Abstract
The envelope of class I viruses can be a target for potent viral inhibitors, such as the human immunodeficiency virus type 1 (HIV-1) inhibitor enfuvirtide, which are derived from the C-terminal heptad repeat (HR2) of the transmembrane (TM) subunit. Resistance to an HR2-based peptide inhibitor of a model retrovirus, subgroup A of the Avian Sarcoma and Leukosis Virus genus (ASLV-A), was studied by examining mutants derived by viral passage in the presence of inhibitor. Variants with reduced sensitivity to inhibitor were readily selected in vitro. Sensitivity determinants were identified for 13 different isolates, all of which mapped to the TM subunit. These determinants were identified in two regions: (i) the N-terminal heptad repeat (HR1) and (ii) the N-terminal segment of TM, between the subunit cleavage site and the fusion peptide. The latter class of mutants identified a region outside of the predicted HR2-binding site that can significantly alter sensitivity to inhibitor. A subset of the HR1 mutants displayed the unanticipated ability to infect nonavian cells. This expanded tropism was associated with increased efficiency of envelope triggering by soluble receptor at low temperatures, as measured by protease sensitivity of the surface subunit (SU) of envelope. In addition, expanded tropism was linked for the most readily triggered mutants with increased sensitivity to neutralization by SU-specific antiserum. These observations depict a class of HR2 peptide-selected mutations with a reduced activation threshold, thereby allowing the utilization of alternative receptors for viral entry.
For an enveloped virus to initiate infection, it must penetrate a target cell by fusion of its surrounding membrane with a host cell membrane. This process is mediated by specific viral proteins embedded in the viral envelope. There are at least two distinct types of such fusogenic proteins, each with a set of common structural characteristics. Class I fusion proteins (8) are found in many disparate virus families, including retroviruses, orthomyxoviruses, paramyxoviruses, filoviruses, arenaviruses (17), coronaviruses (5), and probably baculoviruses (59), while the fusion proteins of alphaviruses and flaviviruses have been denoted as class II (22). Class I envelope proteins are generally cleaved into two functionally distinct domains, an N-terminal surface subunit (designated SU in the case of retroviruses) and a C-terminal transmembrane subunit (transmembrane [TM] for retroviruses). These envelopes assemble into trimeric complexes, while the two subunits of each monomer maintain association. The driving force for membrane fusion is believed to be a major conformational rearrangement of the TM subunit, the end product of which is a structure termed the six-helix bundle (8). The core of this structure is a triple-stranded coiled coil, with each strand contributed by an N-terminal heptad repeat (HR1) from one of the three TM subunits. A second heptad repeat (HR2), which is located on the C-terminal portion of the TM ectodomain, packs within the grooves of the coiled coil in an antiparallel direction. Peptides homologous to these repeats have been shown to block membrane fusion and viral entry, presumably by disrupting the necessary conformational changes in TM (25, 27, 44, 60, 61). An HR2-derived peptide termed enfuvirtide (also known as DP178, T-20, or Fuzeon) has recently been approved for treating advanced human immunodeficiency virus (HIV) infections (34). Emergence of HIV resistance to enfuvirtide is linked to changes within HR1 both in vitro (49) and in vivo (20, 57), specifically residues 36 to 45 of gp41. Enfuvirtide sensitivity has also been reported to be modulated by determinants of coreceptor specificity in gp120 (12, 13) and by gp41 sequences in and around HR2 (21).
The avian sarcoma and leukosis viruses (ASLV) comprise the Alpharetrovirus genus of retroviruses, and have often been used to study receptor-mediated envelope triggering. A potent ASLV HR2-based peptide inhibitor has recently been described and employed as a tool to investigate conformational changes in TM (14, 33, 37). We have identified several envelope mutations which diminish sensitivity to this inhibitor by passaging ASLV subtype A (ASLV-A) in the presence of peptide. Several of these changes are found near the amino terminus of the TM subunit and are not within HR1, the predicted target for HR2 peptide inhibitors. In addition, some mutations within HR1 appear to reduce the requirements for envelope triggering and permit infection on normally refractory mammalian cell lines. These mutants and their phenotypes provide insight into escape mechanisms for an important new class of viral inhibitor.
MATERIALS AND METHODS
Viruses and cells.
QT6, DF-1, and 293T cells were maintained as described previously (37). Murine leukemia virus (MLV) pseudotypes were produced by CaPO4 transfection of 293T cells as described previously (62) using either pHIT111 (52) or MRP-lacZ (see below) as a reporter. Virus-containing medium was filtered (0.45 μm) and stored at −80°C. To produce virus for the SU conformational change assay, pseudotypes were filtered and then concentrated by centrifugation through a cushion of 20% sucrose in Dulbecco's phosphate-buffered saline (D-PBS) at 100,000 × g for 90 min at 4°C. Pelleted virus was resuspended in D-PBS without MgCl2 or CaCl2. To ascertain relative envelope incorporation, viral pseudotypes were concentrated by centrifugation through sucrose, resuspended in sodium dodecyl sulfate (SDS) sample buffer, and examined by Western blotting using anti-SU or anti-MLV Gag antiserum followed by quantitation with [125I]-labeled Protein A as described below. RCASBP(A)-green fluorescent protein (GFP)-infected DF-1 cells were kindly provided by Mark Federspiel (Mayo Clinic). Recombinant ASLV-A was also produced by CaPO4 transfection of QT6 cells with the plasmid pRV-9-hrGFP.
Plasmids and proteins.
The ASLV-A envelope expression vector, pCB6-EnvA, has been described previously (18). Notable mutations identified by sequencing (see below) were subcloned from their TOPO vector into pCB6-EnvA using strategies particular to each mutation. To generate pRV-9-hrGFP, the gene for Renilla reniformis green fluorescent protein from phrGFP-N1 (Stratagene) was amplified by PCR using primers to introduce appropriate terminal SfiI sites (5′-CGCGTAGGCCATTACGGCCGCTAGCACCATGGTGAGC-3′ and 5′-GCCGTAGGCCGAGGCGGCCTATCACACCCACTCGTGCAGGCTG-3′), which were used to clone the gene into the two distinct SfiI sites found within the replication-competent vector pRV-9 (38). MLV-based β-galactosidase reporter plasmid MRP-lacZ was constructed using pZErO-1 (Invitrogen) as a backbone and contains a cytomegalovirus promoter as well as MLV 5′ and 3′ long terminal repeats and the extended packaging signal derived from pLXSN (36). The HR2 peptide R99 (FNLSDHSESIQKKFQLMKEHVNKIG) was synthesized by Alpha Diagnostic International, Inc., with N-terminal acetylation, C-terminal amidation, and purification to greater than 95%. The peptide was reconstituted in water, and aliquots were stored at −20°C. Soluble ASLV-A receptor, sTva, was purified from the medium of Sf9 cells infected with a baculovirus recombinant (2).
Virus selection.
ASLV-A infection of DF-1 cells was initiated either by co-seeding uninfected cells with RCASBP(A)-GFP-infected DF-1 cells at a ratio of 100:1, or by infecting them with either cell-free RCASBP(A)-GFP at a multiplicity of infection of 0.0002 or pRV-9-hrGFP-generated virus at a multiplicity of infection of 0.02. R99 was added directly to the media as described in the text. Media from resistant cell lines was used to infect fresh DF-1 cells, and once the culture was fully infected as assessed by GFP expression, genomic DNA from infected cells was isolated using a QIAamp DNA Mini Kit (QIAGEN). Unselected viral populations were maintained in parallel as a control. The entire envelope gene, apart from the 5′-spliced end that contributes the first 6 amino acids, was amplified using Expand High Fidelity PCR (Roche; a mixture of Taq and Tgo DNA polymerases) and cloned into either pCR-BluntII-TOPO or pcDNA3.1D/V5-His-TOPO (Invitrogen). Envelope sequences were determined for multiple clones derived from each population of infected cells.
Viral infections.
Infection and titration of MLV pseudotypes has been described previously (37). For R99 inhibition studies, peptide was diluted in medium and added to target cells prior to addition of virus dilutions, using an equivalent number of infectious units for each virus. The 50% inhibitory concentration (IC50) values and their standard errors were calculated with nonlinear regression using GraphPad Prism 3 software to generate sigmoidal dose-response curves with variable slope. Data shown in Table 1 were compiled from five experiments, with one to five different virus stocks tested for each envelope. Neutralization assays were performed by incubating antiserum with virus on ice for 75 min, diluting them 10-fold with media, and then infecting cells by centrifugal inoculation at 4°C in a refrigerated, tabletop centrifuge for 2.5 h at 1,700 × g. Monoclonal antibodies mc8C5-4 (40) or a control (CXCR4-specific 12G5; kindly provided by James Hoxie, University of Pennsylvania) were used in one set of experiments, while rabbit polyclonal anti-SU-immunoadhesin or prebleed antiserum was used in another set. Significance of data was determined with a paired Student's t test.
TABLE 1.
Mutations in ASLV-A TM that reduce sensitivity to an HR2 peptide
| Mutation | TM location | R99 IC50 (μM) | Log IC50a | IC50 vs. WT | No. of times isolatedb | 293T infectivityc |
|---|---|---|---|---|---|---|
| None (WT) | N/A | 0.031 | −7.51 ± 0.04 | 1.0 | N/A | <3 × 10−5 |
| T2I | N terminus | 2.2 | −5.66 ± 0.10 | 71 | 1 | <3 × 10−5 |
| S3L | N terminus | 0.25 | −6.60 ± 0.06 | 8.0 | 2 | <3 × 10−5 |
| D11N | N terminus | >50 | >−4.3 | >1,500 | 3 | <3 × 10−5 |
| D11E | N terminus | 0.12 | −6.91 ± 0.05 | 4.0 | 1 | <3 × 10−5 |
| E12K | N terminus | 0.085 | −7.07 ± 0.08 | 2.8 | 1 | <3 × 10−5 |
| A44V | HR1 | 0.090 | −7.05 ± 0.10 | 2.9 | 1 | 2.2 × 10−4 |
| V48D | HR1 | 7.9 | −5.10 ± 0.14 | 260 | 2 | 1.1 × 10−1 |
| K49E | HR1 | 0.54 | −6.27 ± 0.25 | 18 | 1 | <3 × 10−5 |
| A51V | HR1 | 0.31 | −6.51 ± 0.05 | 10 | 1 | 1.2 × 10−4 |
| L53F | HR1 | 0.099 | −7.00 ± 0.06 | 3.2 | 1 | <3 × 10−5 |
| G59R | HR1 | 0.12 | −6.91 ± 0.02 | 4.0 | 4 | <3 × 10−5 |
| L62A | HR1 | 0.22 | −6.65 ± 0.08 | 7.2 | 0d | 2.0 × 10−2 |
| V31I D60N | FP/HR1 | 0.22 | −6.66 ± 0.10 | 7.0 | 1 | <3 × 10−5 |
Log [R99] ± standard error.
Number of independent populations from which this mutation was identified.
Infectious titer on mammalian 293T cells relative to titer on avian QT6 cells.
L62A is an engineered substitution.
SU conformational change assay.
This assay is a variation of one which has been described previously (9, 19), except it was performed with pseudotyped viral particles (1). Partially purified virus was incubated with or without 100 ng of sTva on ice for 30 min, then either heated to 37°C or maintained on ice for another 15 min. to allow conformational change. Virus was returned to ice, and CaCl2 (to 2 mM final concentration) and thermolysin (to 80 ng/μl final concentration) were added and allowed to digest for 30 min. Samples were separated by SDS-polyacrylamide gel electrophoresis (PAGE), transferred to nitrocellulose, Western blotted with antiserum raised against an ASLV-A SU-immunoadhesin (64), and probed with 125I-labeled protein A. Bands were visualized on a Molecular Dynamics Storm 860 digital imager and quantitated with ImageQuant 1.2 software.
RESULTS
Selection of ASLV-A variants with reduced sensitivity to an HR2 inhibitor.
An ASLV-A HR2-based peptide of 25 residues in length, denoted R99, has been found to be a potent inhibitor of virus infection and envelope-mediated cell-cell fusion (14, 37). In order to examine the propensity for acquiring resistance and the determinants of that resistance, recombinant GFP-expressing ASLV-A was passaged on chicken DF-1 cells in the presence of 25 to 50 μg/ml R99 (added fresh every three days) or 5 to 15 μg/ml R99 (added fresh every day). Multiple independent cultures were maintained and occasionally supplemented with uninfected cells. Expression of GFP was used to monitor the fraction of infected cells, which was generally in the 1 to 10% range prior to acquiring resistance. Each of two 8.5-cm plates (∼3 × 106 cells at confluence) generated multiple sequence variants within 1 month that proved to be determinants of resistance (see below). When selections were performed on a smaller scale, 8 of 20 cultures in 11-mm dishes (∼7 × 104 cells) produced virus populations within three months that had a noticeable growth advantage in one case, and 3 of 20 within two months in another case. Overall, these experiments demonstrate that viruses with reduced sensitivity to an HR2-based inhibitor can be readily selected.
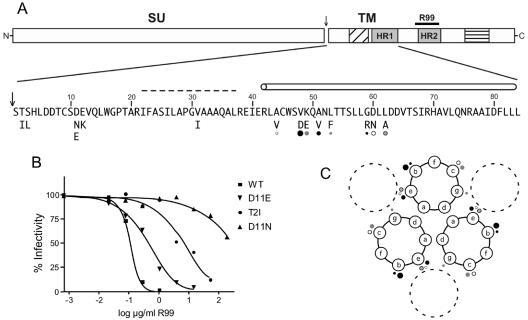
Envelope sequences derived from cells infected with R99-selected virus populations displayed coding changes in the TM subunit, while those from cells infected with virus passaged under nonselective conditions generally did not. In order to assess the R99 sensitivity conferred by specific mutations (Fig. 1A), envelope sequences with these changes were cloned into an expression vector which was used to generate pseudotyped viral particles with an MLV core and a β-galactosidase reporter gene (52, 62). Quail QT6 cells were infected with pseudotyped MLV(EnvA) viruses in the absence or presence of R99 dilutions (Fig. 1B). Mutations listed in Table 1 and shown in Fig. 1A displayed significant reduction in R99 sensitivity. Some of the mutations were observed in multiple independent populations, although the majority were found in a single population each (Table 1), demonstrating the diversity of peptide inhibitor escape determinants. The mutations shown are all single amino acid changes except for one double substitution, V31I/D60N; V31 is within the fusion peptide and D60N is within HR1. Of the remaining 12 mutations, 7 are within the HR1 domain and 5 are found on the amino-terminal side of the predicted fusion peptide domain (23), between the SU-TM cleavage site and the fusion peptide. An ASLV TM structure has not yet been reported. However, the sequence of the ASLV TM is strikingly similar to the corresponding subunit (GP2) of the Ebola virus envelope (16, 55), Using the Ebola virus GP2 structure as a guide (31, 58), the seven ASLV HR1 mutants all map to predicted grooves in the coiled coil against which the HR2 domains pack (Fig. 1C). None of these mutants had a noticeable impact on SU-TM processing or incorporation into retroviral particles (data not shown), and all conferred wild-type levels of infectivity on avian QT6 cells (Fig. 2 and data not shown).
FIG. 1.
ASLV-A mutations with reduced sensitivity to an HR2 peptide. (A) Schematic diagram of the ASLV-A envelope, with an expanded view of the amino acid sequence between the subunit cleavage site (arrow) through the N-terminal heptad repeat (HR1). Shown below the sequence are the identified mutations; each was tested as a single amino acid substitution except for the double mutant V31I/D60N. The fusion peptide is marked by diagonal lines and the membrane-spanning domain by horizontal lines (upper segment); the location of the region from which R99 is derived is shown with a black bar. In the expanded view, the fusion peptide is denoted by the dashed line, and HR1 with a cylinder. (B) Sample R99 inhibition curves for wild-type ASLV-A envelope and three mutants in the N-terminal end of the TM subunit. Infectivity of pseudotyped virus is shown as % of control (no inhibitor) with each point representing the average from one experiment performed in triplicate. (C) Coiled-coil projection indicating location of HR1 mutants. Each of the three inner coils is provided by the HR1 domain from one TM subunit. The dots represent locations in which HR2 peptide resistance determinants have been identified, and correspond to the dots shown in Fig. 1A. Each small dot represents a mutation with low resistance (3- to 4-fold change in IC50), each medium-sized dot shows a mutation with moderate resistance (7- to 20-fold change in IC50), and the large dots indicate the V48D mutation (260-fold change in IC50). The dashed circles correspond to the HR2 helices, which pack antiparallel against the grooves of the central trimer. This projection is based on an alignment with the Ebola GP2 sequence (58) and includes a stutter in the helix at Thr-54 (ASLV numbering).
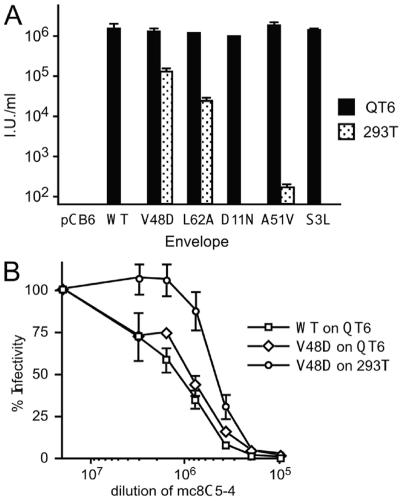
FIG. 2.
Expanded cell tropism of some of the R99-selected mutants. (A) Infectivity of pseudotyped virus particles on avian QT6 cells and mammalian 293T cells. Cells were infected in triplicate by centrifugal inoculation and data normalized to the amount of MLV Gag. Error bars show standard deviations. The pCB6 lane shows no detectable infectivity from a virus made with an empty vector plasmid instead of pCB6-EnvA. (B) Neutralization of MLV pseudotypes with either wild-type ASLV-A or V48D mutant envelopes by mc8C5-4, a monoclonal antibody that competes with the Tva receptor for envelope binding. Infectivity is shown as % of control (no antiserum) and error bars show standard deviations of experiment performed in triplicate.
Expanded tropism of envelope variants.
The sensitivity of HIV type 1 (HIV-1) isolates to HR2-based inhibitors has been reported to correlate inversely with coreceptor affinity (45, 47). ASLV-A is only known to utilize a single receptor, Tva (3), found only in avian cells, but this receptor is closely related to the ligand-binding repeat found in the low-density lipoprotein receptor (LDLR). Although this repeat is found in a wide variety of membrane proteins (39), only Tva has been shown to function as a receptor for ASLV-A. One of the ligand-binding repeats found in human LDLR, LDL-A4, can be converted to an efficient ASLV-A receptor upon substitution of 3 residues (50). To examine the possibility that an envelope with diminished sensitivity to an HR2 peptide might have an altered interaction with proteins containing LDLR ligand-binding repeats, MLV(EnvA) pseudotype entry was tested on human 293T cells. Several R99 escape mutants (A44V, A51V, and V48D), as well as engineered substitution L62A (37), were found to mediate infection on these cells (Table 1 and Fig. 2A). The V48D mutant displayed the highest level of infectivity on mammalian cells, with a titer ∼105 infectious units (IU) per ml on 293T cells, compared to ∼106 I.U./ml on avian cells (Fig. 2A). All of the mutations conferring expanded tropism are within HR1. There did not appear to be a strict correlation between expanded tropism and the level of R99 resistance of the mutants. The expanded infectivity was not restricted to human 293T cells; both V48D and L62A were found to confer infectivity of mouse NIH/3T3 cells and African green monkey COS cells (data not shown), neither of which is normally infectible with the wild-type ASLV-A envelope. However, infectivity on these cell lines was substantially lower than on 293T cells, with 30-fold (3T3) and 140-fold (COS)-lower infectious titers.
A monoclonal antibody against the SU subunit of ASLV-A has recently been reported to block receptor binding and envelope activation (40). In order to further investigate the receptor requirements for expanded tropism, this antibody was tested against the V48D variant, the substitution displaying the greatest infectivity on mammalian cell lines. The V48D envelope was found to be equally sensitive to this antibody as the wild type when examined on QT6 cells, but was less sensitive when mediating infection of human cells (Fig. 2B). This result is consistent with the V48D envelope retaining a requirement for receptor activation, although the reduction in sensitivity on mammalian cells might suggest a divergent receptor-envelope interaction.
Sensitivity of variant envelopes to neutralization.
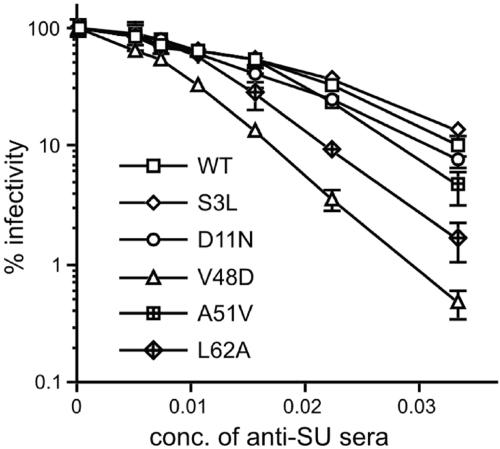
For HIV-1 (24, 26, 32, 63), HIV-2 (53), and simian immunodeficiency virus (35, 42), a reduced requirement for the CD4 receptor is correlated with increased sensitivity to neutralization. To examine any relationship between expanded tropism of ASLV-A and neutralization sensitivity, a panel of six viruses (Fig. 2A), selected to represent an array of phenotypes, was tested against polyclonal antiserum directed against the SU subunit. The pattern of antiserum sensitivity (Fig. 3) generally mirrored 293T infectivity (V48D > L62A > A51V > D11N, S3L and the wild type, with estimated IC50 values of 0.007, 0.011, 0.014, 0.013, 0.014, and 0.014, respectively). However, only the V48D envelope was more sensitive than the wild type by a statistically significant margin (P < 0.01).
FIG. 3.
Neutralization sensitivity of variant envelopes. Neutralization of MLV pseudotypes bearing the ASLV-A envelopes shown, using polyclonal antiserum directed against the SU subunit. Infectivity is shown as % of control (no antiserum) and error bars show standard deviations of experiment performed in quadruplicate on QT6 cells.
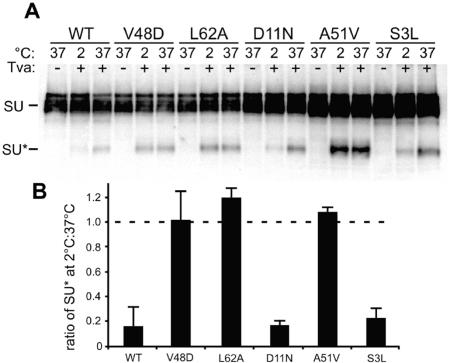
Altered requirements for envelope triggering.
Receptor binding to ASLV Env triggers a series of conformational changes that ultimately lead to membrane fusion. Additionally, triggering of ASLV Env results in increased protease sensitivity of the SU subunit (9, 19). Analysis of SU protease sensitivity was employed to examine whether envelopes with expanded tropism could be triggered independently of soluble receptor. Using the same panel of six viruses as above, envelope triggering, as measured by protease sensitivity, was found to be completely receptor dependent (Fig. 4A). The conformational changes within ASLV Env are strictly temperature dependent and normally occur most efficiently at 37°C (19). This strict temperature dependence was not observed for three of the six envelopes examined (Fig. 4B). A correlation was observed between those envelopes that triggered independently of temperature and expanded tropism, while the tropism of the temperature dependent envelopes was restricted to avian cell lines. Together these data with those presented above suggest that a subset of the peptide resistant envelope proteins have both altered thermodynamic activation and receptor utilization profiles.
FIG. 4.
Altered thermodynamics of ASLV-A envelope triggering. (A) Increased protease sensitivity of SU subunit reveals receptor-triggered conformational change in envelope. Soluble receptor was bound to virus on ice where indicated, then the temperature was either shifted to 37°C or maintained on ice for 15 min as shown. Samples were returned to ice, digested with thermolysin, and resolved by SDS-PAGE and anti-SU Western blot. The positions of unprocessed (SU) and cleaved (SU*) subunit are shown. (B) Some of the mutant envelopes are efficiently triggered by receptor without elevating temperature. The bands from three separate gels were quantitated using [125I]protein A and the ratio of the amount of SU* detected at 2°C compared to 37°C was calculated. Shown are the average ratio and standard deviation for each envelope. The dashed line at a ratio of 1.0 indicates temperature independence.
DISCUSSION
Using ASLV-A as a model for class I envelope function, residues that impact sensitivity to an HR2 peptide inhibitor were identified in two distinct regions of TM, the N-terminal heptad repeat (HR1), and the amino terminus of the subunit (Fig. 1A). The diversity of the thirteen distinct envelope variants described here, as well as the ease with which they were selected, suggests that they represent only a fraction of the possible sensitivity determinants. These mutations increase the R99 IC50 from approximately threefold to more than 1,500-fold (Table 1). The mutations presented two distinct phenotypes, those that displayed expanded tropism and a reduced envelope activation threshold, and those that did not. The former class was only observed with HR1 mutations, although not all HR1 mutations were of this type.
One mechanism whereby substitutions within HR1 could influence R99 sensitivity is by changing HR2 peptide-binding affinity. However, proposing a mechanism of peptide escape for the other mutations (residues 2 to 12 of TM) is less straightforward. A disulfide bond between cysteines at positions 9 and 45 of TM (10) would be expected to bring the amino terminus of TM in proximity to HR1, the target of R99, and thus mutations around position 9 might influence R99-binding affinity through steric hindrance. Indeed, four of the five substitutions in this region are of residues with larger side chains than the wild-type envelope (Table 1). However, this is less apparent for D11N, the change with the strongest resistance to R99. D11E, which preserves the charge at this region while increasing the bulk, has only a modest fourfold effect on peptide sensitivity. This raises the possibility, then, that the negative charge of D11 interacts with other regions of TM within one or more envelope conformations, the disruption of which significantly affects R99 sensitivity.
HIV-1 escape mutants to the HR2 inhibitor enfuvirtide map to residues 36 to 45 of gp41 within the target-binding site for the inhibitor (20, 49, 57). A three-residue motif, GIV (amino acids 36 to 38) within HR1, is a particularly significant region for resistance mutations. Interestingly, all of the ASLV resistant mutations within HR1 also lie within the N-terminal region and none were found in the HR1 C terminus. It is possible that destabilizing mutations at the HR1 N terminus, near the fusion peptide end of the coiled coil, are tolerated because coiled-coil formation initiates at the C terminus and mutations that affect the initiation region are not readily selected. Thus, C terminal mutants could theoretically provide resistance, but they are not seen because function of the TM protein is compromised.
Determinants of baseline sensitivity to peptide inhibitors, however, can also be located in gp120 domains that govern coreceptor specificity (12, 13) as well as a region of gp41 C-terminal to HR1 (21). As the TM subunit of lentiviruses has an N-terminal fusion peptide (15), there is no obvious HIV counterpart to the ASLV segment between the SU/TM cleavage site and its fusion peptide. The results presented here implicate this intervening segment, which is also found in filoviral glycoproteins (16), as a functional component of envelope activation, in addition to identifying an important new region governing HR2 peptide sensitivity. The study of these mutants might provide insight into the role of the TM amino terminus and its relationship to the internal fusion peptide in ASLV and filoviruses. One possibility is that this region acts similarly to the capping structure of influenza HA and helps to bring the apposed membranes together during fusion. It will be interesting to determine if the peptide resistant mutations within the ASLV intervening segment affect the rate of membrane fusion.
An expanded tropism phenotype as was seen in this analysis of ASLV has not been previously reported for any HR2 peptide escape mutant. Determinants of HIV-1 coreceptor specificity within gp120 have been reported to modulate enfuvirtide sensitivity (12, 13), with envelopes that bind coreceptor more efficiently being less sensitive to the inhibitor (45, 47), although this observation has been questioned (20). Thus envelopes with greater coreceptor affinity might be triggered more efficiently, providing less of a target for enfuvirtide inhibition. Whether this increased coreceptor affinity also translates into increased use of alternative coreceptors and expanded tropism of enfuvirtide-insensitive variants has not been studied. Similarly, CD4 independence, and thus an altered glycoprotein activation threshold, of an HIV-2 isolate has been shown to involve either one of two changes within gp41 (48); interestingly, one of these two changes is within the GIV motif that is associated with enfuvirtide resistance, and the other change flanks this motif. The impact of these changes on sensitivity to an HR2-based peptide has not been investigated.
The native structure of influenza hemagglutinin (HA) has been described as metastable (7), where the native form of the glycoprotein on the virion is blocked from a more energetically favorable structure by a thermodynamic barrier. Conformational changes in HA, which can be triggered by acid, heat, or urea, convert the envelope to its lower-energy, fusion-active state. It has been proposed that receptor binding could perform a similar destabilizing role for other viral envelopes (7). As mentioned above, HIV envelopes that exhibit CD4 independence or greater coreceptor affinity demonstrate altered interactions between envelope and receptor(s), and these changes appear to be linked to enfuvirtide sensitivity. Similarly, our analysis of ASLV mutants suggests a model for peptide resistance that, for a subset of the mutants, involves altered triggering of the envelope glycoproteins. Of the thirteen ASLV-A mutants described here, four displayed detectable infectivity on 293T cells. This represents one-half (four out of eight) of the alterations within HR1, illustrating that this phenotype is not uncommon. The activation threshold for the expanded tropism mutant envelopes appears to be lower, as reflected by their in vitro requirements for receptor-mediated triggering (Fig. 4), revealing a potential mechanism by which alternative receptors might trigger these mutants. Such a mechanism would not require a change in the binding affinity for the putative alternative receptor(s). A single amino acid substitution in the SU subunit of the ASLV-B envelope also confers a similar expanded tropism, and it has been suggested that the mechanism for this phenotype involves not receptor affinity but rather the fusogenic capability of the envelope (43).
The TM substitutions that conferred expanded tropism were distinguishable by their slightly increased sensitivity to neutralization as well (Fig. 3). Some enfuvirtide resistance mutations of HIV have also been noted to be more sensitive to neutralization (46). This change in sensitivity may reflect a destabilized native conformation, in which access to neutralizing epitopes is enhanced; alternatively, it may indicate a modification of the conformational changes in envelope such that a distinct set of epitopes is displayed, or that the epitopes are exposed for a longer period of time.
The experiments described here characterize envelope function with single-round infection assays, so it is possible that some or all of the mutations might not be well tolerated in the absence of R99 selection. For HIV-1, viral fitness is decreased for enfuvirtide-selected mutants (30). However, all of the ASLV-A mutant envelopes reported here mediated infection of avian QT6 cells with wild-type efficiency (Fig. 2A and data not shown). In addition, production of replication competent ASLV encoding the L62A envelope variant that displays peptide resistance and expanded tropism did not result in rapid reversion to wild-type sequence (data not shown). Furthermore, the T2I substitution has been found in natural ASLV isolates (28, 54), and the D11E change has been observed in an endogenous, subtype J-like sequence (11). The functional impact of these natural variants has not been explored.
Peptide inhibitors analogous to enfuvirtide and R99 have been described or proposed for a wide variety of human pathogens that encode class I membrane fusion proteins, including severe acute respiratory syndrome (SARS) coronavirus (4, 29), Ebola virus (56), Nipah and Hendra viruses (6), HTLV (41, 51), influenza virus, respiratory syncytial virus, parainfluenza virus, and measles virus (27). The demonstration of the reduced activation threshold of some HR2 peptide-resistant variants may have important consequences for the effective use of this class of inhibitor in antiviral therapy. Although expanded viral host range would be detrimental in vivo, our results also suggest that immune system pressure might provide a counterbalance by selecting against such variant envelopes due to their increased sensitivity to neutralization. These studies thus highlight the requirement for more analysis of variant viruses that are resistant to peptide entry inhibitors.
Acknowledgments
We thank Jackie Reeves for critical reading of the manuscript, Eric Hunter and Christina Ochsenbauer-Jambor for providing mc8C5-4, Peter Vogt and Makoto Nishizawa for pRV-9, Mark Federspiel for RCASBP(A)-GFP-infected DF-1 cells, and John Young for the SUA-rIgG expression plasmid used for generating antisera.
This work was funded by Public Health Service grants F32-AI050341 (S.M.A.), T32-GM07229 (R.C.N.), R01-AI43455 (P.B.), and R01-CA76256 (P.B.).
REFERENCES
- 1.Balliet, J. W. 1998. Early events in subgroup A avian sarcoma and leukosis virus entry. Ph.D. thesis. University of Pennsylvania, Philadelphia, Pa.
- 2.Balliet, J. W., J. Berson, C. M. D'Cruz, J. Huang, J. Crane, J. M. Gilbert, and P. Bates. 1999. Production and characterization of a soluble, active form of Tva, the subgroup A avian sarcoma and leukosis virus receptor. J. Virol. 73:3054-3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bates, P., J. A. T. Young, and H. E. Varmus. 1993. A receptor for subgroup A Rous sarcoma virus is related to the low density lipoprotein receptor. Cell 74:1043-1051. [DOI] [PubMed] [Google Scholar]
- 4.Bosch, B. J., B. E. E. Martina, R. van der Zee, J. Lepault, B. J. Haijema, C. Versluis, A. J. R. Heck, R. de Groot, A. D. M. E. Osterhaus, and P. J. M. Rottier. 2004. Severe acute respiratory syndrome coronavirus (SARS-CoV) infection inhibition using spike protein heptad repeat-derived peptides. Proc. Natl. Acad. Sci. USA 101:8455-8460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bosch, B. J., R. van der Zee, C. A. M. de Haan, and P. J. M. Rottier. 2003. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J. Virol. 77:8801-8811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bossart, K. N., L.-F. Wang, M. N. Flora, K. B. Chua, S. K. Lam, B. T. Eaton, and C. C. Broder. 2002. Membrane fusion tropism and heterotypic functional activities of the Nipah virus and Hendra virus envelope glycoproteins. J. Virol. 76:11186-11198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carr, C. M., C. Chaudhry, and P. S. Kim. 1997. Influenza hemagglutinin is spring-loaded by a metastable native conformation. Proc. Natl. Acad. Sci. USA 94:14306-14313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colman, P. M., and M. C. Lawrence. 2003. The structural biology of type I viral membrane fusion. Nat. Rev. Mol. Cell Biol. 4:309-319. [DOI] [PubMed] [Google Scholar]
- 9.Damico, R., L. Rong, and P. Bates. 1999. Substitutions in the receptor-binding domain of the avian sarcoma and leukosis virus envelope uncouple receptor-triggered structural rearrangements in the surface and transmembrane subunits. J. Virol. 73:3087-3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delos, S. E., and J. M. White. 2000. Critical role for the cysteines flanking the internal fusion peptide of avian sarcoma/leukosis virus envelope glycoprotein. J. Virol. 74:9738-9741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Denesvre, C., D. Soubieux, G. Pin, D. Hue, and G. Dambrine. 2003. Interference between avian endogenous ev/J. 4.1 and exogenous ALV-J. retroviral envelopes. J. Gen. Virol. 84:3233-3238. [DOI] [PubMed] [Google Scholar]
- 12.Derdeyn, C. A., J. M. Decker, J. N. Sfakianos, X. Wu, W. A. O'Brien, L. Ratner, J. C. Kappes, G. M. Shaw, and E. Hunter. 2000. Sensitivity of human immunodeficiency virus type 1 to the fusion inhibitor T-20 is modulated by coreceptor specificity defined by the V3 loop of gp120. J. Virol. 74:8358-8367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Derdeyn, C. A., J. M. Decker, J. N. Sfakianos, Z. Zhang, W. A. O'Brien, L. Ratner, G. M. Shaw, and E. Hunter. 2001. Sensitivity of human immunodeficiency virus type 1 to fusion inhibitors targeted to the gp41 first heptad repeat involves distinct regions of gp41 and is consistently modulated by gp120 interactions with the coreceptor. J. Virol. 75:8605-8614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earp, L. J., S. E. Delos, R. C. Netter, P. Bates, and J. M. White. 2003. The avian retrovirus avian sarcoma/leukosis virus subtype A reaches the lipid mixing stage of fusion at neutral pH. J. Virol. 77:3058-3066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Epand, R. M. 2003. Fusion peptides and the mechanism of viral fusion. Biochim. Biophys. Acta 1614:116-121. [DOI] [PubMed] [Google Scholar]
- 16.Gallaher, W. R. 1996. Similar structural models of the transmembrane proteins of Ebola and avian sarcoma viruses. Cell 85:477-478. [DOI] [PubMed] [Google Scholar]
- 17.Gallaher, W. R., C. DiSimone, and M. J. Buchmeier. 2001. The viral transmembrane superfamily: possible divergence of Arenavirus and Filovirus glycoproteins from a common RNA virus ancestor. BMC Microbiol. 1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilbert, J. M., P. Bates, H. E. Varmus, and J. M. White. 1994. The receptor for the subgroup A avian leukosis-sarcoma viruses binds to subgroup A but not to subgroup C envelope glycoprotein. J. Virol. 68:5623-5628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilbert, J. M., L. D. Hernandez, J. W. Balliet, P. Bates, and J. M. White. 1995. Receptor-induced conformational changes in the subgroup A avian leukosis and sarcoma virus envelope glycoprotein. J. Virol. 69:7410-7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greenberg, M. L., and N. Cammack. 2004. Resistance to enfuvirtide, the first HIV fusion inhibitor. J. Antimicrob. Chemother. 54:333-340. [DOI] [PubMed] [Google Scholar]
- 21.Heil, M. L., J. M. Decker, J. N. Sfakianos, G. M. Shaw, E. Hunter, and C. A. Derdeyn. 2004. Determinants of human immunodeficiency virus type 1 baseline susceptibility to the fusion inhibitors enfuvirtide and T-649 reside outside the peptide interaction site. J. Virol. 78:7582-7589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heinz, F. X., and S. L. Allison. 2001. The machinery for flavivirus fusion with host cell membranes. Curr. Opin. Microbiol. 4:450-455. [DOI] [PubMed] [Google Scholar]
- 23.Hernandez, L. D., and J. M. White. 1998. Mutational analysis of the candidate internal fusion peptide of the avian leukosis and sarcoma virus subgroup A envelope glycoprotein. J. Virol. 72:3259-3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoffman, T. L., C. C. LaBranche, W. Zhang, G. Canziani, J. Robinson, I. Chaiken, J. A. Hoxie, and R. W. Doms. 1999. Stable exposure of the coreceptor-binding site in a CD4-independent HIV-1 envelope protein. Proc. Natl. Acad. Sci. USA 96:6359-6364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang, S., K. Lin, N. Strick, and A. R. Neurath. 1993. HIV-1 inhibition by a peptide. Nature 365:113. [DOI] [PubMed] [Google Scholar]
- 26.Kolchinsky, P., E. Kiprilov, and J. Sodroski. 2001. Increased neutralization sensitivity of CD4-independent human immunodeficiency virus variants. J. Virol. 75:2041-2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lambert, D. M., S. Barney, A. L. Lambert, K. Guthrie, R. Medinas, D. E. Davis, T. Bucy, J. Erickson, G. Merutka, and S. R. Petteway, Jr. 1996. Peptides from conserved regions of paramyxovirus fusion (F) proteins are potent inhibitors of viral fusion. Proc. Natl. Acad. Sci. USA 93:2186-2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leamnson, R. N., and P. R. Shank. 1986. Nucleotide sequence comparison of the 3′ regions of avian retroviruses NY203 and NTRE-2. Virology 151:139-145. [DOI] [PubMed] [Google Scholar]
- 29.Liu, S., G. Xiao, Y. Chen, Y. He, J. Niu, C. R. Escalante, H. Xiong, J. Farmar, A. K. Debnath, P. Tien, and S. Jiang. 2004. Interaction between heptad repeat 1 and 2 regions in spike protein of SARS-associated coronavirus: implications for virus fusogenic mechanism and identification of fusion inhibitors. Lancet 363:938-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lu, J., P. Sista, F. Giguel, M. Greenberg, and D. R. Kuritzkes. 2004. Relative replicative fitness of human immunodeficiency virus type 1 mutants resistant to enfuvirtide (T-20). J. Virol. 78:4628-4637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malashkevich, V. N., B. J. Schneider, M. L. McNally, M. A. Milhollen, J. X. Pang, and P. S. Kim. 1999. Core structure of the envelope glycoprotein GP2 from Ebola virus at 1.9-Å resolution. Proc. Natl. Acad. Sci. USA 96:2662-2667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martín, J., C. C. LaBranche, and F. González-Scarano. 2001. Differential CD4/CCR5 utilization, gp120 conformation, and neutralization sensitivity between envelopes from a microglia-adapted human immunodeficiency virus type 1 and its parental isolate. J. Virol. 75:3568-3580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matsuyama, S., S. E. Delos, and J. M. White. 2004. Sequential roles of receptor binding and low pH in forming prehairpin and hairpin conformations of a retroviral envelope glycoprotein. J. Virol. 78:8201-8209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matthews, T., M. Salgo, M. Greenberg, J. Chung, R. DeMasi, and D. Bolognesi. 2004. Enfuvirtide: the first therapy to inhibit the entry of HIV-1 into host CD4 lymphocytes. Nat. Rev. Drug Discov. 3:215-225. [DOI] [PubMed] [Google Scholar]
- 35.Means, R. E., T. Matthews, J. A. Hoxie, M. H. Malim, T. Kodama, and R. C. Desrosiers. 2001. Ability of the V3 loop of simian immunodeficiency virus to serve as a target for antibody-mediated neutralization: correlation of neutralization sensitivity, growth in macrophages, and decreased dependence on CD4. J. Virol. 75:3903-3915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller, A. D., and G. J. Rosman. 1989. Improved retroviral vectors for gene transfer and expression. BioTechniques 7:980-990. [PMC free article] [PubMed] [Google Scholar]
- 37.Netter, R. C., S. M. Amberg, J. W. Balliet, M. J. Biscone, A. Vermeulen, L. J. Earp, J. M. White, and P. Bates. 2004. Heptad repeat 2-based peptides inhibit avian sarcoma and leukosis virus subgroup A infection and identify a fusion intermediate. J. Virol. 78:13430-13439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nishizawa, M., S.-L. Fu, K. Kataoka, and P. K. Vogt. 2003. Artificial oncoproteins: modified versions of the yeast bZip protein GCN4 induce cellular transformation. Oncogene 22:7931-7941. [DOI] [PubMed] [Google Scholar]
- 39.Nykjaer, A., and T. E. Willnow. 2002. The low-density lipoprotein receptor gene family: a cellular Swiss army knife? Trends Cell Biol. 12:273-280. [DOI] [PubMed] [Google Scholar]
- 40.Ochsenbauer-Jambor, C., S. E. Delos, M. A. Accavitti, J. M. White, and E. Hunter. 2002. Novel monoclonal antibody directed at the receptor binding site on the avian sarcoma and leukosis virus Env complex. J. Virol. 76:7518-7527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Piñón, J. D., S. M. Kelly, N. C. Price, J. U. Flanagan, and D. W. Brighty. 2003. An antiviral peptide targets a coiled-coil domain of the human T-cell leukemia virus envelope glycoprotein. J. Virol. 77:3281-3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Puffer, B. A., S. Pöhlmann, A. L. Edinger, D. Carlin, M. D. Sanchez, J. Reitter, D. D. Watry, H. S. Fox, R. C. Desrosiers, and R. W. Doms. 2002. CD4 independence of simian immunodeficiency virus Envs is associated with macrophage tropism, neutralization sensitivity, and attenuated pathogenicity. J. Virol. 76:2595-2605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rainey, G. J. A., A. Natonson, L. F. Maxfield, and J. M. Coffin. 2003. Mechanisms of avian retroviral host range extension. J. Virol. 77:6709-6719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rapaport, D., M. Ovadia, and Y. Shai. 1995. A synthetic peptide corresponding to a conserved heptad repeat domain is a potent inhibitor of Sendai virus-cell fusion: an emerging similarity with functional domains of other viruses. EMBO J. 14:5524-5531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reeves, J. D., S. A. Gallo, N. Ahmad, J. L. Miamidian, P. E. Harvey, M. Sharron, S. Pöhlmann, J. N. Sfakianos, C. A. Derdeyn, R. Blumenthal, E. Hunter, and R. W. Doms. 2002. Sensitivity of HIV-1 to entry inhibitors correlates with envelope/coreceptor affinity, receptor density, and fusion kinetics. Proc. Natl. Acad. Sci. USA 99:16249-16254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reeves, J. D., F. H. Lee, J. L. Miamidian, C. B. Jabara, M. M. Juntilla, and R. W. Doms. 2005. Enfuvirtide resistance mutations: impact on human immunodeficiency virus envelope function, entry inhibitor sensitivity, and virus neutralization. J. Virol. 79:4991-4999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reeves, J. D., J. L. Miamidian, M. J. Biscone, F.-H. Lee, N. Ahmad, T. C. Pierson, and R. W. Doms. 2004. Impact of mutations in the coreceptor binding site on human immunodeficiency virus type 1 fusion, infection, and entry inhibitor sensitivity. J. Virol. 78:5476-5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reeves, J. D., and T. F. Schulz. 1997. The CD4-independent tropism of human immunodeficiency virus type 2 involves several regions of the envelope protein and correlates with a reduced activation threshold for envelope-mediated fusion. J. Virol. 71:1453-1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rimsky, L. T., D. C. Shugars, and T. J. Matthews. 1998. Determinants of human immunodeficiency virus type 1 resistance to gp41-derived inhibitory peptides. J. Virol. 72:986-993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rong, L., K. Gendron, and P. Bates. 1998. Conversion of a human low-density lipoprotein receptor ligand-binding repeat to a virus receptor: identification of residues important for ligand specificity. Proc. Natl. Acad. Sci. USA 95:8467-8472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sagara, Y., Y. Inoue, H. Shiraki, A. Jinno, H. Hoshino, and Y. Maeda. 1996. Identification and mapping of functional domains on human T-cell lymphotropic virus type 1 envelope proteins by using synthetic peptides. J. Virol. 70:1564-1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Soneoka, Y., P. M. Cannon, E. E. Ramsdale, J. C. Griffiths, G. Romano, S. M. Kingsman, and A. J. Kingsman. 1995. A transient three-plasmid expression system for the production of high titer retroviral vectors. Nucleic Acids Res. 23:628-633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomas, E. R., C. Shotton, R. A. Weiss, P. R. Clapham, and A. McKnight. 2003. CD4-dependent and CD4-independent HIV-2: consequences for neutralization. AIDS 17:291-300. [DOI] [PubMed] [Google Scholar]
- 54.Tomioka, Y., K. Ochiai, K. Ohashi, E. Ono, T. Toyoda, T. Kimura, and T. Umemura. 2004. Genome sequence analysis of the avian retrovirus causing so-called fowl glioma and the promoter activity of the long terminal repeat. J. Gen. Virol. 85:647-652. [DOI] [PubMed] [Google Scholar]
- 55.Volchkov, V. E., V. M. Blinov, and S. V. Netesov. 1992. The envelope glycoprotein of Ebola virus contains an immunosuppressive-like domain similar to oncogenic retroviruses. FEBS Lett. 305:181-184. [DOI] [PubMed] [Google Scholar]
- 56.Watanabe, S., A. Takada, T. Watanabe, H. Ito, H. Kida, and Y. Kawaoka. 2000. Functional importance of the coiled-coil of the Ebola virus glycoprotein. J. Virol. 74:10194-10201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wei, X., J. M. Decker, H. Liu, Z. Zhang, R. B. Arani, J. M. Kilby, M. S. Saag, X. Wu, G. M. Shaw, and J. C. Kappes. 2002. Emergence of resistant human immunodeficiency virus type 1 in patients receiving fusion inhibitor (T-20) monotherapy. Antimicrob. Agents Chemother. 46:1896-1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weissenhorn, W., A. Carfí, K.-H. Lee, J. J. Skehel, and D. C. Wiley. 1998. Crystal structure of the Ebola virus membrane fusion subunit, GP2, from the envelope glycoprotein ectodomain. Mol. Cell 2:605-616. [DOI] [PubMed] [Google Scholar]
- 59.Westenberg, M., H. Wang, W. F. J. IJkel, R. W. Goldbach, J. M. Vlak, and D. Zuidema. 2002. Furin is involved in baculovirus envelope fusion protein activation. J. Virol. 76:178-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wild, C., T. Oas, C. McDanal, D. Bolognesi, and T. Matthews. 1992. A synthetic peptide inhibitor of human immunodeficiency virus replication: correlation between solution structure and viral inhibition. Proc. Natl. Acad. Sci. USA 89:10537-10541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wild, C. T., D. C. Shugars, T. K. Greenwell, C. B. McDanal, and T. J. Matthews. 1994. Peptides corresponding to a predictive alpha-helical domain of human immunodeficiency virus type 1 gp41 are potent inhibitors of virus infection. Proc. Natl. Acad. Sci. USA 91:9770-9774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wool-Lewis, R. J., and P. Bates. 1998. Characterization of Ebola virus entry by using pseudotyped viruses: identification of receptor-deficient cell lines. J. Virol. 72:3155-3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang, P. F., P. Bouma, E. J. Park, J. B. Margolick, J. E. Robinson, S. Zolla-Pazner, M. N. Flora, and G. V. Quinnan, Jr. 2002. A variable region 3 (V3) mutation determines a global neutralization phenotype and CD4-independent infectivity of a human immunodeficiency virus type 1 envelope associated with a broadly cross-reactive, primary virus-neutralizing antibody response. J. Virol. 76:644-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zingler, K., and J. A. T. Young. 1996. Residue Trp-48 of Tva is critical for viral entry but not for high-affinity binding to the SU glycoprotein of subgroup A avian leukosis and sarcoma viruses. J. Virol. 70:7510-7516. [DOI] [PMC free article] [PubMed] [Google Scholar]