Abstract
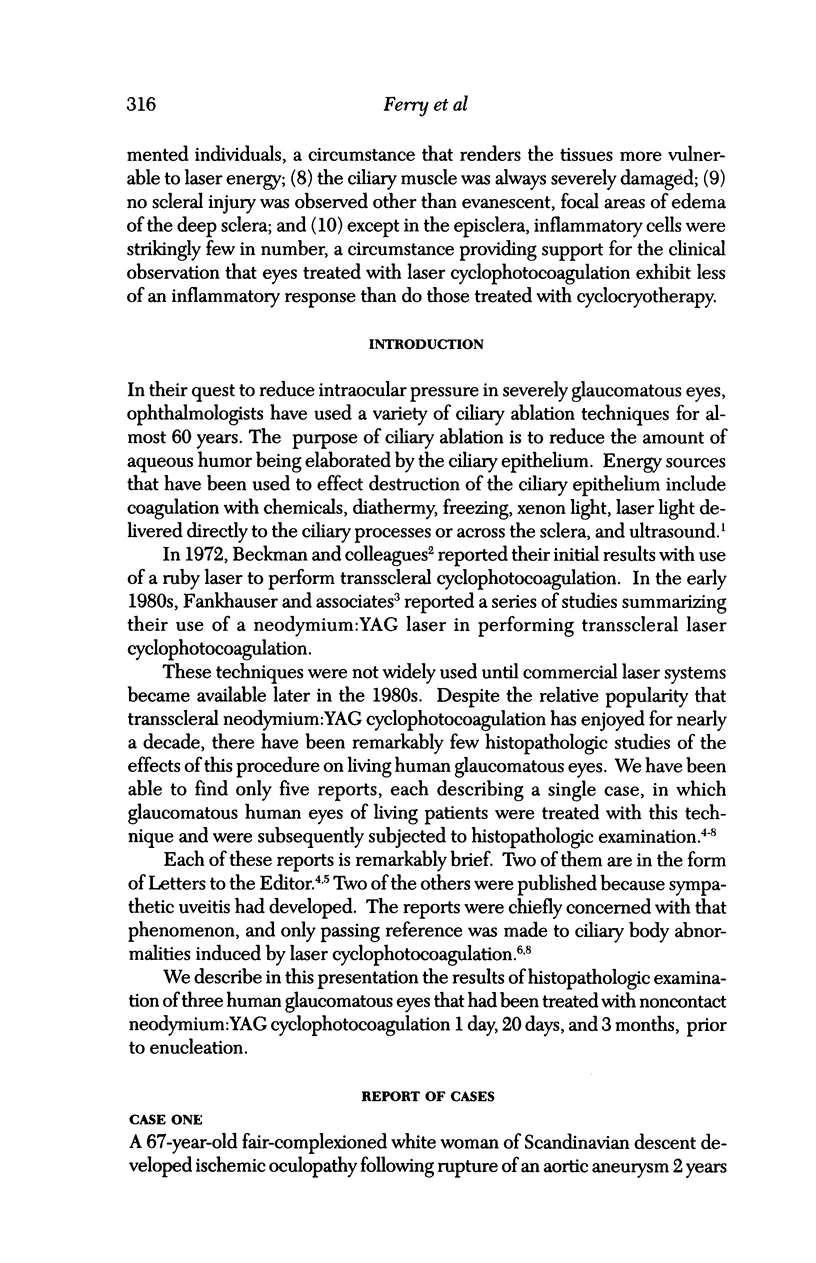
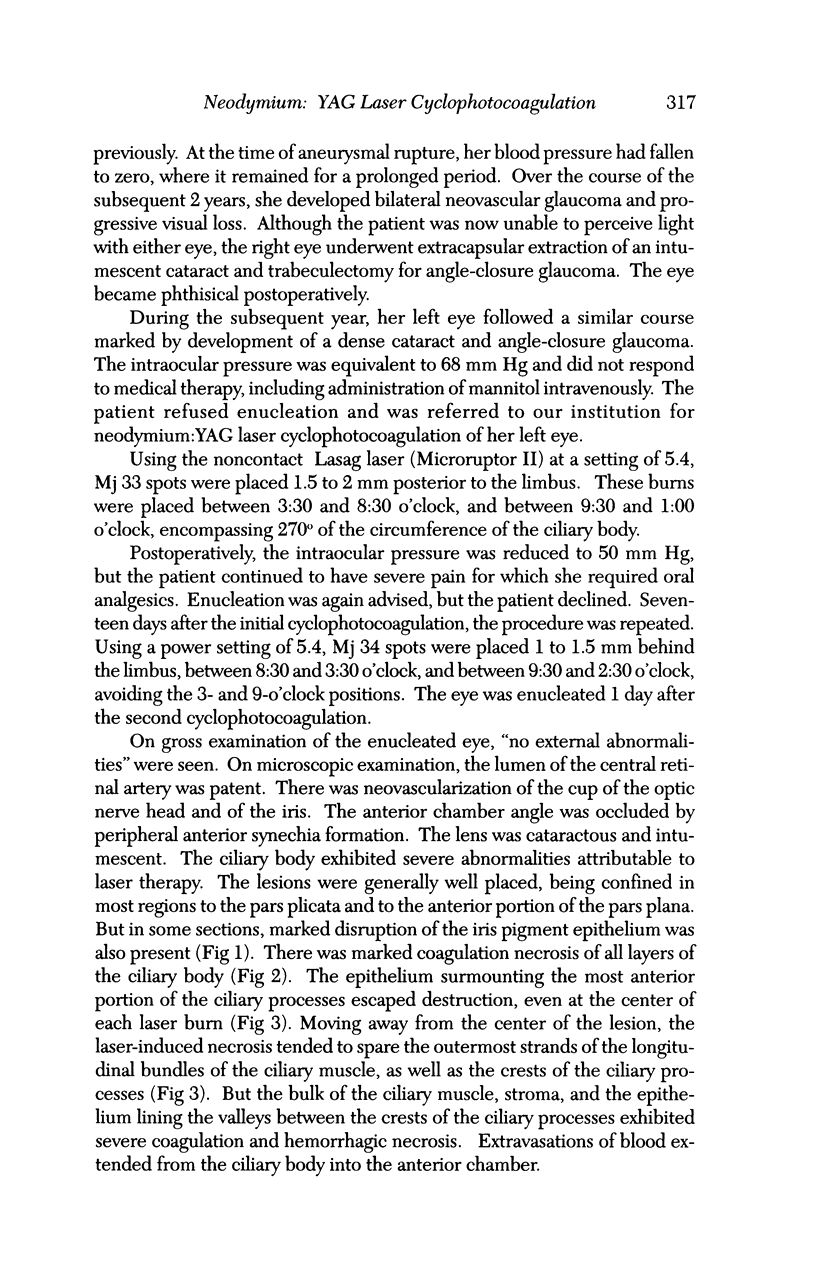
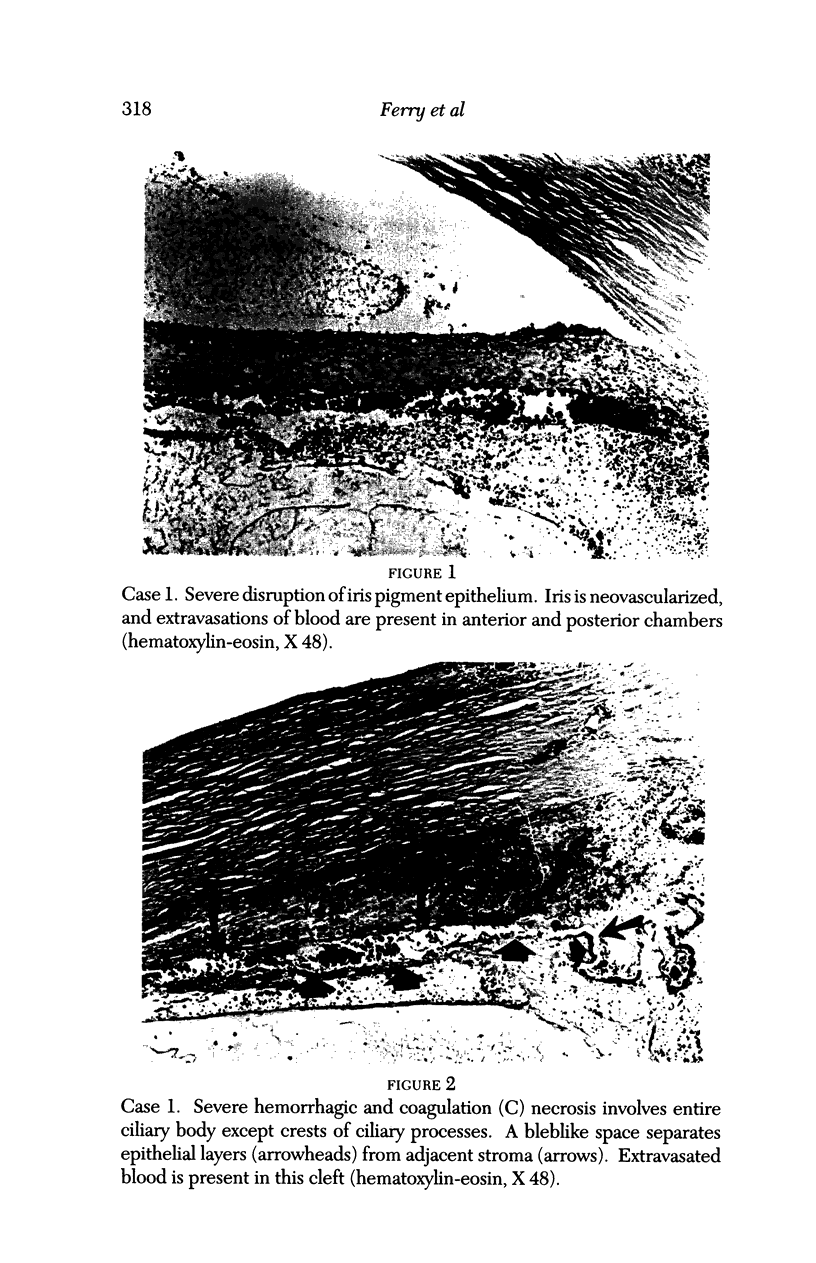
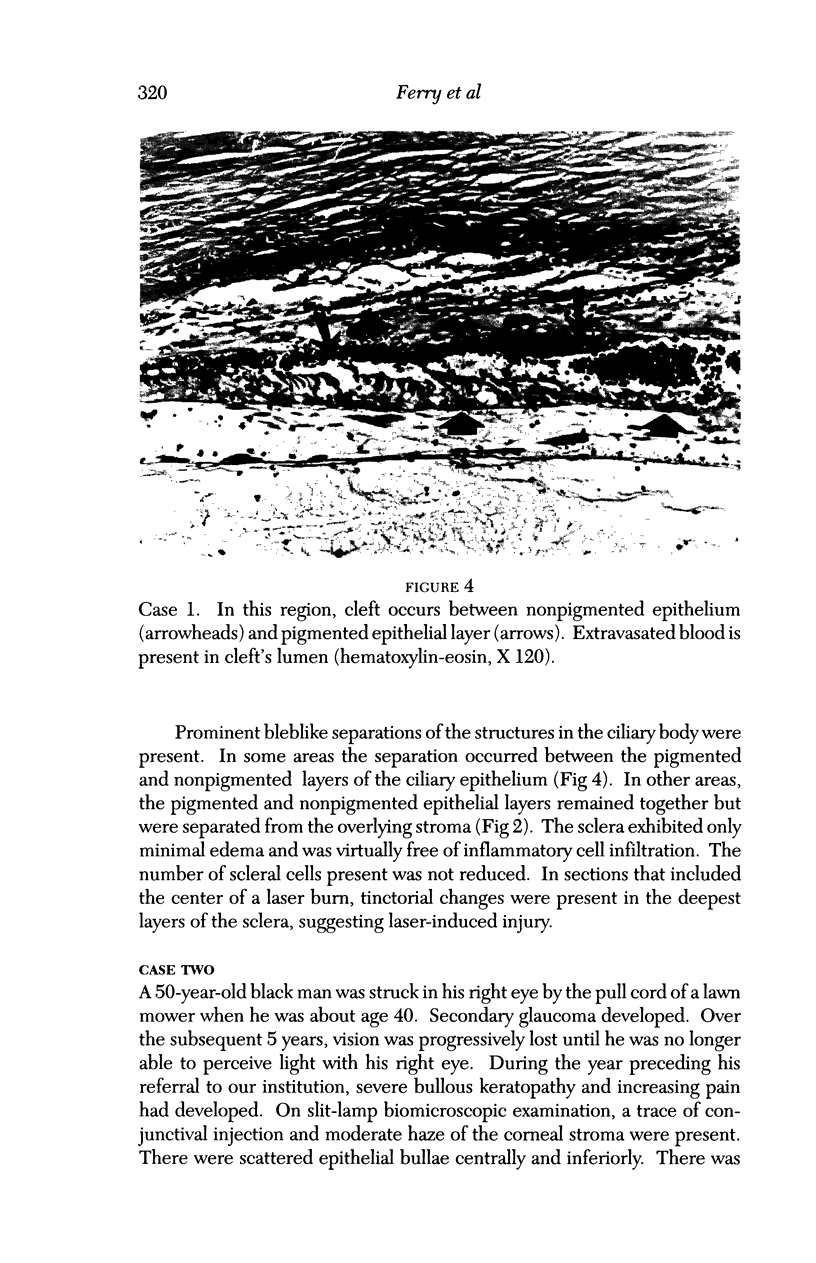
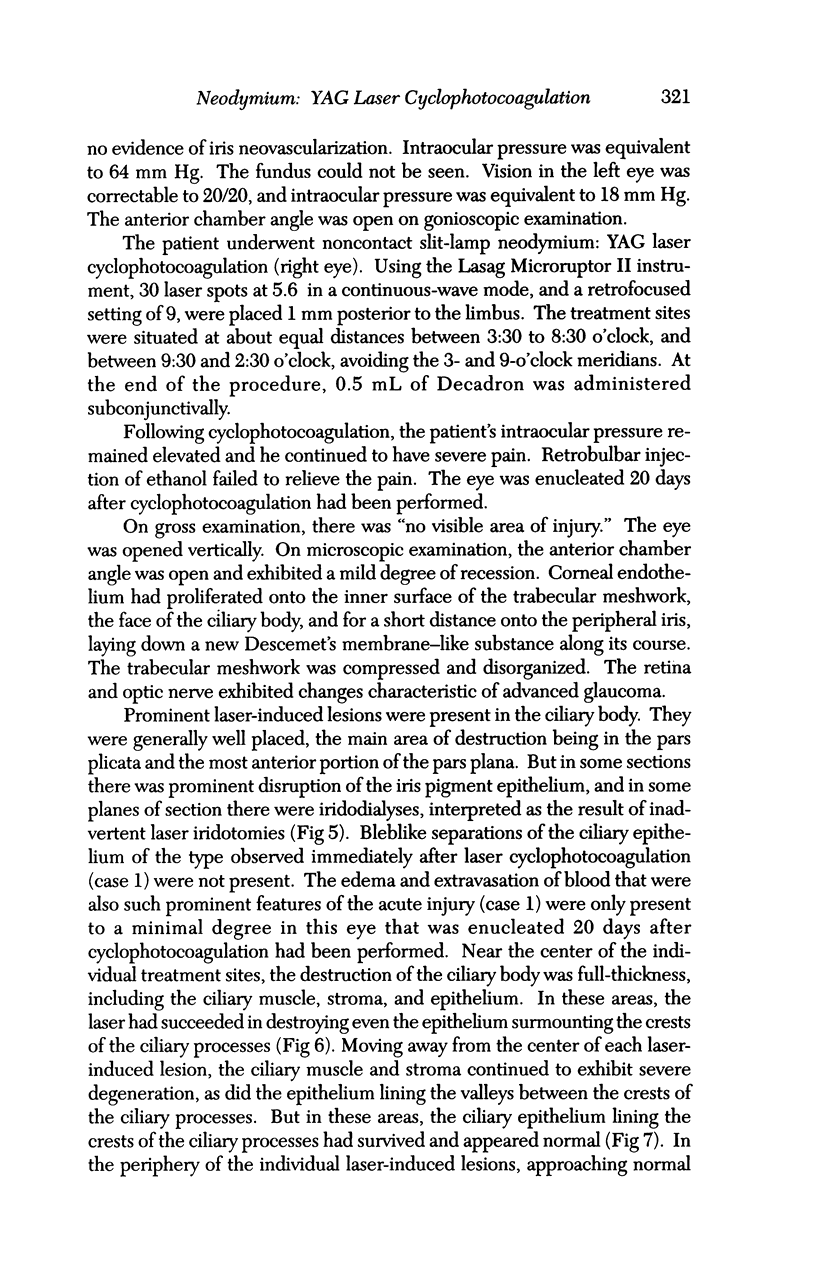
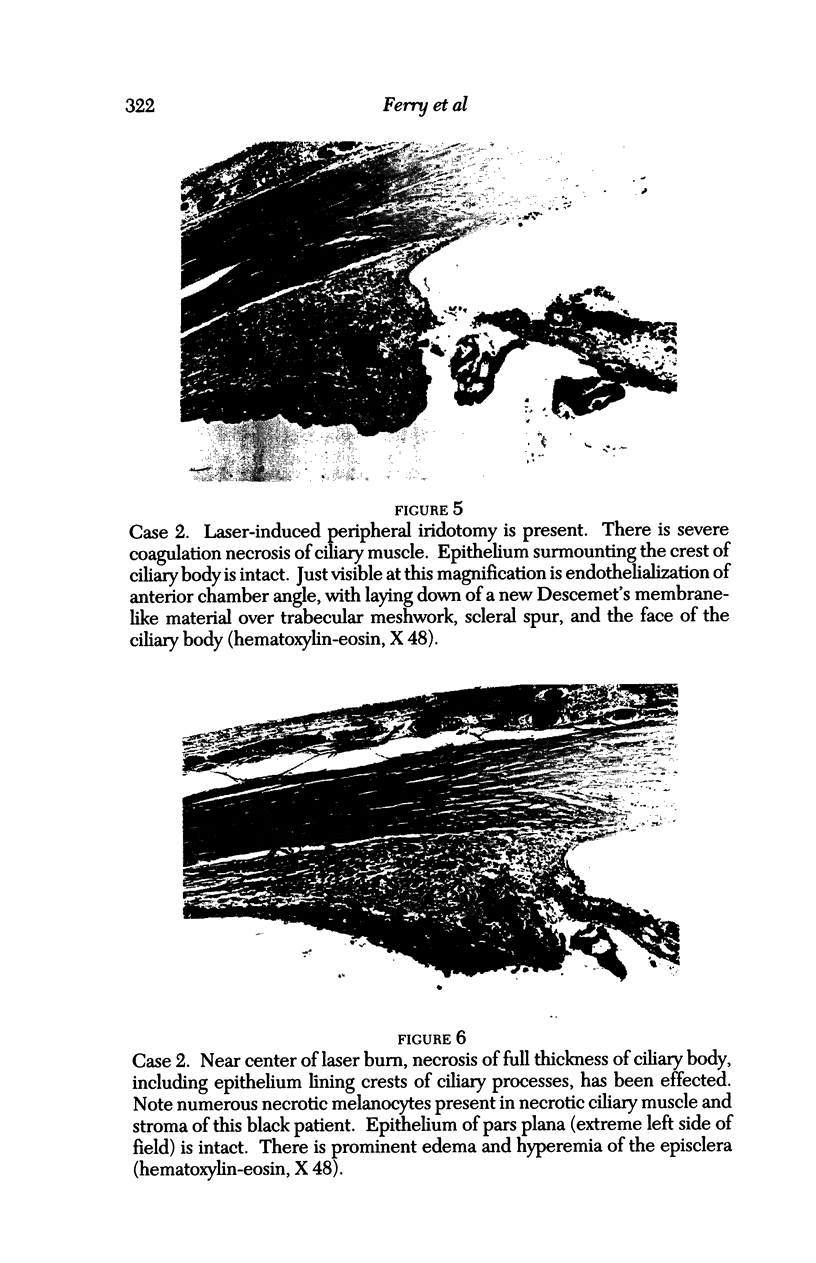
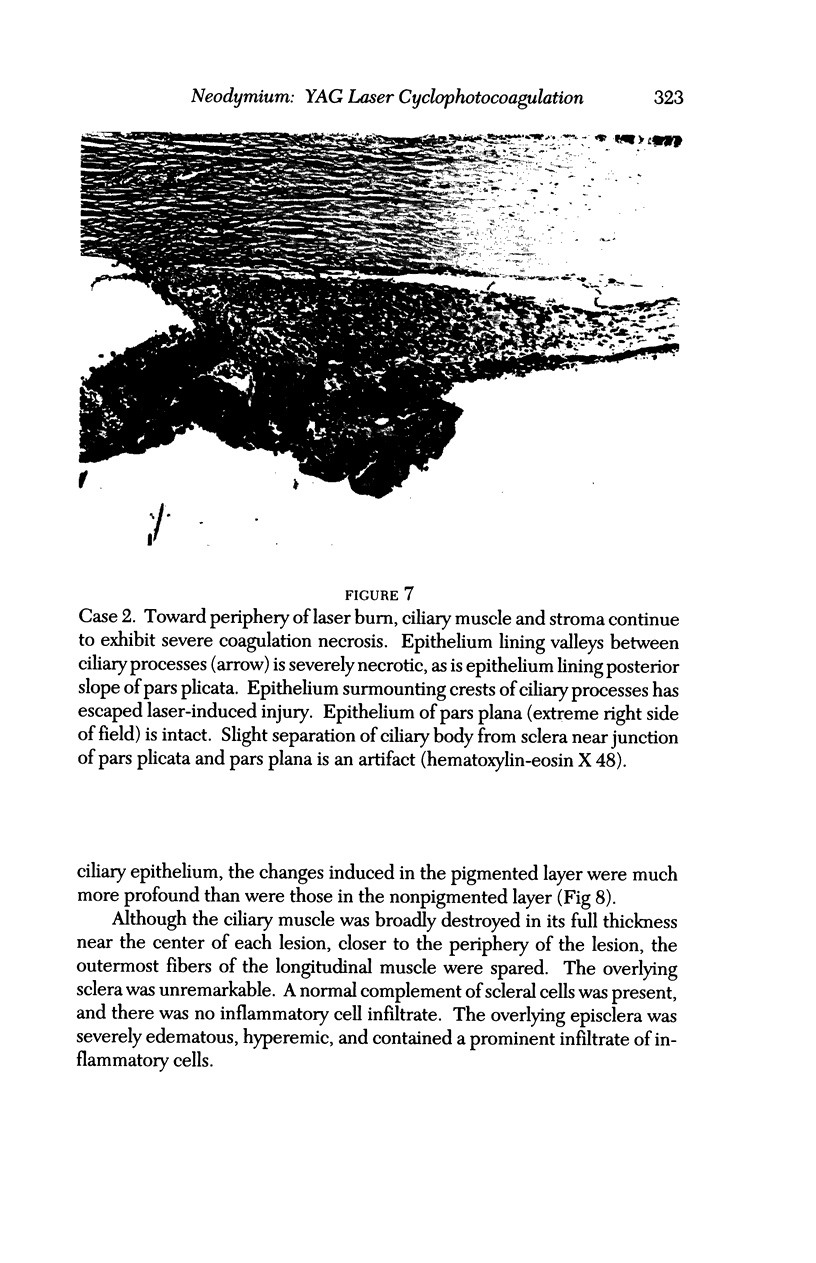
PURPOSE: Although Nd:YAG laser cyclophotocoagulation has been extensively used for nearly a decade in treatment of severe glaucoma, there have been remarkably few reports (each of them extremely brief) of histopathological examination of glancomatous human eyes that had been so treated. We undertook this study to provide further details regarding the nature of the lesions produced in this type of ciliary ablation. METHODS: We chose three representative cases in which a glaucomatous human eye had been subjected to Nd: YAG cyclophotocoagulation, and was subsequently enucleated. To better understand the temporal evolution of the lesions, we selected eyes that were enucleated 1 day, 20 days, and 3 months, respectively, after they had been treated with noncontact Nd: YAG laser cyclophotocoagulation. RESULTS AND CONCLUSIONS: (1) energy levels ranging from 4.4 Joules to 5.6 Joules were effective in producing appropriate lesions; (2) direction of the laser beam 1 to 1.5 mm behind the limbus caused severe destructive lesions of the pars plicata: (3) toward the periphery of the individual treatment sites, the stroma and ciliary muscle continued to exhibit severe degeneration, as did the epithelium lining the valleys between the crests of the ciliary processes; but in those peripheral zones of individual treatment sites, the epithelium lining the crests of the ciliary processes survived and appears normal; (4) bleb-like separations of the ciliary epithelium from the adjacent stroma, particularly along the posterior aspect of the ciliary body lesions, are a prominent early feature of Nd:YAG cyclophotocoagulation; (5) the pigmented epithelium is more vulnerable to laser energy than is the nonpigmented epithelium of the ciliary body; (6) the destruction of the ciliary epithelium is permanent; (7) deeply pigmented persons have more melanocytes in the ciliary body muscle and stroma than do more lightly pigmented individuals, a circumstance that renders the tissues more vulnerable to laser energy; (8) the ciliary muscle was always severely damaged; (9) no scleral injury was observed other than evanescent, focal areas of edema of the deep sclera; and (10) except in the episclera, inflammatory cells were strikingly few in number, a circumstance providing support for the clinical observation that eyes treated with laser cyclophotocoagulation exhibit less of an inflammatory response than do those treated with cyclocryotherapy.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allingham R. R., de Kater A. W., Bellows A. R., Hsu J. Probe placement and power levels in contact transscleral neodymium:YAG cyclophotocoagulation. Arch Ophthalmol. 1990 May;108(5):738–742. doi: 10.1001/archopht.1990.01070070124049. [DOI] [PubMed] [Google Scholar]
- Assia E. I., Hennis H. L., Stewart W. C., Legler U. F., Carlson A. N., Apple D. J. A comparison of neodymium: yttrium aluminum garnet and diode laser transscleral cyclophotocoagulation and cyclocryotherapy. Invest Ophthalmol Vis Sci. 1991 Sep;32(10):2774–2778. [PubMed] [Google Scholar]
- Bechrakis N. E., Müller-Stolzenburg N. W., Helbig H., Foerster M. H. Sympathetic ophthalmia following laser cyclocoagulation. Arch Ophthalmol. 1994 Jan;112(1):80–84. doi: 10.1001/archopht.1994.01090130090024. [DOI] [PubMed] [Google Scholar]
- Bechrakis N. E., Müller-Stolzenburg N. W., Helbig H., Foerster M. H. Sympathetic ophthalmia following laser cyclocoagulation. Arch Ophthalmol. 1994 Jan;112(1):80–84. doi: 10.1001/archopht.1994.01090130090024. [DOI] [PubMed] [Google Scholar]
- Beckman H., Kinoshita A., Rota A. N., Sugar H. S. Transscleral ruby laser irradiation of the ciliary body in the treatment of intractable glaucoma. Trans Am Acad Ophthalmol Otolaryngol. 1972 Mar-Apr;76(2):423–436. [PubMed] [Google Scholar]
- Blasini M., Simmons R., Shields M. B. Early tissue response to transscleral neodymium: YAG cyclophotocoagulation. Invest Ophthalmol Vis Sci. 1990 Jun;31(6):1114–1118. [PubMed] [Google Scholar]
- Blasini M., Simmons R., Shields M. B. Early tissue response to transscleral neodymium: YAG cyclophotocoagulation. Invest Ophthalmol Vis Sci. 1990 Jun;31(6):1114–1118. [PubMed] [Google Scholar]
- Brancato R., Leoni G., Trabucchi G., Cappellini A. Probe placement and energy levels in continuous wave neodymium-YAG contact transscleral cyclophotocoagulation. Arch Ophthalmol. 1990 May;108(5):679–683. doi: 10.1001/archopht.1990.01070070065036. [DOI] [PubMed] [Google Scholar]
- Brown S. V., Higginbotham E., Tessler H. Sympathetic ophthalmia following Nd:YAG cyclotherapy. Ophthalmic Surg. 1990 Oct;21(10):736–737. [PubMed] [Google Scholar]
- Coleman A. L., Jampel H. D., Javitt J. C., Brown A. E., Quigley H. A. Transscleral cyclophotocoagulation of human autopsy and monkey eyes. Ophthalmic Surg. 1991 Nov;22(11):638–643. [PubMed] [Google Scholar]
- Devenyi R. G., Trope G. E., Hunter W. H., Badeeb O. Neodymium: YAG transscleral cyclocoagulation in human eyes. Ophthalmology. 1987 Dec;94(12):1519–1522. doi: 10.1016/s0161-6420(87)33252-x. [DOI] [PubMed] [Google Scholar]
- Duy T. P., Seiler T., Wollensak J. Anderung der Abflussleichtigkeit nach Zyklokryokoagulation bei primärem Glaukom. Eine tonographische Studie. Klin Monbl Augenheilkd. 1987 Feb;190(2):99–102. doi: 10.1055/s-2008-1050336. [DOI] [PubMed] [Google Scholar]
- Edward D. P., Brown S. V., Higginbotham E., Jennings T., Tessler H. H., Tso M. O. Sympathetic ophthalmia following neodymium:YAG cyclotherapy. Ophthalmic Surg. 1989 Aug;20(8):544–546. [PubMed] [Google Scholar]
- Edward D. P., Brown S. V., Higginbotham E., Jennings T., Tessler H. H., Tso M. O. Sympathetic ophthalmia following neodymium:YAG cyclotherapy. Ophthalmic Surg. 1989 Aug;20(8):544–546. [PubMed] [Google Scholar]
- Fankhauser F., van der Zypen E., Kwasniewska S., Rol P., England C. Transscleral cyclophotocoagulation using a neodymium YAG laser. Ophthalmic Surg. 1986 Feb;17(2):94–100. [PubMed] [Google Scholar]
- Ferry A. P. Histopathologic observations on human eyes following cyclocryotherapy for glaucoma. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977 Jan-Feb;83(1):90–113. [PubMed] [Google Scholar]
- Ferry A. P. Histopathologic observations on human eyes following cyclocryotherapy for glaucoma. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977 Jan-Feb;83(1):90–113. [PubMed] [Google Scholar]
- Gaasterland D. E., Pollack I. P. Initial experience with a new method of laser transscleral cyclophotocoagulation for ciliary ablation in severe glaucoma. Trans Am Ophthalmol Soc. 1992;90:225–246. [PMC free article] [PubMed] [Google Scholar]
- Hampton C., Shields M. B. Transscleral neodymium-YAG cyclophotocoagulation. A histologic study of human autopsy eyes. Arch Ophthalmol. 1988 Aug;106(8):1121–1123. doi: 10.1001/archopht.1988.01060140277041. [DOI] [PubMed] [Google Scholar]
- Lam S., Tessler H. H., Lam B. L., Wilensky J. T. High incidence of sympathetic ophthalmia after contact and noncontact neodymium:YAG cyclotherapy. Ophthalmology. 1992 Dec;99(12):1818–1822. doi: 10.1016/s0161-6420(92)31719-1. [DOI] [PubMed] [Google Scholar]
- March W. F., Shaver R. P. Histologic effects of cyclophotocoagulation. Ophthalmology. 1989 Jun;96(6):925–925. doi: 10.1016/s0161-6420(89)32805-3. [DOI] [PubMed] [Google Scholar]
- March W. F., Shaver R. P. Histologic effects of cyclophotocoagulation. Ophthalmology. 1989 Jun;96(6):925–925. doi: 10.1016/s0161-6420(89)32805-3. [DOI] [PubMed] [Google Scholar]
- Marsh P., Wilson D. J., Samples J. R., Morrison J. C. A clinicopathologic correlative study of noncontact transscleral Nd:YAG cyclophotocoagulation. Am J Ophthalmol. 1993 May 15;115(5):597–602. doi: 10.1016/s0002-9394(14)71456-4. [DOI] [PubMed] [Google Scholar]
- Pavlin C. J., Macken P., Trope G. E., Heathcote G., Sherar M., Harasiewicz K., Foster F. S. Ultrasound biomicroscopic imaging of the effects of YAG laser cycloablation in postmortem eyes and living patients. Ophthalmology. 1995 Feb;102(2):334–341. doi: 10.1016/s0161-6420(95)31020-2. [DOI] [PubMed] [Google Scholar]
- Schubert H. D., Federman J. L. The role of inflammation in CW Nd:YAG contact transscleral photocoagulation and cryopexy. Invest Ophthalmol Vis Sci. 1989 Mar;30(3):543–549. [PubMed] [Google Scholar]
- Schubert H. D. Noncontact and contact pars plana transscleral neodymium: YAG laser cyclophotocoagulation in postmortem eyes. Ophthalmology. 1989 Oct;96(10):1471–1475. doi: 10.1016/s0161-6420(89)32702-3. [DOI] [PubMed] [Google Scholar]
- Schubert H. D. Noncontact and contact pars plana transscleral neodymium: YAG laser cyclophotocoagulation in postmortem eyes. Ophthalmology. 1989 Oct;96(10):1471–1475. doi: 10.1016/s0161-6420(89)32702-3. [DOI] [PubMed] [Google Scholar]
- Shields M. B., Shields S. E. Noncontact transscleral Nd:YAG cyclophotocoagulation: a long-term follow-up of 500 patients. Trans Am Ophthalmol Soc. 1994;92:271–287. [PMC free article] [PubMed] [Google Scholar]
- Shields S. M., Stevens J. L., Kass M. A., Smith M. E. Histopathologic findings after Nd:YAG transscleral cyclophotocoagulation. Am J Ophthalmol. 1988 Jul 15;106(1):100–101. doi: 10.1016/s0002-9394(14)76401-3. [DOI] [PubMed] [Google Scholar]
- Simmons R. B., Prum B. E., Jr, Shields S. R., Echelman D. A., Shields M. B. Videographic and histologic comparison of Nd:YAG and diode laser contact transscleral cyclophotocoagulation. Am J Ophthalmol. 1994 Mar 15;117(3):337–341. doi: 10.1016/s0002-9394(14)73142-3. [DOI] [PubMed] [Google Scholar]
- Stewart R. H., Garcia C. A. Staphloma following cyclocryotherapy. Ophthalmic Surg. 1974 Spring;5(1):28–29. [PubMed] [Google Scholar]