Abstract
Pain assessment is critical to optimal pain management interventions. While pain is a highly subjective experience, its management necessitates objective standards of care. The WILDA approach to pain assessment—focusing on words to describe pain, intensity, location, duration, and aggravating or alleviating factors—offers a concise template for assessment in patients with acute and chronic pain.
CME, Part 1 of 3
Target audience: All physicians
Learning objectives:
Understand why pain assessment is key to successful pain management.
Define and explain 5 key components of the WILDA approach to pain assessment.
Know how to assess pain in nonverbal or cognitively impaired patients.
Identify patient populations requiring special consideration when planning optimal pain assessment and management.
Faculty credentials/disclosure:
Regina Fink, RN, PhD, AOCN, is a research nurse scientist at the University of Colorado Hospital in Denver. Dr. Fink has held positions as oncology and pain clinical nurse specialist. She is co–principal investigator of a National Institutes of Health grant on palliative care and is on the speakers bureaus of Purdue Pharmaceuticals, Anestra Corporation, and Roxane Laboratories.
Before beginning this activity, please read the instructions for CME on p. 321. This page also provides important information on method of physician participation, estimated time to complete the educational activity, medium used for instruction, date of release, and expiration. The quiz, evaluation form, and certification appear on pp. 321–323 as well.
According to the International Association for the Study of Pain, pain is an unpleasant sensory and emotional experience arising from actual or potential tissue damage (1). Clinically, pain is whatever the person says he or she is experiencing whenever he or she says it occurs (2). Pain is commonly categorized along a continuum of duration. Acute pain usually lasts hours, days, or weeks and is associated with tissue damage, inflammation, a surgical procedure, or a brief disease process. Acute pain serves as a warning that something is wrong. Chronic pain, in contrast, worsens and intensifies over time and persists for months, years, or a lifetime. It accompanies disease processes such as cancer, HIV/AIDS, arthritis, fibromyalgia, and diabetes. Chronic pain can also accompany an injury that has not resolved over time, such as reflex sympathetic dystrophy, low back pain, or phantom limb pain.
In the USA, 23.3 million surgical procedures are performed each year, and most, if not all, result in some form of pain (3–6). Pain in persons with cancer also remains a significant problem, with studies suggesting that as many as 30% to 40% of cancer patients at diagnosis and 70% to 80% of cancer patients undergoing therapy or in the end stages of life have unrelieved pain (7–12). The Mayday Fund survey noted that pain is a part of life for many Americans, with 46% of respondents reporting pain at some time in their lives (13). It has been estimated that 9% of the US adult population suffers from moderate to severe chronic nonmalignant pain (14).
Despite the existence of evidence-based guidelines, acute pain is not adequately addressed by health care professionals (15). Suboptimal pain management is not the result of lack of scientific information, considering the explosion of research on pain assessment and treatment. Yet reports documenting the inability of health care professionals to use this information continue to appear in the literature. Studies have found that two of the chief barriers for health care professionals are poor pain assessment and lack of knowledge about pain (15, 16). Additionally, clinicians' personal belief systems, attitudes, and fears can directly influence the manner in which they and their patients respond to the varied dimensions ofpain management.
Recognition of the widespread inadequacy of pain management has prompted efforts to correct the problems by a wide variety of organizations, including the Agency for Health Care Policy and Research, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), the American Pain Soci-ety, and the Oncology Nursing Society. The development of practice guidelines and standards reflects the national trend in health care to assess quality of care in high-incidence patients by moni-toring selected patient outcomes, as well as the assessment and management of pain. JCAHO surveyors routinely inquire about pain assessment and management practices and quality assurance activitiesin both inpatient and outpatient care areas.
Assessment of the patient experiencing pain is the cornerstone to optimal pain management. However, the quality and utility of any assessment tool is only as good as the clinician's ability to thoroughly focus on the patient. This means listening empathically, believing and legitimizing the patient's pain, and understanding, to the best of his or her capability, what the patient may be experiencing. A health care professional's empathic understanding of the patient's pain experience and accompanying symptoms confirms that there is genuine interest in the patient as a person. This can influence a positive pain management outcome. After the assessment, quality pain management depends on clinicians' earnest efforts to ensure that patients have access to the best level of pain relief that can be safely provided. Clinicians most successful at this task are those who are knowledgeable, experienced, empathic, and available to respond to patient needs quickly.
THE WILDA APPROACH TO PAIN ASSESSMENT
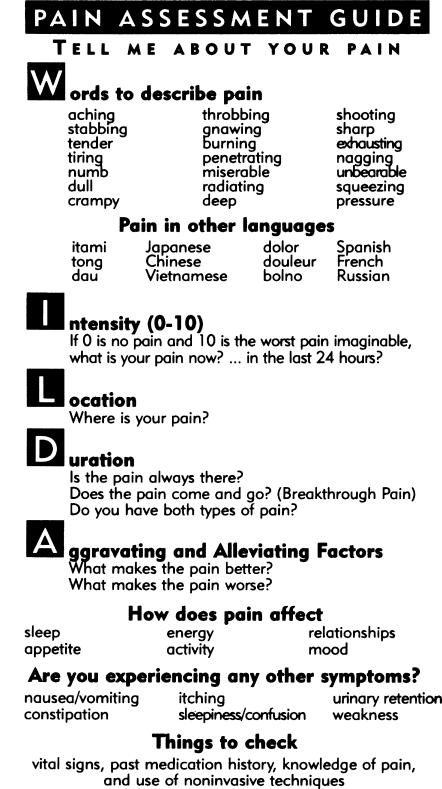
Pain assessment should be ongoing (occurring at regular intervals), individualized, and documented so that all involved in the patient's care understand the pain problem. Using the WILDA approach (Figure 1) ensures that the 5 key components to a pain assessment are incorporated into the process.
Figure 1.
A pocket card for health care providers summarizes the WILDA approach to pain assessment. Copyright (c)1996, Regina Fink, University of Colorado Health Sciences Center.
Pain assessment usually begins with an open-ended inquiry: “Tell me about your pain.” This allows the patient to tell his or her story, including the aspects of the pain experience that are most problematic. The clinician must listen closely to these first words. Patients in pain want to tell their stories, and clinicians need to take time to listen. Stories are narratives that provide meaning in our lives. They can teach, heal, validate, offer reflection, and shape how patients are cared for. Storytelling provides a different lens through which an experience can be viewed.
Words
A patient's statement, “I have pain,” is not descriptive enough to inform a health care professional about pain type. Asking patients to describe their pain using words will guide clinicians to the appropriate interventions for specific pain types. Patients may have more than 1 type of pain. The following questions should be asked of patients:
What does your pain feel like?
Because various pain types are described using different words, what words would you use to describe the pain you are having?
Neuropathic pain. This type of pain can be described as burning, shooting, tingling, radiating, lancinating, or numbness. Sometimes patients say that their pain is like a fire or an electrical jolt. This type of pain can be due to nerve disorders; nerve involvement by a tumor pressing on cervical, brachial, or lumbosacral plexi; postherpetic neuralgia; or peripheral neuropathies secondary to treatment (chemotherapy, radiation fibrosis). Typically, opioids alone will not help neuropathic pain; antidepressants, anticonvulsants, and benzodiazepines may be used as an adjuvant treatment.
Somatic pain. Described as achy, throbbing, or dull, somatic pain is typically well localized. Somatic pain accompanies arthritis, bone or spine metastases, low back pain, and orthopaedic procedures. Nonsteroidal anti-inflammatory drugs are the treatment of choice in patients who can tolerate them (i.e., those who are not at risk for gastrointestinal bleeding or renal failure). Additionally, muscle relaxants, bone-seeking radiopharmaceuticals such as strontium 89 (Metastron), certain biphosphonates (pamidronate), and opioid drugs can also be helpful.
Visceral pain. Pain described as squeezing, pressure, cramping, distention, dull, deep, and stretching is visceral in origin. Visceral pain is manifested in patients after abdominal or thoracic surgery. It also occurs secondary to liver metastases or bowel or venous obstruction. Opioids are the treatment of choice. However, caution should be taken when using this class of drugs with patients who have bowel obstructions.
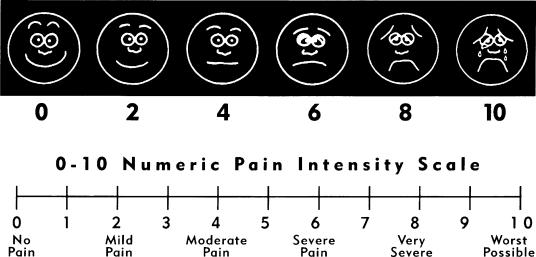
Intensity
The ability to quantify the intensity of pain is essential when caring for persons with acute and chronic pain. Though no scale is suitable for all patients, Dalton and McNaull (18) advocate a universal adoption of a 0 to 10 scale for clinical assessment of pain intensity in adult patients. Standardization may promote collaboration and consistency among caregivers in multiple settings—inpatient, outpatient, and home care environments. Using a pain scale with 0 being no pain and 10 being the worst pain imaginable, a numerical value can be assigned to the patient's perceived intensity of pain. Asking patients to rate their present pain, their pain after an intervention, and their pain over the past 24 hours will enable health care providers to see if the pain is worsening or improving. Also, inquiring about the pain level acceptable to the patient will help clinicians understand the patient's goal of therapy. The Wong/Baker faces rating scale is a visual representation of the numerical scale (19) (Figure 2). Although the faces scale was developed for use in pediatric patients, it has also proven useful with elderly patients and patients with language barriers.
Figure 2.
The reverse side of the pocket card shown in Figure 1 displays the Wong/ Baker faces rating scale, useful with children, the elderly, and patients with language barriers.
Location
Most patients have 2 or more sites of pain. Thus, it is important to ask patients, “Where is your pain?” or “Do you have pain in more than one area?” The pain that the patient may be referring to may be different than the one the nurse or physician is talking about. Having the patient point to the painful area can be more specific and help to determine interventions.
Duration
Breakthrough pain refers to a transitory exacerbation or flare of pain occurring in an individual who is on a regimen of analgesics for continuous stable pain (20). Patients need to be asked, “Is your pain always there, or does it come and go?” or “Do you have both chronic and breakthrough pain?” Pain descriptors, intensity, and location are important to obtain not only on breakthrough pain but on stable (continuous) pain as well.
Aggravating/alleviating factors
Asking the patient to describe the factors that aggravate or alleviate the pain will help plan interventions. A typical question might be, “What makes the pain better or worse?” Analgesics, nonpharmacologic approaches (massage, relaxation, music or visualization therapy, biofeedback, heat or cold), and nerve blocks are some interventions that may relieve the pain. Other factors (movement, physical therapy, activity, intravenous sticks or blood draws, mental anguish, depression, sadness, bad news) may intensify the pain.
Other things to include in the pain assessment are the presence of contributing symptoms or side effects associated with pain and its treatment. These include nausea, vomiting, constipation, sleepiness, confusion, urinary retention, and weakness. Some patients may tolerate these symptoms without aggressive treatment; others may choose to stop taking analgesics or adjuvant medications because of side effect intolerance. Adjustments, alterations, or titration may be all that is necessary.
Inquiring about the presence or absence of changes in appetite, activity, relationships, sexual functioning, irritability, sleep, anxiety, anger, and ability to concentrate will help the clinician understand the pain experience in each individual. Additionally, the clinician should discern how pain is perceived by the patient and his or her family or significant other and what works and doesn't work to help the pain.
PATIENTS' KNOWLEDGE AND BELIEFS ABOUT PAIN
Patients' knowledge and beliefs about pain are assumed to play a role in pain perception, function, and response to treatment (21). Patients may be reluctant to tell their health care providers when they have pain, may attempt to minimize its severity, may not know they can expect pain relief, and may be concerned about taking pain medications for fear of deleterious effects. A comprehensive approach to pain assessment includes evaluating patients' knowledge and beliefs about pain and its management and reviewing common misconceptions about analgesia. Several common myths need to be discussed openly:
Pain is a part of life. I just need to bear it.
I shouldn't take my pain medication until I really need it or else it won't work later.
I don't want to become an addict.
I don't want to get constipated so I'd better not take my pain medication.
I don't want to bother the doctor or nurse; they're busy with other patients.
If it's morphine, I must be getting close to the end.
My family thinks I get confused on pain medication; I'd better not take it.
Discussing these myths during the assessment process not only legitimizes patients' concerns but provides an opportunity to educate patients and families about pain medications and how they work. At times patients and family members believe that behavior such as complaining about pain or inadequate pain relief may result in substandard care (22). Realizing that they have limited time with their health care providers, patients may prioritize the time available to them. Assuming that “good” patients will receive more time and attention, patients decide for themselves that discomfort is not part of the good patient role. This is another misconception to discuss with the patient.
ASSESSING PAIN IN NONVERBAL OR COGNITIVELY IMPAIRED PATIENTS
Patients' self-report is the gold standard of pain assessment. However, pain tools that rely on verbal self-report, such as the 0 to 10 numeric rating scale, may not be appropriate for use in nonverbal or cognitively impaired patients. Additionally, reliance on nonverbal cues—e.g., changes in vital signs, moaning, facial grimacing, or muscle tenseness—is not practical or reliable. Diverse responses to pain atypical of conventional pain behaviors have been noted in patients with Alzheimer's disease by Marzinski (23). For example, a patient who normally rocked and moaned became quiet and withdrawn when experiencing pain.
It is important to obtain feedback from the patient by asking the patient to nod his head, squeeze your hand, move his eyes up and down, or raise his fingers, hand, arm, or leg to signal the presence of pain. If appropriate, offer writing materials, pain intensity charts, or figures that the patient can point to. The following questions can be used as a template for assessment of pain in the nonverbal patient:
After reviewing the patient's history, is there a reason for this patient to be experiencing pain?
When the patient experienced pain in the past, how did he or she usually act? (Note: the family/significant other or other health care providers may need to be questioned about this.)
What is the family/significant other's thoughts or interpretation of the patient's behavior? Do they believe that the patient is having pain? Why do they feel this way?
Has the patient been treated for pain previously? What pharmacologic or nonpharmacologic interventions were used? If there is a reason for or a sign of acute pain, treatment with analgesics or nonpharmacologic measures may be helpful. If a modification of pain behavior occurs, pain treatment should be continued with an explanation to the patient and family.
OTHER POPULATIONS REQUIRING SPECIAL CONSIDERATION
Multiple studies suggest that certain groups of patients who experience moderate to severe pain have been undermedicated and not adequately assessed (8, 24, 25). Patients at risk for pain are the following:
Minorities
Elderly (>70 years old)
Children
Women
Those with a history of substance abuse (alcohol and drug)
Those with high anxiety about postoperative problems
Those with high expectations for optimal pain management
Those with a history of chronic and preoperative pain
Those with a high performance score and those who “look healthier”
Those who experience breakthrough pain
Those with bone metastases or neuropathic pain
The literature supports the notion that these groups and others who have been marginalized by society have problems receiving appropriate medications and don't receive adequate pain assessments. Recognition of who's at risk for suboptimal pain management can enhance care and improve communication between clinicians and patients. The health care professional in a diverse society must increase cultural awareness and sensitivity to provide care to persons with different values, beliefs, and customs.
SUMMARY
Acute and chronic pain not properly assessed can result in inadequate pain management outcomes and can negatively affect the physical, emotional, and psychosocial well-being of patients. Pain assessment is the cornerstone to optimal pain management. Using the WILDA approach, incorporating patient concerns and beliefs, can simplify the pain assessment process. The benefits of decreasing pain and suffering are worthwhile for all concerned.
References
- 1.International Association for the Study of Pain. Pain terms: a list with definitions and notes on usage. Recommended by the IASP Subcommittee on Taxonomy Pain. 1979;6:249. [PubMed] [Google Scholar]
- 2.McCaffery M, Pasero C. Pain: Clinical Manual. 2nd ed. St. Louis, Mo: Mosby; 1999. [Google Scholar]
- 3.Peebles RJ, Schneidman DS. Socio-economic Factbook for Surgery, 1991-92. Chicago, Ill: American College of Surgeons; 1992. [Google Scholar]
- 4.Pellino TA, Ward SE. Perceived control mediates the relationship between pain severity and patient satisfaction. J Pain Symptom Manage. 1998;15:110–116. [PubMed] [Google Scholar]
- 5.Thomas T, Robinson C, Champion D, McKell M, Pell M. Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain. 1998;75:177–185. doi: 10.1016/s0304-3959(97)00218-2. [DOI] [PubMed] [Google Scholar]
- 6.Owen H, McMillan V, Rogowski D. Postoperative pain therapy: a survey of patients' expectations and their experiences. Pain. 1990;41:303–307. doi: 10.1016/0304-3959(90)90007-Z. [DOI] [PubMed] [Google Scholar]
- 7.Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, Pandya KJ. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 8.Desbiens NA, Wu AW, Broste SK, Wenger NS, Connors AF, Jr, Lynn J, Yasui Y, Phillips RS, Fulkerson W. Pain and satisfaction with pain control in seriously ill hospitalized adults: findings from the SUPPORT research investigations. For the SUPPORT investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Crit Care Med. 1996;14:1953–1961. doi: 10.1097/00003246-199612000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Jacox A, Carr DB, Payne R. Management of Cancer Pain, Clinical Practice Guideline No. 9 AHCPR Pub. No. 94-0592. Rockville, Md: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services, 1994.
- 10.Payne R, Weinstein SM, Hill CS. Assessment and management of pain. In: Levin V, editor. Cancer in the Nervous System. New York: Churchill-Livingstone; 1996. [Google Scholar]
- 11.Portenoy RK. Cancer pain. Epidemiology and syndromes. Cancer. 1989;63(11 Suppl):2298–2307. doi: 10.1002/1097-0142(19890601)63:11<2298::aid-cncr2820631140>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 12.Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med. 1993;119:121–126. doi: 10.7326/0003-4819-119-2-199307150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Bostrom M. Summary of the Mayday Fund Survey: public attitudes about pain and analgesics. J Pain Symptom Manage. 1997;13:166–168. doi: 10.1016/s0885-3924(96)00273-4. [DOI] [PubMed] [Google Scholar]
- 14.Chronic Pain in America: Roadblocks to Relief Study conducted by Roper Starch Worldwide, Inc, January 1999.
- 15.Acute Pain Management: Operative or Medical Procedures and Trauma. Clinical Practice Guideline. Rockville, Md: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services; 1992. Acute Pain Management Guidelines Panel. AHCPR Pub. No. 92-0032. [Google Scholar]
- 16.Ferrell BR, Dean GE, Grant M, Coluzzi P. An institutional commitment to pain management. J Clin Oncol. 1995;13:2158–2165. doi: 10.1200/JCO.1995.13.9.2158. [DOI] [PubMed] [Google Scholar]
- 17.Fink RM. A multidisciplinary education and research program to assess and improve outcomes of patients with pain. Unpublished manuscript submitted to the Colorado Hospital Authority Grants Program, Denver, Colo, 1996.
- 18.Dalton JA, McNaull F. A call for standardizing the clinical rating of pain intensity using a 0 to 10 rating scale. Cancer Nurs. 1998;21:46–49. doi: 10.1097/00002820-199802000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Wong D, Whaley L. Clinical Handbook of Pediatric Nursing. 2nd ed. St. Louis, Mo: Mosby; 1986. [Google Scholar]
- 20.Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41:273–281. doi: 10.1016/0304-3959(90)90004-W. [DOI] [PubMed] [Google Scholar]
- 21.Williams DA, Robinson ME, Geisser ME. Pain beliefs: assessment and utility. Pain. 1994;59:71–78. doi: 10.1016/0304-3959(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 22.Cleeland CS. Documenting barriers to cancer pain management. In: Chapman CR, Foley KM, editors. Current and Emerging Issues in Cancer Pain: Research and Practice. New York: Raven Press Ltd; 1993. pp. 321–330. [Google Scholar]
- 23.Marzinski LR. The tragedy of dementia: clinically assessing pain in the confused nonverbal elderly. J Gerontol Nurs. 1991;17:25–28. doi: 10.3928/0098-9134-19910601-08. [DOI] [PubMed] [Google Scholar]
- 24.Zhukovsky DS, Gorowski E, Hausdorff J, Napolitano B, Lesser M. Unmet analgesic needs in cancer patients. J Pain Symptom Manage. 1995;10:113–119. doi: 10.1016/0885-3924(94)00072-s. [DOI] [PubMed] [Google Scholar]
- 25.Bruera E, Schoeller T, Wenk R, MacEachern T, Marcelino S, Hanson J, Suarez-Almazor M. A prospective multicenter assessment of the Edmonton staging system for cancer pain. J Pain Symptom Manage. 1995;10:348–355. doi: 10.1016/0885-3924(95)00052-z. [DOI] [PubMed] [Google Scholar]