CME, Part 2 of 3
Target audience: All physicians
Learning objectives:
Describe a reliable tool for assessing and classifying persons with chronic pain.
Identify common treatment elements and goals of interdisciplinary programs and factors that distinguish them from other types of treatment.
Summarize research results regarding the cost-effectiveness of interdisciplinary treatment.
Faculty credentials/disclosure:
Timothy S. Clark, PhD, is program director of the Baylor Center for Pain Management. Dr. Clark has no significant financial relationships to disclose.
Before beginning this activity, please read the instructions for CME on p. 321. This page also provides important information on method of physician participation, estimated time to complete the educational activity, medium used for instruction, date of release, and expiration. The quiz, evaluation form, and certification appear on pp. 321–323 as well.
The treatment of chronic pain continues to challenge health care providers and health care systems. Interdisciplinary pain centers have been created to address the specific needs faced by individuals with chronic pain. However, the efficacy of these programs has been questioned. Of particular concern in the current health care environment is their costeffectiveness.
DEVELOPMENT OF CHRONIC PAIN SYNDROME
An understanding of the problems addressed by interdisciplinary centers may be helpful. Chronic pain syndrome is a phrase used to describe a constellation of problems often seen in persons dealing with chronic pain. Frequent characteristics are a high level of pain behavior—moaning, wincing, shifting position frequently, or disturbed gait—and the elevated use of medical resources and medications. Persons with chronic pain syndrome are often inactive and fail to carry out normal social and vocational roles. As the syndrome becomes more pronounced, individuals perceive themselves as disabled and may seek some sort of disability reimbursement. Persons with chronic pain syndrome often experience elevated levels of hopelessness, depression, anxiety, and tension.
Often chronic pain syndrome reflects the endpoint in a sequence of events. Patients become aware of their initial symptoms and seek help from their primary care physicians. Should treatment or passage of time be unsuccessful in resolving their symptoms, they frequently are referred to specialists or seek out other medical opinions and treatment on their own. As patients continue through the medical system, they are subjected to multiple diagnostic studies, are treated with a variety of medications, and may be referred to physical therapy or biofeedback and counseling. Surgical interventions are sometimes attempted to resolve the problem.
When pain continues, patients become frustrated and desperate. They increase pain behavior in an attempt to communicate their level of discomfort and its devastating impact on their lives. Frustrated as well, physicians or other health care professionals may begin to probe the impact of other factors such as stress level or lifestyle. Patient begin to fear abandonment because they perceive that the reality of their symptoms is being questioned or that their problems are being attributed to a psychological cause.
WEST HAVEN–YALE MULTIDIMENSIONAL PAIN INVENTORY
Describing and classifying chronic pain syndrome has often been unsuccessful. Examination of the pain site, consideration of the medical diagnosis, and results of diagnostic testing fail to capture the biopsychosocial problem of chronic pain. A number of authors have emphasized the need for multidimensional assessment of patients in the context of their lives. An instrument that has been devised to assess this aspect of patient functioning is the West Haven–Yale Multidimensional Pain Inventory (1). This instrument was designed to measure psychosocial functioning as well as behavioral factors and to be applicable across a wide range of pain sites and etiologies. The instrument is brief (54 items) and has been shown to be sensitive to change in psychosocial functioning. The instrument was empirically derived and has been extensively studied and validated. It has been used at the Center for Pain Management since the inception of its comprehensive outpatient program.
Patients are classified empirically into 1 of 3 major clusters. The first cluster has been labeled “dysfunctional.” Persons in this category report high levels of pain intensity, high levels of pain interference in life activities, and high levels of emotional distress. They often have a low sense of control over their lives and are quite inactive. In a general sample of patients admitted to chronic pain centers, approximately 42% fall into this category.
A second category is “interpersonally distressed.” Persons with this profile perceive themselves to be receiving little social support from their significant other or spouse and/or punitive or negative responses when they engage in pain behavior. Approximately 20% of pain patients fall within this classification.
The final cluster is that of “adaptive coper.” Persons in this group are characterized by low levels of pain intensity, low levels of pain interference in life activities, low levels of emotional distress, and high levels of control over their lives. This group accounts for approximately 29% of patients seen at a pain center.
This classification scheme assists in establishing treatment protocols, defining the types of interventions needed, and documenting patient progress.
INTERDISCIPLINARY PAIN CENTERS
By definition, interdisciplinary pain programs consist of professionals from a variety of disciplines working together in an integrated way with joint goals and with ongoing communication. This stands in contrast to clinics in which patients receive a variety of therapies in a nonintegrated way. For example, multidisciplinary care could consist of physical therapy at one site and biofeedback at another site.
A number of elements are common to most interdisciplinary programs. First, most programs involve medication management to simplify medication schedules and reduce use of opioids. A second element is graded physical exercise, in which patients receive instructions on physical exercise to help them overcome anxiety about physical activity. A third primary component of an interdisciplinary program is cognitive-behavioral training. Patients are given techniques to change thinking patterns that adversely affect their response to pain. Treatment also focuses on teaching behavioral skills, such as relaxation or biofeedback, to self-regulate psychophysiological arousal as well as pain. A fourth focus of the programs is on decreasing the impact of pain on functional life roles. This may include tools and techniques for adaptive living, ergonomics and energy conservation, pacing, and vocational counseling.
Patients seen at interdisciplinary pain centers are often not representative of all individuals with chronic pain. As tertiary centers, comprehensive pain management programs are generally selected for individuals who have complex problems, have previously failed less intense intervention, have higher rates of opioid use, have problems in their vocational functioning, have been seen by a wide range of physicians, and experience high levels of emotional distress. Many individuals perceive the program as a last hope.
PAIN MANAGEMENT SUCCESS
Clear and focused goals are critical for success in interdisciplinary pain management programs. Unrealistic goals, such as elimination of all pain, will lead to disappointment by patients, health care providers, and family members. Over the years, common target goals have been set in interdisciplinary pain programs:
To reduce pain
To increase activity levels, reduce amount of time resting during the day, and carry out functional life activities
To resolve disability claims and return patients to work or vocational training
To reduce opioid medication or use it more appropriately
To reduce emotional distress, such as depression and anxiety, and master coping techniques
To decrease the use of medical resources
RESULTS OF INTERDISCIPLINARY PROGRAMS
Outcomes of interdisciplinary programs have been extensively studied, with a number of reviews of these studies available. Flor et al conducted a meta-analysis of 65 studies and reviewed the outcomes of chronic pain programs (2). They reported a 20% average reduction in pain. Reduction rates in other studies have ranged from 0% to 60%.
Interdisciplinary pain programs have also reduced opioid use (3). One study documented that 65% of patients seen at clinics before enrolling in a pain management program used opioids compared with 20% of patients at discharge from a pain management program. Another study found that 73% of patients reduced their use of opioids while in a pain management program.
A third area of study has been the effects of interdisciplinary pain programs on increased physical activity. Flor et al found that 65% of patients treated at pain programs increased physical activity compared with 35% of conventionally treated patients (2).
Return-to-work issues have been addressed frequently in outcome studies. These studies vary significantly due to the wide variety of factors that can impact vocational return, including chronicity of disability, adaptive and transferable vocational skills, and the job market for which a person is being prepared. In their review of studies, Okifuji et al found that the average return-to-work rate for persons treated at interdisciplinary pain centers was 67% (r3). This rate was substantially higher than the 24% rate achieved by patients who had received only conventional medical treatment.
Clinical studies have also documented significant reductions in health care utilization. In their review of the literature, Okifuji et al found that 17% of patients treated at interdisciplinary centers required further hospitalization, and only 16% required additional surgery (3). In contrast, 47% of conventionally treated patients required hospitalization and 28% required surgery.
The strength of these findings has been demonstrated by a recent Danish study (4). After diagnosis and consultation with a pain specialist, patients were randomly assigned to care with a general practitioner, to placement on a waiting list, or to treatment in an interdisciplinary pain clinic. After 6 months, patients who had participated in the interdisciplinary clinic demonstrated significant pain reduction, improved physical function, improved psychological well-being, and improved quality of sleep. Patients treated by the general practitioner did not improve, and patients on the waiting list deteriorated in these measures.
In a summary, Turk and Okifuji compared the effectiveness of interdisciplinary pain management programs with that of conventional medical treatments (5) (Table 1). Both types of treatment were found to have somewhat limited benefits for pain reduction. The interdisciplinary treatment programs were effective at reducing medication use, reducing emotional distress, reducing health care utilization, reducing iatrogenic consequences, increasing return to work and activity, and closing disability claims. In contrast, conventional medical treatments had negative outcomes in medication reduction, health care utilization, iatrogenic consequences, and return to work.
Table 1.
Summary of clinical effectiveness of interdisciplinary pain centers vs conventional treatments
| Outcome variable | Interdisciplinary pain center | Conventional medical treatment |
| Pain reduction | ± | ± |
| Medication reduction | + | − |
| Reduction in emotional distress | + | ? |
| Health care utilization | + | − |
| Iatrogenic consequences | + | − |
| Activity/return to work | + | − |
| Closure of disability claims | + | ? |
Positive and negative outcomes are indicated by ±; positive outcomes, +; negative outcomes, –; no reported outcomes,?. Modified with permission from Turk DC and Okifuji A. Treatment of chronic pain patients: clinical outcomes, cost-effectiveness, and cost-benefits of multidisciplinary pain centers. Critical Reviews in Physical and Rehabilitation Medicine 1998;10:181–208.
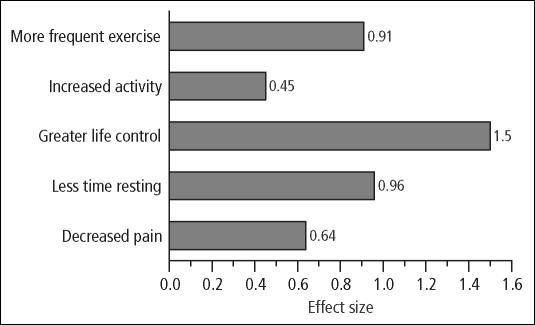
Our experience at the Center for Pain Management has been very similar to that of the other large clinical studies. In a recent review of outcome data, we examined the effect size of a 3-week pain management program. Effect size is a statistical technique designed to measure the significance of treatment as well as the meaningfulness or clinical impact of treatment. Patients demonstrated significant decrease in pain, decrease in time resting, increase in sense of life control, increase in activity levels, and increase in frequency of regular exercise (Figure). Effect size in these areas ranged from moderate to very large. In addition, we found that all patients had created a plan to manage their pain at discharge while only 23% of patients had a plan upon intake. Using the West Haven–Yale Multidimensional Pain Inventory, the percentage classified as “adaptive copers” increased from 15% at admission to 45% at discharge. Patient satisfaction was also quite high, as evidenced by 95% of graduates reporting that they would recommend the program to a friend.
Figure.
Effect size following interdisciplinary treatment (interpretation, 0.2 = small, 0.5 = moderate, and 0.8 = large).
COST-EFFECTIVENESS
In a recent study, Okifuji et al analyzed the cost benefits and cost-effectiveness of interdisciplinary pain management programs (7). Using existing data, they calculated the savings possible for 17,600 patients, the estimated number of patients treated annually in interdisciplinary pain management programs (Table 2). Cost savings were dramatic for persons who had been involved in interdisciplinary treatment programs: $260 million in 1-year posttreatment nonsurgical medical costs would be saved for individuals treated in interdisciplinary programs rather than with conventional or nonsurgical treatment. Patients treated in interdisciplinary programs would spend $280 million less for medical costs in the year following treatment and additional surgery than those treated conventionally. Similarly, annual savings for subsequent surgical costs would be approximately $63 million when patients were treated in an interdisciplinary program rather than surgically.
Table 2.
Cost comparisons among interdisciplinary pain centers, surgical treatment, and conventional medical treatment for an annual cohort of 17,600 patients
| Costs (millions) | |||||
| Treatment | Initial treatment | Subsequent Surgery | 1-year posttreatment (medical*) | Lifetime disability | Total |
| Interdisciplinary pain centers | $142.6 | $25.3 | $197.1 | $1835.3 | $2,200.4 |
| Surgical | $158.4 | $88.7 | N/A | N/A | |
| Conventional | $457.6 | $44.3 | $457.6 | $4,226.8 | $5186.4 |
*Medical treatment excludes surgical procedures
N/A indicates data not available for estimates. Modified from Lawrence Erlbaum Associates with permission.
Cost savings were much more dramatic when costs of lifetime disability benefits were included. When existing data were used regarding reduction of disability benefits for persons who had been involved in interdisciplinary treatment programs, cost savings approximated $2.5 billion over 20 years. When the loss of gainful employment was factored into this equation, the costeffectiveness of interdisciplinary treatment programs was even more dramatic. Using a cost-effective index ([improvement / the cost of treatment] × 100), Okifuji et al found that interdisciplinary treatment was 9 times more cost-effective than conservative treatment and 3.5 times more effective than surgical treatment in helping patients return to work.
SUMMARY
Complex problems require complex solutions. As we have seen, chronic pain syndromes are complex biopsychosocial phenomena that develop over time. Conventional medical strategies designed for acute pain are often unhelpful and costly if patients have developed more chronic pain problems. Research studies have suggested that an interdisciplinary team is more effective than either serial multidisciplinary treatments or fragmented approaches toward care. Fortunately, the cost of interdisciplinary care is relatively low. Okifuji et al noted that interdisciplinary pain centers “have been more rigorously examined than most other treatment modalities used with chronic pain patients. More data are available for the efficacy of … [these centers] … than for any surgical procedures or conventional medical treatment for chronic pain” (3). Although time consuming and costly, treatments received at interdisciplinary pain centers “result in greater clinical effectiveness and cost savings than the alternatives” (3).
References
- 1.Kerns RD, Turk DC, Rudy TE. The West Haven–Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 2.Flor H, Fydrich T, Turk DC. Efficacy of multidisciplinary pain treatment centers: a meta-analytic review. Pain. 1992;49:221–230. doi: 10.1016/0304-3959(92)90145-2. [DOI] [PubMed] [Google Scholar]
- 3.Okifuji AA, Turk DC, Kalauokalani D. Clinical outcomes and economic evaluation of the Multidisciplinary Pain Centers. In: Block A, Kremer EE, Fernandez E, editors. Handbook of Pain Syndromes. Mahwah, NJ: Lawrence Erlbaum Publishers; 1999. pp. 77–97. [Google Scholar]
- 4.Becker N, Sjogren P, Bech P, Olsen AK, Eriksen J. Treatment outcome of chronic non-malignant pain patients managed in a Danish multidisciplinary pain centre compared to general practice: a randomised controlled trial. Pain. 2000;84:203–211. doi: 10.1016/s0304-3959(99)00209-2. [DOI] [PubMed] [Google Scholar]
- 5.Turk DC, Okifuji A. Treatment of chronic pain patients: clinical outcomes, cost-effectiveness, and cost-benefits of multidisciplinary pain centers. Critical Reviews in Physical and Rehabilitation Medicine. 1998;10:181–208. [Google Scholar]