Abstract
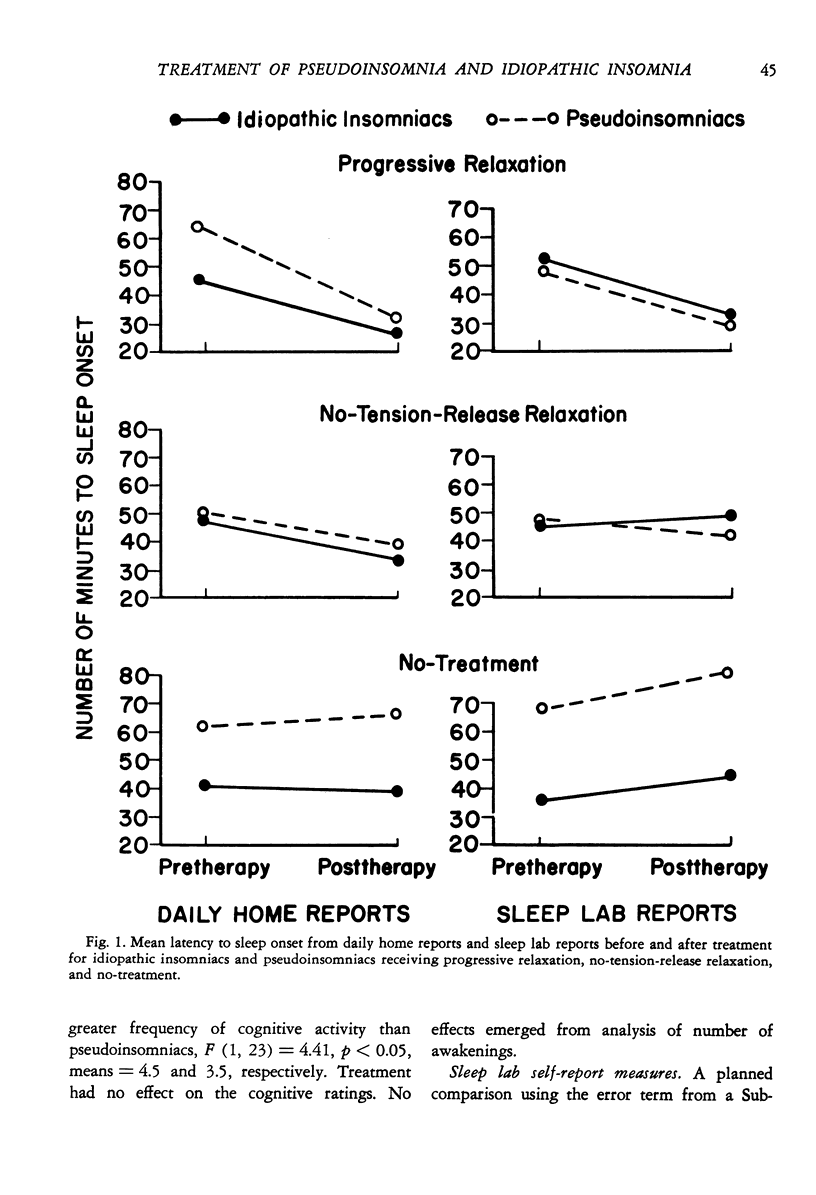
Twenty-nine insomniacs underwent four consecutive sleep laboratory evaluations before and after receiving tension-release relaxation training, no-tension-release relaxation training, or no-treatment. On the basis of the discrepancy between subjective and EEG-defined measures of latency to sleep onset, subjects were classified as pseudoinsomniacs or idiopathic insomniacs. As predicted, tension-release relaxation was significancy more effective than the other two conditions on subjective sleep measures, regardless of insomnia subtype and on objective sleep measures only for idiopathic insomniacs. Subjective improvement was maintained at 12-month followup. Numerous differences between the two subtypes emerged on pretherapy and during-therapy measures distinct from the latency measures, but changes on those variables were unrelated to outcome improvement.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bohlin G. Interaction of arousal and habituation in the development of sleep during monotonous stimulation. Biol Psychol. 1973;1(2):99–114. doi: 10.1016/0301-0511(73)90002-1. [DOI] [PubMed] [Google Scholar]
- Bohlin G. Monotonous stimulation, sleep onset and habituation of the orienting reaction. Electroencephalogr Clin Neurophysiol. 1971 Dec;31(6):593–601. doi: 10.1016/0013-4694(71)90075-7. [DOI] [PubMed] [Google Scholar]
- Borkovec T. D., Grayson J. B., Cooper K. M. Treatment of general tension: subjective and physiological effects of progressive relaxation. J Consult Clin Psychol. 1978 Jun;46(3):518–528. doi: 10.1037//0022-006x.46.3.518. [DOI] [PubMed] [Google Scholar]
- Borkovec T. D., Hennings B. L. The role of physiological attention-focusing in the relaxation treatment of sleep disturbance, general tension, and specific stress reaction. Behav Res Ther. 1978;16(1):7–19. doi: 10.1016/0005-7967(78)90085-2. [DOI] [PubMed] [Google Scholar]
- Borkovec T. D., Weerts T. C. Effects of progressive relaxation on sleep disturbance: an electroencephalographic evaluation. Psychosom Med. 1976 May-Jun;38(3):173–180. doi: 10.1097/00006842-197605000-00003. [DOI] [PubMed] [Google Scholar]
- Carskadon M. A., Dement W. C., Mitler M. M., Guilleminault C., Zarcone V. P., Spiegel R. Self-reports versus sleep laboratory findings in 122 drug-free subjects with complaints of chronic insomnia. Am J Psychiatry. 1976 Dec;133(12):1382–1388. doi: 10.1176/ajp.133.12.1382. [DOI] [PubMed] [Google Scholar]
- Frankel B. L., Patten B. M., Gillin J. C. Restless legs syndrome. Sleep-electroencephalographic and neurologic findings. JAMA. 1974 Dec 2;230(9):1302–1303. doi: 10.1001/jama.230.9.1302. [DOI] [PubMed] [Google Scholar]
- Freedman R., Papsdorf J. D. Biofeedback and progressive relaxation treatment of sleep-onset insomnia: a controlled, all-night investigation. Biofeedback Self Regul. 1976 Sep;1(3):253–271. doi: 10.1007/BF01001167. [DOI] [PubMed] [Google Scholar]
- Good R. Frontalis muscle tension and sleep latency. Psychophysiology. 1975 Jul;12(4):461–467. [PubMed] [Google Scholar]
- Guilleminault C., Eldridge F. L., Dement W. C. Insomnia with sleep apnea: a new syndrome. Science. 1973 Aug 31;181(4102):856–858. doi: 10.1126/science.181.4102.856. [DOI] [PubMed] [Google Scholar]
- Hauri P., Hawkins D. R. Alpha-delta sleep. Electroencephalogr Clin Neurophysiol. 1973 Mar;34(3):233–237. doi: 10.1016/0013-4694(73)90250-2. [DOI] [PubMed] [Google Scholar]
- Haynes S. N., Follingstad D. R., McGowan W. T. Insomnia: sleep patterns and anxiety level. J Psychosom Res. 1974 Apr;18(2):69–74. doi: 10.1016/0022-3999(74)90069-5. [DOI] [PubMed] [Google Scholar]
- Johns M. W., Gay T. J., Masterton J. P., Bruce D. W. Relationship between sleep habits, adrenocortical activity and personality. Psychosom Med. 1971 Nov-Dec;33(6):499–508. doi: 10.1097/00006842-197111000-00003. [DOI] [PubMed] [Google Scholar]
- Kales A., Caldwell A. B., Preston T. A., Healey S., Kales J. D. Personality patterns in insomnia. Theoretical implications. Arch Gen Psychiatry. 1976 Sep;33(9):1128–1124. doi: 10.1001/archpsyc.1976.01770090118013. [DOI] [PubMed] [Google Scholar]
- Karacan I., Salis P. J., Williams R. L. Clinical disorders of sleep. Psychosomatics. 1973 Mar-Apr;14(2):77–88. doi: 10.1016/S0033-3182(73)71360-8. [DOI] [PubMed] [Google Scholar]
- Kazdin A. E., Wilcoxon L. A. Systematic desensitization and nonspecific treatment effects: a methodological evaluation. Psychol Bull. 1976 Sep;83(5):729–758. [PubMed] [Google Scholar]
- Monroe L. J. Psychological and physiological differences between good and poor sleepers. J Abnorm Psychol. 1967 Jun;72(3):255–264. doi: 10.1037/h0024563. [DOI] [PubMed] [Google Scholar]
- Othmer E. Pathophysiologie des gestörten Schlafes und dessen psychopharmakologische Beeinflussung. Arzneimittelforschung. 1966 Feb;16(2):301–304. [PubMed] [Google Scholar]
- Roth T., Kramer M., Lutz T. The nature of insomnia: a descriptive summary of a sleep clinic population. Compr Psychiatry. 1976 Jan-Feb;17(1):217–220. doi: 10.1016/0010-440x(76)90072-9. [DOI] [PubMed] [Google Scholar]
- Scharf M. B., Kales A., Bixler E. O. Readaptation to the sleep laboratory in insomniac subjects. Psychophysiology. 1975 Jul;12(4):412–415. doi: 10.1111/j.1469-8986.1975.tb00013.x. [DOI] [PubMed] [Google Scholar]
- Starker S., Hasenfeld R. Daydream styles and sleep disturbance. J Nerv Ment Dis. 1976 Dec;L63(6):391–400. doi: 10.1097/00005053-197612000-00002. [DOI] [PubMed] [Google Scholar]
- Steinmark S. W., Borkovec T. D. Active and placebo treatment effects on moderate insomnia under counterdemand and positive demand instructions. J Abnorm Psychol. 1974 Apr;83(2):157–163. doi: 10.1037/h0036489. [DOI] [PubMed] [Google Scholar]



