Abstract
Brucella abortus strain RB51 is an attenuated rough mutant used as the live vaccine against bovine brucellosis in the United States and other countries. We previously reported the development of strain RB51 as a bacterial vaccine vector for inducing Th1-type immune responses against heterologous proteins. Because safety concerns may preclude the use of strain RB51-based recombinant live vaccines, we explored the ability of a gamma-irradiated recombinant RB51 strain to induce heterologous antigen-specific immune responses in BALB/c mice. Exposure of strain RB51G/LacZ expressing Escherichia coli β-galactosidase to a minimum of 300 kilorads of gamma radiation resulted in complete loss of replicative ability. These bacteria, however, remained metabolically active and continued to synthesize β-galactosidase. A single intraperitoneal inoculation of mice with 109 CFU equivalents of gamma-irradiated, but not heat-killed, RB51G/LacZ induced a β-galactosidase-specific Th1-type immune response. Though no obvious differences were detected in immune responses to B. abortus-specific antigens, mice vaccinated with gamma-irradiated, but not heat-killed, RB51G/LacZ developed significant protection against challenge with virulent B. abortus. In vitro experiments indicated that gamma-irradiated and heat-killed RB51G/LacZ induced maturation of dendritic cells; however, stimulation with gamma-irradiated bacteria resulted in more interleukin-12 secretion. These results suggest that recombinant RB51 strains exposed to an appropriate minimum dose of gamma radiation are unable to replicate but retain their ability to stimulate Th1 immune responses against the heterologous antigens and confer protection against B. abortus challenge in mice.
Brucella abortus is a facultative, intracellular, gram-negative bacterial pathogen that can cause abortion in pregnant cattle and undulant fever in humans (6). Upon infection, B. abortus enters macrophage-monocyte lineage cells and multiplies within the phagosomes by inhibiting phagosome-lysosome fusion (7, 22). B. abortus strains exhibiting a smooth phenotype contain a surface-exposed O-polysaccharide chain (O antigen) as part of their lipopolysaccharide (LPS) structure (5). Truly rough strains do not contain O antigen in their LPS. Smooth LPS is a virulence factor of B. abortus, and therefore, rough strains are significantly less virulent than the smooth strains they were derived from (2, 19, 25, 31). The O antigen is also an immunodominant component of smooth B. abortus strains; infected animals develop antibodies to this antigen. However, as in most intracellular bacterial infections, cell-mediated immunity (CMI) plays a major role in acquired resistance to B. abortus infection. Hence, vaccination of cattle with live rough strains, such as B. abortus RB51, results in effective protection against brucellosis. B. abortus strain RB51 is an attenuated stable rough mutant derived from the virulent strain 2308 (25). Strain RB51 is currently used as the live vaccine of choice against bovine brucellosis in the United States and many other countries. Being a rough mutant, strain RB51 does not induce antibodies to the O antigen, thereby facilitating clear serological differentiation of vaccinated from infected animals. Vaccination with live strain RB51 results in a biased T-helper 1 (Th1)-specific immune response characterized by the induction of specific CD8+ cytotoxic T cells, CD4+ helper T cells that secrete gamma interferon (IFN-γ), and predominance of immunoglobulin G2a (IgG2a) isotype antigen-specific antibodies (11, 27, 28, 29, 30).
B. abortus is a potent stimulator of CMI. Heat-killed B. abortus promotes a strong Th1-type immune response and simultaneously inhibits primary as well as secondary Th2 immune responses (1, 26, 32). Studies performed with heat-killed B. abortus containing a chemically conjugated human immunodeficiency virus (HIV) peptide indicated that B. abortus can enhance cell-mediated immune responses, including cytotoxic CD8+ T lymphocytes, even in major histocompatibility complex class II-knockout mice, although these mice have low CD4+ T-cell numbers and defective CD4-dependent T-helper responses (9, 16). Interleukin-12 (IL-12) plays an important role in the induction of a Th1 immune response (21). In vivo studies showed that heat-killed B. abortus induces the secretion of IL-12 and tumor necrosis factor alpha (TNF-α) and identified dendritic cells (DCs) as a major source of IL-12 (13, 14). The LPS of B. abortus is 1,000-fold less toxic than the LPS of Escherichia coli (10). Taken together, these features form a strong basis for using B. abortus as a vaccine carrier to induce a Th1-biased immune response against specific antigens.
We are exploring the development of strain RB51 as a vaccine expression and delivery platform for the purpose of inducing a Th1-biased immune response against specific protein antigens. Previously, using a plasmid-based system, we have shown that strain RB51 can be engineered to express heterologous proteins, and mice vaccinated with such recombinant RB51 strains develop a strong Th1-type immune response to the foreign proteins (29). It is apparent that the use of live, recombinant RB51 strains for vaccination of a variety of animal species would be limited by safety concerns. Therefore, we are researching strategies to inactivate recombinant RB51 strains without interfering with the induction of Th1-type immune responses. In this study we examined the effect of two different modes of inactivation, heat treatment and gamma irradiation, on the induction of a heterologous antigen-specific immune response by a recombinant RB51 strain. Our studies demonstrated that strain RB51G/LacZ (a recombinant RB51 strain expressing β-galactosidase of E. coli) exposed to an appropriate minimum dose of gamma radiation remained metabolically active, continued to synthesize β-galactosidase, and was more effective than the heat-killed preparation in inducing IL-12 secretion from dendritic cells in vitro. Gamma-irradiated strain RB51G/LacZ was better than the heat-killed preparation in inducing β-galactosidase-specific Th1-type immune responses in mice after one immunization. Further, mice vaccinated with gamma-irradiated, but not heat-killed, strain RB51G/LacZ developed a significant level of resistance against virulent B. abortus strain 2308 challenge.
MATERIALS AND METHODS
Bacterial strains.
B. abortus strains RB51 and 2308 were from our culture collection. Generation of strain RB51G/LacZ was described previously (29). This strain harbors plasmid pBBgroE/lacZ, which contains the lacZ gene of E. coli expressed from the Brucella groE promoter. The bacteria were grown in tryptic soy broth (TSB) or tryptic soy agar (TSA) at 37°C as previously described (25). Strain RB51G/LacZ was grown in the presence of 30 μg/ml of chloramphenicol.
Vaccine preparation.
Strain RB51G/LacZ was grown in TSB with chloramphenicol to mid-log phase, and aliquots of 1 × 1011 CFU/ml were stored at −80°C until use. On the day of immunization, an aliquot of the vaccine was subjected to gamma irradiation using a 60Co source irradiator (Gammacell 220 irradiator). Another aliquot was subjected to heat killing by being incubated in a 65°C water bath for 30 min. The bacteria were washed several times with sterile saline before use in subsequent experiments. Irradiated and heat-killed vaccine preparations were confirmed to be nonviable by being plated on TSA plates.
β-Galactosidase enzyme assay.
β-Galactosidase was assayed in strain RB51G/LacZ per the previously described methods (20). Briefly, 100 μl of bacterial cells was added to 900 μl of Z buffer (6 mM Na2HPO4, 40 mM NaH2PO4, 10 mM KCl, 1 mM MgSO4, 50 mM β-mercaptoethanol) and permeabilized with 20 μl of chloroform and 10 μl of 0.1% sodium dodecyl sulfate. The contents were mixed by vortexing for 20 s and incubated for 5 min at room temperature. Two hundred microliters of substrate solution (4 mg of o-nitrophenyl-β-d-galactopyranoside per ml in Z buffer) was added, and the mixture was incubated for 3 min at room temperature before the reaction was stopped by adding 0.5 ml of 1 M Na2CO3. The solutions were centrifuged for 5 min at 15,000 × g, and the optical density was measured at A420.
Alamar Blue assay.
Live, irradiated, or heat-killed strain RB51G/LacZ suspensions were washed in saline solution and resuspended in TSB to the original concentration. In a 96-well flat-bottomed cell culture plate, 90 μl of bacterial suspension and 10 μl of Alamar Blue (Biosource International) were mixed and incubated at 37°C for 1 h. The change in color of the stain from blue to pink was considered positive for intact respiratory electron transport chain and metabolic activity (3).
Scanning electron microscopy.
Aliquots of 0.5 ml of freshly grown strain RB51G/LacZ cultures were subjected to heat killing or gamma irradiation. An aliquot without any treatment was used as a control. Each aliquot was then mixed with 0.5 ml of stock buffer (0.2 M sodium cacodylate buffer, pH 6.8, containing 4 mM magnesium chloride, 2 mM calcium chloride, 0.5% sodium chloride) and incubated for 10 min at room temperature. The bacterial cells were then spun down and resuspended in primary fixative (2.5% glutaraldehyde and 2% paraformaldehyde in stock buffer). Following 1 h of incubation, the bacteria were washed three times with 0.1 M stock buffer. Secondary fixation was done in 1% osmium oxide and 1.5% potassium ferricyanide for 1 h. The fixed bacteria were filtered onto 0.45-mm Millipore filter paper. The bacteria were sandwiched between filter papers and dehydrated in increasing concentrations of ethanol and then mounted on a 12-mm stub with double-side carbon tape, sputter coated with Au/Pd nanoparticles, and imaged with a NOVA NanoSEM microscope (FEI Company, Hillsboro, OR).
Mouse experiments.
Female BALB/c mice 4 to 6 weeks of age were injected intraperitoneally with 4 × 108 CFU of live or 4 × 109 CFU equivalents of irradiated or heat-killed strain RB51G/LacZ. As a negative control, one group of mice was injected with saline alone. Mice were bled at 3 weeks postinoculation (p.i.) to obtain sera for enzyme-linked immunosorbent assay (ELISA). Between 3 and 4 weeks p.i., three mice from each group were euthanized, and their splenocytes were used for in vitro culture to determine cytokine production upon stimulation with specific antigens. At 6 weeks p.i., five mice from each group were challenged by intraperitoneal inoculation of 2 × 104 CFU of B. abortus virulent strain 2308. After 2 weeks, all the challenged mice were euthanized and the bacterial burden in their spleens was determined as previously described (25).
Indirect ELISA.
The presence of serum IgG, IgG1, and IgG2a isotypes with specificity for β-galactosidase or strain RB51 antigen extract was determined by indirect ELISA. The antigens (β-galactosidase purchased from Sigma-Aldrich) and strain RB51 antigen extracts were prepared as previously described (28) and were diluted to a 5-μg/ml concentration in carbonate buffer (pH 9.6) and used to coat the wells of polystyrene plates (100 μl/well; Nunc-Immuno plate with a MaxiSorp surface). After overnight incubation at 4°C, the plates were washed four times in wash buffer (Tris-buffered saline at pH 7.4, 0.05% Tween 20) and blocked with 2% bovine serum albumin (BSA) in Tris-buffered saline. After 1 h at room temperature, the blocking solution was discarded, and the diluted mouse serum samples (1:100 dilutions in blocking solution) were added to the wells (50 μl/well). Each serum sample was tested in triplicate wells. The plates were incubated for 4 h at room temperature and washed four times, and isotype-specific goat anti-mouse horseradish peroxidase conjugates (Kirkegaard & Perry Laboratories, Gaithersburg, Md.) were added (50 μl/well) at an appropriate dilution. After 1 h of incubation at room temperature, the plates were washed four times, and 100 μl of substrate solution (TMB Microwell peroxidase substrate; Kirkegaard & Perry Laboratories, Gaithersburg, Md.) was added to each well. After 20 min of incubation at room temperature, the enzyme reaction was stopped by adding 100 μl of stop solution (0.185 M sulfuric acid), and the A450 was recorded with a microplate reader (Molecular Devices, Sunnyvale, CA).
Splenocyte cultures and cytokine quantification.
Splenocytes from the inoculated mice (three mice/group) were obtained according to methods previously described (28) and were cultured in the presence of different stimulants: 10 μg/ml of β-galactosidase, 107 CFU equivalents of heat-inactivated B. abortus RB51, or 10 μg/ml of a synthetic peptide, TPHPARIGL, representing the naturally processed H-2Ld-restricted epitope spanning amino acids 876 to 884 of β-galactosidase (8). In the case of the peptide stimulation, 50 U/ml of IL-2 was added to the wells. Cells with plain medium and cells stimulated with 2.5 μg/ml of concanavalin A (ConA) were used as the controls. The splenocytes were cultured for 72 h, and their supernatants were tested for IFN-γ, IL-5, and IL-10 by sandwich ELISA using BDOptEIASets (PharMingen, San Diego, Calif.). In these assays, the lower detection limits were 3.1 pg, 15.6 pg, and 31.3 pg per ml for IFN-γ, IL-5, and IL-10, respectively. The assays were performed in triplicate.
Generation of bone marrow-derived DCs.
DC cultures derived from the bone marrow of female 10- to 12-week-old BALB/c mice were prepared according to previously described methods (15, 18) with few modifications. Briefly, the femurs and tibias from 10- to 12-week-old BALB/c mice were collected in ice-cold Hanks' balanced salt solution with 50 μg/ml of gentamicin. The muscles were removed, and the ends of the bones were cut off with scissors and crushed. The bone marrow was flushed out with 2 to 3 ml of medium in a syringe with a 25-gauge needle. All bone marrow cells were collected and washed twice with Hanks' balanced salt solution. The cells were cultured in 10-cm petri dishes at a concentration of 5 × 105 cells/ml in a 10-ml volume. The cells were maintained at 37°C with 5% CO2 in RPMI 1640 supplemented with 5% fetal calf serum, 3% supernatant of J558L cells transferred with granulocyte-macrophage colony-stimulating factor (20 ng/ml), 2 mM l-glutamine, 0.05 μM β-mercaptoethanol, 100 U/ml penicillin, 100 μg/ml streptomycin, and 0.25 μg/ml amphotericin B. After 3 days the nonadherent cells were discarded and 10 ml of fresh medium was added. On day 5, 5 ml of medium was replaced with fresh medium. On day 7 an additional 5 ml of medium was added to the cells. On day 8 the cells were collected, washed, and resuspended in the medium without granulocyte-macrophage colony-stimulating factor, and they contained approximately 75 to 80% immature DCs as determined by flow cytometry.
Stimulation of dendritic cells with bacterial preparations.
Immature DCs were plated in medium at a density of 1 × 106/ml in 24-well plates (Costar) and either left untreated or stimulated by the addition of E. coli LPS at 100 ng/ml or irradiated or heat-killed strain RB51G/LacZ (1 × 106 CFU equivalents/ml). After 24 h of culturing in the presence of the stimulants, the cell culture supernatants were collected for cytokine quantification, and the cells were stained with different fluorochrome-conjugated antibodies to cell surface markers and subjected to flow cytometry analysis. In the supernatants, the concentrations of TNF-α, IL-10, and IL-12 (p40 subunit and the bioactive p70 form) were determined by sandwich ELISA using BDOptEIASets (PharMingen, San Diego, Calif.). The lower detection limits were 15.6 pg/ml for TNF-α and IL-12 p40 and 62.5 pg/ml for IL-12 p70. The assays were performed in triplicate.
Flow cytometric analysis.
Dendritic cells were washed in cold PBS and resuspended at a concentration of 5 × 106 to 10 × 106 cells/ml. One hundred microliters of cells was mixed with 100 μl of a 10% dilution of normal rabbit serum and 1% BSA in PBS for 15 min. The cells were then washed with 2 ml of flow buffer (0.5% BSA and 0.1% sodium azide in PBS). The DCs were stained for cell surface markers using anti-CD11c-fluorescein isothiocyanate, anti-CD40-phycoerythrin, biotin-conjugated anti-CD80 antibodies, or isotype-matched controls for 30 min in the dark. The cells were washed twice with 2 ml flow buffer, and the cells reacted with CD80 antibodies were stained with streptavidin-phycoerythrin for 20 min in the dark. All antibodies were obtained from BD PharMingen (San Diego, CA) and used at a concentration of 0.5 μg/106 cells. After final incubation, the cells were washed twice in flow buffer and fixed in 0.3 ml of 2% paraformaldehyde. Dual-color immunophenotyping of cell samples was performed on a Beckman Coulter Epics XL flow cytometer (Miami, Fla.). The data were analyzed using WinMDI software.
RESULTS
Effect of gamma radiation and heat treatment on the replication ability of strain RB51G/LacZ.
After aliquots of strain RB51G/LacZ were exposed to different doses of gamma radiation, the CFU present in each aliquot were determined by culturing on TSA plates. As shown in Fig. 1A, increased exposure to gamma radiation led to a gradual decrease in CFU of strain RB51G/LacZ and a total loss of replicative ability of the bacteria was observed at a minimum radiation dose of 300 kilorads. Incubation of strain RB51G/LacZ at 65°C for a minimum of 30 min resulted in complete loss of its replicative ability (Fig. 1B). Strain RB51G/LacZ aliquots exposed to 350 to 400 kilorads of gamma radiation or subjected to heat killing at 65°C for 30 min were used for vaccination of mice and in vitro immune response analyses.
FIG. 1.
Effect of gamma irradiation (A) and heat treatment (B) on the viability of strain RB51G/LacZ. Aliquots of strain RB51G/LacZ were exposed to different doses of gamma radiation or incubated at 65°C for 0, 15, and 30 min, and the viable bacteria in each aliquot were determined by plating 10-fold dilutions on TSA plates. Data are presented as means ± standard deviations of triplicate estimations.
Strain RB51G/LacZ exposed to gamma radiation remains metabolically active.
The metabolic activity of live, gamma-irradiated, and heat-killed strain RB51G/LacZ was tested using Alamar Blue dye. The Almar Blue dye undergoes reduction, and therefore a change in color from blue to pink, only in the presence of active energy metabolism where the reducing agents are generated in the cell through the electron transport chain (3). The live and gamma-irradiated bacteria remained metabolically active as seen by their ability to change Alamar Blue dye's color from blue to pink. Even the bacteria exposed to higher doses of gamma radiation, up to 1,200 kilorads, remained metabolically active (data not shown). However, the heat-killed bacteria failed to convert Alamar Blue color from blue to pink, indicating the loss of their metabolic activity (data not shown).
Scanning electron microscopy did not reveal any obvious structural damage to the bacteria exposed to 400 kilorads of gamma radiation. Except for the presence of some probable fragmented bacterial structural components, the heat-killed bacteria also did not show any apparent structural damage (Fig. 2).
FIG. 2.
Scanning electron micrographs of strain RB51G/LacZ without any treatment (live control) or after exposure to 350 kilorads of gamma radiation (irradiated) or heat treatment at 65°C for 30 min (heat killed). Arrows in the “heat-killed” panel show the probable fragmented bacterial components.
Expression of β-galactosidase by gamma-irradiated strain RB51G/LacZ.
To determine if de novo expression of β-galactosidase occurs in gamma-irradiated strain RB51G/LacZ, aliquots of live and irradiated bacteria were subjected to heat shock by being incubated at 42°C for 1 hour and analyzed for an increase in β-galactosidase activity. Prior to heat shock, both live and irradiated bacterial preparations exhibited similar levels of β-galactosidase activity. Following heat shock, the enzyme activity in both these preparations increased, indicating the up-regulation of the groE promoter and subsequent new synthesis of the foreign protein (Fig. 3). No β-galactosidase activity was detected in the heat-killed bacterial preparation (Fig. 3).
FIG. 3.
Increased expression of β-galactosidase in live and gamma-irradiated strain RB51G/LacZ following heat shock. Aliquots of the bacteria containing identical CFU were used directly or after exposure to 350 kilorads of gamma radiation or heat treatment at 65°C for 30 min. The β-galactosidase activity in each bacterial suspension was determined before (−) and after (+) subjection to heat shock. Three aliquots of each bacterial suspension were used for the enzyme assay. The data are presented as means ± standard deviations.
Induction of specific antibody responses.
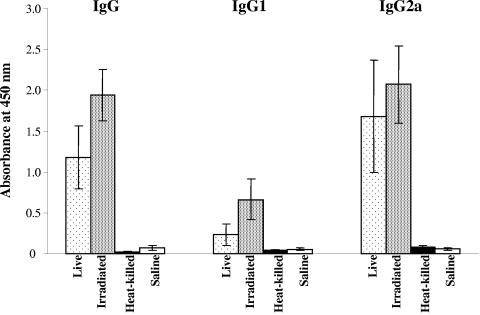
Development of antibodies specific to β-galactosidase and strain RB51 in the vaccinated mice was determined by ELISA. Serum from mice immunized with live and gamma-irradiated strain RB51G/LacZ contained significant levels of IgG specific to β-galactosidase. Assays with IgG2a- and IgG1-specific conjugates revealed that the β-galactosidase-specific IgG present in these mouse sera was predominantly of the IgG2a subisotype (Fig. 4); the IgG1 subisotype was present in low levels. No β-galactosidase-specific IgG was detected in serum from mice inoculated with heat-killed strain RB51G/LacZ or saline alone.
FIG. 4.
ELISA detection of β-galactosidase-specific IgG, IgG1, and IgG2a in serum of mice inoculated with live, gamma-irradiated, and heat-treated strain RB51G/LacZ or inoculated with saline alone. Sera collected from three mice of each group at 3 weeks postinoculation were diluted 1 in 100 and assayed for the presence of specific antibodies. Results are shown as means ± standard deviations of absorbance at 450 nm of the color developed.
Mice in all groups, except the saline-inoculated one, developed similar concentrations of antibodies specific to the antigens of strain RB51 (data not shown). Again, these antibodies were predominantly of the IgG2a subisotype but not IgG1.
Induction of specific CMI responses.
Specific CMI responses of the vaccinated mice were determined by quantification of IFN-γ, IL-5, and IL-10 secreted by the splenocytes upon in vitro stimulation with the antigens. When stimulated with intact β-galactosidase or the specific H-2Ld-restricted β-galactosidase peptide, splenocytes from mice inoculated with live and gamma-irradiated strain RB51G/LacZ secreted higher amounts of IFN-γ than the splenocytes from mice inoculated with heat-killed bacteria (Table 1). Splenocytes from all groups, except the saline-inoculated one, secreted similarly high levels of IFN-γ upon stimulation with strain RB51 antigens. After stimulation with specific antigens, no IL-5 and IL-10 were detected in any culture supernatants, while splenocytes from all groups produced similarly high amounts of IFN-γ, IL-5, and IL-10 upon mitogen stimulation with ConA (data not shown).
TABLE 1.
Production of IFN-γ secreted by splenocytes of immunized and saline-inoculated mice after in vitro stimulation with specific antigens
| Stimulant | Concn (pg/ml) of IFN-γ secreted by in vitro-stimulated splenocytes of micea
|
|||
|---|---|---|---|---|
| Inoculated with saline | Immunized with:
|
|||
| Live RB51G/LacZ | Irradiated RB51G/LacZ | Heat-killed RB51G/LacZ | ||
| Medium | —b | — | — | — |
| ConA | >2,000 | >2,000 | >2,000 | >2,000 |
| Heat-killed RB51 | 20 ± 0.1 | >2,000 | >2,000 | >2,000 |
| β-Galactosidase | — | 816 ± 80.2* | 723.8 ± 57.4* | 129.4 ± 79.1c |
| β-Galactosidase peptide | — | 398 ± 91.7** | 818.5 ± 388.8** | — |
Values are means ± standard deviations (n = 3). Means with the same number of asterisks were not significantly different from each other by Student's t test (P > 0.1).
—, below the level of detection.
Significantly different from means with one asterisk (P < 0.05).
Protection against virulent B. abortus challenge.
Two weeks after challenge, mice immunized with gamma-irradiated or live strain RB51G/LacZ contained significantly lower numbers of bacteria in their spleen than did the saline-inoculated control group of mice (Table 2). In contrast, the splenic bacterial burden of mice immunized with heat-killed strain RB51G/LacZ was similar to that of the saline group. These data indicate that gamma-irradiated, but not heat-killed, strain RB51G/LacZ can stimulate the development of protective immunity against challenge with B. abortus virulent strain 2308.
TABLE 2.
Protection against B. abortus 2308 challenge in the vaccinated mice.
| Immunization | Saline | RB51G/LacZ
|
||
|---|---|---|---|---|
| Live | Irradiated | Heat-killed | ||
| No. of bacteria/spleen (log10 CFU ± SD) | 5.35 ± 0.15 | 4.25 ± 0.25a | 4.5 ± 0.2a | 5.4 ± 0.10 |
| Log U of protection | 1.1 | 0.85 | −0.05 | |
Significantly different from the saline group by Student's t test (P < 0.05).
Maturation and cytokine production by in vitro-stimulated dendritic cells.
After 24 h of culture immature bone marrow-derived dendritic cells in the presence of heat-treated or gamma-irradiated RB51G/LacZ resulted in maturation with similar extents of expression of costimulatory molecules CD40 and CD80 (Fig. 5). However, supernatants from the cultures stimulated with irradiated RB51G/LacZ contained higher amounts of IL-12 p40 and IL-12 p70 than those stimulated with heat-killed RB51G/LacZ (Table 3). The heat-killed, but not irradiated, bacteria induced low levels of TNF-α secretion from the maturing dendritic cells. However, the two bacterial preparations induced similar levels of IL-10 secretion. Culture supernatants of dendritic cells stimulated with E. coli LPS contained all the cytokines tested (Table 3).
FIG. 5.
Flow cytometric evaluation of CD11c, CD40, and CD80 expression on bone marrow-derived dendritic cells following in vitro stimulation with gamma-irradiated (IR) and heat-treated (HK) strain RB51G/LacZ or LPS of E. coli. Thin lines, labeling with isotype control antibody. Thick lines, labeling with specific antibody.
TABLE 3.
Production of specific cytokines by bone marrow-derived dendritic cells after in vitro stimulation with specific antigens
| Stimulant | Concn of cytokine secreted by dendritic cells (pg/ml)a
|
|||
|---|---|---|---|---|
| IL-12 p40 | IL-12 p70 | IL-10 | TNF-α | |
| Medium | —b | — | 41.9 ± 0.1 | — |
| E. coli LPS | 400.7 ± 2.9 | 451.4 ± 65.8 | 1,255.7 ± 7.8 | 388.2 ± 43.8 |
| Irradiated RB51G/LacZ | 580.1 ± 79.3* | 481.7 ± 10.2** | 126.6 ± 3.9 | — |
| Heat-killed RB51G/LacZ | 329.5 ± 39.9* | 201.8 ± 16.3** | 119.1 ± 2.6 | 24.0 ± 0.6 |
Values are means ± standard deviations. There were significant differences between means with the same number of asterisks by Student's t test (P < 0.05).
—, below the level of detection.
DISCUSSION
Exposure of strain RB51G/LacZ to a minimum dose of 300 kilorads of gamma radiation completely abolished the bacteria's ability to replicate. However, even after exposure to higher doses of radiation (up to 1,200 kilorads), the gamma-irradiated bacteria remained metabolically active as demonstrated by the Alamar Blue assay. This finding was not unexpected since gamma radiation at the doses tested mainly damages DNA and RNA. In strain RB51G/LacZ, the expression of β-galactosidase was achieved through transformation with a plasmid containing the lacZ gene under the Brucella groE promoter. The groE promoter is up-regulated under stressful conditions, including heat shock (17, 29). Exploiting this promoter feature, we examined if continued expression of β-galactosidase occurred in the gamma-irradiated bacteria. Interestingly, only the bacteria exposed to 300 to 400 kilorads of gamma radiation, but not those exposed to higher doses (>800 kilorads; data not shown), exhibited increased β-galactosidase activity following heat shock, suggesting that the groE promoter and the lacZ gene present on the plasmid were undamaged by the low dose of radiation. To the best of our knowledge, no studies have been published documenting the dosage effect of ionizing radiation on plasmid-carried gene expression in bacteria. However, previous studies show that bacteria exposed to appropriate doses of gamma irradiation are unable to replicate but sustain the multiplication of plasmids (24). In addition, protozoal parasites, such as Toxoplasma gondii, exposed to very low doses of gamma radiation remain metabolically active and continue to synthesize proteins but lose their ability to replicate (12).
The gamma-irradiated strain RB51G/LacZ was more efficient than the heat-killed preparation in inducing a β-galactosidase-specific Th1-type immune response. In the vaccinated mice, the development of a Th1-type response was demonstrated by the detection of predominantly IgG2a, but not IgG1, antibodies specific to β-galactosidase in the serum as well as by the secretion of IFN-γ, but not IL-5, by the splenocytes of vaccinated mice upon in vitro stimulation with specific antigens. The secretion of IFN-γ by splenocytes upon stimulation with the H-2Ld-restricted peptide of β-galactosidase suggests the development of antigen-specific CD8+ T cells in the vaccinated mice. The levels of β-galactosidase-specific immune responses detected in mice inoculated with the irradiated strain RB51G/LacZ were similar to those detected in mice that received the live bacteria. However, this comparison may not be appropriate since the irradiated bacteria were inoculated at a higher dose than the live bacteria (109 CFU equivalents of irradiated bacteria and 108 CFU of the live bacteria). Our initial studies with 108 CFU equivalents of the irradiated strain did not result in the induction of significant levels of β-galactosidase-specific immune responses. Moreover, unlike the irradiated bacteria, the live bacteria do replicate to some extent in mice; in BALB/c mice inoculated with 108 CFU of live strain RB51G/LacZ, the bacteria persist for at least 4 weeks (29). How this prolonged persistence of the live bacteria contributes to the total β-galactosidase antigen load in the mice is not known. Since mice inoculated with 109 CFU of live strain RB51G/LacZ die within 3 to 4 days, we could not use this higher dose for the comparison. All mice that received 109 CFU equivalents of irradiated or heat-killed strain RB51G/LacZ remained healthy throughout the study and did not show any signs of toxicity.
Gamma-irradiated and heat-killed bacteria induced comparable levels of immune responses against the antigens of strain RB51. This is in sharp contrast to the β-galactosidase-specific immune responses detected in these mice, where the heat-treated bacteria failed to induce significant levels of antibody and CMI responses to β-galactosidase. This might suggest that the amount of β-galactosidase antigen present in the heat-treated bacteria is not sufficient to induce an immune response after one inoculation. However, when tested by Western blotting, immediately after irradiation and heat treatment, the two bacterial preparations contained similar amounts of the β-galactosidase antigen (data not shown). Since the gamma-irradiated bacteria, unlike the heat-treated bacteria, continue to synthesize β-galactosidase, it is possible that the mice inoculated with the irradiated bacteria were exposed to more antigen. In addition, the β-galactosidase synthesis by the gamma-irradiated strain RB51G/LacZ might have increased after the bacteria entered the host macrophages. In support of this possibility, our in vitro experiments indicated that, following heat shock, the expression of β-galactosidase increased in strain RB51G/LacZ exposed to 350 to 400 kilorads of gamma radiation (Fig. 3). It is known that, similar to heat shock response, the groE promoter is up-regulated during intracellular localization of the bacteria (17, 29). Therefore, the observed differences in β-galactosidase-specific immune responses between the mice inoculated with gamma-irradiated bacteria and those inoculated with heat-treated bacteria could be mainly because of the amount of antigen exposure.
Immunization of mice with gamma-irradiated strain RB51G/LacZ conferred a significant level of protection against virulent B. abortus challenge. In contrast, immune responses induced by the heat-killed strain RB51G/LacZ were not protective. Nevertheless, no apparent differences were observed in the level or type of strain RB51-specific immune responses induced by these two preparations. Since our immune response analyses were carried out using whole antigens of strain RB51, we may have failed to detect differences in immune responses specific to individual antigens that play a major role in the protective mechanisms. It is possible that, like β-galactosidase expression, the gamma-irradiated bacteria are capable of synthesis of some strain RB51 proteins, leading to the induction of enhanced immune responses to these proteins.
Since induction of the observed Th1-type immune response begins with interaction between the antigen and the antigen-presenting cells, we examined the effect of gamma-irradiated and heat-killed strain RB51G/LacZ on dendritic cells. No significant difference was found between the two bacterial preparations with regard to their ability to induce maturation of the dendritic cells as shown by the expression of CD80 and CD40. However, gamma-irradiated bacteria induced more IL-12 secretion by the dendritic cells. It is noteworthy that IL-12 is a key cytokine necessary for the development of Th1-type immune responses (21). Dendritic cells stimulated with the heat-killed, but not irradiated, bacteria secreted detectable levels of TNF-α. Previous studies indicated that gamma irradiation reduces the endotoxicity of LPS from gram-negative bacteria (4, 23). It remains to be tested if the observed lack of TNF-α secretion by dendritic cells stimulated with the gamma-irradiated bacteria was because of the reduction in LPS endotoxicity of strain RB51G/LacZ after exposure to gamma radiation.
In conclusion, the results demonstrate the effectiveness of using optimal minimum-dose radiation exposure to abolish the replication capacity of recombinant B. abortus RB51 strains without affecting their ability to induce heterologous antigen-specific Th1-type immune responses and protective immunity against virulent B. abortus after just one immunization. The complete loss of replication ability of the vector should make it safer for use as a recombinant vaccine delivery system. In addition, gamma-irradiated strain RB51 may be a safer alternative to the live vaccine for inducing protective immunity against Brucella infections.
Acknowledgments
This work was partially supported by Public Health Service grant AI053431-01A1 from the National Institute of Allergy and Infectious Diseases to R.V. and H.H.
REFERENCES
- 1.Agranovich, I., D. E. Scott, D. Terle, K. Lee, and B. Golding. 1999. Down-regulation of Th2 responses by B. abortus, a strong Th1 stimulus, correlates with alterations in the B7.2-CD28 pathway. Infect. Immun. 67:4418-4426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allen, C. A., L. G. Adams, and T. A. Ficht. 1998. Transposon-derived Brucella abortus rough mutants are attenuated and exhibit reduced intracellular survival. Infect. Immun. 66:1008-1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker, C. N., S. N. Banerjee, and F. C. Tenover. 1994. Evaluation of Alamar colorimetric MIC method for antimicrobial susceptibility testing of gram-negative bacteria. J. Clin. Microbiol. 32:1261-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bandekar, J. R., and D. P. Nerkar. 1987. Antitumor activity of lipopolysaccharide and radio-detoxified lipopolysaccharide of Vibrio parahaemolyticus. Microbiol. Immunol. 31:675-681. [DOI] [PubMed] [Google Scholar]
- 5.Cherwonogrodzky, J. W., G. Dubray, E. Moreno, and H. Mayer. 1990. Antigens of Brucella, p. 19-64. In K. Nielsen and J. R. Duncan (ed.), Animal brucellosis. CRC Press, Inc., Boca Raton, Fla.
- 6.Corbel, M. J. 1997. Brucellosis: an overview. Emerg. Infect. Dis. 3:213-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frenchick, P. J., R. J. Markham, and A. H. Cochrane. 1985. Inhibition of phagosome-lysosome fusion in macrophages by soluble extracts of virulent Brucella abortus. Am. J. Vet. Res. 46:332-335. [PubMed] [Google Scholar]
- 8.Gavin, M. A., M. J. Gilbert, S. R. Riddell, P. D. Greenberg, and M. J. Bevan. 1993. Alkali hydrolysis of recombinant proteins allows for the rapid identification of class I MHC-restricted CTL epitopes. J. Immunol. 151:3971-3980. [PubMed] [Google Scholar]
- 9.Golding, B., J. Inman, P. Highet, R. Blackburn, J. Manischewitz, and N. Blyveis. 1995. Brucella abortus conjugated with a gp120 or V3 loop peptide derived from human immunodeficiency virus (HIV) type 1 induces neutralizing anti-HIV antibodies, and the V3-B. abortus conjugate is effective even after CD4+ T-cell depletion. J. Virol. 69:3299-3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein, J., T. Hoffman, C. Frasch, E. F. Lizzio, P. R. Beining, D. Hochstein, Y. L. Lee, R. D. Angus, and B. Golding. 1992. Lipopolysaccharide (LPS) from Brucella abortus is less toxic than that from Escherichia coli, suggesting the possible use of B. abortus or LPS from B. abortus as a carrier in vaccines. Infect. Immun. 60:1385-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.He, Y., R. Vemulapalli, A. Zeytun, and G. G. Schurig. 2001. Induction of specific cytotoxic lymphocytes in mice vaccinated with Brucella abortus RB51. Infect. Immun. 69:5502-5508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hiramoto, R. M., A. J. Galisteo, N. do Nascimento, and H. F. de Andrade, Jr. 2002. 200 Gy sterilised Toxoplasma gondii tachyzoites maintain metabolic functions and mammalian cell invasion, eliciting cellular immunity and cytokine response similar to natural infection in mice. Vaccine 20:2072-2081. [DOI] [PubMed] [Google Scholar]
- 13.Huang, L. Y., J. Aliberti, C. A. Leifer, D. M. Segal, A. Sher, D. T. Golenbock, and B. Golding. 2003. Heat-killed Brucella abortus induces TNF and IL-12p40 by distinct MyD88-dependent pathways: TNF, unlike IL-12p40 secretion, is Toll-like receptor 2 dependent. J. Immunol. 171:1441-1446. [DOI] [PubMed] [Google Scholar]
- 14.Huang, L. Y., C. Reis e Sousa, Y. Itoh, J. Inman, and D. E. Scott. 2001. IL-12 induction by a TH1-inducing adjuvant in vivo: dendritic cell subsets and regulation by IL-10. J. Immunol. 167:1423-1430. [DOI] [PubMed] [Google Scholar]
- 15.Inaba, K., M. Inaba, N. Romani, H. Aya, M. Deguchi, S. Ikehara, S. Muramatsu, and R. M. Steinman. 1992. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J. Exp. Med. 176:1693-1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lapham, C., B. Golding, J. Inman, R. Blackburn, J. Manischewitz, P. Highet, and H. Golding. 1996. B. abortus conjugated with a peptide derived from the V3 loop of human immunodeficiency virus (HIV) type 1 induces HIV-specific cytotoxic T-cell responses in normal and in CD4+ cell-depleted BALB/c mice. J. Virol. 70:3084-3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin, J., and T. A. Ficht. 1995. Protein synthesis in Brucella abortus induced during macrophage infection. Infect. Immun. 63:1409-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lutz, M. B., N. Kukutsch, A. L. Ogilvie, S. Rossner, F. Koch, N. Romani, amd G. Schuler. 1999. An advanced culture method for generating large quantities of highly pure dendritic cells from mouse bone marrow. J. Immunol. Methods 223:77-92. [DOI] [PubMed] [Google Scholar]
- 19.McQuiston, J. R., R. Vemulapalli, T. J. Inzana, G. G. Schurig, N. Sriranganathan, D. Fritzinger, T. L. Hadfield, R. A. Warren, Luther E. Lindler, N. Snellings, D. Hoover, S. M. Halling, and S. M. Boyle. 1999. Genetic characterization of a Tn5-disrupted glycosyltransferase gene homolog in Brucella abortus and its effect on lipopolysaccharide composition and virulence. Infect. Immun. 67:3830-3835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller, J. H. 1992. A short course in bacterial genetics: a laboratory manual and handbook for Escherichia coli and related bacteria. Cold Spring Harbor Laboratory, Cold Spring Harbor, N.Y.
- 21.O'Garra, A., and N. Arai. 2000. The molecular basis of T helper 1 and T helper 2 cell differentiation. Trends Cell Biol. 10:542-550. [DOI] [PubMed] [Google Scholar]
- 22.Pizarro-Cerda, J., E. Moreno, V. Sanguedolce, J. L. Mege, and J. P. Gorvel. 1998. Virulent Brucella abortus prevents lysosome fusion and is distributed within autophagosome-like compartments. Infect. Immun. 66:2387-2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Previte, J. J., Y. Chang, and H. M. el-Bisi. 1967. Detoxification of Salmonella typhimurium lipopolysaccharide by ionizing radiation. J. Bacteriol. 93:1607-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Radford, A. J., D. G. MacPhee, and D. C. Reanney. 1983. Preparation of plasmid DNA by gamma-irradiation of recA cells. Plasmid 10:229-302. [DOI] [PubMed] [Google Scholar]
- 25.Schurig, G. G., R. M. Roop II, T. Bagchi, S. M. Boyle, D. Buhrman, and N. Sriranganathan. 1991. Biological properties of RB51: a stable rough strain of Brucella abortus. Vet. Microbiol. 28:171-188. [DOI] [PubMed] [Google Scholar]
- 26.Scott, D. E., I. Agranovich, J. Inman, M. Gober, and B. Golding. 1997. Inhibition of primary and recall allergen-specific T-helper cell type 2-mediated responses by a T-helper cell type 1 stimulus. J. Immunol. 159:107-116. [PubMed] [Google Scholar]
- 27.Vemulapalli, R., S. Cravero, C. L. Calvert, T. E. Toth, N. Sriranganathan, S. M. Boyle, O. L. Rossetti, and G. G. Schurig. 2000. Characterization of specific immune responses of mice inoculated with recombinant vaccinia virus expressing an 18-kDa outer membrane protein of B. abortus. Clin. Diagn. Lab. Immunol. 7:114-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vemulapalli, R., A. J. Duncan, S. M. Boyle, N. Sriranganathan, T. E. Toth, and G. G. Schurig. 1998. Cloning and sequencing of yajC and secD homologs of Brucella abortus and demonstration of immune responses to YajC in mice vaccinated with B. abortus RB51. Infect. Immun. 66:5684-5691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vemulapalli, R., Y. He, S. M. Boyle, N. Sriranganathan, and G. G. Schurig. 2000. Brucella abortus strain RB51 as a vector for heterologous protein expression and induction of specific Th1-type immune responses. Infect. Immun. 68:3290-3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vemulapalli, R., Y. He, S. Cravero, N. Sriranganathan, S. M. Boyle, and G. G. Schurig. 2000. Overexpression of protective antigen as a novel approach to enhance vaccine efficacy of Brucella abortus strain RB51. Infect. Immun. 68:3286-3289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Winter, A. J., G. G. Schurig, S. M. Boyle, N. Sriranganathan, J. S. Bevins, F. M. Enright, P. H. Elzer, and J. D. Kopec. 1996. Protection of BALB/c mice against homologous and heterologous species of Brucella by rough strain vaccines derived from Brucella melitensis and Brucella suis biovar 4. Am. J. Vet. Res. 57:677-683. [PubMed] [Google Scholar]
- 32.Zaitseva, M. B., H. Golding, M. Betts, M. A. Yamauchi, E. T. Bloom, L. E. Butler, L. Stevan, and B. Golding. 1995. Human peripheral blood CD4+ and CD8+ T-cells express Th1-like cytokine mRNA and proteins following in vitro stimulation with heat-inactivated Brucella abortus. Infect. Immun. 63:2720-2728. [DOI] [PMC free article] [PubMed] [Google Scholar]