Abstract
Expanded options for treatments directed against pathogens that can be used for bioterrorism are urgently needed. Treatment regimens directed against such pathogens can be identified only by using data derived from in vitro and animal studies. It is crucial that these studies reliably predict the efficacy of proposed treatments in humans. The objective of this study was to identify a levofloxacin treatment regimen that will serve as an effective therapy for Bacillus anthracis infections and postexposure prophylaxis. An in vitro hollow-fiber infection model that replicates the pharmacokinetic profile of levofloxacin observed in humans (half-life [t1/2], 7.5 h) or in animals, such as the mouse or the rhesus monkey (t1/2, ∼2 h), was used to evaluate a proposed indication for levofloxacin (500 mg once daily) for the treatment of Bacillus anthracis infections. The results obtained with the in vitro model served as the basis for the doses and the dose schedules that were evaluated in the mouse inhalational anthrax model. The effects of levofloxacin and ciprofloxacin treatment were compared to those of no treatment (untreated controls). The main outcome measure in the in vitro hollow-fiber infection model was a persistent reduction of culture density (≥4 log10 reduction) and prevention of the emergence of levofloxacin-resistant organisms. In the mouse inhalational anthrax model the main outcome measure was survival. The results indicated that levofloxacin given once daily with simulated human pharmacokinetics effectively sterilized Bacillus anthracis cultures. By using a simulated animal pharmacokinetic profile, a once-daily dosing regimen that provided a human-equivalent exposure failed to sterilize the cultures. Dosing regimens that “partially humanized” levofloxacin exposures within the constraints of animal pharmacokinetics reproduced the antimicrobial efficacy seen with human pharmacokinetics. In a mouse inhalational anthrax model, once-daily dosing was significantly inferior (survival end point) to regimens of dosing every 12 h or every 6 h with identical total daily levofloxacin doses. These results demonstrate the predictive value of the in vitro hollow-fiber infection model with respect to the success or the failure of treatment regimens in animals. Furthermore, the model permits the evaluation of treatment regimens that “humanize” antibiotic exposures in animal models, enhancing the confidence with which animal models may be used to reliably predict the efficacies of proposed antibiotic treatments in humans in situations (e.g., the release of pathogens as agents of bioterrorism or emerging infectious diseases) where human trials cannot be performed. A treatment regimen effective in rhesus monkeys was identified.
The possible misuse of pathogenic microorganisms as weapons or agents of terror and their potential to inflict widespread death and illness have been acknowledged since 1346, when Mongols catapulted plague-infected corpses into the Crimean city of Caffa (27). Several small-scale incidents of biowarfare and bioterrorism that occurred during the 20th century (23) ultimately led to modest preparations for such an attack against American military personnel and the country's civilian population during the last decade of that period (2). Those preparations were severely tested in September and October 2001, when the American public was intentionally exposed to spores from the organism Bacillus anthracis by use of the U.S. Postal Service as a delivery vehicle. The event was limited in scope, with a total of 22 confirmed cases of anthrax, 11 cases of inhalational anthrax, and 5 fatalities. A review of these events suggests that those preparations, particularly an antibiotic prophylaxis plan in New York City (5), prevented an equal number of inhalational anthrax cases (6, 20). While these preparations limited the effects of this incident of bioterrorism, their ability to deal with this event might well have been overwhelmed if a larger-scale attack had occurred. It is therefore in the public interest to generate a comprehensive and a medically sound strategy to deal with bioterrorism in general and B. anthracis in particular. Such a plan could limit casualties and attenuate the long-term effects on society, including the economic impact (20) that a future large-scale bioterrorism incident might cause.
An important element of such a preparedness strategy is the development of new treatments for those exposed to B. anthracis spores. The traditional development paradigm for new anti-infective agents is not applicable. In the case of bioterrorism-related pathogens, ethical considerations preclude the conduct of phase II and III human studies. Preclinical data plus human phase I studies must serve as the sole basis for the design of efficacious dosing regimens. At present, U.S. regulatory approval of a drug for use against B. anthracis and other biodefense category agents requires the demonstration of efficacy in one or more animal species (15). Animals, including primates, often handle drugs far differently than humans do. Differences in pharmacokinetic parameters such as drug clearance, volume of distribution, and half-life (t1/2) can drive unanticipated changes in antimicrobial efficacy. Since animal models are the cornerstone of the process of evaluation of the dose and the schedule of drugs chosen for the therapy of infections caused by biodefense pathogens, it is crucial that these studies be designed properly so that the resulting data are robust, are interpretable for dose and schedule recommendations, and reliably predict the success or failure of the proposed treatment regimens in humans.
Pharmacokinetic (PK) and pharmacodynamic (PD) principles, as applied to the design of antibiotic treatment regimens, are used to identify the drug exposure and dosing frequency that optimize therapeutic outcomes. The recognition that a particular measure of drug exposure (e.g., the time above the agent's MIC, the peak concentrations relative to the MIC, or the ratio of the area under the drug's concentration-time curve to the MIC) is most predictive of the antimicrobial effect has facilitated the development of optimized treatment regimens (7, 8). The focus of the present work is the application of an in vitro pharmacodynamic infection model to the design of treatment regimens and the validation of the system predictions in a murine model of inhalational anthrax. The hollow-fiber infection model, described below in Materials and Methods, is capable of simulating the pharmacokinetic profile of any drug in any species. This model system has previously been demonstrated to produce results that correlate with outcomes in clinical trials (3, 4, 9, 10).
Here, we examined the in vitro pharmacodynamic properties of the fluoroquinolone levofloxacin against the avirulent Δ-Sterne strain of B. anthracis. Levofloxacin is attractive for use as an agent for the treatment of B. anthracis infections because it is currently used in humans with once-daily dosing, whereas agents such as ciprofloxacin and doxycycline are administered twice daily. We used the results from the hollow-fiber system to predict the success or the failure of treatment regimens against a fully virulent strain of B. anthracis (Ames strain) in the mouse, a species that serves as a surrogate for humans for the study of antimicrobial effects against B. anthracis. In addition, other investigators (21) used our information to design an Ames strain challenge study with rhesus monkeys, which was successful and led to the granting by the U.S. Food and Drug Administration (FDA) of an indication for levofloxacin as therapy for B. anthracis infections (Levaquin package insert, FDA approval for modification to include indication for B. anthracis infections and post-exposure prophylaxix, November 2004). The previously documented efficacies of ciprofloxacin and doxycycline against B. anthracis infections in the rhesus monkey form the basis for the recommendation of the use of these agents for the treatment of inhalational anthrax in humans (18).
MATERIALS AND METHODS
Bacteria, media, susceptibility testing, and frequency of mutation to resistance.
Two Bacillus anthracis isolates, the Δ-Sterne and the Ames strains, were selected for use in these experiments. The Δ-Sterne strain, which lacks the pX01 and pX02 virulence plasmids containing the toxin and capsule genes, respectively, was used in the in vitro hollow-fiber infection model studies. In one series of experiments, a strain with a point mutation that rendered the organisms sporulation negative (28) was also used. For the mouse model experiments, the fully virulent Ames strain was employed. The MIC and minimum bactericidal concentration (MBC) values were determined by replicate tests in cation-adjusted Mueller-Hinton broth (Becton Dickinson, Sparks, MD) by methods outlined by the CLSI (formerly the NCCLS) (24). Levofloxacin powder was provided by Johnson & Johnson Pharmaceutical Research and Development, LLC, Spring House, PA. Ciprofloxacin powder was obtained from Sigma-Aldrich, St. Louis, MO. The mutation frequency of the B. anthracis isolate to 3× the MICs of levofloxacin and ciprofloxacin was determined by inoculating 15 ml of a bacterial suspension of 2.9 × 107 CFU/ml onto Mueller-Hinton agar supplemented with the drug at 3× the MIC and onto drug-free agar. After 72 h of incubation, the colonies were counted and the mutation frequency was calculated by dividing the number of CFU/ml that grew on the surface of the drug-containing agar by the number of CFU/ml that grew on the surface of the drug-free agar.
In vitro hollow-fiber pharmacokinetic infection model.
The hollow-fiber infection model was used to study the response of Bacillus anthracis to levofloxacin exposure under conditions of simulated human or animal pharmacokinetics (the BALB/c mouse and rhesus monkey have similar levofloxacin pharmacokinetics, with half-lives of about 2 h). Cellmax Cellulosic MPS hollow-fiber cartridges were obtained from Spectrum Laboratories, Rancho Domingues, CA. The hollow-fiber cartridge consists of a bundle of hollow-fiber capillaries encased in a plastic housing. The fibers are fabricated from porous material that permits the passage of nutrients and low-molecular-weight species such as antibiotics but excludes cells and high-molecular-weight compounds. Approximately 10 ml of extracapillary space lies between the fibers and the cartridge body. Nutrient growth medium (Mueller-Hinton II broth in these experiments) in a central reservoir is continuously pumped through the hollow fibers, and low-molecular-weight compounds rapidly equilibrate across the fibers with the extracapillary space. Thus, microorganisms that are sequestered in the extracapillary space are exposed to conditions approximating those that prevail in the central reservoir.
Antibiotic was infused into the central reservoir at the desired times over a period of 1 h by computer-driven syringe pumps. Antibiotic was eliminated from the system by instilling fresh drug-free medium into the central reservoir and withdrawing the medium at an identical rate. The rate of elimination of antibiotic was the rate of fresh medium infusion divided by the volume of the medium in the total system. As described, the system simulates a single-compartment model with exponential elimination.
Ten milliliters of a suspension of Bacillus anthracis (106 CFU/ml) was inoculated into the extracapillary space of a hollow-fiber cartridge for each experimental condition, and the experiment was initiated by infusing antibiotic. Unless stated otherwise, a 1-ml sample was taken daily from the extracapillary space and subjected to quantitative culture on drug-free Trypticase soy agar (total organisms) or Mueller-Hinton II agar containing 3× the MIC of levofloxacin or ciprofloxacin (resistant organisms). Samples were also taken from the central reservoir at regular intervals over the first 48 h and assayed for levofloxacin or ciprofloxacin concentrations, as described below.
Mouse inhalational anthrax challenge.
For antibiotic efficacy studies, 6- to 8-week-old female BALB/c mice were challenged by aerosol with between 50 and 100 times the established 50% lethal dose (8 × 104 CFU) of a spore preparation from the fully virulent Ames strain of B. anthracis. Antibiotic treatment (0.2 ml intraperitoneally, 10 mice/group) was initiated 24 h after challenge. Multiple doses (n = 5; 37.5 to 300 mg/kg of body weight/day) and schedules (n = 3; every 24, 12, or 6 h) of levofloxacin were examined, for a total of 15 different regimens. The pharmacokinetics of levofloxacin were determined in BALB/c mice, with drug concentrations being determined by a microbiological assay (14). All drug concentrations were analyzed simultaneously by using a population modeling approach with the BigNPAG software of Leary et al. (22). The analysis demonstrated a half-life of levofloxacin in BALB/c mice of 1.8 h (population median value). The area under the concentration-time curve (AUC)/MIC ratios for 24 h ranged from 0 (controls) to 176. Groups received treatment for 21 days, according to the dose and the schedule. Control mice received injections of phosphate-buffered saline (0.2 ml intraperitoneally) every 12 h. Time to death was an end point examined by stratified Kaplan-Meier analysis and also by Cox proportional hazards modeling. The surviving mice from each group were euthanized at day 41 postchallenge. The mouse organs were quantitatively cultured after death to validate the cause of death as B. anthracis infection.
Fluoroquinolone concentration determinations.
Samples obtained from each of the treatment models were stored at −20°C until they were assayed for the levofloxacin or the ciprofloxacin concentration by a modification of the methodology described by Wright et al. (29). A 200-μl aliquot of sample was mixed with 400 μl of acetonitrile and centrifuged at 13,000 × g for 5 min. The supernatant was collected and mixed with an equal volume of mobile-phase buffer. The mobile phase was a 60:40 mixture of 0.02 M sodium phosphate, pH 3, containing 0.2% triethylamine and 0.2% sodium dodecyl sulfate and acetonitrile and was delivered at a rate of 1.5 ml/min. The stationary phase consisted of an Alltech Adsorbosphere HS C18 column (150 by 4.6 mm). Levofloxacin was detected fluorometrically by using excitation and emission wavelengths of 295 and 480, respectively. Ciprofloxacin was detected by using excitation and emission wavelengths of 275 and 450, respectively.
In vitro PK modeling.
All samples for levofloxacin concentration determination were simultaneously analyzed for the six initial regimens by using a population approach with the NPAG program of Leary et al. (22). The ciprofloxacin control regimen was similarly analyzed.
RESULTS
In vitro PK and PD of levofloxacin against B. anthracis.
MIC and MBC determinations were performed for both levofloxacin and ciprofloxacin. The MIC for the Δ-Sterne strain was 0.12 mg/liter for levofloxacin and was 0.06 mg/liter for ciprofloxacin. The observed MBCs were 16-fold higher than the MICs for both drugs. Other spore-forming strains of B. anthracis showed a similar discordance between the MIC and the MBC (the Ames strain, among others [data not shown]). In the case of a strain with a point mutation that rendered the organisms sporulation negative (28), the MIC/MBC ratio was 1.0. The mutational frequency to resistance for levofloxacin was <1/(5 × 108), and that to resistance for ciprofloxacin was <1/(4.35 × 108) on one occasion and 1/(5.9 × 107) on another.
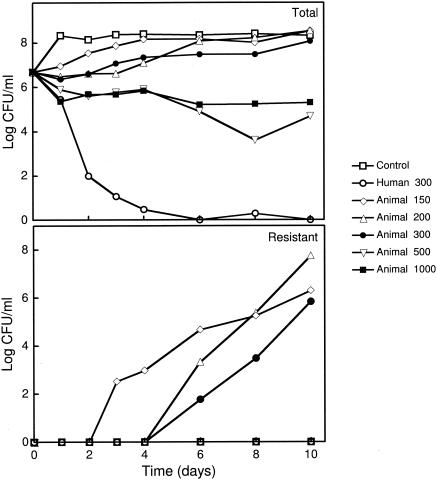
The first hollow-fiber system experiment consisted of an untreated control and six simulated treatment regimens. A once-daily dosing regimen that used human pharmacokinetics for levofloxacin (t1/2 = 7.5 h) was examined, where the AUC at 24 h (AUC24)/MIC ratio was 300, an exposure typically attained with a daily 500-mg dose in humans. Five once-daily regimens by the use of animal pharmacokinetics with AUC24/MIC ratios ranging from 150 to 1,000 were evaluated, including a regimen that had an AUC24/MIC ratio of 300. The imposition of animal pharmacokinetics resulted in peak concentrations that were higher than those seen in human regimens and trough concentrations that were lower (Fig. 1). As ciprofloxacin is approved for the therapy of B. anthracis at a dose and a schedule of 500 mg every 12 h, it is a necessary positive control. Consequently, we also examined this agent as part of this and subsequent experiments (data shown subsequently).
FIG. 1.
A pharmacokinetic profile that approximates free (non-protein-bound) drug concentrations that result from once-daily administration of 500 mg levofloxacin to human subjects (dashed line) is depicted. The solid line describes an equivalent levofloxacin exposure (the same AUC24) under conditions of monkey and murine pharmacokinetics. The datum points (circles and squares) represent the experimentally attained levofloxacin concentrations in the hollow-fiber infection model.
Levofloxacin (AUC24 = 36 mg · h/liter and AUC24/MIC = 300 with administration once daily with human pharmacokinetics and t1/2 = 7.5 h) and ciprofloxacin (AUC24 = 16 mg · h/liter and AUC24/MIC = 267 with administration twice daily with rhesus monkey and murine kinetics and t1/2 = 2.2 h) effectively sterilized the cultures over the course of the 10-day experiment (Fig. 2, upper panel). The ciprofloxacin dose simulated was the approved dose of 500 mg every 12 h.
FIG. 2.
Antimicrobial activity of levofloxacin (once-daily dosing) against Bacillus anthracis in the hollow-fiber infection model under conditions of human and monkey-murine pharmacokinetics. (Upper panel) Effects on the total bacterial population. An untreated culture served as a control. The simulated pharmacokinetic profile (human or animal) and AUC24/MIC ratio of each treatment regimen are shown. (Lower panel) Emergence of levofloxacin-resistant organisms during the experiment. Samples were plated on medium containing 3× the MIC of levofloxacin to enumerate resistant organisms. With animal pharmacokinetics, resistant organisms emerged and replaced the susceptible organisms with an AUC24/MIC ratio of ≤300. No resistant organisms were observed in the control, the human pharmacokinetics, or the animal pharmacokinetics with AUC24/MIC ratios of 500 and 1,000. The datum points for those treatment regimens are superimposed along the x axis.
Human-equivalent exposures of levofloxacin with animal pharmacokinetics (with administration once daily, AUC24/MIC ratios ≤ 300, and t1/2 = 2 h) permitted growth to near control levels. Higher exposures prevented growth but did not sterilize the cultures.
The emergence of antibiotic-resistant organisms in each regimen was evaluated by plating samples on antibiotic-containing medium. Throughout the course of the experiment, no organisms resistant to the fluoroquinolones were observed in the no-treatment control. The once-daily levofloxacin regimen with human pharmacokinetics sterilized the culture (Fig. 2, upper panel) and therefore did not select resistant organisms. When an animal pharmacokinetic profile was employed, there was the emergence of resistance when the AUC24/MIC ratio was ≤300. The time frame of resistance emergence was related to the exposure intensity. The AUC24/MIC ratio of 150 selected resistant clones by day 3 of the experiment. Resistant organisms emerged after day 4 with AUC24/MIC ratio regimens of 200 and 300; but the AUC24/MIC regimen of 300 had a lower growth rate, suggesting partial suppression of growth of resistant organisms (Fig. 2, lower panel). This type of behavior has been seen in a previously published animal experiment with Pseudomonas aeruginosa (19) and likely represents the differential effects of a drug exposure on the mixed sensitive and resistant bacterial populations. It is likely that resistant clones were not present a priori in the levofloxacin experiments but, rather, were generated during therapy by error-prone DNA repair mechanisms. More intensive exposures did not select resistant organisms.
Why did in vitro once-daily dosing of levofloxacin with animal pharmacokinetics fail?
We suspected that in the case of animal pharmacokinetics (murine or rhesus pharmacokinetics, which are virtually equivalent for levofloxacin), levofloxacin concentrations fell below the MIC for a significant fraction of the dosing interval (∼12 h, or about 50% of the dosing interval for the regimen with an AUC/MIC of 150), resulting in the exhaustion of persistence or the so-called postantibiotic effect (PAE) (13), allowing regrowth of the organisms to baseline levels. We also hypothesized that the spore form of B. anthracis played a major role in the inability of levofloxacin to sterilize the cultures when animal pharmacokinetics were imposed.
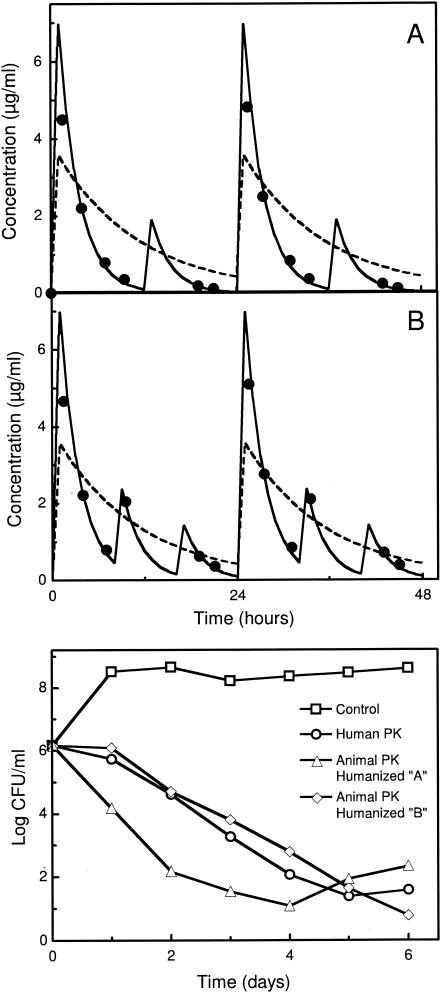
We tested these hypotheses by sampling five times daily over three 24-h dosing intervals from the once-daily levofloxacin regimens (AUC24/MIC = 250) simulating human and monkey-murine pharmacokinetics (Fig. 3, upper panel). Under the experimental conditions simulating human pharmacokinetics, the spore-positive culture was sterilized. With animal pharmacokinetics, an exposure intensity of AUC24/MIC of 250 resulted in substantial cell killing following each dose, but regrowth between hours 20 and 24 restored the bacterial population density to nearly baseline values. These cycles of killing and regrowth were observed with both spore-positive and spore-negative strains. When the exposure increased to an AUC24/MIC ratio of 1,000 (Fig. 3, lower panel), the spore-negative strain was eradicated in 72 h, while the spore-positive strain persisted, as in the earlier experiments. Under conditions of animal pharmacokinetics, the short elimination half-life results in levofloxacin concentrations that fall below the MIC for a substantial fraction of the dosing interval in regimens producing AUC24/MIC ratios in the range of 250 to 300, allowing regrowth of the cultures. Even with greater exposure intensities, drug levels drop to near MIC levels within 24 h with animal pharmacokinetics. It is also likely that the vegetative form rather than the spore form is selectively killed by the antibiotic. Exposure to subinhibitory concentrations of quinolones may also promote sporulation. We speculate that the regimen simulating human pharmacokinetics succeeded because the levofloxacin concentrations remained above the MIC for the entire dosing interval, leaving little chance for vegetative organisms to form spores before being killed and ensuring that the organisms arising from newly germinating spores were killed by the prevailing drug concentrations.
FIG. 3.
Bacterial killing and regrowth and the role of sporulation in treatment regimens simulating human and animal pharmacokinetics. (Upper panel) Results obtained with daily treatment regimens with an AUC24/MIC of 250. The simulated human exposure sterilized the culture within 72 h. With animal pharmacokinetics, a cycle of killing and regrowth was seen during each 24-h dosing interval. Similar results were seen with wild-type and sporulation-negative organisms. (Lower panel) A simulated animal exposure at an AUC24/MIC of 1,000 rapidly sterilized the cultures of the spore-negative [spore (−)] organisms but not cultures of spore-positive [spore (+)] bacteria.
Restoring efficacy to once-daily levofloxacin under conditions of animal pharmacokinetics.
Once-daily levofloxacin was effective when it was studied with human pharmacokinetics (Fig. 2, upper panel) but was ineffective with the much shorter half-life seen in animals. While many experimental and clinical data indicate that fluoroquinolones are drugs for which AUC24/MIC ratio is the exposure measure most closely linked to microbiological and clinical outcomes (1, 7, 11, 17, 25), it has been shown by Craig and colleagues that under experimental conditions that impose very short half-lives, aminoglycosides and fluoroquinolones behave as though the time that the concentration is greater than the MIC is the determining parameter when the dosing interval is very long relative to the half-life (26). Such conditions prevailed in these studies, where levofloxacin was administered once every 10 to 12 half-lives.
In order to design a dosing regimen that would be effective in the rhesus monkey inhalational anthrax model and predictive of efficacy in humans, a set of dose administration schedules was evaluated, in which a large proportion of the total daily dose was administered at the beginning of a 24-h dosing interval and smaller doses were administered at 8 and 16 h or a single supplementary dose was administered at 12 h. The last two sets of doses produced levofloxacin concentrations that transiently approximated the concentrations seen in humans with a 500-mg dose administered once daily. These “partially humanized” pharmacokinetic profiles and the efficacies of these treatment regimens are presented in Fig. 4. The regimen that used human pharmacokinetics was effective, as before. “Partially humanized” fractionated regimens under conditions of simulated monkey and murine pharmacokinetics similarly reduced the culture densities over the time frame of the experiment. No levofloxacin-resistant organisms were recovered from any culture subjected to “partially humanized” treatment regimens.
FIG. 4.
Efficacy of levofloxacin against B. anthracis under “partially humanized” animal pharmacokinetic profiles. (Upper panels) Treatment regimens in which levofloxacin was administered at the beginning of each 24-h dosing interval (AUC = 23 mg · h/liter) and a smaller dose at 12 h (AUC = 6.1 mg · h/liter; partially humanized [A]) or in which levofloxacin was administered in three decreasing doses at 8-h intervals (AUCs = 22, 7.5, and 4.5 mg · h/liter, respectively; partially humanized [B]). For each regimen, the solid line depicts the theoretical pharmacokinetic profile of the partially humanized regimens with datum points for the measured levofloxacin concentrations. The broken line shows an equivalent human exposure (AUC24 = 36 mg · h/liter; AUC24/MIC = 300). (Lower panel) Effect of the human exposure and “partially humanized” animal exposures on B. anthracis cultures.
Further examination of effect of dose schedule on efficacy of ciprofloxacin against Bacillus anthracis.
The results described above led us to question whether ciprofloxacin would remain effective when it was administered once daily with its rhesus monkey and BALB/c mouse pharmacokinetic profile (half-life, circa 2.2 h). We compared ciprofloxacin as a twice-daily regimen, the dosing schedule approved for use in humans, and a matching AUC24 regimen administered once daily. The total AUC developed for 24 h for either dosing schedule under conditions that simulated rhesus monkey or murine pharmacokinetics (AUC24) was 16.0 mg · h/liter, giving an AUC24/MIC ratio of 267. This is approximately the value developed in a rhesus monkey challenge experiment in which ciprofloxacin was studied previously (18). The emergence of resistance was also examined (Fig. 5). Ciprofloxacin administered at 12-h intervals produced a major decline in culture density with no emergence of resistance. As with levofloxacin, administration of the total ciprofloxacin dose once daily resulted in failure of the treatment regimen, accompanied by the emergence of resistance. This emergence of resistance occurred on day 1 of the experiment (1% of the total population grew on medium containing three times the baseline MIC of ciprofloxacin), in contrast to day 4 to 5 of the experiment when levofloxacin was administered daily with monkey and murine pharmacokinetics (Fig. 2, lower panel).
FIG. 5.
Effect of dose schedule on efficacy of ciprofloxacin against B. anthracis. A ciprofloxacin exposure of an AUC24 of mg · h/liter (AUC24/MIC = 256) was given as two equal doses at 12-h intervals or as a single dose at 24-h intervals. The twice-daily regimen substantially reduced the total culture density and no resistant organisms were observed. Daily dosing prevented culture growth for 2 days, but the culture density increased to near control levels thereafter. Resistant organisms emerged after 1 day and replaced the susceptible organisms in the culture by day 2. The growth of an untreated control is also shown.
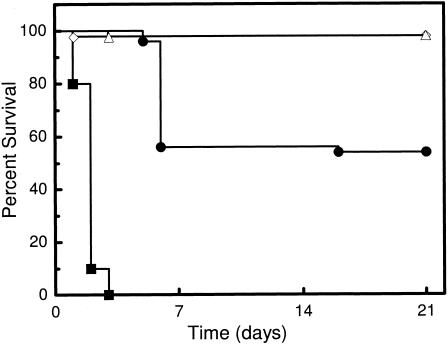
Confirmation of predictions of failure and success in the BALB/c mouse model of inhalational anthrax.
The results obtained with the in vitro hollow-fiber pharmacodynamic system data led to the prediction that if levofloxacin were administered once daily in an animal aerosol challenge model of fully virulent B. anthracis infection, there would be a high probability of therapeutic failure if the antibiotic's elimination half-life is approximately 2 h in that animal model. In order to test this prediction, we conducted an aerosol challenge using BALB/c mice.
The schedule of administration had a significant impact on time to death. With matching AUC24/MIC ratios, a daily dosing regimen was significantly inferior in terms of survivorship relative to the regimens of every 12 h or every 6 h (Fig. 6). If the once-daily dosing group was removed from the analysis, there was no significant difference between regimens of every 6 h and every 12 h. The failure of the once-daily dosing regimen and the therapeutic success of the fractionated doses were accurately predicted by the in vitro hollow-fiber studies. It should also be noted that not all the animals died in the once-daily regimen. This is likely because the BALB/c mouse model has an immune system, whereas the in vitro model has no immune function, making the results from the in vitro model conservative.
FIG. 6.
Effect of dose schedule on efficacy of levofloxacin in an in vivo mouse model of inhalational anthrax. Dosing at 12- and 6-h intervals (triangles and diamonds, respectively) conferred virtually complete protection (one death in each treatment group [the data curves overlap]), whereas 30% of the animals treated once daily (circles) died. All untreated control animals (squares) died within 3 days. A stratified Kaplan-Meier analysis demonstrated that the schedule of administration significantly influenced survivorship (P < 0.000001).
DISCUSSION
The development of reliable therapeutic regimens directed against agents of bioterrorism, such as Bacillus anthracis and Yersinia pestis, is difficult because the well-proven approach with preclinical data as well as data from phase I through phase III clinical trials cannot be employed for ethical reasons. Thus, only in vitro data, the results of animal studies, and the pharmacokinetics of the drugs of interest in humans can be applied to the identification of doses and administration schedules that would provide effective therapy to individuals intentionally exposed to such agents. FDA has provided draft guidance (25a) regarding demonstration of the effectiveness of a drug against B. anthracis by recommending the use of the rhesus monkey disease and treatment model for inhalational anthrax (postexposure), as described by Friedlander et al. (18) for ciprofloxacin, doxycycline, and penicillin G. While the rhesus monkey model is arguably the best animal model for evaluation of the doses and schedules of drugs for use against B. anthracis, the rhesus monkey often handles drugs quite differently than humans do, and these differences can result in the drawing of erroneous inferences from the animal model.
The case of levofloxacin is particularly instructive. This fluoroquinolone has been used in humans on a once-daily basis with great success for both community-based and nosocomial infections (12, 25). The half-life of this agent in people with normal renal function is 7 to 9 h (25). In the rhesus monkey, the half-life is 1.8 h. As noted above, a similar elimination half-life prevails in mice. This fluoroquinolone can be administered to humans once daily because the time that the drug concentration remains above the MIC plus the duration of the so-called persistent effect (the in vivo PAE) nearly meets or even exceeds the dosing interval of 24 h. When animal models of infection are employed, these conditions are sometimes not met, and it is important to understand the impact that the animal pharmacokinetic profile has on the treatment outcome. Our in vitro model system of infection allows the pathogen of interest to be grown to a nearly clinical infection density. The antimicrobial effect of drug regimens can be evaluated; and the effects of exposure intensity, dose schedule, and either animal or human elimination half-lives can be simulated. Consequently, the impact of the pharmacokinetic profile on the predictive value of an animal model with regard to efficacy in humans can be discerned.
In this evaluation, we examined the fluoroquinolone levofloxacin for its effect against the Δ-Sterne strain (in vitro evaluation) and the Ames strain (in vivo evaluation) of Bacillus anthracis. In these evaluations, a ciprofloxacin exposure that has previously been shown to be effective in the rhesus monkey inhalational anthrax model was included as a positive treatment control. A no-treatment regimen was also included as a negative control. These controls were compared to a standard levofloxacin exposure with human pharmacokinetics and a range of exposures with rhesus monkey and murine pharmacokinetics. In the first evaluation, the results were clear and striking. Levofloxacin, administered under conditions of human pharmacokinetics, rapidly sterilized the system, as did the positive ciprofloxacin control. All of the once-daily levofloxacin regimens with rhesus monkey pharmacokinetics failed to sterilize the system over 10 days, with some regimens employing exposures over three times greater than the human exposure, and some allowed growth approximating that seen in the no-treatment controls.
This surprising finding was investigated, and two reasons for the failure of once-daily dosing with levofloxacin with animal kinetics were identified. The first was that when the exposure approximated that seen in humans (equal AUC24/MIC ratios), the rhesus monkey pharmacokinetics caused the drug concentration to drop below the MIC so early in the dosing interval that the persistent effect generated was dissipated and there was sufficient time for regrowth of the pathogen back to nearly baseline levels. Each daily levofloxacin administration resulted in a cycling in the number of organisms (Fig. 3, upper panel), where there was initial killing followed by the release of the effect and subsequent regrowth. It would appear that a sufficient number of bacterial replications occur during these cycles to permit the emergence of resistant organisms during the first several days of antibiotic exposure.
This cycling seen at human-equivalent exposures does not explain the observation that more intensive exposures were incompletely effective under conditions of animal pharmacokinetics. Consequently, we hypothesized that the well-known spore form of this organism may have played a role. We examined the parent strain and a sporulation-negative mutant. In the case of a greater exposure (AUC24/MIC = 1,000; Fig. 3, lower panel), which results in levofloxacin concentrations above the MIC for most of the dosing interval and a persistent effect that covers the rest of the interval, cultures of the sporulation-negative mutant were sterilized within 24 h, but in cultures of the sporulation-positive isolate, viable organisms were recovered over the course of the 72-h experiment. This indicates that the spore form also plays a role in the failure of therapy with once-daily dosing with animal pharmacokinetics.
This outcome is not limited to levofloxacin. Daily dosing with ciprofloxacin at a 24-h exposure equivalent to the total daily exposure generated with dosing every 12 h resulted in microbiological failure for the once-daily exposure but microbiological success for the regimen that gave half the dose every 12 h with rhesus monkey pharmacokinetics.
Another surprising finding was the fact that both ciprofloxacin and levofloxacin fostered the emergence of resistance during therapy when they were dosed daily with animal pharmacokinetics but not when they were dosed with human PK (Fig. 2 and 5). Ciprofloxacin allowed the early emergence of resistance, with 1% of the population being resistant in 24 h. Resistance also occurred with levofloxacin, taking between 3 and 4 days to be amplified. Of note, higher exposures suppressed the amplification of resistant populations, even though these regimens failed to sterilize the system. We speculate that the spore form survives the antibiotic exposure but does not become fluoroquinolone resistant.
Given the discordance in outcomes when human versus rhesus monkey and murine pharmacokinetic profiles are produced, we needed to identify a strategy that would allow regimens to be evaluated in animals whose results could be bridged to humans. Consequently, we used the in vitro system to evaluate “humanizing” regimens that would produce a near-human concentration-time profile, within the constraints of animal pharmacokinetics. Such an approach has previously been described in an animal model system (16). Humanizing the exposure profile with one or two small supplementary exposures midway through the dosing interval, which transiently push the concentrations near those seen in humans, allowed an excellent microbiological effect (Fig. 4).
It was important to validate the predictions of the in vitro system. We predicted from the in vitro system that once-daily dosing would fail in an animal system. Figure 6 demonstrates that once-daily dosing resulted in significantly worse mortality in an inhalational challenge in mice by using the fully virulent Ames strain compared to that achieved with dosing every 12 h or every 6 h (P ≪ 0.001). This is a prospective validation of the system. It should be noted that not all of the animals died with once-daily dosing. This is likely because the animals have an immune system, while the in vitro system does not, making the predictions of the in vitro system conservative.
As importantly, the predictions of success of the system were also validated. The drug's sponsor (Ortho-McNeil Pharmaceutical) performed an inhalational challenge in rhesus monkeys with the Ames strain using a “partially humanized” regimen. Thirty rhesus monkeys (15 males and 15 females) were challenged with approximately 50× the 50% lethal dose of B. anthracis (Ames strain), and approximately 24 h later five animals of each sex per group were treated with vehicle (controls), levofloxacin (initial daily dose, 15 mg/kg; second daily dose, 4 mg/kg at hour 12 of the dosing interval), or ciprofloxacin (16 mg/kg every 12 h) for 30 days. Overall, the therapeutic success of the partially humanized levofloxacin treatment regimen paralleled the results seen with ciprofloxacin in the rhesus monkey, as predicted by the in vitro hollow-fiber infection model, indicating that levofloxacin should be at least as efficacious as ciprofloxacin for the treatment of inhalational anthrax (21). These results obtained with rhesus monkeys, combined with data from our in vitro model system and data from the murine inhalational challenge, formed the basis for a supplementary New Drug Application on the part of the sponsor to FDA for an indication for levofloxacin for the therapy and prophylaxis of Bacillus anthracis. This submission was recently approved (Levaquin package insert, FDA approval for modification to include indication for B. anthracis infections and post-exposure prophylaxix, November 2004).
These results demonstrate the important role that the in vitro hollow-fiber infection model can play in optimizing the design of animal models of antibiotic efficacy for agents of bioterrorism. Importantly, both the success and the failure of the treatment regimens in mouse and rhesus monkey inhalational anthrax challenges were correctly predicted. The results of this study also suggest that the success of ciprofloxacin as previously evaluated in rhesus monkey inhalational challenges was dependent on a twice-daily administration schedule. The in vitro model was instrumental in the design of a “partially humanized” treatment regimen that attained therapeutic success in rhesus monkeys, bridging the gap between human and animal levofloxacin pharmacokinetics. The in vitro application of PK and PD principles in the hollow-fiber infection model embodies a new paradigm in the design of animal studies intended to support the use of a drug in humans, particularly in the case of bioterrorism-related pathogens and other emerging infections, where human trials are not possible.
The bridging of the results of these studies to the recommendation of a treatment regimen for humans exposed to Bacillus anthracis spores requires an estimation of the probability that the proposed levofloxacin dosage, 500 mg daily, will produce a levofloxacin exposure sufficient to confer protection in treated individuals. A 10,000-subject Monte Carlo simulation based upon levofloxacin clearances observed in a database of 272 patients with community-acquired infections was performed. The simulated human levofloxacin exposure attained in most of the hollow-fiber studies described in these studies, a free-drug AUC of 36 mg · h/liter (AUC/MIC = 300) would be met or exceeded in 64% of the cases. In one experiment (Fig. 3), a simulated human exposure to an AUC of 30 mg · h/liter (AUC/MIC = 250) was equally effective. The probability of meeting that exposure target was 77%. Simulated “partially humanized” exposures under the constraints of animal pharmacokinetics were effective with exposures as low as an AUC of 28.1 mg · h/liter (AUC/MIC = 234). For the mouse inhalational anthrax challenge studies, the levofloxacin dose administered produced an AUC/MIC of 176. In the case of the successful inhalational anthrax challenge study with rhesus monkeys that served as the basis for the approval of levofloxacin for the treatment of Bacillus anthracis infections, the free-drug AUC was 23.4 mg · h/liter (AUC/MIC = 195). Such an exposure would be attained in >90% of treated individuals.
Finally, we have demonstrated that the emergence of resistance can occur rapidly with these agents. Further work needs to be undertaken to identify the doses and the schedules of these agents that will prevent this from occurring in wild-type strains. This is of some concern but is of lesser concern for Bacillus anthracis infections because of a lack of human-to-human transmission. Of greater importance, work must be done to identify regimens that will have activity against resistant isolates.
Acknowledgments
This work was supported by grant 1 PO1 AI060908-01A1 to G.L.D. and by a grant from Johnson & Johnson Pharmaceutical Research and Development, LLC.
G. L. Drusano serves as a consultant to Johnson & Johnson Pharmaceutical Research and Development, LLC.
Footnotes
This paper is dedicated to the memory of Mark R. Deziel.
REFERENCES
- 1.Andes, D., and W. A. Craig. 2002. Pharmacodynamics of the new fluoroquinolone gatifloxacin in murine thigh and lung infection models. Antimicrob. Agents Chemother. 46:1665-1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atlas, R. M. 2002. Bioterriorism: from threat to reality. Annu. Rev. Microbiol. 56:167-185. [DOI] [PubMed] [Google Scholar]
- 3.Bilello, J. A., G. Bauer, M. N. Dudley, G. A. Cole, and G. L. Drusano. 1994. The effect of 2′,3′-didehydro-3′-deoxythymidine (D4T) in an in vitro hollow fiber pharmacodynamic model system correlates with results of dose- ranging clinical studies. Antimicrob. Agents Chemother. 38:1386-1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bilello, J. A., P. A. Bilello, J. J. Kort, M. N. Dudley, J. Leonard, and G. L. Drusano. 1995. Efficacy of constant infusion of A-77003, an inhibitor of the human immunodeficiency virus (HIV) protease in limiting acute HIV type 1 infection in vitro. Antimicrob. Agents Chemother. 39:2523-2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blank, S., L. C. Moskin, and J. R. Zucker. 2003. An ounce of prevention is a ton of work: mass antibiotic prophylaxis for anthrax, New York City, 2001. Emerg. Infect. Dis. 9:615-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brookmeyer, R., and N. Blades. 2002. Prevention of inhalational anthrax in the U.S. outbreak. Science 295:1861. [DOI] [PubMed] [Google Scholar]
- 7.Craig, W. A. 1998. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin. Infect. Dis. 26:1-10. [DOI] [PubMed] [Google Scholar]
- 8.Drusano, G. L. 2004. Antimicrobial pharmacodynamics: the interactions between bug and drug. Nat. Rev. Microbiol. 2:289-300. [DOI] [PubMed] [Google Scholar]
- 9.Drusano, G. L., J. A. Bilello, S. L. Preston, E. O'Mara, S. Kaul, S. Schnittman, and R. Echols. 2001. Hollow fiber unit evaluation of a new human immunodeficiency virus (HIV)-1 protease inhibitor, BMS 232632, for determination of the linked pharmacodynamic variable. J. Infect. Dis. 183:1126-1129. [DOI] [PubMed] [Google Scholar]
- 10.Drusano, G. L., P. A. Bilello, W. T. Symonds, D. S. Stein, J. McDowell, A. Bye, and J. A. Bilello. 2002. Pharmacodynamics of abacavir in an in vitro hollow-fiber model system. Antimicrob. Agents Chemother. 46:464-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Drusano, G. L., D. E. Johnson, M. Rosen, and H. C. Standiford. 1993. Pharmacodynamics of a fluoroquinolone antimicrobial in a neutropenic rat model of Pseudomonas sepsis. Antimicrob. Agents Chemother. 37:483-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Drusano, G. L., S. L. Preston, C. Fowler, M. Corrado, B. Weisinger, and J. Kahn. 2004. The relationship between fluoroquinolone AUC/MIC ratio and the probability of eradication in patients with nosocomial pneumonia. J. Infect. Dis. 189:1590-1597. [DOI] [PubMed] [Google Scholar]
- 13.Eagle, H., and A. D. Musselman. 1940. The slow recovery of bacteria from the toxic effect of penicillin. J. Bacteriol. 58:475-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edberg, S. C. 1986. The measurement of antibiotics in human body fluids: techniques and significance, p. 382-399. In V. Lorian (ed.), Antibiotics in laboratory medicine, 2nd ed. The Williams & Wilkins Co., Baltimore, Md.
- 15.Federal Register. 2002. Fed. Regist. 67:37988-37998. [PubMed] [Google Scholar]
- 16.Fluckiger, U., C. Segessenmann, and A. U. Gerber. 1991. Integration of pharmacokinetics and pharmacodynamics of imipenem in a human-adapted mouse model. Antimicrob. Agents Chemother. 35:1905-1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forrest, A., D. E. Nix, C. H. Ballow, T. F. Goss, M. C. Birmingham, and J. J. Schentag. 1993. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob. Agents Chemother. 37:1073-1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedlander, A. M., S. L. Welkos, M. L. Pitt, J. W. Ezzell, P. L. Worsham, K. J. Rose, B. E. Ivins, J. R. Lowe, G. B. Howe, P. Mikesell, et al. 1993. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 167:1239-1243. [DOI] [PubMed] [Google Scholar]
- 19.Jumbe, N., A. Louie, R. Leary, W. Liu, M. R. Deziel, V. H. Tam, R. Bachhawat, C. Freeman, J. B. Kahn, K. Bush, M. N. Dudley, M. H. Miller, and G. L. Drusano. 2003. Application of a mathematical model to prevent in-vivo amplification of antibiotic-resistant bacterial populations during therapy. J. Clin. Investig. 112:275-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaufmann, A. F., M. I. Meltzer, and G. P. Schmid. 1997. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? Emerg. Infect. Dis. 3:83-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelley, M., et al. 2003. Abstr. 43rd Intersci. Conf. Antimicrob. Agents Chemother., abstr. B331A.
- 22.Leary, R., R. Jelliffe, A. Schumitzky, and M. van Guilder. 2001. An adaptive grid, non-parametric approach to pharmacokinetic and dynamic (PK/PD) models, p. 389-392. In Proceedings of the 14th IEEE Symposium on Computer Based Medical Systems. IEEE Computer Society, Bethesda, Md.
- 23.Leitenberg, M. 2001. Biological weapons in the twentieth century: a review and analysis. Crit. Rev. Microbiol. 27:267-320. [DOI] [PubMed] [Google Scholar]
- 24.National Committee for Clinical Laboratory Standards. 1997. Document M7-A4. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 25.Preston, S. L., G. L. Drusano, A. L. Berman, C. L. Fowler, A. T. Chow, B. Dornseif, V. Reichl, J. Natarajan, M. Corrado. 1998. Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 279:125-129. [DOI] [PubMed] [Google Scholar]
- 25a.U.S. Food and Drug Administration. 2002. Draft guidance for industry, inhalational anthrax (post-exposure)—development of antimicrobial drugs. CDER, U.S. Food and Drug Administration, Washington, D.C.
- 26.Vogelman, B., S. Gudmundsson, J. Leggett, J. Turnidge, S. Ebert, and W. A. Craig. 1988. Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J. Infect. Dis. 158:831-847. [DOI] [PubMed] [Google Scholar]
- 27.Wheelis, M. 2002. Biological warfare at the 1346 siege of Caffa. Emerg. Infect. Dis. 8:971-975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Worsham, P. L., and M. R. Sowers. 1999. Isolation of an asporogenic (spoOA) protective antigen-producing strain of Bacillus anthracis. Can. J. Microbiol. 45:1-8. [DOI] [PubMed] [Google Scholar]
- 29.Wright, D. H., V. K. Herman, F. N. Konstantinides, and J. C. Rotschafer. 1998. Determination of quinolone antibiotics in growth media by reversed-phase high-performance liquid chromatography. J. Chromatogr. B Biomed. Sci. Appl. 709:97-104. [DOI] [PubMed] [Google Scholar]