-page “starred box” that contained all the data of essential importance and included pertinent medical problems.5,6
Figure 2.
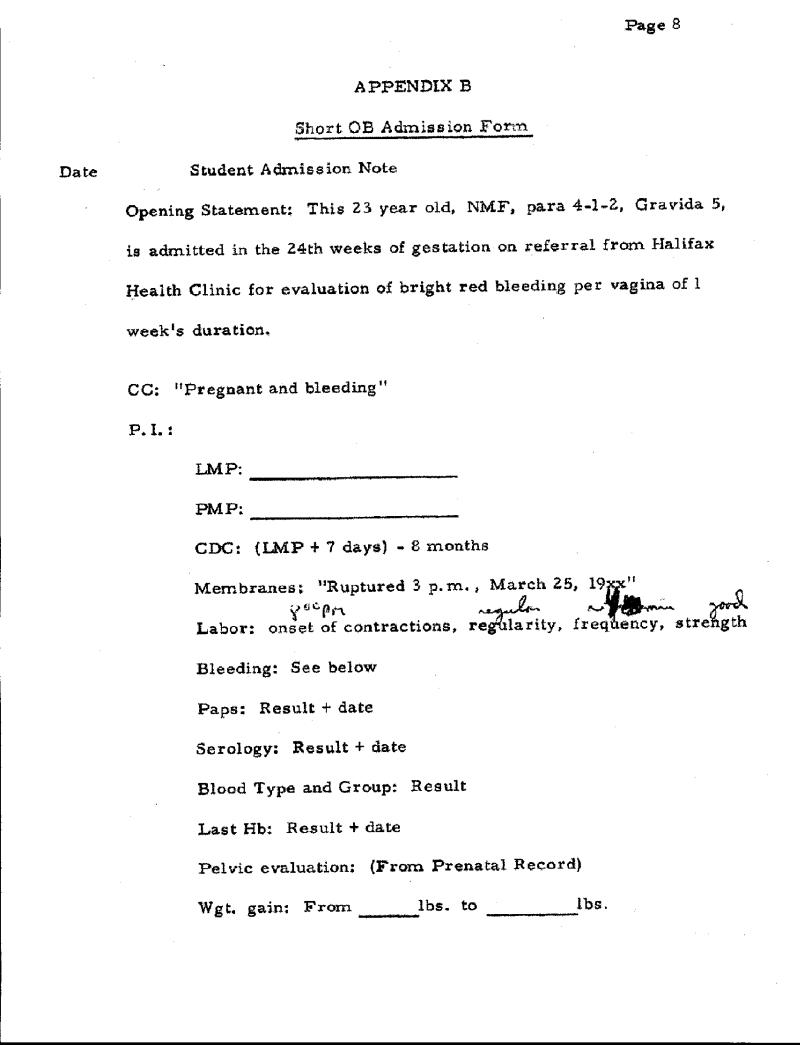
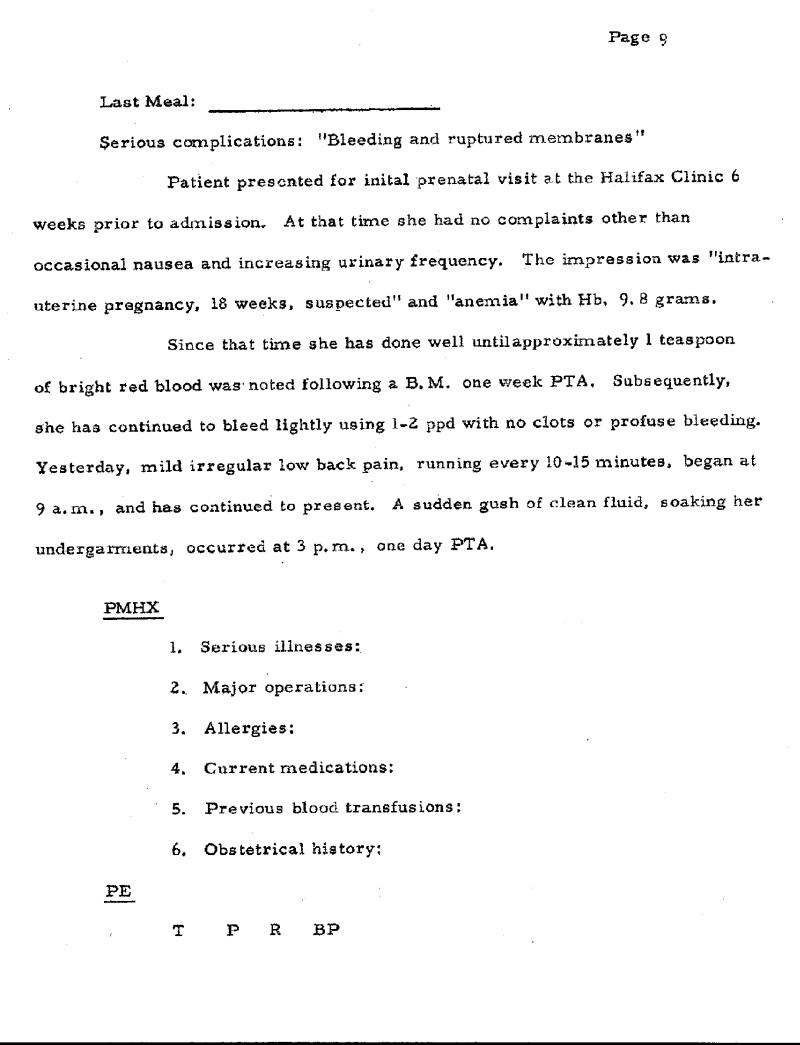
Original admit note taken from the 1971 student orientation manual in the Division of Obstetrics at Duke University Medical Center. Original computer version of admit note. Known data were added to the form by the computer, leaving only five items to be entered by the resident.
We wrote these programs in assembly language simply because there were no other adequate languages available for interactive minicomputers. We had written several programs, each dedicated to a specific purpose—INPUT, FRAMES, MASSAGE, PRINT, RETRIEVE, and STORE. These programs were run in sequence. They worked but created an undesirable overhead; for example, if you needed to use MASSAGE to do a calculation in the middle of a branching questionnaire, you had to switch programs.
In 1972, we decided to formalize these tool-kit programs as a formal programming language that we called gemisch.7 The functionalities of the individual programs were converted into commands in the new language. The new language represented a considerable increase in the scale of what we could produce. We still use it today, and it has grown into a powerful, high-level database management. It is interpretive, translated into a pseudocode for execution.
gemisch is characterized by extremely powerful text manipulating functionality, smart print-generating capability, variable and flexible file types and file-handling routines, display functionality within the limitation of character-based and other features that made it easy to interface to any type of device or provide any functionality.8 I note that many other groups developed their own languages during this period, including MUMPS and HELP. In spite of the criticisms we have heard over the years, controlling our programming environment enabled us to survive four changes in operating systems, meet a variety of interface requirements and make the programs do whatever was necessary.9 With the addition of GUI functionality, I am not convinced that continued use of this language is not in our best interest.
We next developed a computer-based record for primary care.10 This application used a different design and was transaction oriented. Each encounter was a record, and encounters were linked by the patient ID. Although we started this project strictly as a clinical CPR (computerized patient record), we quickly understood that for the system to be affordable and used, we must also meet the needs for practice management, such as scheduling and accounting. A new family medicine unit was formed, which was affiliated with the Durham County Hospital. Although this group started with the identical CPR system that was implemented at Duke, within a month the system had changed so much that applications were two different packages supported by two different groups. We quickly found ourselves supporting four sites, with a programming staff of 25 people. We needed a solution that would permit the same program to be used in all settings and reduce the support requirements.
By 1975, our concept of what would be required to support a CPR began to have form. Our experience had further taught us the limits of reproducing documents that looked like the ones that worked with paper-based procedures. Bill Stead was now a renal fellow, and he took one year—his only dedicated extended period of time—and worked with me.
During 1975, we took a new approach to the electronic patient record. Bill defined a data structure that represented data according to its meaning as contrasted to its planned use. He then prototyped modules to capture into this structure the records of the patients he was seeing in his nephrology clinic. I then programmed the modules needed to use this structure to support practice management aspects of the primary care clinics.
The resulting computer-based patient record—TMR—had the characteristics that we felt were significant and necessary for handling the multiple features required to support a variety of clinics:
Modular construction which simplifies programming, documentation and maintenance
Data-independent programming through data definition dictionaries, which permit the same program to function differently in a variety of clinics
A combination of problem-oriented and timeoriented formats to generate a record that would more completely satisfy the need for patient care
Two input modes—a parameter-oriented, direct input mode for source data entry and indirect input using paper or dictation to capture input for subsequent input by third party
The direct coupling of protocols to data entry and data display
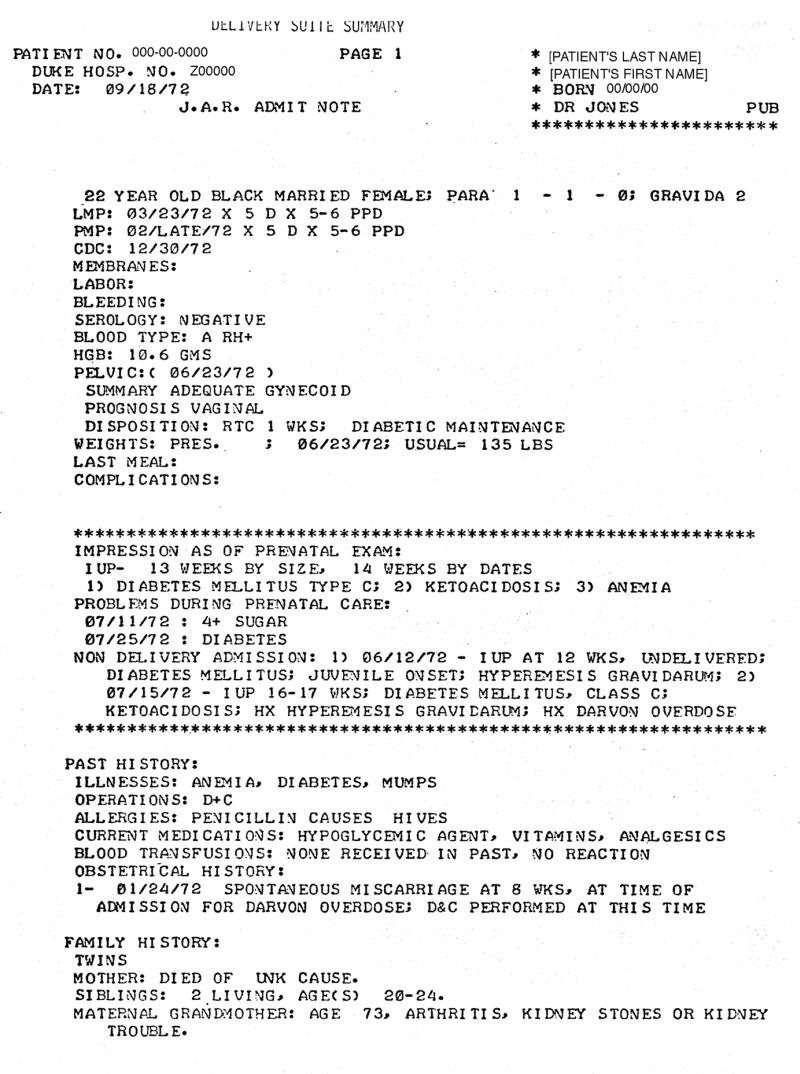
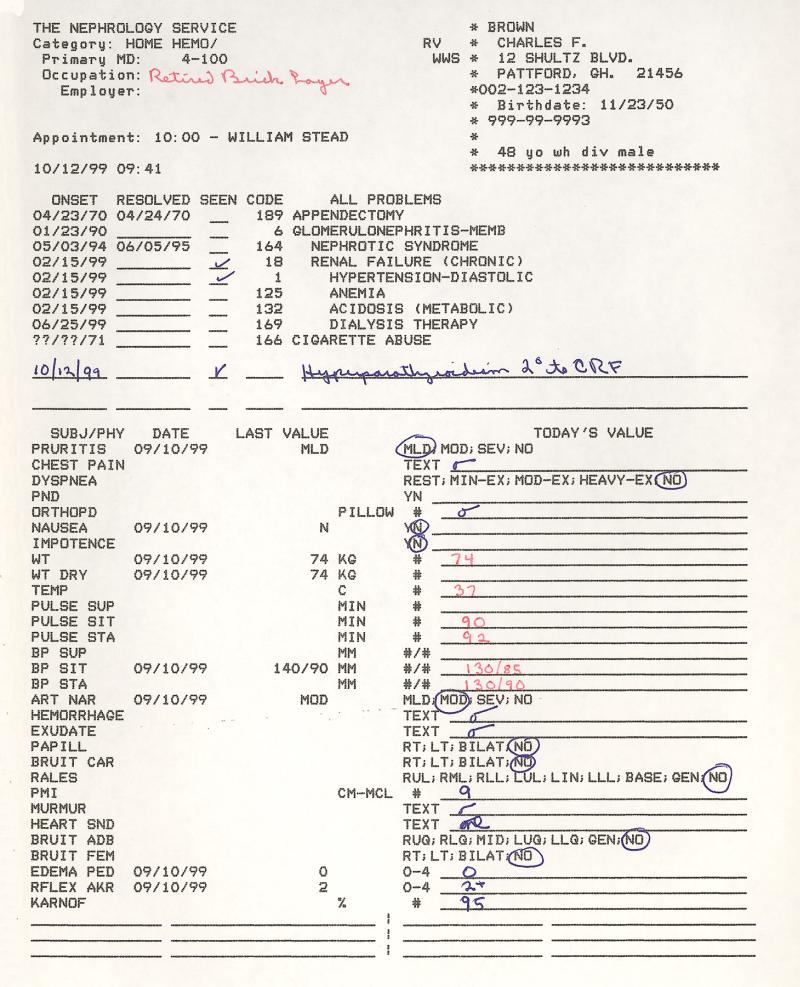
The design of the new TMR took about three to five years before we were able to enter a complete medical record into the computer.11–16 The renal clinic at the Durham VA Hospital provided our first experience with real-time data entry by providers. The physicians were required to enter all prescriptions directly into the computer. Figure 3▶ shows the rolling cart that provided access to the terminal used by physicians to input the prescription data. The high repeat rate of medications for this population of patients meant that drugs could be re-ordered with a minimum of keystrokes. This was clearly a time-saving activity and was well received by the physicians.17 The record included demographics, problem list, drugs and allergies, and laboratory data as well as history and physical examination findings. The physicians entered these data directly when it made sense. They used notes on encounter printouts when paper was a better interface. Figure 4▶ shows the paper renal encounter entry form on which data were entered by both nurse and physician for subsequent entry into the computer by a data entry person. In these cases, a physician assistant “brought the record up.”18
Figure 3.

View of rolling cart, used to move computer terminal to hallway outside examining rooms in the Durham VA hospital. Dr. Bill Yarger is shown entering prescription data into the terminal for a patient he has just seen. Physicians were required to enter prescriptions directly into this terminal after a patient visit.
Figure 4.
Computer-generated patient pre-encounter form used to capture data during a patient encounter. The computer completed much of the form, including the most recent value for time-oriented data items. Nurses wrote on the form in blue ink and the physicians wrote in red ink. A data entry person eventually entered the data into the computer.
University Health Services Clinic, Family Medical Clinic, and later obstetrics were converted to TMR.19 One program supported the four sites with differences and customization accomplished through a metadata dictionary. Working with physician-focused clinical systems and patient-management- focused systems was a valuable experience. We learned to tailor the capture of data to the user. We learned to block delays in performance to natural transition times. We learned to maximize data stored on a single screen and to minimize keystrokes for entry of data. Figure 5▶ shows a patient management component—one day of an inpatient encounter. All clinical and billable data were entered on this screen, usually from the paper encounter sheet filled in by the nurse and physician.
Figure 5.
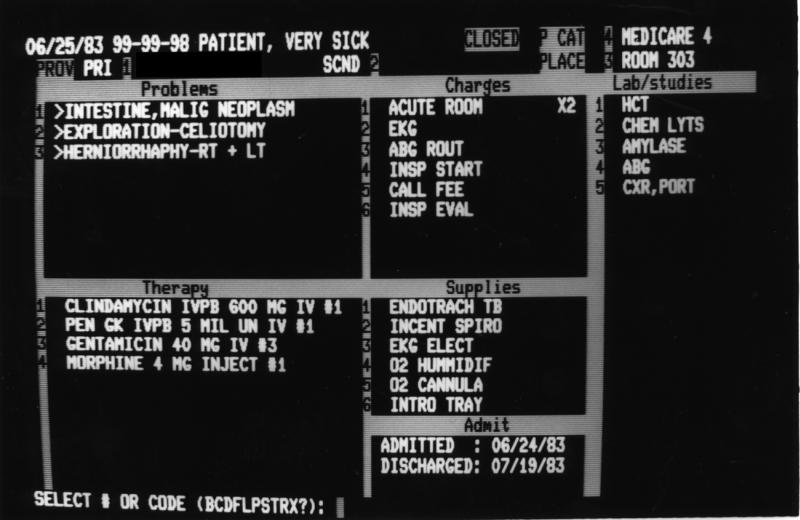
One-day screen for an inpatient encounter. This screen permitted the collection of all items, including disposition, that were recorded during a patient encounter. Items were entered using a text completer routine. A subsequent screen displayed the super bill. The ICD-9 and CPT codes were automatically extracted from the metadictionary.
In 1980, a start-up family practice unit in Los Angeles purchased TMR for installation into their clinic of 35 providers. This, our first non-Duke implementation, was the first site to use all the pieces of TMR in one setting. The academic setting had tended to use only aspects they were pioneering. This experience taught us the difference between a local academic setting and a remotely supported private setting.20,21
The Division of Cardiology had created a research database for patients with coronary artery disease, starting in the late 1960s.22 In 1983, that application was moved to TMR and coupled with clinical functionality. The question was, could data acquired as part of the process of delivering care be used as a research database? To a large extent, with interesting exceptions, the answer was yes.23
Supporting Cardiology required additional functionality in the form of new data collection screens, new displays, and new data types. Figure 6▶ shows a cardiology data entry screen. We designed frame drivers that collected input data from a number of diagnostic tests, including cardiac catheterization, echo cardiograms, and treadmills. A template, including the most likely data to be entered, was defined in the dictionary for each doctor. It also required new report-writing capability to translate structured data into narrative reports and an inverted file to optimize cross-record retrieval.24,25 The TMR protocol system was also used to track patients with coronary artery disease for follow-up.26 Research needs also required the development of a query system.27
Figure 6.
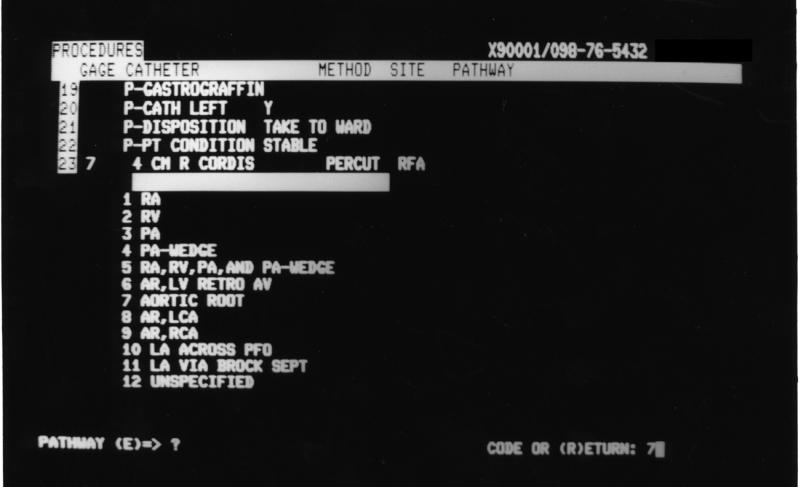
Data capture screen used by the Division of Cardiology. This screen illustrates the method for the capture of data for a cardiac catheterization. The point of data entry is for the pathway of the catheter. Entry is selected from the list retrieved from the metadictionary.
In 1982, we also installed our first inpatient system in the Kenneth Norris Cancer Research Hospital here in Los Angeles. That site still runs TMR. As TMR was installed in additional settings at Duke, we needed to interact with the hospital information system.28 Kenneth Norris Hospital also was the site of the development of an independent (but real-time interfaced with TMR) laboratory system.29,30 This experience taught us the differences between focused, departmental systems and the computerized record. We learned what should be stored in the laboratory system for management purposes and what needed to be passed back to the CPR. We learned about synchronization of databases and events, such as system backup, and we learned about persistence of data in the patient's record and in the departmental system database.
We learned there are major differences between inpatient and outpatient systems.31,32 The volume of data increases significantly in the inpatient setting. Patients stay for longer periods of time. Late charges are a fact of life. Patients are grouped in wards rather than from an appointment list. On the other hand, decision support has a more immediate value. Drugs are more powerful, and the risks of drug–drug interactions and adverse reactions are greater. We defined new types of displays and new pathways through the system. The inpatient system tracked patients as they moved from one location to another. Tests that had to be scheduled were queued for scheduling when they were ordered, resulting in considerable time savings and increased efficiencies. Table 1▶ compares what we learned about the outpatient, inpatient, and intensive care environments.
Table 1.
Comparison of Outpatient, Inpatient, and Intensive Care Settings Relating to the Electronic Health Record
| Intensive Care | Inpatient | Outpatient | |
|---|---|---|---|
| Volume of data | Highest | Medium | Low |
| Need for quick response | Highest | Medium | Low |
| Value of decision support | Immediate | Daily | Long |
| Persistence value of data | Very short | Short | Long |
| Medical device integration | High | Medium | Low–none |
In 1988, we began the bedside pilot project in a surgical intensive care unit , in which we interfaced to a number of bedside instruments and implemented online nursing notes.33–37
Over the years, we continued to try to involve the providers of care in the electronic system.38 Key requirements were response time, clarity of use, minimal effort, and return on investment. The addition of decision support features39,40 and evaluation in efficiency and quality41,42 support the case for ROI. Stead demonstrated labor savings in the renal division.17 We developed a philosophy for the demand-oriented medical record—the ability to deliver what the provider wanted when and how they wanted it.43 In the family medicine setting, we were able to alter provider prescribing habits through computer feedback.44,45 The Medical Record became a key and dependable part of the family medicine practice.46 Laboratory data were delivered to providers as an e-mail messages that could then be annotated and e-mailed to the patients.47 Automatic links to literature retrieval were provided, with the results linked into the patients' records.48
The obstetrics system has continued to evolve over the past 30 years. At Duke, the system expanded to include some inpatient activity.49 Clinical records for the newborn babies were automatically created and included important data about the mother's pregnancy and the birth process. The obstetric database now includes two generations of pregnancy history and birth data. The obstetric system made a significant impact on fetal mortality and morbidity when a regional database was established to track prenatal experiences of pregnant women over a five-county area. The computer was used to ensure adequate prenatal care and to make sure prenatal data were available at the points of delivery.50 The 30 years‘ accumulation of rich clinical data in obstetrics has resulted in several research studies.51–54
The multiple implementations of TMR throughout Duke required us to learn how to deal with multiple databases that must interact.55 An example is the seamless transition from one appointment system to another. We had to deal with different vocabularies, synchronization of databases,56 scalability and accommodating growth,57 interfacing to other systems for analysis,58 and development of data interface standards.59–61 We gained valuable experience in the operation of several types of clinical information systems.62–65 We learned how to estimate the requirements for clinical information systems.66–68 The different applications of TMR permitted us to understand how to transition from a paper system to an electronic record system.69,70 We experimented with different approaches in the use of paper and automation.71–73
Major active development in TMR continued until 1997.74 Work on computerized clinical guidelines was integrated into TMR.75,76 Maintenance programming continues. For example, early this year we accommodated the required changes for the new APC codes. The TMR data, which are very rich in clinical content, continue to be mined for knowledge.56,77 New versions of TMR have been prototyped,78 but the long-term future of TMR has yet to be determined.
Lessons about Clinical Systems and Databases
A key factor in the long-term survival and ubiquitous use of TMR was the adoption of a data model in which input, storage, and planned use were all independent. For example, historical data could be input from a mark-sense short form or a long form. Input was direct from a scanner and from frames through which textual data were entered. Storage was organized in a modular fashion, by category of data, independent of input source or mode. Output could be a short narrative report, a long narrative report, or just a listing of the abnormal findings.
We stored in the patient's record only the data that varied from patient to patient. Data were mostly structured, and free text was used to enhance meaning, to capture the gestalt of the interaction, or to substitute for a term not defined in the metadata dictionary. Data elements were stored as pointers to categorical sections in the dictionary of metadata.
The metadata dictionary, in compiled form, is stored as a fixed-length, directly pointer-accessed file. Figure 7▶ identifies the content of the metadata dictionary. It defines the data elements for each section of the patient record—problems, procedures, studies, therapies, clinical findings, supplies, providers, places, accounting, etc. The metadata dictionary permits the use of one program that runs in a variety of settings and a variety of clinical specialties. The metadata dictionary contains all the business rules for any given implementation. The dictionary contains such things as data element definitions, vocabulary and external code sets, physical resources, data capture protocols, billing algorithms, decision-support rules, work flow, information flow, linkages, management information, report generation, drug–drug interactions, and resources. Any and all data elements stored in TMR and the rules for their use are stored in the metadata dictionary. Figure 8▶ shows the detail for a problem entry in the data dictionary.
Figure 7.
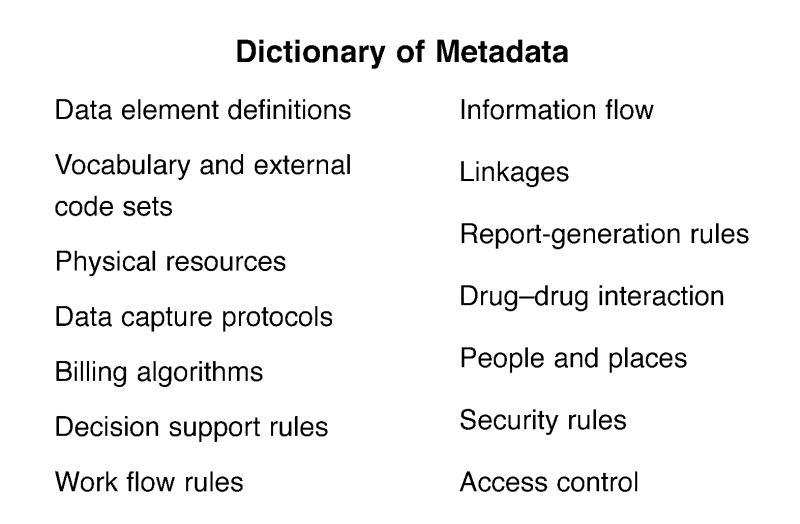
Types of data stored in the metadata dictionary.
Figure 8.
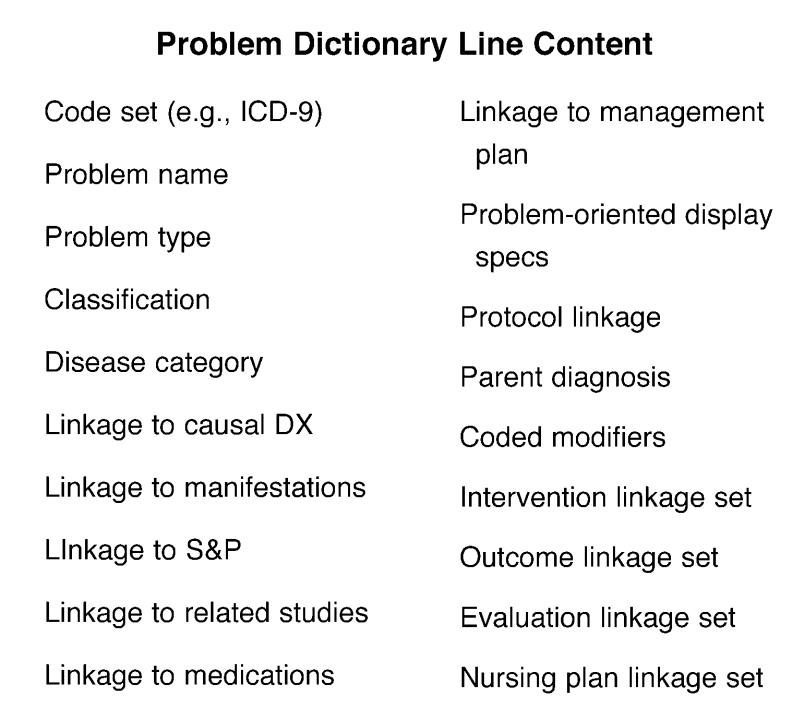
Details of metadata entry for a problem.
Limited resources and large amounts of data demanded a very compact storage of data. We also knew we wanted to permit variable-length free-text data as well as coded structured data. The architecture of the gemisch record is shown in Figure 9▶. Each data element, called a node, is represented by a three-bit code, or trit. Numbers are stored as characters. The record contains a large buffer (initially set to 4 KB, now set at 64 KB), in which the text is entered from one end and node pointer pairs from the other end, moving toward each other. Text is terminated with a special character. The node-pointer pairs are in sort order and permit direct access to the text. A deletion clears the trit and removes the node-pointer pair. Updates are in place if an update is the same length or shorter or is relocated with a first-fit algorithm. When the two sets meet, an automatic garbage collection is performed.
Figure 9.
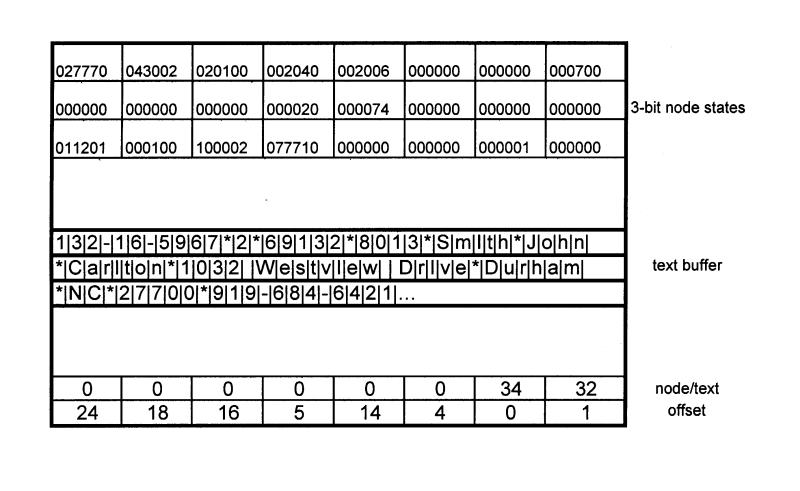
The gemisch record structure. This object-oriented format permits maximum compression of data and rapid retrieval of individual data elements.
Data are stored as delimited strings containing pointers to the appropriate metadata line, a date-time stamp, and result. The result may be any of a number of data types, including coded data which, in turn, is defined in the metadata dictionary. Time-oriented data may be stored by repeating the date, time, and result strings or as a sparse matrix, with date-time stored only once as a column heading. Data fields are variable length and permit repetition of data elements with a repeat delimiter. Health Level 7 messages use a similar delimited syntax. Figure 10▶ illustrates the storage of data in the gemisch record.
Figure 10.
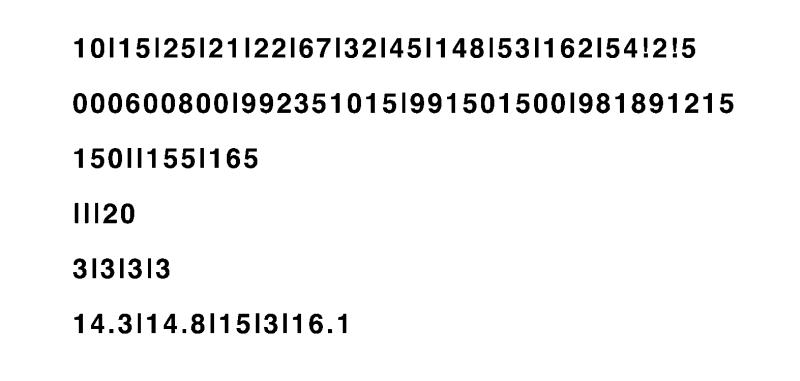
Database structure for time-oriented data. The first line shows the codes in display order delimited by “|”. A search of this line quickly identified what items were present. The second line shows the date-time stamp for items present (column heading) Subsequent lines contain the actual data values.
Post-compositional data elements can be defined at the time of use under control of the metadata dictionary, which ensures that the combination makes sense. For example, phase, timing and location may define a heart murmur. Rather than pre-composing these terms in the dictionary by defining all possible combinations, TMR permits the dynamic definition at the time of use, by sequentially prompting for additional detail. One physician might enter murmurs and stop. Another might add that it is systolic, and a third might fully define it.
The Medical Record programs use a modular design in which we localize the things that deal with a set of data. The modules are monitor, registration, appointments, problems, studies, history and physical findings, therapies, encounters, accounting, and subroutines. The continued development of TMR over the past 25 years has followed a pattern of first programming a specific solution to a requirement as a separate program or conditional code. The patch is then generalized, with the business rules defined in the metadata dictionary. Finally, each module is reworked every three or four years, and the new functionality is integrated seamlessly into the module.
Modules are much like classes. Some of the routines are components that are reused. For example, TMR includes a completer subroutine that is reused for every data entry. The completer interfaces between the user program and the metadata dictionary—which also contains a synonym list for each data element.
The basic patient record in TMR contains all time- independent data and the latest sets of time-oriented data. The amount of time-oriented data is controlled by volume of data. Older data are stored in online archive files by class, with pointers to the data contained in the primary record. Any data element, regardless of the volume of data, is online and retrievable with a maximum of two disk reads.
Data are stored redundantly to optimize tasks and enhance response time. For example, the encounter storage includes the problems and procedures that are dealt with in the encounter, the resources used, studies ordered, medications dispensed, supplies, professional fees, and disposition. Encounter problems, subject to business rules defined in the dictionary, are also stored in a summary problem section. The dictionary defines parent–child linkages, and a more precise definition replaces a more general definition in the summary problem lists. The study data are also stored as time-oriented data. Therapy data (prescription drugs, immunizations, and allergies) are stored with prescribing data in a therapy class section.
Other types of files enhance performance. Each updated record is stored in a daily file as well as the total file. At the end of the day, the daily records are used to generate reports, create the day's statistics, and provide real-time backup of active data. Accounting data are transferred and redundantly stored in a collection's workstation. Accounting data are used to validate the integrity of the files before transferring the daily records to the backup total file. Other files track protocols and other events that need to be monitored. An inverted file supports across patient retrievals. This inverted file actually has better response characteristics than some commercial databases.
This data architecture has survived for more than 30 years. We also wrote our own record management routines for optimum utilization of disk space. Patient records that are on the order of a few hundred kilobytes expand to tens of megabytes in a relational database system.
Two other lessons were gleaned from our experiences. First, decision-support algorithms need to be integrated seamlessly into the normal flow of the work process. Second, the CPR is more than a repository for data. Enhancements to work flow and automatic linkages to events and actions made the programs much more useful. Examples include automatically queuing ordered tests that must be scheduled and linking the appointment process into the disposition event.
Implications for Medical Informatics
All application developments in TMR have been done with a clinical partner in the specialty area. The clinical partner is active in the practice; often the fact that the co-developer is using the system has prevented embarrassing errors and much more sensible design.
The most critical partnership in the development of TMR was the relationship between Bill Stead and me. As a partnership, we performed as a medical informaticist using Bill's clinical expertise and my technical expertise. Part of that relationship was each teaching the other. It wasn't just “this is how you should do it.” It was getting a level of understanding so that we each knew why we were doing it in a certain way.
The reason we could meet any requirement was that we controlled our tools at the leading edge—hardware and software. You can do whatever you have to do to enhance response, accommodate volume, or interface a device. Examples include interfacing the scanner to the computer (at a cost of $15) or modifying DEC's operating system to a seven-user time operating system.79 In the early obstetrics system, typing a character on a teletype located in the delivery room captured the computer to service the interrupt. Having our own language permitted us to accommodate new operating systems and new computers without having to change the application. We satisfied most of the Y2K problems by changing the language. Even independent systems can be interfaced.
The modular structure of TMR promoted rapid prototyping as stand-alone projects. Periodically, these stan-alone prototypes are incorporated back into the module.
The file design permits scaling the system to handle any volume of data or number of records—supporting any number of computers, servers, or disks.
Significant advances in hardware and software capabilities occurred over the lifetime of TMR. The first systems were implemented on a Digital Equipment Corporation (DEC) Linc-8 and then PDP-12 minicomputer with 4 KB of 12-bit memory. The data were stored on 300-KB small magnetic tape units. The display was a 12-line, 20-column cathode ray tube. Our first printers were teletypes with uppercase only, printing on rolls of paper. From there, we evolved to drum printers, then to line printers, and now to laser printers. Operating systems became available that supported multiple users and sophisticated file-handling systems. Video terminals evolved from 12-line 20-character displays to 24-line 80-character and then full graphic displays with multiple fonts. Memory size increased from 4 to 8 to 64 to 256 KB and then to megabytes. Storage devices increased from 300 KB to 2.1 MB, through 80, 300, and 600 MB, and now to gigabyte storage. Connectivity moved from twisted pair to coax to fiber. We used RADs, line drivers, modems, and finally Internet.
Change in technology only moves the challenges; it does not eliminate them.
Acknowledgments
The author acknowledges the contributions of Bill Stead in preparing this talk. His passion for history and documentation helped recall the experiences throughout the years. The author also acknowledges some of the many people who contributed to the development to TMR and GEMISCH over the years. The original development team included Alton Brantley, Steve Feagin, Steven Lloyd, Bill Stead, and E. L. (Skip) Walter. Mark Straube joined the team early and is the keeper of GEMISCH; he continues to adopt and modify the language. Jim Collins, Edward Hammond III, Ruby Grewal, and many others have also made contributions.
In the application areas, contributors from Duke University have been, in obstetrics, Rick Jelovsek, Bob Brame, Marvin Hage and Kay Schlitz; in family medicine, Harvey Estes, Steve Gehlbach, John Hansen, Kim Yarnall, and Lloyd Michener; in nephrology, Bill Stead, Bill Yarger, and Jim Fitzwilliams. Other contributors from Duke have been David Pryor, Rob Califf, Pat Blunden, and others in cardiology; Joe Moylan, Kevin Fitzpatrick, and all the nurses in intensive care; Skip Burton in dermatology; Al Heyman in neurology; John Rice in rheumatology; and Bill Peters in bone marrow transplantation. Contributors outside Duke have included Marshall Berns, John Casagrande, John Daniels, Michael Hillier, Jon Sternburg, Lois Funderburk, Kay Hammond, and many others.
This lecture was originally presented at the AMIA Annual Symposium, November 4–8, 2000, in Los Angeles, California.
References
- 1.Hammond WE, Brantley AB, Thompson Jr. HK. Interface of PDP-12 computer and optical scanner. Decus Proc. 1970187–90.
- 2.Stead WW, Heyman A, Thompson HK Jr, Hammond WE. Computer-assisted interview of patients with functional headache. Arch Intern Med. 1972;129:950–5. [PubMed] [Google Scholar]
- 3.Pearlman MH, Hammond WE, Thompson HK Jr. An automated well-baby questionnaire. Pediatrics. 1973;51(6):972–9. [PubMed] [Google Scholar]
- 4.Stead WW, Hammond WE, Estes EH. Evaluation of an audio mode of the automated medical history. Methods Inf Med. 1977;16(1):20–3. [PubMed] [Google Scholar]
- 5.Stead WW, Hammond WE, Brame RG. A computerized obstetrical record. 1972;2:5–14. [Google Scholar]
- 6.Stead WW, Brame RG, Hammond WE, Jelovsek FR, Estes EH, Parker RT. A computerized obstetrical medical record. Obstet Gynecol. 1977;49(4):502–9. [PubMed] [Google Scholar]
- 7.Hammond WE, Brantley BA, Feagin SJ, Lloyd SC, Stead WW, Walter EL. gemisch: a minicomputer informationsupport system. Proc IEEE. 1973;61(11):1575–83. [Google Scholar]
- 8.Straube MJ, Hammond WE, Stead WS. The gemisch programming language. In: Orthner HF, Blum BI (eds). Implementing Health Care Information Systems. New York: Springer-Verlag, 1989.
- 9.Hammond WE, Stead WW. The evolution of gemisch and TMR. In: Orthner HF, Blum BI (eds). Implementing Health Care Information Systems. New York: Springer-Verlag, 1989.
- 10.Hammond WE. Computerization of the primary medical record. Proc 25th Annu Conf Eng Med Bio. 1972;14:129. [Google Scholar]
- 11.Hammond WE, Stead WW, Feagin SJ, Brantley BA, Straube MJ. Data base management system for ambulatory care. Proc 1st Annu Symp Comput Appl Med Care. 1977;1:173–87. [Google Scholar]
- 12.Hammond WE, Stead WS, Feagin SJ, Brantley BA, Straube MF. Database system for ambulatory care. In: Blum B (ed). Information System for Patient Care. New York: Springer-Verlag, 1983.
- 13.Hammond WE, Stead WW. The evolution of a computerized medical information system—TMR. Proc 10th Annu Symp Comput Appl Med Care. 1986;10:147–56. [Google Scholar]
- 14.Hammond WE. Computerized medical record systems. MD Comput. 1987;4(3):5–6.3657464 [Google Scholar]
- 15.Hammond WE. Patient management systems: the early years. ACM Conf Hist Med Inf. 1987:153–64.
- 16.Stead WS, Hammond WE. Computer-based medical records: the centerpiece of TMR. MD Comput. 1988;5(5): 48–62. [PubMed] [Google Scholar]
- 17.Stead WW, Hammond WE. How to realize labor savings with a computerized medical record. Proc 4th Annu Symp Comput Appl Med Care. 1980;4(2):1200–1205. [Google Scholar]
- 18.Stead WW, Garrett LE, Hammond WE. Practicing nephrology with a computerized medical record. Kidney Int. 1983;24:446–54. [DOI] [PubMed] [Google Scholar]
- 19.Hammond WE. Ambulatory care systems—TMR. Proc 6th Annu Symp Comput Appl Med Care. 1982;6:75. [Google Scholar]
- 20.Hammond WE, Stead WW, Straube MJ, Hammond WE III. Experiences in the transfer of a medical information system from an academic setting to a private setting. Proc 5th Annu Symp Comput Appl Med Care. 1981;5:949–52. [Google Scholar]
- 21.Hammond WE, Stead WS. Transportability of software. In: Bakker AR, Ball MJ, Scherrer JR, Willems JL (eds). Towards New Hospital Information Systems. Proceedings of an IMIA Working Conference (Nijmegen, The Netherlands; May 14–18, 1988). Amsterdam, The Netherlands: Elsevier Science Publishers, 1988:293–8.
- 22.Rosati RA, McNeer JF, Starmer CF, Mittler BS, Morris JJ Jr, Wallace AG. A new information system for medical practice. Arch Intern Med. 1975;135:1017–24. [PubMed] [Google Scholar]
- 23.Pryor DB, Stead WW, Hammond WE, Califf RM, Rosati RA. Features of TMR for a successful clinical and research database. Proc 6th Annu Symp Comput Appl Med Care. 1982;6:79–84. [Google Scholar]
- 24.Hammond WE, Stead WW, Straube MJ, Lutz MW. TMR: meeting the demand for a variety of report modalities. Proc 8th Annu Symp Comput Appl Med Care. 1984;8:421–4. [Google Scholar]
- 25.Lutz MW, Hammond WE, Stead WW, Blunden PB, Pryor DB. An automated programming system to create medically oriented report generators. Proc 9th Annu Symp Comput Appl Med Care. 1985;9:422–6. [Google Scholar]
- 26.Blunden PB, Ross CC, McCants CB, Hammond WE, Muhlbaier LH. Protocol-driven automated follow-up for a large clinical cardiology database. Proc 8th AAMSI Cong. 1989:135–43.
- 27.Hammond WE, Straube MJ, Blunden PB, Stead WS. Query: the language of databases. Proc 13th Annu Symp Comput Appl Med Care. 1989;13:419–23. [Google Scholar]
- 28.Hammond WE, Stead WW, Straube MJ, Kelly M, Winfree RG. An interface between a hospital information system and a computerized medical record. Proc 4th Annu Symp Comput Appl Med Care. 1980;4(3):1537–40. [Google Scholar]
- 29.Hammond WE, Stead WS. TLS—the laboratory system: a networked patient care system and laboratory care system. Proc 11th Annu Symp Comput Appl Med Care. 1987;11:778–2. [Google Scholar]
- 30.Stead WW, Hammond WE, Winfree RG. Beyond a basic HIS: work stations for department management. Proc 8th Annu Symp Comput Appl Med Care. 1984;8:197–9. [Google Scholar]
- 31.Stead WW, Hammond WE. Functions required to allow TMR to support the information requirements of a hospital. Proc 7th Annu Symp Comput Appl Med Care. 1983;7:106–9. [Google Scholar]
- 32.Stead WS, Pryor DB, Smith PK, Hammond WE. Hospital information systems: a clinician's expectation. In: Bakker AR, Ball MJ, Scherrer JR, Willems JL (eds). Towards New Hospital Information Systems. Proceedings of an IMIA Working Conference (Nijmegen, The Netherlands; May 14–18, 1988). Amsterdam, The Netherlands: Elsevier Science Publishers, 1988:329–36.
- 33.Hammond WE, Stead WS. Bedside terminals: an overview. MD Comput. 1988;5(1):5–6. [PubMed] [Google Scholar]
- 34.Hammond WE, Grewal R, Straube MJ, Stead WW. Networking data sources for intensive care monitoring. Proc 8th AAMSI Cong. 1989:227–81.
- 35.Grewal R, Arcus J, Bowen J, et al. Bedside computerization of the ICU, design issues: benefits of computerization vs. ease of paper and pen. Proc 15th Annu Symp Comput Appl Med Care. 1991;15:793–7. [PMC free article] [PubMed] [Google Scholar]
- 36.Grewal R, Arcus K, Bowen J, et al. Design and development of an automated nursing note. MedInfo. 1992:1054–8.
- 37.Fitzpatrick KT, Satz D, Hammond WE, et al. Automated acuity scoring within a computer-based medical record. Proc 16th Annu Symp Comput Appl Med Care. 1992;16:673–7. [PMC free article] [PubMed] [Google Scholar]
- 38.Garrett LE, Stead WW, Hammond WE. Conversion of manual to total computerized medical records: experience with selected abstraction. SAMS/SCM Joint Annu Conf Comput Ambul Med. 1981:23–5. [DOI] [PubMed]
- 39.Hammond WE, Stead WS. Adopting TMR for physician/nurse use. Proc 15th Annu Symp Comput Appl Med Care. 1991;15:833–7. [PMC free article] [PubMed] [Google Scholar]
- 40.Hammond WE. The impact of a computerized medical record on clinical decision making for nephrology patients. Comput Ambul Med. 1981:29–30.
- 41.Stead WW, Hammond WE. Computerized medical records: a new resource for clinical decision making. J Med Sys. 1983;7:213–20. [DOI] [PubMed] [Google Scholar]
- 42.Garrett LE, Stead WW, Hammond WE. Effect of automated records on provider efficiency. Clin Res. 1982;30:299. [Google Scholar]
- 43.Garrett LE, Hammond WE, Stead WS. The effects of computerized medical records on provider efficiency and quality of care. Methods Inf Med. 1986;5(3):151–7. [PubMed] [Google Scholar]
- 44.Stead WW, Hammond WE. Demand-oriented medical records: toward a physician workstation. Proc 11th Annu Symp Comput Appl Med Care. 1987;11:275–80. [Google Scholar]
- 45.Wilkinson WE, Gehlbach SH, Hammond WE. Using computer-generated feedback to improve physician prescribing. Proc 6th Annu Symp Comput Appl Med Care. 1982;6:76–8. [Google Scholar]
- 46.Gelbach SH, Wilkerson WE, Hammond WE, et al. Improving drug prescribing in a primary care practice. Med Care. 1984;22(3):193–210. [DOI] [PubMed] [Google Scholar]
- 47.Yarnall KSH, Michener JL, Hammond WE. The Medical Record: a comprehensive computer system for the family physician. J Am Bd Fam Pract. 1994;7(4):324–34. [PubMed] [Google Scholar]
- 48.Lundy MS, Hammond WE, Lobach DF. Documenting data delivery: design, deployment and decision. Proc 20th Annu Symp Comput Appl Med Care. 1996;20:807–12. [PMC free article] [PubMed] [Google Scholar]
- 49.Hammond JE, Hammond WE, Stead WS. Information management through integration of distributed resources—the TMR–NLM connection: a prototype. Proc 14th Annu Symp Comput Appl Med Care. 1990;14:719–23. [Google Scholar]
- 50.Jelovsek FR, Smith R, Blackmon L, Hammond WE. Computerized nursery discharge summary. Methods Inf Med. 1977;16(4):199–204. [PubMed] [Google Scholar]
- 51.Jelovsek FR, Burkett E, Deason BP, Hammond WE. A regional maternal–child health telecommunication network. Proc 4th MedInfo. 1983;4:1155–8. [Google Scholar]
- 52.Jelovsek FR, Hammond WE. Formal error rate in computerized obstetrical medical record. Methods Inf Med. 1977;17(3):151–7. [PubMed] [Google Scholar]
- 53.Hage ML, Helms MJ, Hammond WE. Changing rates of ceasarean delivery: the Duke experience 1978–1986. Obstet Gynecol. 1988;72:98–101. [PubMed] [Google Scholar]
- 54.Hage ML, Dudley A, Stead WW, Hammond WE, Neyland C, Hammond CB. Acute childbirth morbidity: its measurement using hospital charges. Am J Obstet Gynecol. 1992;166(6):1853–62. [DOI] [PubMed] [Google Scholar]
- 55.Prather JC, Lobach DF, Hales JW, Hage ML, Hammond WE. Medical data mining: discovery in a clinical data warehouse. Proc 21th Annu Symp Comput Appl Med Care. 1997;21:101–5. [PMC free article] [PubMed] [Google Scholar]
- 56.Stead WS, Hammond WE. Computer–based medical record: the need for storing a single datum in multiple orientations. Proc 12th Annu Symp Comput Appl Med Care. 1988;12:625–9. [Google Scholar]
- 57.Hammond WE, Straube MJ, Stead WS. The synchronization of distributed databases. Proc 14th Annu Symp Comput Appl Med Care. 1990;14:345–9. [Google Scholar]
- 58.Hammond WE, Stead WW, Straube MJ, Hammond WE III. Adapting to the day-to-day growth of TMR. Proc 7th Annu Symp Comput Appl Med Care. 1983;7:101–5. [Google Scholar]
- 59.Dozier JA, Hammond WE, Stead WW. Creating a link between medical and analytical databases. Proc 9th Annu Symp Comput Appl Med Care.1985;9:478–82. [Google Scholar]
- 60.Straube MJ, Hammond WE, Stead WS. Real–time information exchange between heterogeneous database systems; design strategy amd lessons learned during implementation. Proc AAMSI Cong. 1988:202–11.
- 61.Hammond WE. Transferring clinical lab data between independent computer systems. SN Standardization News. 1988:28–30.
- 62.McDonald CJ, Hammond WE. Standard formats for electronic transfer of clinical data. Ann Intern Med. 1989;110(5):333–4. [DOI] [PubMed] [Google Scholar]
- 63.Hammond WE, Stead WW, Straube MJ, Collins JD. Experiences in the development of an ambulatory care medical information system. 3rd USA–JAPAN Comput Conf. 1978:452–6.
- 64.Hammond WE, Stead WW, Straube MJ, Jelovsek FR. A clinical data base management system. Policy Anal Info Sys. 1980;4:91–5. [Google Scholar]
- 65.Hammond WE, Stead WW, Straube MJ, Jelovsek FR. A perinatal database management system for ambulatory care. 1st Int Symp Comput Perinatal Med. 1981:64–5.
- 66.Jelovsek FR, Hammond WE, Deason BP. Use of TMR in a woman's clinic. Proc 6th Annu Symp Comput Appl Med Care. 1982;6:828–31. [Google Scholar]
- 67.Hammond WE, Stead WW, Straube MJ, Jelovsek FR. Functional characteristics of a computerized medical record. Methods Inf Med. 1980;19(3)157–62. [PubMed] [Google Scholar]
- 68.Stead WW, Hammond WE. Calculating storage requirements for office practice systems. Proc 9th Annu Symp Comput Appl Med Care. 1985;9:68–71. [Google Scholar]
- 69.Stead WW, Hammond WE. Storage requirements for office practice systems. Med Elect. 1986;17(6):104–6. [Google Scholar]
- 70.Garrett LE, Stead WW, Hammond WE. A method of handling subjective and physical data; experience with two systems. Proc 6th Annu Symp Comput Appl Med Care. 1982;6:232–235. [Google Scholar]
- 71.Stead WW, Hammond WE, Straube MJ. A chartless record: Is it adequate? Proc 6th Annu Symp Comput Appl Med Care. 1982;6:89–94. [Google Scholar]
- 72.Hammond WE. TMR: profile of an electronic patient record. Proc 7th MedInfo. 1992:730–6.
- 73.Hammond WE. Implementing CPR systems; the pathway to the paperless medical record. 2nd Natl Conf Comput Med Rec. 1993:137–47.
- 74.Hammond WE, Stead WS. TMR: future directions. In: Bakker AR, Ball MJ, Scherrer JR, Willems JL (eds). Towards New Hospital Information Systems. Proceedings of an IMIA Working Conference (Nijmegen, The Netherlands; May 14–18, 1988). Amsterdam, The Netherlands: Elsevier Science Publishers, 1988:97–104.
- 75.Lobach DF, Hammond WE. Development and evaluation of a computer-assisted management protocol (CAMP): improved compliance with care guidelines for diabetes mellitus. Proc 18th Annu Symp Comput Appl Med Care. 1994;18:787–91. [PMC free article] [PubMed] [Google Scholar]
- 76.Lobach DF, Hammond WE. Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am J Med. 1997;102:89–98. [DOI] [PubMed] [Google Scholar]
- 77.Prather JC, Lobach DF, Hales JW, Hage ML, Fehrs SJ, Hammond WE. Converting a legacy system database into a relational format to enhance query efficiency. Proc 19th Annu Symp Comput Appl Med Care. 1995;19:372–376. [PMC free article] [PubMed] [Google Scholar]
- 78.Hammond WE, Hales JW, Lobach DF, Straube MJ. Integration of a computer–based patient record system into the primary care setting. Comput Nurs. 1997;15(2):61–8. [PubMed] [Google Scholar]
- 79.Walter E, Brantley AB, Feagin SJ, Hammond WE. A timeshared operating system for the PDP-11. Decus Proc. 1972:303–8.


