Abstract
This paper presents a theoretical model of bottle feeding readiness in preterm infants, which hypothesizes relationships between bottle feeding readiness, experience, and outcomes. The synactive theory of development provided the conceptual foundation for the model. The model, which is currently being tested, is designed to establish bottle feeding readiness criteria that will help nurses decide when to offer a bottle to a preterm infant The model may also provide a useful framework for determining preterm infant readiness for other aspects of care.
Keywords: preterm infants, infant feeding, theoretical model
A MODEL OF FEEDING READINESS FOR PRETERM INFANTS
Although breastfeeding presents fewer physiologic challenges than bottle feeding to growing preterm infants (Aguayo, 2001), many of these infants are bottle fed either formula or expressed breast milk (Pinelli, Atkinson, & Saigal, 2001). Achieving competence at bottle feeding takes time, with the transition from gavage to full bottle feedings reported to last 10 to 14 days (Pickler, Mauck, & Geldmaker, 1997).
Helping the preterm infant achieve bottle feeding competence is a primary responsibility of nurses (Kinneer & Beachy, 1994) yet, there are no universally accepted criteria for determining when an infant is ready to be fed a bottle. Consequently; already vulnerable infants are subject to a trial-and-error approach to this most complex and critical activity, with potentially harmful immediate consequences such as apnea, bradycardia, hypoxia, fatigue, and agitation (Shaker, 1999), as well as long term consequences such as delayed oral feeding and increased length of hospitalization (Schanler, Shulman, Lau, Smith, & Heitkemper, 1999).
“Contingent caregiving,” i.e., providing care when the infant indicates readiness to receive care, has been reported to have positive effects on immediate neurobehavioral responses and on long-term developmental outcomes (Als & Gilkerson, 1995; Als, Duffy, & McAnulty, 1996; Becker, Grunwald, Moorman, & Stuhr, 1993; Fleisher et al., 1995), Bottle feeding is an activity that seems especially amenable to contingent caregiving and recent research supports the use of “demand” or “self-regulatory” behaviors as indicators for bottle feeding (McCain & Gartside, 2002; Pridham et al., 2001), However, no reported studies have examined the complex relationships among the neurologic, physiologic, and behavioral components of feeding readiness or the relationship of infants’ feeding experiences to readiness and outcomes in preterm infants.
The model presented in this paper (Figure 1) hypothesizes that bottle feeding outcomes can be predicted from bottle feeding readiness. Bottle feeding readiness for any specific bottle feeding is based on: 1) neurologic maturation; 2) severity of illness; and 3) pre-feeding autonomic, motor, and behavioral state organization. Bottle feeding outcomes, the results of a bottle feeding, are defined as: 1) during-feeding autonomic, motor, and behavioral state organization; 2) suck-swallow-breathe coordination; 3) feeding performance; and 4) after-feeding autonomic, motor, and behavioral state organization. Bottle feeding experience, defined as opportunities for, and “success” at, bottle feeding, is considered to be positively related to both bottle feeding readiness and bottle feeding outcomes. This model, which is currently being tested, provides a foundation for establishing empirically supported bottle feeding readiness criteria for clinical practice.
Figure 1.
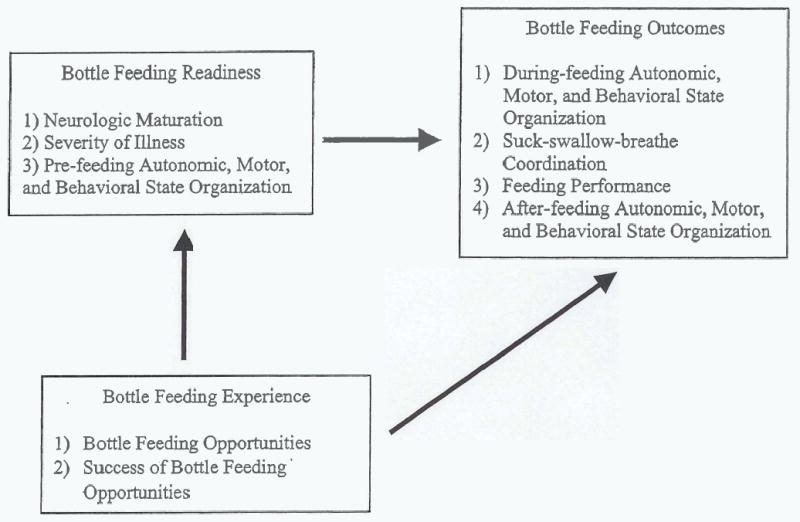
Model of feeding readiness for preterm infants
CONCEPTUAL PERSPECTIVE
The synactive theory of development provides the basis for the model (Als & Brazelton, 1981). The theory posits that preterm infants interact with and adapt to their environment through the integrated activity of four subsystems — autonomic, motor, behavioral, and attentional. At the core of the theory is self-regulation, fee achievement of a balanced, stable integration of the subsystems. Thus, all autonomic, motor, and behavioral activity is driven by the infant's internal need to self-regulate, The synactive theory suggests that caregivers of preterm infants can assist infants to meet self-regulatory goals by providing care contingent upon the infant's own behaviors.
The autonomic subsystem involves organization of heart and respiratory rate and rhythm. The infant must gain control over autonomic functioning first, since the ability to achieve and maintain control in other areas depends on the smooth and reliable function of autonomic mechanisms. Bottle feeding stresses the fragile organization of the preterm infant's autonomic subsystem, and infants with poor organization have difficulty bottle feeding.
The motor subsystem involves the ability to achieve and maintain muscle tone, posture, and smooth body movement An infant with poor motor organization may have difficulty bottle feeding, while the act of bottle feeding itself costs a preterm infant in terms of energy expenditure. Hence, an infant may become disorganized by a bottle feeding.
The behavioral subsystem is reflected in the infant's level of wakefulness — from sleep state to full arousal, and in the pattern of behavior state transitions. A quiet alert state at feeding has been correlated with improved bottle feeding outcomes (McCain, Gartside, Greenberg, & Lott, 2001). However, bottle feeding tends to tax the infant, possibly resulting in restless or agitated behavior states.
Although the feeding readiness model is not a test of synactive theory, the model considers before the feeding, during the feeding and after the feeding autonomic, motor, and behavior state organization. Additionally, the relationships of these variables to other components of bottle feeding readiness and outcomes are taken into account
BOTTLE FEEDING READINESS
Though mechanisms of bottle feeding have been studied extensively, decisions about bottle feeding readiness continue to be made using untested “criteria.” A survey of 576 neonatal intensive care units found that fewer than 50% had specific policies for the initiation of bottle or breast feeding. Many nurseries relied on unwritten guidelines for initiating bottle feedings that included the infant's post-conceptional age (PCA), weight, and developmental and maturational characteristics (Sidell & Froman, 1994). In another survey, however, neonatal intensive care nurses ranked behavioral and physiologic factors higher than physical factors in deciding whether to initiate bottle feedings for preterm infants (Kinneer et al., 1994). The ability to suck nonnutritively was the most important behavioral factor, and gagging with gavage tube insertion was the most important physiological factor in the nurses' decisions. The most important physical factor in decision-making was the infant's PCA. Still other researchers have found that the decision to begin bottle or breast feedings is based on prenatal history, presence of ventilator or other mechanical support, and complicating disorders, in addition to birth weight and gestational age (Romero & Kleinman, 1993).
Although these characteristics may be useful, survey results do not provide empirical evidence of their ability to predict feeding outcomes. Moreover, the characteristics do not account for the many and subtle changes that influence a preterm infant's ability to bottle feed at any particular feeding. Readiness is often defined as maturational readiness to begin the oral, bottle feeding process rather than readiness to feed from a bottle when it is offered. The literature suggests that several factors contribute to a preterm infant's readiness to do the latter - to feed from a bottle when it is offered. These factors include neurologic maturation, severity of illness, and ability to organize autonomic, motor, and behavioral state systems from feeding to feeding.
NEUROLOGIC MATURATION
Neurological immaturity is evident in the preterm infant's inability to successfully bottle feed Sucking activity is a reflection of increased neurologic maturation in preterm infants (Medoff-Cooper, Verklan, & Carlson, 1993), and bottle feeding, the most highly organized behavior of the young infant, involves the coordination of sucking, swallowing, and breathing. Although swallowing and sucking have been observed in utero as early as 13 and 18 weeks gestation, respectively, the coordination of the two usually does not occur before 32 to 34 weeks gestation (Bu'Lock, Woolridge, & Baum, 1990). Coordination of sucking and swallowing with breathing typically occurs even later, at 37 weeks gestation (Mathew, 1988). However, the “transition time” from gavage to bottle feeding has decreased significantly over the last 10 years (Pridham et al., 1998), and most neonatal centers initiate bottle feedings before coordination is present This probably reflects the fact that PCA is only a general indicator of successful feeding; many preterm infants can successfully bottle feed before 37 weeks post-conceptional age.
SEVERITY OF ILLNESS
The effects of illness severity, or morbidity, complicate the already complex process of bottle feeding. Morbidity has been found to account for 12% of the variance in PCA at first bottle feeding and 42% of the variance in PCA at complete bottle feedings in preterm infants (Pickler et al., 1997). Ventilatory support, in particular, is related to delays in achievement of feeding milestones (Bier, Ferguson, Cho, Oh, & Vohr, 1993), and oxygen use itself contributes to delayed achievement of feeding milestones (Pridham, Sondel, Chang, & Green, 1993) (Becker et al., 1993). The occurrence of apnea without mechanical ventilation or oxygen support also delays the achievement of bottle feeding milestones in preterm infants (Mandich, Ritchie, & Mullett, 1996).
While respiratory disorders, particularly those requiring oxygen or ventilator use, contribute most to delays in bottle feeding onset and progress, other medical complications, including infection, can also delay the transition from gavage to bottle feedings (Bazyk, 1990). Thus, a number of illness parameters need to be considered when examining feeding readiness.
PRE-FEEDING AUTONOMIC, MOTOR, AND BEHAVIORAL STATE ORGANIZATION
Bottle feeding is a physiologically challenging activity for preterm infants because of their neurologic immaturity, difficulty in regulating autonomic functions, and difficulty in achieving behavioral state organization when presented with stimuli. Immature feeding ability causes physiological distress, exhibited as bradycardia or heart rate variations, and changes in respiratory patterns, exhibited as apnea, nasal flaring, or hypoxemia (Poets, Langner, & Bohnhorst, 1997). Behavioral reactions to adverse feeding effects include fatigue, agitation, and disorganization (VandenBerg, 1990). Thus, immature cardiorespiratory and neurobehavioral control leads to poor bottle feeding performance (Daniels, Devlieger, Minami, Eggermont, & Casaer, 1990).
The difficulties of bottle feeding for preterm infants are related to the mechanical complexity of the process. The act requires a somewhat organized pattern of sucking, swallowing, and breathing. As the infant sucks, liquid fills the mouth and triggers swallowing. While the infant swallows, respiration is suppressed, and the infant's level of oxygenation declines. Even though the infant may attempt to take additional breaths, breathing may remain obstructed for several seconds after the swallow is completed (Koenig, Davies, & Thach, 1990). Given the physiological distress associated with bottle feeding, it is logical to assume that the more stable the infant's autonomic state, the more likely it is that the infant can feed with success though that assumption remains untested.
Motor organization is related to autonomic organization. Preterm infants exhibit clusters of “behaviors” that perhaps indicate readiness for feeding, including fussiness without crying, hand-to-mouth activity, rooting, and hiccups (Cagan, 1995). However, the relationship of these clustered behaviors to feeding readiness and outcomes has not been examined.
The relationship between behavior state and feeding readiness in preterm infants has been frequently studied. A pre-feeding quiet, alert state has been associated with greater bottle feeding success (Pickler, Frankel, Walsh, & Thompson, 1996), and several studies have documented the effectiveness of pre-feeding nonnutritive sucking in achieving this optimal (McCain, 1992; McCain, 1997; McCain et al., 2002b). However, preterm infants can achieve this state without the assistance of nonnutritive sucking. In fact, the only states in which feeding seems contraindicated are deep sleep and fussy crying.
To date, no studies have examined the relationships among autonomic, motor, and behavioral organization during the pre-feeding period. However, it seems likely that there are strong relationships among these parameters, and the feeding readiness model therefore posits relationships among them as well as relationships of the organization of these subsystems to other feeding readiness variables. The model also posits a relationship between organization and neurologic maturation since theoretically, maturation underpins organization. Finally, the model hypothesizes that organization can be used to predict feeding outcomes.
BOTTLE FEEDING OUTCOMES
Suek-swallow-breathe coordination and the ability to maintain autonomic, motor, and behavioral state organization during and after feeding have been cited as hallmarks of efficient bottle feeding (Pickler et al., 1997; Shaker, 1990). However, the relationships among these variables remain unclear. While feeding performance has been examined in a number of studies, often it has been looked at in “trial” feedings, typically, 5-minute observations, rather than actual feedings during which the infant is offered his or her entire prescribed feeding amount and allowed to complete it in his or her own time frame.
SUCK-SWALLOW-BREATHE COORDINATION
The ability to achieve and maintain coordinated sucking, swallowing, and breathing appears to be an important factor in bottle feeding. Sucking is a complex behavior that results from the integration of the muscular activities of the lips, cheeks, jaws, tongue, and palate. Although sucking is the only part of the suck-swallow-breathe triad that the infant can control, a crucial sequence of events must occur if the infant is to be successful in oral feeding. The ability to transfer milk into the mouth from a bottle and form a bolus while pushing it to the back of the mouth to generate the swallow reflex requires precise timing of all muscle movements (Lau & Schanler, 1996).
In preterm infants, continuous sucking is common at the beginning of a feeding. This continuous sucking involves no interruptions for breathing and essentially represents a single, long suck burst (Shiao, 1997). Intermittent sucking follows, during which the sucking is interrupted for breathing. As the infant matures, breathing becomes more coordinated with sucking, creating a situation in which the infant breathes through the suck.
Swallowing is also a complex behavior and, like sucking, requires proper coordination of the muscles of the mouth, palate, pharynx, larynx, and esophagus. Sucking does not automatically activate swallowing — rather, the bolus of milk stimulates chemoreceptors in the pharynx so that the swallow is initiated (Lau et al., 1996). During the swallow, breathing is suppressed; thus the coordination of swallowing and breathing is a major concern of caregivers.
As the infant matures, there is a trend toward synchronized coordination of sucking, swallowing and breathing on a 1:1:1 or 2:2:1 ratio (Paludetto, Robertson, & Martin, 1986; Wolff, 1968). This ratio can be achieved by healthy preterm infants as early as 36 to 37 weeks gestation. However, delay in the development of any of the necessary parameters, such as breathing, can lead to de-synchronization and oral feeding difficulty. With less well coordinated sucking and breathing, the ratio is more sucking to breathing, at around 2:1 to 4:1. Breathing is particularly affected during continuous sucking at the start of a feeding and when milk flows rapidly (Mathew, 1991).
Preterm infants may be fed orally prior to achieving coordination of sucking, swallowing and breathing. Because the infant learns to protect the airway, either by alternating periods of prolonged respiratory pause, during which vigorous sucking occurs, with long breathing bursts, or by blocking the nipple with the tongue. These compensatory mechanisms reflect the infant's inability to perform suction-expression-swallow in parallel with inspiration and expiration. Thus, preterm infants tend to suck, swallow, and breathe in an alternate, rather than coordinated fashion.
During-feeding and Post-feeding Autonomic, Motor, and Behavioral State Organization
To bottle feed, the infant must be able to coordinate the mechanisms of bottle feeding with autonomic, motor, and behavioral responses. Specifically, in addition to achieving and maintaining a coordinated suck-swallow-breathe action, the infant must be able to maintain cardiorespiratory control and control over motor tone and activity, and must achieve and sustain a quietly alert behavior state. Moreover, these control mechanisms must occur in a smooth fashion in order for the infant to obtain the full nutritional value of the feeding.
As noted earlier, feeding taxes the preterm infant's ability to maintain control of basic autonomic, motor, and behavior state functioning (Daniels et al., 1988; Daniels et al., 1990; Mathew, 1988). Research suggests that the preterm infant's ability to achieve a quietly awake state prior to bottle feeding and to maintain that state throughout the feeding is associated with successful early bottle feedings (McCain, 1997; Pickler et al., 1996). However, the ability of bottle feeding readiness criteria to predict the post-feeding organization of autonomic, motor, and behavioral state systems has not been studied.
Feeding Performance
A number of studies have examined feeding performance in preterm infants. Using measures of proficiency (amount of formula taken during first 5 minutes of a feeding/total volume ordered), efficiency (total volume/total time), and overall transfer (percent of prescribed formula taken), Lau and colleagues found that restricted milk flow, flow that requires the infant to be actively sucking, has resulted in improved performance in all areas, although unrestricted milk flow was also tolerated (Lau & Schanler, 2000; Lau, Sheena, Shulman, & Schanler, 1997). “Successful” feeding, defined as overall transfer of 80%, was not dependent on a 1:1 coordination of sucking to breathing. Infants who had a proficiency ≥30% and efficiency ≥1.5 ml/min attained full oral feeding at an earlier post-conceptional age and were successful, taking in 30 ml in 20 minutes, with 9 ml taken during the first 5 minutes of the feeding. Other researchers have found that feeding performance, as measured by the volume of formula taken per minute, was related to post-conceptional age (Casaer, Daniels, Devlieger, De Cock, & Eggermont, 1982).
Feeding performance has been little studied in relation to other feeding outcomes, such as autonomic, motor, and behavioral state organization. Moreover, the relationships between feeding readiness indicators and feeding performance have not received much research attention. In the feeding readiness model, measures of feeding performance are posited to be correlated with other feeding outcomes. In addition, it is hypothesized that feeding performance is predicted by readiness indicators.
Bottle Feeding Experience
The contribution of bottle feeding experience to feeding readiness has been rarely examined. Although sucking is essentially organized at birth in full-term infants, experience is important in maintaining this behavior (Alberts, 1994). Non-oral feeding methods, which are almost universally used for preterm infants, reduce sensory input to the mouth, and this may delay the development of oral feeding ability (Medoff-Cooper & Gennaro, 1996).
The preterm infant's ability to suck nonnutritively is often used as an indicator of nutritive sucking readiness; however, nonnutritive sucking (NNS) is not predictive of successful bottle feeding (Pinelli & Symington, 2003). NNS has been repeatedly shown to differ from nutritive sucking (Bosack, 1973; Wolff, 1968) and, of course, swallowing is not necessary so there is less interruption of breathing. The greatest benefits of nonnutritive sucking are its ability to calm an agitated infant (DiPietro, Cusson, Caughy, & Fox, 1994) and to bring a sleeping infant to a more alert state for a feeding (McCain, 1994; Pickler et al., 1996). In fact, experience in nutritive sucking results in maturation of the sucking mechanism, and preterm infants gradually improve their ability to suck and swallow (Gryboski, 1969; Medoff-Cooper et al., 1993). Early introduction of oral feeding may provide practice at oral feeding that enhances nutritive sucking skills (Simpson, Schanler, & Lau, 2002). Also, nutritive sucking probably provides the infant with behavioral reinforcement that motivates the infant to continue that behavior (Medoff-Cooper, Weininger, & Zukowsky, 1989).
Significance of the Readiness Model
During the past 25 years, efforts to reduce the preterm birth rate have failed and success in the near future appears unlikely (Creasy, Jarvis, Myers, Markowitz, & Kerkering, 1993; Creasy, 1993; Goldenberg & Rouse, 1998; Moore & Freda, 1998). Efforts to provide care that improves physiologic and behavioral outcomes for preterm infants therefore are of great importance. Earlier “models” of preterm infant feeding (Glass & Wolf, 1994) emphasize the relationship of the infant's medical condition to feeding ability and suggest that assessment of feeding needs to include behavior state before, during, and after the feeding, autonomic or physiological responsiveness, and suck-swallow-breathe coordination. Unfortunately, however, many of the relationships among these components have not been examined. The model presented here posits relationships among components of feeding readiness, experience at bottle feeding, and feeding outcomes.
Better understanding of bottle feeding readiness and its relationship to bottle feeding outcomes will provide useful information for the management of bottle feeding of preterm infants. Identification of readiness criteria associated with the greatest likelihood of successful feeding can provide the basis for clinical guidelines that should reduce adverse physiological responses to bottle feedings and result in a smoother, less traumatic, and potentially shorter transition time to all bottle feeding.
Acknowledgments
This work was supported by R01 NR05182 from the National Institute of Nursing Research, National Institutes of Health.
References
- Aguayo J. Maternal lactation for preterm infants. Early Human Development. 2001;65:S19–S29. doi: 10.1016/s0378-3782(01)00203-1. [DOI] [PubMed] [Google Scholar]
- Alberts JR. Learning as adaptation of the infant. Acta Paediatrica Supplement. 1994;397:77–85. doi: 10.1111/j.1651-2227.1994.tb13269.x. [DOI] [PubMed] [Google Scholar]
- Als H, Brazelton TB. A new model of assessing the behavioral organization in preterm and fullterm infants. Journal of the American Academy of Child Psychiatry. 1981;20:239–263. doi: 10.1016/s0002-7138(09)60987-0. [DOI] [PubMed] [Google Scholar]
- Als H, Duffy FH, McAnulty GB. Effectiveness of individualized neurodevelopmental care in the newborn intensive care unit (NICU) Acta Paediatrica Supplement. 1996;416:21–30. doi: 10.1111/j.1651-2227.1996.tb14273.x. [DOI] [PubMed] [Google Scholar]
- Als H, Gilkerson L. Developmentally supportive care in the neonatal intensive care unit. Zero to Three. 1995;15 (6):3–10. [Google Scholar]
- Bazyk S. Factors associated with the transition to oral feeding in infants fed by nasogastric tubes. American Journal of Occupational Therapy. 1990;44:1070–1078. doi: 10.5014/ajot.44.12.1070. [DOI] [PubMed] [Google Scholar]
- Becker PT, Grunwald PC, Moorman J, Stuhr S. Effects of developmental care on behavioral organization in very-low-birth-weight infants. Nursing Research. 1993;42:214–220. [PubMed] [Google Scholar]
- Bier JA, Ferguson A, Cho C, Oh W, Vohr BR. The oral motor development of low-birth-weight infants who underwent orotracheal intubation during the neonatal period. American Journal of Diseases of Children. 1993;147:858–862. doi: 10.1001/archpedi.1993.02160320060020. [DOI] [PubMed] [Google Scholar]
- Bosack TN. Effects of fluid delivery on the sucking response of the human newborn. Journal of Experimental Child Psychology. 1973;15:77–85. doi: 10.1016/0022-0965(73)90132-x. [DOI] [PubMed] [Google Scholar]
- Bu’Lock, F., Woolridge, M. W., & Baum, J. D. (1990). Development of co-ordination of sucking, swallowing and breathing: Ultrasound study of term and preterm infants. Developmental Medicine and Child Neurology, 32, 669–678.p [DOI] [PubMed]
- Cagan J. Feeding readiness behavior in preterm infants. Neonatal Network. 1995;14(2):82. [Google Scholar]
- Casaer P, Daniels H, Devlieger H, De Cock P, Eggermont E. Feeding behaviour in preterm neonates. Early Human Development. 1982;7:331–346. doi: 10.1016/0378-3782(82)90035-4. [DOI] [PubMed] [Google Scholar]
- Creasy GL, Jarvis PA, Myers BJ, Markowitz PI, Kerkering KW. Mental and motor development for three groups of premature infants. Infant Behavior & Development. 1993;16:365–372. [Google Scholar]
- Creasy RK. Preterm birth prevention: Where are we? American Journal of Obstetrics and Gynecology. 1993;168:1223–1230. doi: 10.1016/0002-9378(93)90373-q. [DOI] [PubMed] [Google Scholar]
- Daniels H, Devlieger H, Casaer P, Ramaekers V, van Den BJ, Eggermont E. Feeding, behavioural state and cardiorespiratory control. Acta Paediatrica Scandinavica. 1988;77:369–373. doi: 10.1111/j.1651-2227.1988.tb10662.x. [DOI] [PubMed] [Google Scholar]
- Daniels H, Devlieger H, Minami T, Eggermont E, Casaer P. Infant feeding and cardiorespiratory maturation. Neuropediatrics. 1990;21:9–10. doi: 10.1055/s-2008-1071449. [DOI] [PubMed] [Google Scholar]
- DiPietro JA, Cusson RM, Caughy MO, Fox NA. Behavioral and physiologic effects of nonnutritive sucking during gavage feeding in preterm infants. Pediatric Research. 1994;36:207–214. doi: 10.1203/00006450-199408000-00012. [DOI] [PubMed] [Google Scholar]
- Fleisher BE, VandenBerg K, Constantinou J, Heller C, Benitz WE, Johnson A. Individualized developmental care for very-low-birth-weight premature infants. Clinical Pediatrics. 1995;34:523–529. doi: 10.1177/000992289503401003. [DOI] [PubMed] [Google Scholar]
- Glass RP, Wolf LS. A global perspective on feeding assessment in the neonatal intensive care unit. American Journal of Occupational Therapy. 1994;48:514–526. doi: 10.5014/ajot.48.6.514. [DOI] [PubMed] [Google Scholar]
- Goldenberg RL, Rouse DJ. Prevention of premature birth. New England Journal of Medicine. 1998;339:313–320. doi: 10.1056/NEJM199807303390506. [DOI] [PubMed] [Google Scholar]
- Gryboski JD. Suck and swallow in the premature infant. Pediatrics. 1969;43:96–102. [PubMed] [Google Scholar]
- Kinneer MD, Beachy P. Nipple feeding premature infants in the neonatal intensive-care unit factors and decisions. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1994;23:105–112. doi: 10.1111/j.1552-6909.1994.tb01859.x. [DOI] [PubMed] [Google Scholar]
- Koenig JS, Davies AM, Thach BT. Coordination of breathing, sucking, and swallowing during bottle feedings in human infants. Journal of Applied Physiology. 1990;69:1623–1629. doi: 10.1152/jappl.1990.69.5.1623. [DOI] [PubMed] [Google Scholar]
- Lau C, Schanler RJ. Oral motor function in the neonate. Clinics in Perinatology. 1996;23:161–178. [PubMed] [Google Scholar]
- Lau C, Schanler RJ. Oral feeding in premature infants: Advantage of a self-paced milk flow. Acta Paediatrica. 2000;89:453–459. doi: 10.1080/080352500750028186. [DOI] [PubMed] [Google Scholar]
- Lau C, Sheena HR, Shulman RJ, Schanler RJ. Oral feeding in low birth weight infants. Journal of Pediatrics. 1997;130:561–569. doi: 10.1016/s0022-3476(97)70240-3. [DOI] [PubMed] [Google Scholar]
- Mandich MB, Ritchie SK, Mullett M. Transition times to oral feeding in premature infants with and without apnea. Journal of Obstetric, Gynecologic and Neonatal Nursing. 1996;25:771–776. doi: 10.1111/j.1552-6909.1996.tb01493.x. [DOI] [PubMed] [Google Scholar]
- Mathew OP. Respiratory control during nipple feeding in preterm infants. Pediatric Pulmonology. 1988;5:220–224. doi: 10.1002/ppul.1950050408. [DOI] [PubMed] [Google Scholar]
- Mathew OP. Breathing patterns of preterm infants during bottle feeding: Role of milk flow. Journal of Pediatrics. 1991;119:960–965. doi: 10.1016/s0022-3476(05)83056-2. [DOI] [PubMed] [Google Scholar]
- McCain GC. Faclilitating inactive awake states in preterm infants: a study of three interventions. Nursing Research. 1992;41:157–160. [PubMed] [Google Scholar]
- McCain GC. Modulation of preterm infant behavioral state prior to oral feeding. Neonatal Network. 1994;13(4):75. [Google Scholar]
- McCain GC. Behavioral state activity during nipple feedings for preterm infants. Neonatal Network. 1997;16:43–47. [PubMed] [Google Scholar]
- McCain GC, Garside P. Behavirol responses of preterm infants to a standard-care and semi-demand feeding protocol. Newborn and Infant Nursing Reviews. 2002;2:187–193. [Google Scholar]
- McCain GC, Gartside P, Greenberg JM, Lott JW. A feeding protocol for healthy preterm infants that shortens time to oral feeding. Journal of Pediatrics. 2001;139:374–379. doi: 10.1067/mpd.2001.117077. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B, Gennaro S. The correlation of sucking behaviors and Bayley Scales of Infant Development at six months of age in VLBW infants. Nursing Research. 1996;45:291–296. doi: 10.1097/00006199-199609000-00007. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B, Verklan T, Carlson S. The development of sucking patterns and physiologic correlates in very-low-birth-weight infants. Nursing Research. 1993;42:100–105. [PubMed] [Google Scholar]
- Medoff-Cooper B, Weininger S, Zukowsky K. Neonatal sucking as a clinical assessment tool: preliminary findings. Nursing Research. 1989;38:162–165. [PubMed] [Google Scholar]
- Moore ML, Freda MC. Reducing preterm and low birthweight births: still a nursing challenge. MCN, American Journal of Maternal Child Nursing. 1998;23:200–208. doi: 10.1097/00005721-199807000-00007. [DOI] [PubMed] [Google Scholar]
- Paludetto R, Robertson SS, Martin RJ. Interaction between nonnutritive sucking and respiration in preterm infants. Biology of the Neonate. 1986;49:198–203. doi: 10.1159/000242531. [DOI] [PubMed] [Google Scholar]
- Pickler RH, Frankel HB, Walsh KM, Thompson NM. Effects of nonnutritive sucking on behavioral organization and feeding performance in preterm infants. Nursing Research. 1996;45:132–135. doi: 10.1097/00006199-199605000-00002. [DOI] [PubMed] [Google Scholar]
- Pickler RH, Mauck AG, Geldmaker B. Bottle-feeding histories of preterm infants. Journal of Obstetric Gynecologic and Neonatal Nursing. 1997;26:414–420. doi: 10.1111/j.1552-6909.1997.tb02723.x. [DOI] [PubMed] [Google Scholar]
- Pinelli J, Atkinson SA, Saigal S. Randomized trial of breastfeeding support in very low-birth-weight infants. Archives of Pediatric and Adolescent Medicine. 2001;155:548–553. doi: 10.1001/archpedi.155.5.548. [DOI] [PubMed] [Google Scholar]
- Pinelli, J. & Symington, A. (2003). Non-nutritive sucking for promoting physiologic stability and nutrition in preterm infants. The Cochrane Library, (Oxford), 2. [DOI] [PubMed]
- Poets CF, Langner MU, Bohnhorst B. Effects of bottle feeding and two different methods of gavage feeding on oxygenation and breathing patterns in preterm infants. Acta Paediatrica. 1997;86:419–423. doi: 10.1111/j.1651-2227.1997.tb09034.x. [DOI] [PubMed] [Google Scholar]
- Pridham K, Brown R, Sondel S, Green C, Wedel NY, Lai HC. Transition time to full nipple feeding for premature infants with a history of lung disease. Journal of Obstetric Gynecologic and Neonatal Nursing. 1998;27:533–545. doi: 10.1111/j.1552-6909.1998.tb02620.x. [DOI] [PubMed] [Google Scholar]
- Pridham K, Kosorok MR, Greer F, Kayata S, Bhattacharya A, Grunwald PC. Comparison of caloric intake and weight outcomes of an ad lib feeding regimen for preterm infants in two nurseries. Journal of Advanced Nursing. 2001;35:751–759. doi: 10.1046/j.1365-2648.2001.01907.x. [DOI] [PubMed] [Google Scholar]
- Pridham KF, Sondel S, Chang A, Green C. Nipple feeding for preterm infants with bronchopulmonary dysplasia. Journal of Obstetric Gynecologic and Neonatal Nursing. 1993;22:147–155. doi: 10.1111/j.1552-6909.1993.tb01794.x. [DOI] [PubMed] [Google Scholar]
- Romero R, Kleinman RE. Feeding the very low-birth-weight infant. Pediatrics in Review. 1993;14:123–132. doi: 10.1542/pir.14-4-123. [DOI] [PubMed] [Google Scholar]
- Schanler RJ, Shulman RJ, Lau C, Smith EO, Heitkemper MM. Feeding strategies for premature infants: randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics. 1999;103:434–439. doi: 10.1542/peds.103.2.434. [DOI] [PubMed] [Google Scholar]
- Shaker CS. Nipple feeding premature infants: A different perspective. Neonatal Network. 1990;8:9–17. [PubMed] [Google Scholar]
- Shaker CS. Nipple feeding preterm infants: An individualized, developmentally supportive approach. Neonatal Network. 1999;18:15–22. doi: 10.1891/0730-0832.18.3.15. [DOI] [PubMed] [Google Scholar]
- Shiao SY. Comparison of continuous versus intermittent sucking in very-low-birth-weight infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1997;26:313–319. doi: 10.1111/j.1552-6909.1997.tb02147.x. [DOI] [PubMed] [Google Scholar]
- Sidell EP, Froman RD. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 1994;23:783–789. doi: 10.1111/j.1552-6909.1994.tb01953.x. [DOI] [PubMed] [Google Scholar]
- Simpson C, Schanler RJ, Lau C. Early introduction of oral feeding in preterm infants. Pediatrics. 2002;110:517–522. doi: 10.1542/peds.110.3.517. [DOI] [PubMed] [Google Scholar]
- VandenBerg KA. Nippling management of the sick neonate in the NICU: The disorganized feeder. Neonatal Network. 1990;9:9–16. [PubMed] [Google Scholar]
- Wolff PH. The serial organization of sucking in the young infant. Pediatrics. 1968;42:943–956. [PubMed] [Google Scholar]


