Abstract
Objective To carry out an economic evaluation of a general practitioner with special interest service for non-urgent skin problems compared with hospital outpatient care.
Design Cost effectiveness analysis and cost consequences analysis alongside a randomised controlled trial.
Setting General practitioner with special interest dermatology service covering 29 general practices in Bristol.
Participants Adults referred to a hospital dermatology clinic who were potentially suitable for management by a general practitioner with special interest.
Interventions Participants were randomised 2:1 to receive either care by general practitioner with special interest service or usual hospital outpatient care.
Main outcome measures Costs to NHS, patients, and companions, and costs of lost production. Cost effectiveness, using the two primary outcomes of dermatology life quality index scores and improved patient perceived access, was assessed by incremental cost effectiveness ratios and cost effectiveness acceptability curves. Cost consequences are presented in relation to all costs and both primary and secondary outcomes from the trial.
Results Costs to the NHS for patients attending the general practitioner with special interest service were £208 ($361; euro 308) compared with £118 for hospital outpatient care. Based on analysis with imputation of missing data, costs to patients and companions were £48 and £51, respectively; costs of lost production were £27 and £34, respectively. The incremental cost effectiveness ratios for general practitioner with special interest care over outpatient care were £540 per one point gain in the dermatology life quality index and £66 per 10 point change in the access scale.
Conclusions The general practitioner with special interest service for dermatology is more costly than hospital outpatient care, but this additional cost needs to be weighed against improved access and broadly similar health outcomes.
Introduction
General practitioners with special interests have been defined as general practitioners who supplement their generalist role by delivering high quality, improved access to services. They do not provide the same breadth of clinical care as a consultant led service but the intention is that they should provide care of equivalent quality and outcome.1 Dermatology is one area in which general practitioner with special interest services are being developed, but there is little evidence about the cost effectiveness of any such services compared with standard hospital outpatient care.2,3 Some evidence exists that an outreach model of care where consultant dermatologists hold clinics in general practice surgeries is more costly,4,5 and some evidence suggests that general practitioner with special interest diabetic clinics in Bradford incurred broadly similar costs to those of hospital clinics.6 Estimating cost effectiveness for general practitioner with special interest services provides something of a challenge given that the purpose of these services is largely related to improving access rather than to improving clinical outcomes. The estimation of, for example, a cost per quality adjusted life year (QALY) gained is therefore unlikely to be helpful in making decisions about the relative cost effectiveness of these services.
We compared the costs and cost effectiveness of a general practitioner with special interest service in dermatology with routine hospital outpatient care, taking into account the need to consider access as an important outcome of the service. General practitioner with special interest care is intended to treat patients who would otherwise be seen in a hospital setting, making the routine hospital outpatient service the appropriate comparator.
Methods
Our study was carried out in parallel with a randomised controlled trial assessing the effectiveness, accessibility, and acceptability of a general practitioner with special interest dermatology service compared with routine hospital outpatient care, for patients with non-urgent skin conditions.7 Effectiveness data were obtained from the associated randomised trial.
Our economic evaluation was carried out in two forms. Firstly, we used cost effectiveness analyses to compare costs from an NHS perspective with the two primary outcomes from the trial: change in the dermatology life quality index (scored from 0 to 30, with a lower score representing a better quality of life; standard deviation of change in the score for all patients 4.49) and accessibility of care (based on three questions concerning access and scored from 0 to 100; standard deviation of score at follow-up for all patients 19.8). These cost effectiveness analyses allow comparison of cost data with a single outcome. Secondly, we used a cost consequences analysis8 to compare costs from several perspectives (NHS, patient, and companion, and lost production to society) with both primary and secondary outcomes, where secondary outcomes additionally included patient satisfaction with the consultation, satisfaction with facilities, attendance rates, and waiting times. Such presentation of data allows decision makers to compare a broad set of outcomes with information on cost. Information about lost production is provided because the potentially different access to the two services may affect the time required to attend appointments, and thus the extent to which production is lost.
Collection and valuation of resource use data
We collected data on use of resources for all patients enrolled in the trial for nine months after randomisation. Most data on use of NHS resources were obtained from computerised systems in the hospital, general practitioner with special interest service, and general practice surgeries. Data included information about numbers and types of consultations (including hospital, general practitioner with special interest, general practitioner, and district nurse), investigations and procedures carried out, and drugs prescribed for the skin condition. These data were collected using computerised data collection forms on a per patient basis at the end of the follow-up period. Additional NHS data came from two sources: detailed time and motion studies carried out to obtain information about the time spent with patients with non-urgent conditions in the hospital outpatient setting; and inquiring of nurses about consumables used during procedures.
Information about the resources used by patients and their companions was obtained from questionnaires administered six weeks after the first appointment and at nine months after randomisation. Information collected included over the counter drugs, use of non-NHS practitioners, travel, care of dependants during consultations, and unpaid time off work.
We obtained information about lost production (time off work to attend appointments) from the patient questionnaires and linked this with information about the number of appointments attended.
We then applied unit costs including VAT in 2004 sterling prices from UK sources (table 1). Consultations with general practitioners with special interest were valued using information about the time spent on the service by the relevant practitioners and their salary costs, administrative time and costs, overheads, and consultant clinical support for two sessions per week. Hospital consultations were valued using information from the time and motion study about the time spent on consultations with patients suitable for the service, salary costs, administrative time and costs, and overheads.
Table 1.
Resources measured, source of unit cost data, and unit costs applied
| Resource (source) | Unit cost (£) |
|---|---|
| Hospital consultations* | 47.15 |
| General practitioner with special interest service*: | |
| General practitioner consultation | 78.49 |
| Nurse consultation | 72.48 |
| General practitioner at doctor's surgery† | 19.00 |
| Home visit by general practitione† | 59.00 |
| Practice nurse at doctor's surgery† | 9.00 |
| Home visit by district nurse† | 20.00 |
| Tests‡ | |
| Biochemistry | 2.85 |
| Haematology | 3.00 |
| Histopathology | 44.41 |
| Immunology | 15.00 |
| Microbiology | 13.90 |
| Mycology | 22.75 |
| Patch test | 9.71 |
| Radiology | 15.00 |
| Skin prick test | 9.71 |
| Virology | 10.15 |
| Investigations and treatments§ | |
| PUVA course (hospital outpatient clinic) | 101.97 |
| Excision or incisional biopsy | |
| General practitioner with special interest | 16.44 |
| Hospital outpatient clinic | 15.80 |
| Punch biopsy | |
| General practioner with special interest | 15.92 |
| Hospital outpatient clinic | 15.80 |
| Curettage and cautery | |
| General practitioner with special interest | 19.85 |
| Hospital outpatient clinic | 5.19 |
| Triamcinolone acetonide injection (service and clinic) | 1.70 |
| Hosiery (service and clinic)§ | 2.12 |
| Prescribed drugs¶ | Variable |
| Over the counter drugs** | Variable |
| Private health practitioners** | Variable |
| Fares** | Variable |
| Parking charges** | Variable |
| Car travel (per mile)†† | 0.41 |
| Absence from work (per hour lost)§§ | 11.56 |
PUVA=psoralens plus long wave ultraviolet radiation.
Calculated from hospital and general practitioner with special interest finance data, detailed time and motion studies, and national information.9
Curtis and Netten9
Hospital department.
Values are for additional cost of procedure over and above consultation cost. For general practitioner with special interest, calculated from consumables used using NHS logistics; for hospital, obtained from hospital finance departments.
British National Formulary.
As reported by patients.
Automobile Association.
New earnings survey for city of Bristol.
Discounting was not required given that all effects of the service were expected to be noted within a one year period.
Statistical analysis
Where possible we present data on both resource use and costs. For some items of resource (for example, drugs, methods of travel) the variety of different types means that only cost data can be presented in an interpretable way. Data are reported as means; standard deviations are presented for resource use only. Data were analysed using Stata release 9.0.
Data on use of NHS resources were complete, but data were missing from the questionnaires that provided information on costs to the patient and companion, and lost production costs. Missing data arose from several sources: not attending the allocated appointment so failing to complete one of the questionnaires; withdrawal from the study; failure to fully complete questionnaires; and failure to complete particular items within a questionnaire. Given that some of these reasons, particularly the first, suggest that data are not missing completely at random, we present data both with and without imputation. We carried out imputation of data separately for patient and companion costs and for costs of lost production, based on models containing age, sex, and all elements of the relevant cost category and using the multiple imputation by chained equation procedure (mvis) in Stata.
The primary outcome measures (dermatology life quality index, access score) were combined with mean NHS costs to estimate incremental cost effectiveness ratios. These represent the additional cost per additional dermatology life quality index point gained and the additional cost per additional 10 point increase on the access scale. Uncertainty was represented through the use of cost effectiveness acceptability curves obtained using bootstrapped data. These curves show the probability that the use of the general practitioner with special interest service is cost effective compared with the outpatient appointment for a range of values that the decision maker might be willing to pay. Given that these curves depend on the decision maker's willingness to pay for improved outcomes and the decision maker's budget constraints, we include only NHS costs in these analyses.
Sensitivity analyses
The statistical analyses account for uncertainty surrounding the data collection. We used sensitivity analysis to account for structural uncertainties of which there are two of concern. Firstly, whether the longer waiting period for a hospital appointment would result in resource use within the hospital arm of the trial taking place later than that within the general practitioner with special interest arm. For this reason, we also collected data on use of NHS resources for 12 months from the date of randomisation; results for this extended time period are presented in the first sensitivity analysis.
Secondly, there was concern that the scheme was under-utilised during this trial with a consequent influence on unit costs. Overall, 22% of appointments were unfilled; costs assuming that these appointments were filled were used in the second sensitivity analysis (£60.05 for an appointment with a general practitioner with special interest; £55.28 for an appointment with a nurse).
Results
Overall, 556 adult patients with non-urgent skin problems were randomised: 354 to care by a general practitioner with special interest and 202 to hospital outpatient care.
Resource use and costs
Table 2 presents the results of use of physical resources associated with each form of care. The total numbers of consultations for patients in the two arms of the trial were broadly similar. Table 3 shows the mean cost per patient achieved by combining NHS resource use with information on valuation. Despite the similar number of consultations, the costs associated with patients treated by a general practitioner with special interest were higher than for those treated as hospital outpatients. Adding in the costs of consultations in primary care, investigation, treatment, and drugs increased this difference, and the total NHS costs associated with general practitioner with special interest care are about 75% higher than those associated with hospital outpatient care. Table 4 shows costs associated with patient and companion resource use as well as costs of lost production, using data both with and without imputation. Using both forms of estimation, patient and companion costs, and costs of lost production are higher for the hospital arm, but the difference is smaller for the imputed patient and companion costs than for the estimate made without imputation. These costs are of a lower order than those facing the NHS.
Table 2.
Means (SD) for resource use for nine months after randomisation to general practitioner with special interest care or hospital outpatient care for non-urgent skin problems
| Resource item | General practitioner with special interest group (n=354) | Hospital outpatient group (n=202) |
|---|---|---|
| NHS resource use | ||
| Hospital consultations: | ||
| Doctor | 0.175 (0.551) | 1.42 (1.04) |
| Nurse | 0.0565 (0.286) | 0.0841 (0.342) |
| General practitioner with special interests consultation: | ||
| General practitioner | 1.54 (1.29) | 0 |
| Nurse | 0.155 (0.707) | 0 |
| General practice surgery | 0.726 (1.521) | 0.629 (1.268) |
| Home visit by district nurse | 0.00282 (0.0532) | 0 |
| Surgery visit to practice nurse | 0.316 (2.756) | 0.188 (0.989) |
| Home visit by district nurse | 0.00847 (0.159) | 0 |
| Investigations: | ||
| Biochemistry | 0.0198 (0.139) | 0.0495 (0.278) |
| Haematology | 0.107 (0.353) | 0.0396 (0.196) |
| Histopathology | 0.172 (0.393) | 0.109 (0.312) |
| Immunology | 0.00282 (0.0532) | 0.00495 (0.0704) |
| Microbiology | 0.00565 (0.0751) | 0.0198 (0.140) |
| Mycology | 0.0226 (0.149) | 0.0297 (0.1702) |
| Patch test | 0.0960 (0.540) | 0.139 (0.631) |
| Radiology | 0.00847 (0.0918) | 0.00495 (0.0704) |
| Skin prick test | 0.0282 (0.197) | 0 |
| Virology | 0 | 0.00495 (0.0704) |
| Treatments: | ||
| PUVA course: | ||
| Provided by general practitioner with special interests | 0 | 0 |
| Provided by hospital | 0.0169 (0.184) | 0.00495 (0.0704) |
| Excision: | ||
| Provided by general practitioner with special interests | 0.0621 (0.253) | 0 |
| Provided by hospital | 0 | 0.0347 (0.183) |
| Incisional biopsy: | ||
| Provided by general practitioner with special interests | 0.0339 (0.1962) | 0 |
| Provided by hospital | 0.0141 (0.1182) | 0.00990 (0.0993) |
| Punch biopsy: | ||
| Provided by general practitioner with special interests | 0.0621 (0.2418) | 0 |
| Provided by hospital | 0.00282 (0.0532) | 0.0347 (0.183) |
| Curettage and cautery: | ||
| Provided by general practitioner with special interests | 0.0508 (0.2325) | 0 |
| Provided by hospital | 0 | 0.0545 (0.228) |
| Triamcinolone acetonide injection: | ||
| Provided by general practitioner with special interests | 0.0141 (0.219) | 0 |
| Provided by hospital | 0 | 0 |
| Hosiery: | ||
| Provided by general practitioner with special interests | 0.00565 (0.0751) | 0 |
| Provided by hospital | 0 | 0 |
| Patient resource use | ||
| Consultations with private practitioners*: | ||
| Private doctor (n=202, n=115) | 0.0248 (0.185) | 0.0261 (0.160) |
| Homoeopath (n=197, n=113) | 0.0406 (0.333) | 0.00885 (0.0941) |
| Acupuncturist (n=196, n=115) | 0.0204 (0.226) | 0.0957 (0.772) |
| Herbalist (n=196, n=114) | 0.553 (0.463) | 0.0263 (0.209) |
| Reflexologist (n=257, n=144) | 0.0233 (0.318) | 0 |
| Aromatherapist (n=196, n=112) | 0.00510 (0.0714) | 0 |
| Other (n=197, n=116) | 0.0102 (0.101) | 0.0690 (0.367) |
PUVA=psoralens plus long wave ultraviolet radiation.
Patient numbers relate to general practitioner with special interest service and hospital outpatient clinic, respectively.
Table 3.
Mean NHS costs (£) nine months after randomisation for general practitioner with specialist care or hospital outpatient care for non-urgent skin problems
| Resource item | General practitioner with special interest group (n=354) | Hospital outpatient group (n=202) |
|---|---|---|
| Hospital consultations: | ||
| Doctor | 8.26 | 66.99 |
| nurse | 0.36 | 0.54 |
| General practitioner with special interest service consultations: | ||
| General practitioner | 121.06 | 0 |
| Nurse | 11.26 | 0 |
| Total specialist care | 140.94 | 67.53 |
| Visit to doctor's surgery | 13.79 | 11.95 |
| Home visit by general practitioner | 0.05 | 0 |
| Surgery visit to practice nurse | 2.85 | 1.69 |
| Home visit by district nurse | 0.17 | 0 |
| Total primary care | 16.86 | 13.63 |
| Total consultations | 157.80 | 81.16 |
| Investigations: | ||
| Biochemistry | 0.06 | 0.07 |
| Haematology | 0.32 | 0.12 |
| Histopathology | 7.65 | 4.84 |
| Immunology | 0.04 | 0.07 |
| Microbiology | 0.08 | 0.28 |
| Mycology | 0.51 | 0.68 |
| Patch test | 4.27 | 6.16 |
| Radiology | 0.13 | 0.07 |
| Skin prick test | 0.27 | 0 |
| Virology | 0 | 0.05 |
| Total | 13.33 | 12.33 |
| Treatments | ||
| PUVA course: | ||
| Provided by general practitioner with special interests | 0 | 0 |
| Provided by hospital | 1.73 | 0.50 |
| Excision: | ||
| Provided by general practitioner with special interests | 1.02 | 0 |
| Provided by hospital | 0 | 0.55 |
| Incisional biopsy: | ||
| Provided by general practitioner with special interests | 0.56 | 0 |
| Provided by hospital | 0.22 | 0.16 |
| Punch biopsy: | ||
| Provided by general practitioner with special interests | 0.99 | 0 |
| Provided by hospital | 0.04 | 0.55 |
| Curettage and cautery: | ||
| Provided by general practitioner with special interests | 1.00 | 0 |
| Provided by hospital | 0 | 0.28 |
| Triamcinolone acetonide injection: | ||
| Provided by general practitioner with special interests | 0.02 | 0 |
| Provided by hospital | 0 | 0 |
| Hosiery: | ||
| Provided by general practitioner with special interests | 0.01 | 0 |
| Provided by hospital | 0 | 0 |
| Total | 5.61 | 2.04 |
| Specialist care drugs | 22.22 | 12.26 |
| Primary care drug | 8.95 | 10.34 |
| Total cost to NHS | 207.91 | 118.13 |
PUVA=psoralens plus long wave ultraviolet radiation.
Table 4.
Mean costs (£) to patient and companion, and lost production costs with and without imputation for nine months after randomisation to general practitioner with special interest care or hospital outpatient care for non-urgent skin problems
|
Resource item
|
General practitioner with special interest care
|
Hospital outpatient care
|
||
|---|---|---|---|---|
| Without imputation | With imputation | Without imputation | With imputation | |
| Patient and companion costs* | ||||
| Patient travel to hospital (n=295, n=106) | 0.53 | 0.70 | 3.32 | 2.35 |
| Patient travel to general practitioner with special interest service (n=271, n=198) | 3.98 | 3.88 | 0 | 0.04 |
| Patient travel to primary care (n=271, n=198) | 0.34 | 0.34 | 0.55 | 0.53 |
| Companion travel (n=282, n=143) | 0.04 | 0.06 | 0.23 | 0.19 |
| Over the counter drugs (n=211, n=120) | 26.36 | 33.65 | 36.23 | 38.53 |
| Private practitioners (n=192, n=110) | 1.00 | 0.66 | 0.82 | 0.45 |
| Unpaid time off work (n=170, n=100) | 7.48 | 8.92 | 9.36 | 9.21 |
| Total | 39.73 | 48.21 | 50.51 | 51.30 |
| Lost production* | ||||
| Associated with patient (n=177, n=98) | 23.38 | 24.55 | 27.37 | 29.66 |
| Associated with companion (n=256, n=142) | 0.59 | 2.59 | 2.69 | 4.69 |
| Total | 23.97 | 27.14 | 30.06 | 34.35 |
Patient numbers relate to general practitioner with special interest service and hospital outpatient clinic, respectively.
Cost effectiveness analyses from an NHS perspective
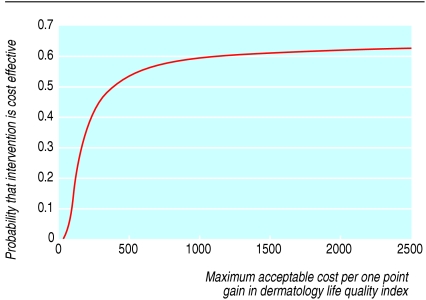
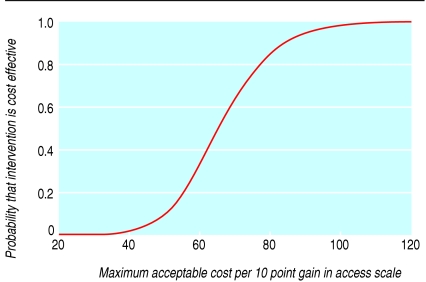
Table 5 contains data on cost and effectiveness when patients are only included who provided a dermatology life quality index score at the nine month follow-up or for whom an access score was available as well as incremental cost effectiveness ratios for the two primary outcomes. Neither option is dominant: for both primary outcomes, care by the general practitioner with special interest is both more beneficial (albeit not necessarily noticeably so on average) and more costly. The additional cost of a one point gain in the dermatology life quality index through use of the general practitioner with special interest service is in the region of £540, whereas a gain of 10 points in the access score can be obtained for £65. Uncertainty around these estimates is represented by the cost effectiveness acceptability curves, which show the probability that care by a general practitioner with special interest is cost effective compared with the maximum that decision makers might be willing to pay for these outcome gains (figs 1 and 2). For example, decision makers who are willing to pay £100 for a 10 point gain in the access scale would always find care by a general practitioner with special interests cost effective, whereas a decision maker willing to pay only £60 for such a gain would find care cost effective with only a probability of 33%.
Table 5.
Mean cost (£) to NHS and effectiveness information for those patients for whom outcome data are available, and ICERs (incremental cost effectiveness ratios) for general practitioner with specialist care over hospital outpatient care for the two primary outcome measures
| Primary outcome | General practitioner with special interest care | Hospital outpatient care | Difference between groups | ICER for general practitioner with special interest care over hospital outpatient care |
|---|---|---|---|---|
| Gain in dermatology life quality index score: | (n=257) | (n=155) | ||
| NHS costs
|
224.87
|
127.61
|
97.26
|
540.33 per 1 point gain
|
| Effectiveness
|
2.54
|
2.36
|
0.18
|
|
| Access scale: | (n=266) | (n=125) | ||
| NHS costs
|
243.71
|
140.97
|
102.74
|
65.61 per 10 point change
|
| Effectiveness | 76.13 | 60.47 | 15.66 |
Fig 1.
Cost effectiveness acceptability curve showing probability that care by general practitioner with special interest in dermatology is cost effective for a range of decision makers' maximum willingness to pay for a one point gain in dermatology life quality index score
Fig 2.
Cost effectiveness acceptability curve showing probability that care by general practitioner with special interest in dermatology is cost effective for a range of decision makers' maximum willingness to pay for a 10 point gain in access scale score
A societal perspective on consequences of cost
Table 6 provides a balance sheet summarising the costs and effects across all different perspectives and for all outcomes assessed. There is evidence of a difference between the NHS costs in the two arms of the trial, but not for patient or companion costs and costs of lost production. Outcomes are poorer for outpatient care on all measures, with evidence of differences beyond chance for all measures except those for the dermatology life quality index.
Table 6.
Cost consequences (mean, 95% confidence interval) comparing care of non-urgent skin problems by general practitioner with special interest service and hospital outpatient clinic over nine months
| Variables | General practitioner with special interest group | Hospital outpatient group |
|---|---|---|
| Costs (£): | ||
| NHS costs | 207.92 (189.51 to 226.32) | 118.14 (103.15 to 133.13) |
| Costs to patients and companions | 48.21 (32.51 to 63.91)* | 51.30 (31.32 to 71.27)* |
| Societal costs of lost production | 27.14 (8.82 to 45.46)* | 34.35 (10.91 to 57.78)* |
| Outcomes: | ||
| Gain in dermatology life quality index score | 2.54 (2.00 to 3.08) | 2.36 (1.62 to 3.10) |
| Access scale | 76.13 (73.79 to 78.46) | 60.47 (57.43 to 63.50) |
| Consultation satisfaction | 71.05 (69.38 to 72.72) | 65.93 (62.98 to 68.87) |
| Facilities scale | 79.83 (78.21 to 81.46) | 74.71 (72.04 to 77.38) |
| Waiting time (days) | 72 (69.34 to 75.50) | 113 (108.15 to 117.84) |
Using imputed values to allow calculation of confidence intervals.
Sensitivity analysis
The costs for use of NHS resources by all patients at 12 months was £224.14 for care by a general practitioner with special interest and £132.91 for outpatient care. Compared with costs at nine months, these values did not indicate that carrying out analysis using nine month data had adversely affected the costs of care by a general practitioner with special interests.
Using a reduced cost for care by a general practitioner with special interests to reflect possible under-utilisation caused by the trial resulted in a reduced cost to the NHS of £176.80 for the general practitioner with special interest arm. This reduced cost for such care was still greater than that for outpatient care.
Discussion
Costs incurred by the NHS for a general practitioner with special interest service for non-urgent skin problems were about 75% higher than those for care provided in a hospital outpatient clinic. Although the number of consultations was slightly higher among patients receiving care from a general practitioner with special interest, the major contribution to the increased costs in the service was the higher unit costs associated with consultations rather than with hospital specialist consultations. The main reason for these higher costs is that the patients attending the general practitioner with special interest service always see the relatively costly general practitioner with special interests, whereas outpatients might see the relatively costly consultant but may also see one of the consultant team (registrar or clinical assistant) who is less costly. Mean costs to patients and companions were slightly lower in the general practitioner with special interest service, but the confidence intervals were similar. Health outcomes for general practitioner with special interest services were slightly better, but the difference was minimal. Benefits were, however, found with access, satisfaction, waiting times, and facilities in the general practitioner with special interest service. The cost effectiveness acceptability curve for the access scale suggests that a decision maker who is willing to pay £100 for an improvement of 10 points in the access scale would always find the general practitioner with special interest service cost effective.
Strengths and weaknesses of study
This study provides rigorous evidence about the cost effectiveness of a general practitioner with special interest service from both NHS and societal perspectives. It is based on data collected from a randomised controlled trial, and NHS resource use data were successfully collected from reliable sources for all participants. Data obtained from the patient questionnaire were, however, more variable for quality and completion, and some imputation of data was required.
The study is based on one geographical area and its findings may not apply to other settings. Information about resource use is, however, provided separately from information about costs, which allows decision makers in the NHS to use this information in planning their own general practitioner with special interest services.
A further limitation is the extent to which the general practitioner with special interest service was operating at full capacity. Despite the use of a 2:1 ratio for randomisation and attempts to enable patients from outside the trial catchment area to utilise the service, on average the service was under-utilised, with 22% of appointments remaining unfilled. Although this is likely to have affected resource use, the sensitivity analysis suggested that the decision would not be changed by increased use of the service. Under-utilisation of the service may also have led to greater benefits being apparent than would be the case if the service was fully utilised, particularly for waiting times, but also potentially for satisfaction with care.
Relation with previous studies
In line with previous studies of outreach clinics4,5,10,11 and other studies attempting to shift care from secondary to primary services,11 the general practitioner with special interest service was more costly than outpatient care. The limitations of this study in relation to under-utilisation are also similar to those of research on service development more generally.12
Implications for policy
The implications for policy depend largely on whether the evidence about the cost effectiveness of this service is generalisable to similar services. In turn, this is likely to depend on the context in which such services are provided and their relative size and scope.
If this service is typical, then those making the decision about whether the increased cost to the NHS of general practitioner with special interest services is worth incurring must set the potential for using these funds to treat others who might benefit from increased outcomes against the benefits noted here for increased access to care. The cost effectiveness acceptability curve for the access scale suggests that, if decision makers are prepared to pay £100 for an improvement in access of 10 points on this scale, the general practitioner with special interest service would always be cost effective. The important question in interpreting these values is therefore to ask how much decision makers are willing to pay to improve access to health care rather than spending funds on greater improvements in health outcome. Indeed, the scheme affects several outcomes (table 6), all of which decision makers may want to take into account.
Given the changing UK context of the introduction in the NHS of “payment by results” (whereby primary care trusts will commission activity from hospitals based on a standard national price tariff13) it is useful to compare costs estimated in this research with those in the national tariff. Using the national tariff for dermatology outpatients, the mean cost of commissioning specialist care from a hospital for the patients in this study would have been £127 per patient (based on the new and follow-up consultation rates in the outpatient arm), compared with £182 per patient actually spent in the general practitioner with special interest arm.14 Although primary care trusts are encouraged to shift resources to deliver services in new ways, particularly through the use of general practitioner with special interests,13 these calculations illustrate the value that the trusts will need to place on the benefits of general practitioner with special interest services to justify this extra investment.
Conclusion
The general practitioner with special interest service for dermatology evaluated here was more costly to the NHS but less costly to patients and companions and in terms of lost production. Increased NHS costs must be offset against the marginally greater benefits in terms of health and the greater benefits in terms of access that were experienced.
What is already known on this topic
General practitioner with special interest services are being developed throughout England
No robust evidence exists about the economics of such schemes in terms of their relative cost effectiveness compared to routine hospital care
What this study adds
Patients referred to the general practitioner with special interest service incurred higher NHS costs for little difference in clinical outcome compared with routine outpatient care
The higher cost of general practitioner with special interest services must be offset against the improvements in access measured in several ways
We thank the other members of the research team: Zoe Crosby, Viv Harrison, David de Berker, and Mary Wallace, and the patients and staff who supported this project (Bristol South and West Primary Care Trust, United Bristol Healthcare Trust, and the members of the trial advisory group). The Department of Social Medicine, University of Bristol is the lead centre of the Medical Research Council Health Services Research Collaboration.
Contributors: CS, SN, JC, and TJP designed the study and obtained funding. JC and SN coordinated the study on a day to day basis. SH and AN set up databases. AN and OA collected data. The analysis was carried out by JC, SN, and OA. The paper was written by JC with comments and contributions from all authors, who all approved the final version of the paper. JC is guarantor.
Funding: NHS service delivery and organisation research and development programme.
Competing interests: None declared.
Ethical approval: United Bristol Healthcare Trust local research ethics committee.
References
- 1.Department of Health, Royal College of General Practitioners. Implementing a scheme for general practitioners with special interests. London: DoH, 2002.
- 2.Kernick D. Developing intermediate care provided by general practitioners with a special interest: the economic perspective. Brit J Gen Pract 2003;53: 553-6. [PMC free article] [PubMed] [Google Scholar]
- 3.Rosen R, Stevens R, Jones R. General practitioners with special clinical interests. BMJ 2003;327: 460-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black M, Leese B, Gosden T, Mead N. Specialist outreach clinics in general practice: what do they offer? Brit J Gen Pract 1997;47: 558-61. [PMC free article] [PubMed] [Google Scholar]
- 5.Bond M, Bowling A, Abery A. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Comm Health 2000;54: 149-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nocon A, Rhodes PJ, Wright JP, Eastham J, Williams DRR, Harrison SR, et al. Specialist general practitioners and diabetes clinics in primary care: a qualitative and descriptive evaluation. Diabet Med 2004;21: 32-8. [DOI] [PubMed] [Google Scholar]
- 7.Salisbury C, Noble A, Horrocks S, Crosby Z, Harrison V, Coast J, et al. Evaluation of a general practitioner with special interest service for dermatology: randomised controlled trial. BMJ 2005;331:doi = 10.1136/bmj.38670.494734.7C. [DOI] [PMC free article] [PubMed]
- 8.Coast J. Is economic evaluation in touch with society's health values? BMJ 2004;329: 1233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Curtis L, Netten A. Unit costs of health and social care 2004. Canterbury: Personal Social Services Research Unit, University of Kent, 2004.
- 10.Bowling A, Bond A. A national evaluation of specialists' clinics in primary care settings. Brit J Gen Pract 2001;51: 264-9. [PMC free article] [PubMed] [Google Scholar]
- 11.Powell J. Systematic review of outreach clinics in primary care in the UK. J Health Serv Res Policy 2002;7: 177-83. [DOI] [PubMed] [Google Scholar]
- 12.Coast J, Hensher M, Mulligan JA, Shepperd S, Jones J. Conceptual and practical difficulties with the economic evaluation of health services developments. J Health Serv Res Policy 2000;5: 42-8. [DOI] [PubMed] [Google Scholar]
- 13.Department of Health. Reforming NHS financial flows. Introducing payment by results. London: DoH, 2002.
- 14.Department of Health. National tariff 2005/6. London: DoH, 2004.