Abstract
Cross-sectional studies have shown that the capacity of CD8+ cells from human immunodeficiency virus (HIV)-infected patients and simian immunodeficiency virus (SIV) SIVmac-infected macaques to suppress the replication of human and simian immunodeficiency viruses in vitro depends on the clinical stage of disease, but little is known about changes in this antiviral activity over time in individual HIV-infected patients or SIV-infected macaques. We assessed changes in the soluble factor-mediated noncytolytic antiviral activity of CD8+ cells over time in eight cynomolgus macaques infected with SIVmac251 to determine the pathophysiological role of this activity. CD8+ cell-associated antiviral activity increased rapidly in the first week after viral inoculation and remained detectable during the early phase of infection. The net increase in antiviral activity of CD8+ cells was correlated with plasma viral load throughout the 15 months of follow-up. CD8+ cells gradually lost their antiviral activity over time and acquired virus replication-enhancing capacity. Levels of antiviral activity correlated with CD4+ T-cell counts after viral set point. Concentrations of β-chemokines and interleukin-16 in CD8+ cell supernatants were not correlated with this antiviral activity, and α-defensins were not detected. The soluble factor-mediated antiviral activity of CD8+ cells was neither cytolytic nor restricted to major histocompatibility complex. This longitudinal study strongly suggests that the increase in noncytolytic antiviral activity from baseline and the maintenance of this increase over time in cynomolgus macaques depend on both viral replication and CD4+ T cells.
CD8+ T lymphocytes are thought to play a major role in controlling human and simian immunodeficiency virus replication (5, 24, 28, 58) through direct lysis of human immunodeficiency virus (HIV)/simian immunodeficiency virus (SIV) antigen-expressing target cells in a major histocompatibilty complex (MHC) class 1-restricted manner, and, through noncytotolytic antiviral response (35, 44, 68; reviewed in reference 24), mainly due to an as-yet-undetermined cell antiviral factor (CAF) (9, 14, 37, 41, 67).
Despite the many efforts made over the last 18 years to identify CAF, this molecule remains elusive. It does not seem to correspond to known cytokines, including alpha interferons (α-IFN), IFN-β, and IFN-γ, tumor necrosis factor alpha, and interleukin-1 (IL-1) to IL-13, IL-15, IL-16, and IL-18 (42), although some of the noncytolytic antiviral activity of CD8+ T cells can be attributed to β-chemokines such as MIP-1α, MIP-1β, and RANTES, which inhibit HIV entry by binding to one of its coreceptors, CCR5, but do not inhibit the replication of CXCR4 using viruses (2, 14, 34, 63). CAF is not restricted by MHC class I molecules and inhibits virus production at the transcriptional level (13, 16, 37, 40), in various types of cell (2, 59). Similar noncytotoxic CD8+ cell antiviral responses have also been reported in nonhuman primate models (7, 8, 11, 12, 20, 29, 39, 51, 69).
Several observations suggest that noncytolytic antiviral response may play a role in controlling infection and/or prevent the development of AIDS. This antiviral activity was detected during primary infection coinciding with or preceding the decrease in plasma viral load (PVL) in both HIV type 1 (HIV-1)-infected patients and SIVmac-infected rhesus macaques (44, 69), was correlated with circulating CD4+ T-cell counts during the asymptomatic stages of chronic HIV infection (10, 43, 56), but was low in patients with AIDS (43). The decrease in noncytolytic antiviral activity with progression has been confirmed by a longitudinal study (31); however, that study included only five patients followed from asymptomatic phase to AIDS and did not take into account the role of soluble factors.
Noncytolytic antiviral activity is also associated with the absence of progression to AIDS in both HIV-1-infected patients (long-term nonprogressors [LTNP]) (4) and nonhuman primate models (12, 20, 51), further suggesting that it may favor the persistence of clinical good health. However, most of the evidence supporting this hypothesis comes from cross-sectional studies, which may not be entirely appropriate for analysis of the relationship between this activity and other progression markers, and the mechanisms by which soluble factor-mediated noncytolytic antiviral activity is downregulated during symptomatic stages remain unknown.
Nonhuman primates infected with SIV are the most relevant models of HIV infection and AIDS (19, 33, 52, 60) and are particularly suitable for studies concerning the leveling off of the immune response in the early phase of infection. Cynomolgus macaque and Chinese rhesus macaque SIV infection models provide the closest match to human HIV-1 infection and progression profiles (38, 53, 62), particularly with regard to the recently reported diversity of virus load set points in untreated HIV-1-infected patients (26, 27, 45, 54, 57).
We carried out a longitudinal study of the soluble factor-mediated antiviral activity of CD8+ cells in cynomolgus macaques, from primary infection with SIVmac to the development of immunodeficiency, to elucidate the mechanisms underlying the triggering of this antiviral activity and its maintenance or loss over time.
MATERIALS AND METHODS
Animals.
Eighteen adult cynomolgus macaques (Macaca fascicularis) imported from Mauritius were included in the present study. They tested negative for SIV, herpesvirus B, filovirus, STLV-1, SRV-1, SRV-2, measles, hepatitis B-HbsAg, and hepatitis B-HbcAb before inclusion in the study. Animals were housed in single cages within level 3 biosafety facilities and were handled in accordance with EC guidelines for experiments using nonhuman primates (Journal Officiel des Communautés Européennes, L358, December 18, 1986). Macaques were anesthetized with 10 to 20 mg of ketamine (Imalgène; Rhône-Mérieux, Lyon, France)/kg before each blood sample was taken.
Virus inoculation.
Macaques were inoculated via the saphenous vein, with 50 AID50 (50% animal infectious dose) of pathogenic SIVmac251 (kindly provided by A. M. Aubertin, Université Louis Pasteur, Strasbourg, France) in 1 ml of phosphate-buffered saline (PBS). The virus stock used was a cell-free supernatant of rhesus macaque peripheral blood mononuclear cells (PBMC) infected in vitro with a culture supernatant obtained by the coculture of rhesus PBMC and a spleen homogenate from a rhesus macaque infected with SIVmac251 (provided by R. C. Desrosiers, New England Regional Primate Center, Southborough, MA). The stock was titrated after intravenous, intrarectal, and intravaginal inoculation (33, 50).
Determination of T-lymphocyte subsets.
The percentages of CD4+- and CD8+ T-lymphocytes were determined by flow cytometry using direct immunofluorescence labeling. We incubated 3 × 105 PBMC for 30 min at 4°C with fluorochrome-labeled anti-rhesus CD3 monoclonal antibody (MAb; clone FN18; Biosource International, California) and anti-human CD8 MAb (DK25; Dako, Glostrup, Denmark) or anti-human CD4 MAb (MT310; Dako, Glostrup, Denmark). Isotype-matched fluorescein isothiocyanate- and phycoerythrin-conjugated immunoglobulins (Immunotech, Marseilles, France) were used as controls. Stained cells were washed twice in PBS and fixed (Cell-fix; BD Biosciences, San Diego, CA). The data were acquired with a Facscan cytometer. We analyzed at least 5,000 events in the lymphocyte gate, defined by forward and side scatter plots, using CellQuest software (BD Biosciences, San Diego, CA).
PVL.
PVLs were measured as previously described (66). Blood samples were collected into EDTA; plasma was separated from blood cells by centrifugation and stored at −80°C before testing. A quantitative nucleic acid probe-linked enzyme-linked immunosorbent assay (ELISA) was used to determine viral loads in plasma as previously described (6, 66). Standards of 0.1 × 107 to 2 × 107 RNA copies/ml diluted in plasma from noninfected macaques, negative controls, and 200-μl plasma samples were treated with a commercial high-purity viral RNA extraction kit (Roche Diagnostics, Mannheim, Germany). We then used 10 μl of the extracted viral RNA for DIG-labeling reverse transcription-PCR in a final volume of 50 μl containing 10 mM Tris-HCl (pH 8.3); 1.5 mM MgCl2; 50 mM KCl; 0.25 mM concentrations of dATP, dCTP, and dGTP; 0.24 mM dTTP; 10 μM digoxigenin-11-dUTP (PCR DIG Labeling Mix; Roche Diagnostics, Mannheim, Germany); 10 pmol of each primer specific for the SIV gag gene (primers GAG98 5′--ATGTAGTATGGGCAAACGAAT--3′ and GAG356 5′--GTGCTGTTGGTCTACTTGTTTTTG--3′); 20 U of recombinant RNase inhibitor (RNAsin; Promega, Madison, WI), 12.5 U of Moloney murine leukemia virus reverse transcriptase (Perkin-Elmer, Wellesley, MA); and 1.25 U of Taq polymerase (Roche Diagnostics). The volume was adjusted to 50 μl per reaction with water. The tubes were subjected to reverse transcription for 25 min at 42°C, followed by denaturation for 5 min at 94°C, and 35 PCR cycles consisting of denaturation (35 s at 94°C), annealing (45 s at 60°C), and extension (1 min at 72°C). The tubes were heated for an additional 5 min at 60°C and 5 min at 72°C at the end of the PCR. We then used 10 μl of the amplification products for ELISA-DIG detection (Roche Diagnostics), using a probe specific for the gag gene (GAG12S, 5′--GATTTGGATTAGCAGAAAGCCTGTTGGAGAACAAAGAAGGATGTCAA--3′) according to the manufacturer's instructions. This made it possible to quantify samples by colorimetry (405 nm, Dynex MRX II; Dynex, Issy les Moulineaux, France), with a detection limit of 25 SIV RNA copies per ml. This method has been used routinely in previous work (6, 48).
Enrichment and activation of CD8+ cells.
Blood samples were diluted 1:2 in PBS, and PBMC were isolated by centrifugation on a Ficoll cushion (MSL; Eurobio, Courtaboeuf, France). CD8+ T cells were positively selected on immunomagnetic beads coated with anti-CD8 antibodies (Miltenyi, Bergisch Gladbach, Germany). The purity of positively selected CD8+ cells was consistently >95%, as determined by flow cytometry. CD8+ cells were suspended at a density of 3 × 106 cells/ml in RPMI 1640 medium supplemented with 10% heat-decomplemented fetal calf serum (FCS), and 20 U of recombinant human IL-2 (Roche Diagnostics)/ml. They were then stimulated by incubation for 3 days with 5 μg of concanavalin A (Boehringer Mannheim, Mannheim, Germany)/ml at 37°C. The culture supernatant was discarded, cells were washed, resuspended in fresh medium at a density of 3 × 106 cells/ml, and incubated for a further 3 days. Day 6 supernatants were collected, frozen and stored until testing for the suppression of viral replication.
Suppression of SIV replication by CD8+ cell culture supernatants.
We assessed the antiviral activity of CD8+ cell culture supernatants by measuring the inhibition of SIVmac251 replication in primary CD4+ T cells. This culture system was more suitable for the large-scale screening of series of supernatants than macaque CD4+ cells, which can only be obtained in limited quantities as the volume of blood samples that can be taken from cynomolgus macaques is limited. SIVmac251 replicated more consistently and reproducibly in human cells than in macaque cells in preliminary experiments.
Peripheral blood lymphocytes from normal human donors were stimulated by incubation for 2 days with phytohemagglutinin P (1:2,000 dilution; Difco) in IL-2 (20 U/ml)-supplemented RPMI medium. The peripheral blood lymphocytes were then washed and cultured for 24 h in RPMI medium supplemented with 10% FCS, antibiotics, glutamine, and IL-2 (20 U/ml). We then enriched the cell suspension in activated CD4+ T cells, using immunomagnetic beads coated with anti-CD4 antibodies (Miltenyi). The resulting cell preparations contained more than 95% CD4+ T cells, as shown by flow cytometry, and were used as target cells.
A stock of SIVmac251 produced in CEMX174 cells was titrated on activated human CD4+ T cells. We mixed 105 activated human CD4+ T cells with SIVmac (100 TCID50) and cultured them in RPMI 1640 medium supplemented with rhuIL-2 (20 U/ml) in triplicate wells (105 cells per well), alone (positive control for virus replication), or in the presence of a 1:5 dilution of the CD8+ cell supernatant to be tested (day 6 of CD8+ cell cultures), in 96-well flat-bottom plates, with a final volume of 200 μl per well. Positive controls for the inhibition of SIV replication were included by adding 10 mM zidovudine to triplicate wells in each assay. Twice weekly, we collected 100 μl of supernatant, which was then frozen and stored. The collected supernatant was replaced with 100 μl of fresh medium supplemented with a 1:5 dilution of the same CD8+ cell culture supernatant. Virus production was followed by measuring reverse transcriptase (RT) activity in supernatant fluids with a commercial immunoassay as previously described (17) (Retrosys; Innovagen, Lund, Sweden). The percentage suppression was calculated as follows by using RT concentrations of supernatants collected 6 days after SIV infection: suppression = {1 − [(mean RT concentration in triplicate wells supplemented with a 1:5 dilution of CD8+ cell supernatant)/(mean RT concentration in triplicate wells cultivated without CD8 cell supernatant)]} × 100.
This assay may be influenced by the presence of multiple components in the supernatants, since enhancement and inhibition of virus production can both be detected.
CD4+ T-cell viability assay.
Cell preparations enriched in activated CD4+ T cells were cultured for 3 days in 96-well plates (105 cells per well). The cells were cultured in RPMI medium supplemented with 10% FCS, antibiotics, 200 mM l-glutamine, and 20 U of recombinant human IL-2/ml in the presence of a 1:5 dilution of CD8+ cell supernatants or without such supernatants as a control.
After 3 days in culture, the cells were washed in PBS and viability tested as reported previously (46). We added 200 μl of 0.005% (wt/vol) neutral red dye in culture medium to each well and incubated the cells at 37°C, in an atmosphere containing 5% CO2, for 1 h. We then washed the cells and added 200 μl of 1% acetic acid-50% aqueous ethanol. Five minutes later, we determined the optical density at 540 nm by using an automatic microplate reader (Microplate Autoreader EL311; Bio-Tek Instruments, Inc., Winooski, VT). Wells containing CD4+ T cells incubated with CD8+ cell supernatant were compared to control wells containing CD4+ T cells incubated in the absence of CD8+ cell supernatant.
Chemokine ELISA.
Concentrations of RANTES, MIP-1α, and MIP-1β were determined in CD8+ cell culture supernatants (day 6) by means of an in-house ELISA. Microtiter plates (Immunoplate, Maxisorp; Nunc, Roskilde, Denmark) were coated with 100 μl/well of a 4-μg/ml solution of monoclonal antibody to human RANTES, MIP-1α, or MIP-1β (R&D Systems, Abingdon, United Kingdom) in PBS. Plates were incubated overnight at room temperature and then washed with 0.1% Tween 20 in PBS. We added 300 μl of blocking buffer (1% bovine serum albumin in PBS) to each well, and the plates were incubated for 1 h at room temperature. The plates were washed, and we then added the human recombinant proteins used as standards (R&D Systems), and the samples, in duplicate (100 μl/well). The plates were then incubated for 2 h at room temperature. They were washed, and 100 μl of biotinylated anti-human RANTES, MIP-1α, or MIP-1β detection antibody (5 to 20 μg/ml; R&D Systems) was added. Plates were incubated for 2 h at room temperature and washed three times with 300 μl of 0.1% Tween 20 in PBS, and 100 μl of streptavidin-horseradish peroxidase (Zymed, San Francisco, CA)/well was added. The plates were incubated for 20 min at room temperature and then washed with PBS-Tween. We added tetramethylbenzidine substrate (ICN, Aurora, OH) and incubated the plates for 20 min at room temperature in the dark. The reaction was stopped by adding 50 μl of 2 M H2SO4 per well. The optical density of each sample and standard was determined by using a microtiter plate reader set at 450 nm.
Defensin ELISA.
Concentrations of α-defensins were determined in CD8+ cell supernatants by means of an ELISA kit specific for human neutrophil protein1-3 (HyCult Biotechnology, Norwood, MA). Cross-reactivity with macaque defensins was confirmed, using supernatants from human and simian polymorphonuclear cells as positive controls in preliminary experiments (data not shown).
IL-16 ELISA.
Concentrations of IL-16 were determined in CD8+ cell supernatants by means of an ELISA kit developed for human interleukin-16, but cross-reacting with macaque IL-16 (Biosource International, California).
Statistical analysis.
Statistical analysis was carried out by using the nonparametric Wilcoxon rank sum test and analysis of variance (ANOVA). Differences between the three groups were analyzed by means of the Kruskal-Wallis test. Correlations between two sets of data were evaluated by means of the Spearman's rank correlation test, using Statview Software (SAS Institute, Inc., Cary, NC). A P value of <0.05 was taken to indicate statistical significance.
RESULTS
Antiviral activities in SIVmac251-infected cynomolgus macaques.
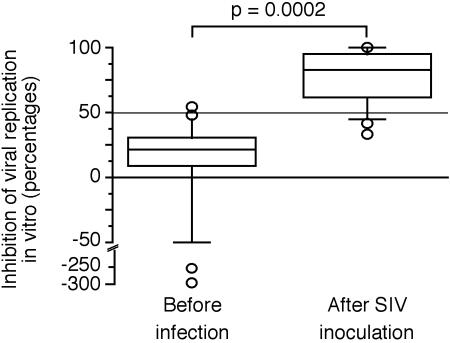
Soluble-factor-mediated antiviral activity of CD8+ cells isolated from 18 macaques recently infected with a pathogenic SIVmac251 biological isolate (second month after infection) was compared to that of CD8+ cells isolated from the same macaques before infection. Supernatants of CD8+ cells cultured after SIV infection inhibited more strongly SIV replication than supernatants of CD8+ cells isolated before infection (Fig. 1; Wilcoxon rank sum test, P = 0.0002). Most of the supernatants from uninfected animals displayed only weak inhibition (<50%), whereas most of the CD8+ cells isolated after infection inhibited viral replication more strongly (≥50% suppression). The cutoff point calculated by using the Student t test for a risk α = 0.025 based on the percentage inhibition displayed by noninfected macaques was 55%, close to the 50% cutoff generally used in studies of this type (40). Some supernatants of CD8+ cells collected before infection even increased virus production.
FIG. 1.
Suppression of SIVmac replication by supernatant fluids of CD8+ lymphocytes isolated from 18 macaques before infection and 2 months after infection with SIVmac251. The data are represented as a box plot in which the top and bottom of the boxes correspond to the 75th and 25th percentiles, respectively; the horizontal line within the box is the median of the population, and the upper and lower error bars are the 90th and 10th percentiles, respectively; individual values outside the 90th and 10th percentiles are individually plotted as circles. Negative values indicate enhanced viral replication. All CD8+ cell supernatants were tested at a dilution of 1:5 in a CD4+ T-cell acute infection assay. The inhibition of viral replication obtained with the supernatants of CD8+ cells isolated after infection is compared to that obtained with the supernatants of CD8+ cells isolated before infection, using the Wilcoxon rank test.
This assay can therefore be used to assess noncytolytic antiviral activity during SIV infection but may be influenced by the presence of multiple components in the supernatants, since both suppression and enhancement of virus production was detected.
CD8+ cell-secreted soluble factor-mediated inhibition of virus replication is noncytolytic and is not MHC restricted.
We then tried to elucidate the mechanisms underlying the observed antiviral response. The inhibition, by CD8+ cell supernatants, of SIV production in vitro was dose dependent, as shown in Fig. 2A. The 50% inhibitory concentration was reached at a dilution of almost 1:10.
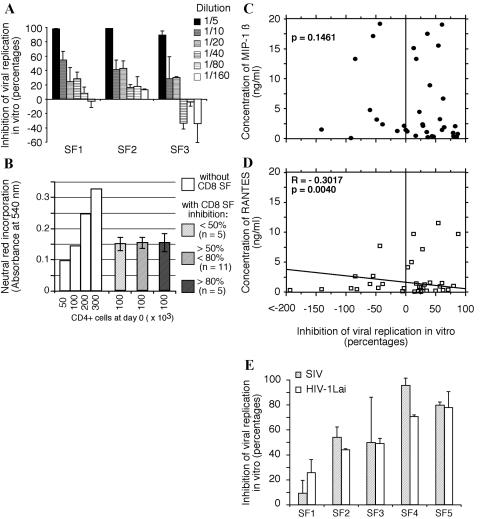
FIG. 2.
Characterization of soluble factor-mediated CD8+ lymphocyte antiviral activity. (A) Dose dependence of the suppression of SIVmac replication in vitro. Titrations of three supernatant fluids giving more than 80% suppression when tested at a dilution of 1:5 are shown. (B) Impact of CD8+ cell supernatants on the viability of activated CD4+ T cells, as measured by neutral red staining. Staining was performed after 3 days in culture, on 100,000 activated CD4+ T cells in the presence of a 1:5 dilution of CD8+ cell supernatant fluid. Mean absorbance values at 540 nm are shown for the neutral red staining of cultures incubated in the presence of a 1:5 dilution of supernatants displaying various degrees of inhibition and were collected from 7 to 35 days after infection. As a control, 50,000, 100,000, 200,000, or 300,000 cells were cultured without CD8+ cell supernatants. (C) Spearman's rank correlation analysis of the possible relationship between CD8 antiviral activity and MIP-1β concentration. (D) Spearman's rank correlation analysis of the possible relationship between CD8 antiviral activity and RANTES concentration. (E) The inhibition of HIV-1Lai and SIVmac251replication is compared for 5 CD8+ supernatants, with percent inhibition given for tests at a dilution of 1:5 against SIVmac251. HIV-1Lai replication was resistant to MIP-1α, MIP-β, or RANTES alone or in association.
We also investigated the effect of a series of inhibitory supernatants on the viability of CD4+ T cells. No significant difference in neutral red staining was observed between cells cultured with supernatants displaying various degrees of inhibition of HIV replication (Fig. 2B), confirming that antiviral activity was not dependent on changes in target cell viability.
Trypan blue dye exclusion assay confirmed that CD4+ T-cell growth was not significantly affected by inhibitory supernatants (data not shown) and that no major cytolytic effect occurred.
Thus, the antiviral activity of CD8+ cells measured in the present study is mediated by soluble factors via noncytotoxic mechanisms and, since the target cells used to support virus replication are xenogeneic human CD4+ T cells, this inhibition was clearly not MHC restricted.
Antiviral activity is not related to β-chemokines, α-defensins, or IL-16.
MIP-1α was undetectable in most supernatants, but low concentrations (<904 pg/ml) were detected in some (data not shown). Concentrations of RANTES and MIP-1β were higher in some CD8+ cell supernatants, but the concentration of MIP-1β was not correlated to the inhibition of viral replication in vitro (Fig. 2C). RANTES concentration was negatively correlated with levels of antiviral activity (Fig. 2D). These β-chemokines were therefore not involved in the observed inhibition of viral replication.
The inhibition of HIV-1 Lai and SIVmac251 replication was compared for supernatants available in sufficiently large quantities. Replication was inhibited to a similar extent for HIV-1 Lai and SIVmac (Fig. 2E), confirming that CD8+-cell-associated antiviral activity is not mediated by β-chemokines, since the HIV-1 Lai virus stock used was resistant to inhibition by recombinant RANTES, MIP-1-α, and MIP-1-β, alone and in association (data not shown).
We also tried to detect α-defensins in 24 supernatants displaying strong inhibition in vitro (suppression >50%). We detected no α-defensins (sensitivity of the assay 50 pg/ml) in any of the CD8+ cell supernatant fluids tested (data not shown), suggesting that these antiviral factors (70) are not involved in the observed inhibition of viral replication.
IL-16 concentrations were also measured in 26 supernatants displaying <50% inhibition and in 17 supernatants displaying >50% inhibition. Concentrations of IL-16 were low (43 ± 81 pg/ml, from undetectable to 300 pg/ml), not correlated with antiviral activity, and far below the concentrations previously reported to inhibit HIV replication in vitro (41).
Longitudinal follow-up of CD4+ cell counts and PVLs.
Eight cynomolgus macaques were exposed to 50 AID50 of SIVmac251 produced in macaques after intravenous inoculation and were monitored for 15 months. As expected in this model (6), various progression profiles were observed when we monitored CD4+ T-cell counts and PVL over time (Fig. 3). The eight macaques were assigned to three groups according to progression profile.
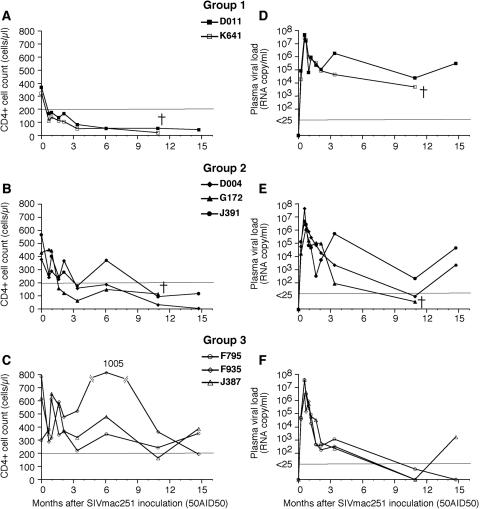
FIG. 3.
Changes in CD4+ T-cell counts (A, B, and C) and PVLs (D, E, and F) with time after infection. Animals are displayed according to their progression profiles: rapid decrease in CD4+ T-cell counts (group 1, A and D), maintenance of normal or subnormal CD4+ T-cell counts (group 3, C and F), and intermediate profiles (group 2, B and E). †, Death of the animal.
Macaques D011 and K641 (group 1) progressed rapidly, showing a marked, rapid decrease in CD4+ T-cell counts within the first month of infection, with no return to baseline (Fig. 3A), and little or no control of PVL (Fig. 3D). Macaque K641 died on day 348. Macaques D004, G172, and J391 (group 2) showed a slower decline in CD4+ T-cell counts (Fig. 3B), as confirmed by ANOVA on data collected within the first 6 months (P = 0.02). These macaques showed partial control of PVL (Fig. 3E), which fell to undetectable levels in one case (G172). Macaque G172 died on day 335 of infection; this animal had low CD4+ T-cell counts despite the lack of detectable virus in the plasma (discordant animal). In contrast, macaques F795, F935, and J387 (group 3) showed little or no decrease in CD4+ T-cell counts (Fig. 3C). PVL control was significantly better in group 3 than in group 1 (ANOVA, P = 0.0002) or group 2 (ANOVA, P = 0.02), with the virus becoming undetectable over time (Fig. 3F).
CD4+ T-cell counts were inversely correlated with PVL (Spearman's rank correlation test, P = 0.0337) after viral set point if the discordant animal G172 was excluded, and cellular viral loads in PBMC were correlated with PVL (Spearman's correlation test, P < 0.0001) (data not shown).
Longitudinal follow-up of soluble factor-mediated CD8+ cell antiviral activity.
The soluble-factor-mediated antiviral activity was monitored over time in these macaques, starting before infection and continuing until 15 months after exposure to SIV. CD8+ cells at baseline showed little or no antiviral activity in vitro (suppression of <50%), a finding consistent with observations for uninfected rhesus macaques in a similar assay (1), and a larger cohort of cynomolgus macaques (Fig. 1). Remarkably, the supernatants of CD8+ cells from three animals (D004, J391, and K641) reproducibly increased virus production at baseline.
Changes in CD8+ cell antiviral activity were then monitored after exposure to SIVmac251, and the results were analyzed in two different ways. We first plotted percentage inhibition over time (calculated as described in Materials and Methods). Since both stimulatory and inhibitory activities were observed before infection, and this feature was reproducible, we hypothesized that increases in the secretion of soluble antiviral factors after infection may compensate for preexisting stimulatory capacities. We therefore also expressed changes in antiviral activity by calculating the net deviation of antiviral activity from baseline values, as previously described (1), to reflect changes in this balance after infection and to take preinfection data for each animal into account more accurately. Statistical analysis was performed for each data set separately.
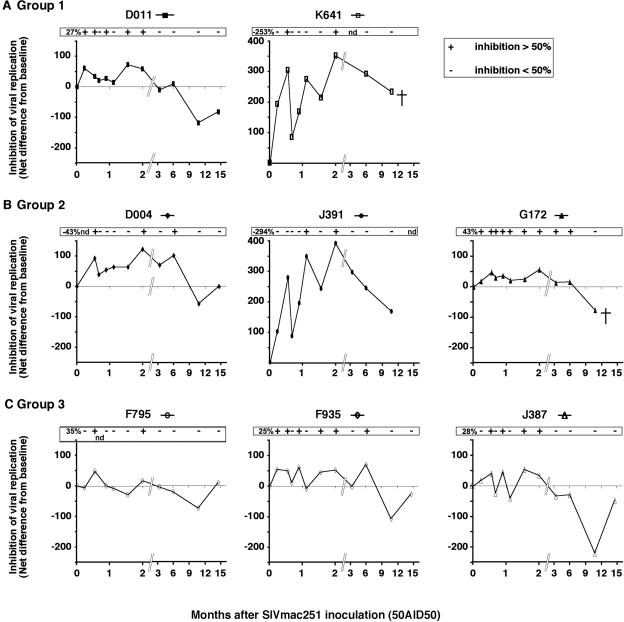
Although the percent inhibition at baseline differed considerably between monkeys, the antiviral activity of CD8+ cells increased within a week of exposure to the virus in all seven macaques tested (Fig. 4) (Wilcoxon rank test, P < 0.001). Macaques displaying enhancement of virus production before infection showed much weaker enhancement, or even inhibition, after infection. By 2 weeks after exposure, the antiviral activity of CD8+ cells exceeded 50% inhibition of replication in seven of the eight animals (mean 58% ± 32%, Fig. 4).
FIG. 4.
Changes in soluble factor-mediated CD8+ cell-derived antiviral activity with time after infection. The ability of CD8+ supernatants at a 1:5 dilution to inhibit SIVmac replication in CD4+ T cells was tested. Differences in the level of inhibition from baseline (net difference from baseline) were calculated by subtracting the percent suppression measured at baseline from the percent suppression measured at each time point and are shown separately for each macaque of group 1 (A), group 2 (B), and group 3 (C). At the top of each graph, at each time point, a “+” is marked if viral replication was inhibited by ≥50% and a “−” indicates the percent suppression was <50%. †, Death of the animal.
Correlation of CAF with biological markers of progression.
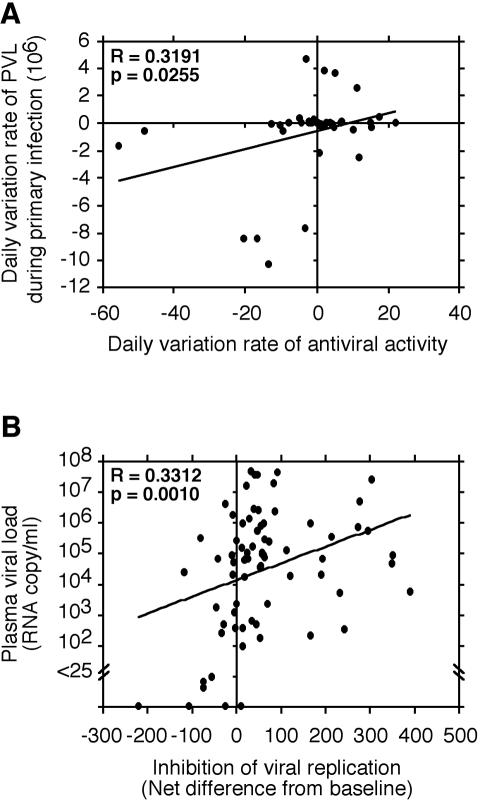
During the first month of infection, the daily rate of increase in the antiviral capacity of CD8+ cells was correlated with the daily rate of increase in PVL (Spearman's rank correlation test, P = 0.0255) (Fig. 5A).
FIG. 5.
Spearman's rank correlation analysis of the relationship between the soluble factor-mediated antiviral activity of CD8+ cells and PVL. (A) Spearman's rank correlation analysis of the relationship between daily variation of PVL and daily variation of antiviral activity during primary infection (day 0 to day 69). (B) Spearman's rank correlation analysis of the relationship between the net difference from baseline of the soluble factor-mediated antiviral activity of CD8+ cells during infection and PVL (day 7 to day 441). The P and r values are given in the top left corner of each graph.
The percent inhibition of viral replication by CD8+ cell supernatants was not correlated with PVL, but the net increase in antiviral activity from baseline was (Fig. 5B) (Spearman's rank correlation test, P = 0.0018).
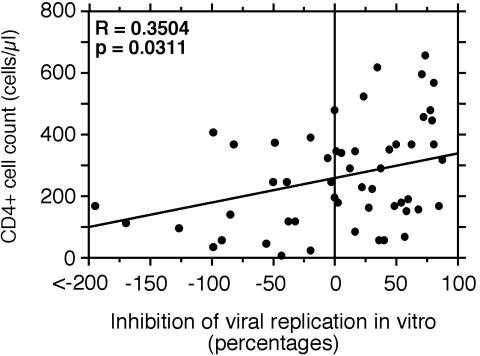
Indeed, the level of inhibition of viral replication achieved with the supernatants of CD8+ cells isolated after viral set point was positively correlated with peripheral blood CD4+ T-cell count (Fig. 6) (Spearman's rank correlation test, P = 0.0311).
FIG. 6.
Spearman's rank correlation analysis of the relationship between the soluble factor-mediated antiviral activity of CD8+ cells (inhibition of SIVmac replication provided by a 1:5 dilution of CD8+ cell supernatants) and peripheral blood CD4+ T-cell counts after viral set point. The P and r values are given in the top left corner of each graph.
After the early phase of infection, the antiviral activity of CD8+ cell supernatants was lost over time in all macaques (Fig. 4), with most supernatants from CD8+ cells isolated late in the follow-up period (days 327 and 441) eventually increasing virus production. This also applied to K641 and J391, which had lower enhancing capacities than at baseline, accounting for the maintenance of a positive net difference in inhibition from baseline.
We therefore concluded that increases in the potential of CD8+ cells to secrete antiviral factor(s) are driven in vivo by levels of virus production but that the maintenance of this reservoir depends on both the persistence of viral load and CD4+ T-cell count. This may account for the decrease in antiviral activity with disease progression in the macaques of groups 1 and 2, and the decrease in antiviral activity after the decrease in viral load to undetectable levels in the macaques of group 3.
Although G172 might appear to contradict this hypothesis because of a sustained antiviral activity despite of low viral load and rapid CD4+ decline (Fig. 3), this macaque displayed the highest percentage suppression at baseline (43% inhibition), which suggests a natural tendency to develop antiviral activity independently of its infection status and CD4+ T cells. This may have allowed him to maintain further antiviral activity above 50% suppression (Fig. 4B).
Correlation of CAF with CD8+ proliferative response.
The antiviral activity of CD8+ cells (percentage inhibition of replication) was correlated with CD8+ cell growth in response to concanavalin A in vitro (data not shown; Spearman's rank correlation test, P = 0.001), whereas the net increase in antiviral activity was not. This may indicate that cell growth is required for the optimal secretion of suppressive factors or that the concentration of these factors increases because faster growth results in the production of larger numbers of secreting CD8+ cells at the end of a 3-day culture period. However, CD8+ cell growth was not correlated with CD4+ T-cell counts, which suggests that the ability of CD8+ cells to grow in culture did not change significantly with progression, at least during the 15-month period of follow-up.
DISCUSSION
The longitudinal follow-up of eight cynomolgus macaques over a period of 15 months after SIVmac251 infection indicated that antiviral activity of CD8+ cells increases within 2 weeks of exposure, as has been described during HIV-1 primary infection in humans (44), and SIV primary infection in Indian rhesus macaques (69). Noncytolytic antiviral activity is then sustained during primary infection and gradually lost over time. CD8+ cells even went on to enhance viral replication at later time points. The observed antiviral activity was not cytolytic, not MHC restricted, soluble factor mediated, and not linked to β-chemokines (RANTES, MIP-1α, and MIP-1β), IL-16, or α-defensins. This antiviral activity therefore resembles that of human CAF (21, 63).
The daily rate of increase in CD8+-cell-associated antiviral activity was positively correlated with the daily rate of increase in PVL during the first 2 months of infection, and the net increase in antiviral activity was correlated with PVL throughout the 15 months of observation. Conversely, the net increase of antiviral activity from baseline was not correlated with blood CD4+ T-cell counts, although the level of antiviral activity was.
Although the rapid increase in antiviral activity after SIVmac infection is consistent with a role in viral inhibition in vivo, no inverse relationship was found between CD8+ antiviral activity and PVL, in contrast to what was observed in three HIV-1 patients during primary infection (44). Differences between our results and those of Mackewitz et al. may be due to differences between assays or differences in the nature of antiviral activity during HIV and SIV infections or may reflect limitations of the analysis due to small sample size.
Nevertheless, our results suggest that CAF activity may not play a major role in the control of virus load and in ultimate clinical outcome, although this activity may synergize with other antiviral responses showing a trend toward inverse correlation with viral load in this species (53).
In the present study, CD8+ cells isolated 12 to 15 months after infection had no significant antiviral activity, regardless of the level of natural control of viral load. This is consistent with the findings of Landay et al. (31) that the decrease in noncytolytic antiviral activity is associated with a major decrease in blood CD4+ T-cell count and with other cross-sectional studies, suggesting that CD8+-cell-associated noncytolytic antiviral activity is associated with better clinical status (10, 23, 43). In our study, although the antiviral activity of CD8+ cells isolated after viral set point was correlated with CD4+ T-cell counts, a decrease in antiviral activity over time was also observed in macaques that did not show progression to low CD4+ T-cell counts and controlled their PVLs efficiently. Consistent with this observation, a strong noncytolytic antiviral activity is generally associated with high CD4+ T-cell counts in HIV-positive asymptomatic individuals, except in some patients with exceptionally high CD4+ cell counts and undetectable viral loads, who have a poor antiviral response (10). Furthermore, although strong CD8+ cell-associated noncytolytic antiviral activity are generally detected in HIV-1-infected LTNP (43, 56), some HIV-1-infected LTNP with low viral loads and stable CD4+ T-cell counts also have weak CD8+ cell-mediated immune activity (18, 22). We therefore suggest that the increase in noncytolytic antiviral activity depends on viral load and that both preserved CD4+ T-cell counts and a viral load exceeding a certain threshold are required to sustain antiviral activity over time.
In our study, the secretion of antiviral factor(s) by CD8+ cells correlated with CD8+ cell growth in vitro but CD8+ cell growth was not correlated with CD4+ T-cell counts, and no difference in CD8+ cell growth was observed between groups. This suggests that the ability of CD8+ cells to grow in culture did not change significantly with progression, at least during the 15 months of follow-up. However, we cannot exclude the possibility that the proliferative capacity of CD8+ cells is associated with CD4+ T-cell proliferation, which was not evaluated in the present study. The potential relevance of CD4+ cells may therefore reflect the importance of IL-2 in maintaining the pool of CD8+ cells responsible for antiviral activity, as previously suggested (3, 30). The accumulation of unresponsive T cells known to occur in the blood of SIV-infected macaques (47, 61) may also have contributed to the observed decrease in CAF over time.
Low CD8+ cell antiviral activity has occasionally been reported in uninfected individuals (25, 36, 55), such as the uninfected macaques in the present study, and CAF activity has also been detected in the supernatants of a CTL line specific for Epstein-Barr virus (32). This suggests that the effector phase of HIV replication control by CAF in vitro does not depend on the recognition of HIV-specific determinants. Nevertheless, the increase in the potential of CD8+ cells to secrete antiviral factors in SIV-infected macaques may involve antigen-specific mechanisms. Although the soluble antiviral response observed in the present study was noncytolytic and not MHC restricted, antiviral factors may be secreted by SIV-specific CD8+ T cells, the populations of which are known to expand in vitro after mitogen stimulation and culture with recombinant IL-2 (49, 64, 65). Alternatively, the pool of CD8+ cells able to secrete soluble antiviral factors may be activated and/or expanded through non-antigen-specific mechanisms closely related to infection (e.g., inflammation, bystander immune activation), which should be further explored.
Some CD8+ cell supernatants from uninfected or infected macaques increased SIV replication in vitro, as was previously reported for HIV-2-infected baboons and HIV-1-infected patients in studies using coculture to assess antiviral activity (8). This activity seems to have a poor prognostic value, since all of the macaques displayed CD8+ cell-mediated replication-enhancing capacities 1 year after infection and since slow progressors in group 3 did not present such activity before infection. Although the pathogenic implications of this activity remain unclear, the prevention of this adverse immune response may prolong the asymptomatic course of infection, as suggested by Blackbourn et al. (8).
Although the mechanism by which CD8+ cells increase HIV-1 replication in CD4+ T cells is unknown, a recent report suggested that contact-dependent inhibition may conceal the enhancement of viral replication at the level of transcription in macrophages (15). This may explain why enhancement of viral replication by CD8+ cells was rarely reported (8), since most studies have assessed antiviral activity in coculture assays.
In conclusion, the present study provides evidence for a rapid increase in soluble factor-mediated CD8+ cell antiviral activity in cynomolgus macaques after SIV infection. This secretion then gradually declines over time and correlated with CD4+ cell counts, suggesting that the triggering of noncytolytic antiviral activity is dependent on viral load and that preserved CD4+ T-cell counts and a viral load exceeding a certain threshold are both required to sustain it over time. Although the role of this antiviral activity in controlling virus replication in vivo remains uncertain, these findings suggest that therapeutic vaccination in combination with highly active antiretroviral therapy might help to increase soluble factor-mediated antiviral immunity in HIV-infected individuals once viral load has been reduced to undetectable levels.
Acknowledgments
This study was supported by the Agence Nationale de Recherche sur le SIDA et les Hépatites Virales (ANRS, Paris, France) and the Commissariat à l'Energie Atomique (CEA, Paris France). V.D. received a scholarship grant from the Ministère délégué à la Recherche et la Technologie (MRT, Paris, France), and K.B.-C. received a CIFRE grant allocated by the ANRT and GlaxoSmithKline Laboratories (Marly le Roi, France).
We thank Yves Rivière (Institut Pasteur, Paris, France) for helpful discussions and constructive comments on the manuscript and are grateful to D. Renault, P. Pochard, and J. C. Wilk for animal care.
Footnotes
This paper is dedicated to the memory of Dominique Dormont.
REFERENCES
- 1.Aubertin, A. M., R. Le Grand, Y. Wang, C. Beyer, L. Tao, O. Neildez, F. Barre-Sinoussi, B. Hurtrel, C. Moog, T. Lehner, and M. Girard. 2000. Generation of CD8+ T cell-generated suppressor factor and beta-chemokines by targeted iliac lymph node immunization in rhesus monkeys challenged with SHIV-89.6P by the rectal route. AIDS Res. Hum. Retrovir. 16:381-392. [DOI] [PubMed] [Google Scholar]
- 2.Barker, E., K. N. Bossart, and J. A. Levy. 1998. Primary CD8+ cells from HIV-infected individuals can suppress productive infection of macrophages independent of beta-chemokines. Proc. Natl. Acad. Sci. USA 95:1725-1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barker, E., C. E. Mackewicz, and J. A. Levy. 1995. Effects of TH1 and TH2 cytokines on CD8+ cell response against human immunodeficiency virus: implications for long-term survival. Proc. Natl. Acad. Sci. USA 92:11135-11139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barker, E., C. E. Mackewicz, G. Reyes-Teran, A. Sato, S. A. Stranford, S. H. Fujimura, C. Christopherson, S. Y. Chang, and J. A. Levy. 1998. Virological and immunological features of long-term human immunodeficiency virus-infected individuals who have remained asymptomatic compared with those who have progressed to acquired immunodeficiency syndrome. Blood 92:3105-3114. [PubMed] [Google Scholar]
- 5.Benito, J. M., M. Lopez, and V. Soriano. 2004. The role of CD8+ T-cell response in HIV infection. AIDS Rev. 6:79-88. [PubMed] [Google Scholar]
- 6.Benlhassan-Chahour, K., C. Penit, V. Dioszeghy, F. Vasseur, G. Janvier, Y. Riviere, N. Dereuddre-Bosquet, D. Dormont, R. Le Grand, and B. Vaslin. 2003. Kinetics of lymphocyte proliferation during primary immune response in macaques infected with pathogenic simian immunodeficiency virus SIVmac251: preliminary report of the effect of early antiviral therapy. J. Virol. 77:12479-12493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blackbourn, D. J., L. F. Chuang, K. F. Killam, Jr., and R. Y. Chuang. 1994. Inhibition of simian immunodeficiency virus (SIV) replication by CD8+ cells of SIV-infected rhesus macaques: implications for immunopathogenesis. J. Med. Primatol 23:343-354. [DOI] [PubMed] [Google Scholar]
- 8.Blackbourn, D. J., C. P. Locher, B. Ramachandran, S. W. Barnett, K. K. Murthy, K. D. Carey, K. M. Brasky, and J. A. Levy. 1997. CD8+ cells from HIV-2-infected baboons control HIV replication. AIDS 11:737-746. [DOI] [PubMed] [Google Scholar]
- 9.Brinchmann, J. E., G. Gaudernack, and F. Vartdal. 1990. CD8+ T cells inhibit HIV replication in naturally infected CD4+ T cells. Evidence for a soluble inhibitor. J. Immunol. 144:2961-2966. [PubMed] [Google Scholar]
- 10.Castelli, J. C., S. G. Deeks, S. Shiboski, and J. A. Levy. 2002. Relationship of CD8+ T cell noncytotoxic anti-HIV response to CD4+ T cell number in untreated asymptomatic HIV-infected individuals. Blood 99:4225-4227. [DOI] [PubMed] [Google Scholar]
- 11.Castro, B. A., J. Homsy, E. Lennette, K. K. Murthy, J. W. Eichberg, and J. A. Levy. 1992. HIV-1 expression in chimpanzees can be activated by CD8+ cell depletion or CMV infection. Clin. Immunol. Immunopathol. 65:227-233. [DOI] [PubMed] [Google Scholar]
- 12.Castro, B. A., C. M. Walker, J. W. Eichberg, and J. A. Levy. 1991. Suppression of human immunodeficiency virus replication by CD8+ cells from infected and uninfected chimpanzees. Cell. Immunol. 132:246-255. [DOI] [PubMed] [Google Scholar]
- 13.Chen, C. H., K. J. Weinhold, J. A. Bartlett, D. P. Bolognesi, and M. L. Greenberg. 1993. CD8+ T lymphocyte-mediated inhibition of HIV-1 long terminal repeat transcription: a novel antiviral mechanism. AIDS Res. Hum. Retrovir. 9:1079-1086. [DOI] [PubMed] [Google Scholar]
- 14.Cocchi, F., A. L. DeVico, A. Garzino-Demo, S. K. Arya, R. C. Gallo, and P. Lusso. 1995. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science 270:1811-1815. [DOI] [PubMed] [Google Scholar]
- 15.Copeland, K. F., P. J. McKay, J. J. Newton, and K. L. Rosenthal. 1998. Enhancement of HIV-1 replication in human macrophages is induced by CD8+ T-cell soluble factors. Clin. Exp. Immunol. 114:87-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Copeland, K. F., P. J. McKay, and K. L. Rosenthal. 1995. Suppression of activation of the human immunodeficiency virus long terminal repeat by CD8+ T cells is not lentivirus specific. AIDS Res. Hum. Retrovir. 11:1321-1326. [DOI] [PubMed] [Google Scholar]
- 17.Ekstrand, D. H., R. J. Awad, C. F. Kallander, and J. S. Gronowitz. 1996. A sensitive assay for the quantification of reverse transcriptase activity based on the use of carrier-bound template and non-radioactive-product detection, with special reference to human-immunodeficiency-virus isolation. Biotechnol. Appl. Biochem. 23(Pt. 2):95-105. [PubMed] [Google Scholar]
- 18.Ferbas, J., A. H. Kaplan, M. A. Hausner, L. E. Hultin, J. L. Matud, Z. Liu, D. L. Panicali, H. Nerng-Ho, R. Detels, and J. V. Giorgi. 1995. Virus burden in long-term survivors of human immunodeficiency virus (HIV) infection is a determinant of anti-HIV CD8+ lymphocyte activity. J. Infect. Dis. 172:329-339. [DOI] [PubMed] [Google Scholar]
- 19.Franchini, G., J. Nacsa, Z. Hel, and E. Tryniszewska. 2002. Immune intervention strategies for HIV-1 infection of humans in the SIV macaque model. Vaccine 20(Suppl. 4):A52-A60. [DOI] [PubMed] [Google Scholar]
- 20.Gauduin, M. C., R. L. Glickman, R. Means, and R. P. Johnson. 1998. Inhibition of simian immunodeficiency virus (SIV) replication by CD8+ T lymphocytes from macaques immunized with live attenuated SIV. J. Virol. 72:6315-6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Geiben-Lynn, R., M. Kursar, N. V. Brown, E. L. Kerr, A. D. Luster, and B. D. Walker. 2001. Noncytolytic inhibition of X4 virus by bulk CD8+ cells from human immunodeficiency virus type 1 (HIV-1)-infected persons and HIV-1-specific cytotoxic T lymphocytes is not mediated by beta-chemokines. J. Virol. 75:8306-8316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geretti, A. M., E. G. Hulskotte, M. E. Dings, C. A. van Baalen, G. van Amerongen, S. G. Norley, P. Boers, R. Gruters, and A. D. Osterhaus. 1999. Decline of simian immunodeficiency virus (SIV)-specific cytotoxic T lymphocytes in the peripheral blood of long-term nonprogressing macaques infected with SIVmac32H-J5. J. Infect. Dis. 180:1133-1141. [DOI] [PubMed] [Google Scholar]
- 23.Gomez, A. M., F. M. Smaill, and K. L. Rosenthal. 1994. Inhibition of HIV replication by CD8+ T cells correlates with CD4 counts and clinical stage of disease. Clin. Exp. Immunol. 97:68-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gulzar, N., and K. F. Copeland. 2004. CD8+ T cells: function and response to HIV infection. Curr. HIV Res. 2:23-37. [DOI] [PubMed] [Google Scholar]
- 25.Hsueh, F. W., C. M. Walker, D. J. Blackbourn, and J. A. Levy. 1994. Suppression of HIV replication by CD8+ cell clones derived from HIV-infected and uninfected individuals. Cell. Immunol. 159:271-279. [DOI] [PubMed] [Google Scholar]
- 26.Hu, D. J., S. Vanichseni, T. D. Mastro, S. Raktham, N. L. Young, P. A. Mock, S. Subbarao, B. S. Parekh, L. Srisuwanvilai, R. Sutthent, C. Wasi, W. Heneine, and K. Choopanya. 2001. Viral load differences in early infection with two HIV-1 subtypes. AIDS 15:683-691. [DOI] [PubMed] [Google Scholar]
- 27.Hubert, J. B., M. Burgard, E. Dussaix, C. Tamalet, C. Deveau, J. Le Chenadec, M. L. Chaix, E. Marchadier, J. L. Vilde, J. F. Delfraissy, L. Meyer, C. Rouzioux, et al. 2000. Natural history of serum HIV-1 RNA levels in 330 patients with a known date of infection. AIDS 14:123-131. [DOI] [PubMed] [Google Scholar]
- 28.Jin, X., D. E. Bauer, S. E. Tuttleton, S. Lewin, A. Gettie, J. Blanchard, C. E. Irwin, J. T. Safrit, J. Mittler, L. Weinberger, L. G. Kostrikis, L. Zhang, A. S. Perelson, and D. D. Ho. 1999. Dramatic rise in plasma viremia after CD8+ T cell depletion in simian immunodeficiency virus-infected macaques. J. Exp. Med. 189:991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kannagi, M., L. V. Chalifoux, C. I. Lord, and N. L. Letvin. 1988. Suppression of simian immunodeficiency virus replication in vitro by CD8+ lymphocytes. J. Immunol. 140:2237-2242. [PubMed] [Google Scholar]
- 30.Kinter, A. L., S. M. Bende, E. C. Hardy, R. Jackson, and A. S. Fauci. 1995. Interleukin 2 induces CD8+ T cell-mediated suppression of human immunodeficiency virus replication in CD4+ T cells and this effect overrides its ability to stimulate virus expression. Proc. Natl. Acad. Sci. USA 92:10985-10989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landay, A. L., C. E. Mackewicz, and J. A. Levy. 1993. An activated CD8+ T cell phenotype correlates with anti-HIV activity and asymptomatic clinical status. Clin. Immunol. Immunopathol. 69:106-116. [DOI] [PubMed] [Google Scholar]
- 32.Le Borgne, S., M. Fevrier, C. Callebaut, S. P. Lee, and Y. Riviere. 2000. CD8+ cell antiviral factor activity is not restricted to human immunodeficiency virus (HIV)-specific T cells and can block HIV replication after initiation of reverse transcription. J. Virol. 74:4456-4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Le Grand, R., P. Clayette, O. Noack, B. Vaslin, F. Theodoro, G. Michel, P. Roques, and D. Dormont. 1994. An animal model for antilentiviral therapy: effect of zidovudine on viral load during acute infection after exposure of macaques to simian immunodeficiency virus. AIDS Res. Hum. Retrovir. 10:1279-1287. [DOI] [PubMed] [Google Scholar]
- 34.Leith, J. G., K. F. Copeland, P. J. McKay, D. Bienzle, C. D. Richards, and K. L. Rosenthal. 1999. T cell-derived suppressive activity: evidence of autocrine noncytolytic control of HIV type 1 transcription and replication. AIDS Res. Hum. Retrovir. 15:1553-1561. [DOI] [PubMed] [Google Scholar]
- 35.Levy, J. A. 2003. The search for the CD8+ cell anti-HIV factor (CAF). Trends Immunol. 24:628-632. [DOI] [PubMed] [Google Scholar]
- 36.Levy, J. A., F. Hsueh, D. J. Blackbourn, D. Wara, and P. S. Weintrub. 1998. CD8 cell noncytotoxic antiviral activity in human immunodeficiency virus-infected and -uninfected children. J. Infect. Dis. 177:470-472. [DOI] [PubMed] [Google Scholar]
- 37.Levy, J. A., C. E. Mackewicz, and E. Barker. 1996. Controlling HIV pathogenesis: the role of the noncytotoxic anti-HIV response of CD8+ T cells. Immunol. Today 17:217-224. [DOI] [PubMed] [Google Scholar]
- 38.Ling, B., R. S. Veazey, C. Penedo, K. Xu, J. D. Lifson, and P. A. Marx. 2002. Longitudinal follow up of SIVmac pathogenesis in rhesus macaques of Chinese origin: emergence of B-cell lymphoma. J. Med. Primatol. 31:154-163. [DOI] [PubMed] [Google Scholar]
- 39.Locher, C. P., D. J. Blackbourn, and J. A. Levy. 1999. Suppression of human immunodeficiency virus type 1 replication by a soluble factor produced by CD8+ lymphocytes from HIV-2-infected baboons. Immunol. Lett. 66:151-157. [DOI] [PubMed] [Google Scholar]
- 40.Mackewicz, C. E., D. J. Blackbourn, and J. A. Levy. 1995. CD8+ T cells suppress human immunodeficiency virus replication by inhibiting viral transcription. Proc. Natl. Acad. Sci. USA 92:2308-2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mackewicz, C. E., J. A. Levy, W. W. Cruikshank, H. Kornfeld, and D. M. Center. 1996. Role of IL-16 in HIV replication. Nature 383:488-489. [DOI] [PubMed] [Google Scholar]
- 42.Mackewicz, C. E., H. Ortega, and J. A. Levy. 1994. Effect of cytokines on HIV replication in CD4+ lymphocytes: lack of identity with the CD8+ cell antiviral factor. Cell. Immunol. 153:329-343. [DOI] [PubMed] [Google Scholar]
- 43.Mackewicz, C. E., H. W. Ortega, and J. A. Levy. 1991. CD8+ cell anti-HIV activity correlates with the clinical state of the infected individual. J. Clin. Investig. 87:1462-1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mackewicz, C. E., L. C. Yang, J. D. Lifson, and J. A. Levy. 1994. Non-cytolytic CD8 T-cell anti-HIV responses in primary HIV-1 infection. Lancet 344:1671-1673. [DOI] [PubMed] [Google Scholar]
- 45.Madec, Y., F. Boufassa, C. Rouzioux, J. F. Delfraissy, and L. Meyer. 2005. Undetectable viremia without antiretroviral therapy in patients with HIV seroconversion: an uncommon phenomenon? Clin. Infect. Dis. 40:1350-1354. [DOI] [PubMed] [Google Scholar]
- 46.Martin, M., N. Serradji, N. Dereuddre-Bosquet, G. Le Pavec, G. Fichet, A. Lamouri, F. Heymans, J. J. Godfroid, P. Clayette, and D. Dormont. 2000. PMS-601, a new platelet-activating factor receptor antagonist that inhibits human immunodeficiency virus replication and potentiates zidovudine activity in macrophages. Antimicrob. Agents Chemother. 44:3150-3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maul, D. H., C. H. Miller, P. A. Marx, M. L. Bleviss, D. L. Madden, R. V. Henrickson, and M. B. Gardner. 1985. Immune defects in simian acquired immunodeficiency syndrome. Vet. Immunol. Immunopathol. 8:201-214. [DOI] [PubMed] [Google Scholar]
- 48.Mederle, I., R. Le Grand, B. Vaslin, E. Badell, B. Vingert, D. Dormont, B. Gicquel, and N. Winter. 2003. Mucosal administration of three recombinant Mycobacterium bovis BCG-SIVmac251 strains to cynomolgus macaques induces rectal IgAs and boosts systemic cellular immune responses that are primed by intradermal vaccination. Vaccine 21:4153-4166. [DOI] [PubMed] [Google Scholar]
- 49.Miller, M. D., C. I. Lord, V. Stallard, G. P. Mazzara, and N. L. Letvin. 1990. The gag-specific cytotoxic T lymphocytes in rhesus monkeys infected with the simian immunodeficiency virus of macaques. J. Immunol. 144:122-128. [PubMed] [Google Scholar]
- 50.Neildez, O., R. Le Grand, A. Cheret, P. Caufour, B. Vaslin, F. Matheux, F. Theodoro, P. Roques, and D. Dormont. 1998. Variation in virological parameters and antibody responses in macaques after a traumatic vaginal exposure to a pathogenic primary isolate of SIVmac251. Res. Virol. 149:53-68. [DOI] [PubMed] [Google Scholar]
- 51.Ondoa, P., L. Kestens, D. Davis, C. Vereecken, B. Willems, K. Fransen, J. Vingerhoets, G. Zissis, P. ten Haaft, J. Heeney, and G. van der Groen. 2001. Longitudinal comparison of virus load parameters and CD8 T-cell suppressive capacity in two SIVcpz-infected chimpanzees. J. Med. Primatol. 30:243-253. [DOI] [PubMed] [Google Scholar]
- 52.Parker, R. A., M. M. Regan, and K. A. Reimann. 2001. Variability of viral load in plasma of rhesus monkeys inoculated with simian immunodeficiency virus or simian-human immunodeficiency virus: implications for using nonhuman primate AIDS models to test vaccines and therapeutics. J. Virol. 75:11234-11238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Reimann, K. A., R. A. Parker, M. S. Seaman, K. Beaudry, M. Beddall, L. Peterson, K. C. Williams, R. S. Veazey, D. C. Montefiori, J. R. Mascola, G. J. Nabel, and N. L. Letvin. 2005. Pathogenicity of simian-human immunodeficiency virus SHIV-89.6P and SIVmac is attenuated in cynomolgus macaques and associated with early T-lymphocyte responses. J. Virol. 79:8878-8885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Richardson, B. A., D. Mbori-Ngacha, L. Lavreys, G. C. John-Stewart, R. Nduati, D. D. Panteleeff, S. Emery, J. K. Kreiss, and J. Overbaugh. 2003. Comparison of human immunodeficiency virus type 1 viral loads in Kenyan women, men, and infants during primary and early infection. J. Virol. 77:7120-7123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosok, B., P. Voltersvik, B. M. Larsson, J. Albert, J. E. Brinchmann, and B. Asjo. 1997. CD8+ T cells from HIV type 1-seronegative individuals suppress virus replication in acutely infected cells. AIDS Res. Hum. Retrovir. 13:79-85. [DOI] [PubMed] [Google Scholar]
- 56.Salerno-Goncalves, R., W. Lu, and J. M. Andrieu. 2000. Quantitative analysis of the antiviral activity of CD8+ T cells from human immunodeficiency virus-positive asymptomatic patients with different rates of CD4+ T-cell decrease. J. Virol. 74:6648-6651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sarr, A. D., G. Eisen, A. Gueye-Ndiaye, C. Mullins, I. Traore, M. C. Dia, J. L. Sankale, D. Faye, S. Mboup, and P. Kanki. 2005. Viral dynamics of primary HIV-1 infection in Senegal, West Africa. J. Infect. Dis. 191:1460-1467. [DOI] [PubMed] [Google Scholar]
- 58.Schmitz, J. E., M. J. Kuroda, S. Santra, V. G. Sasseville, M. A. Simon, M. A. Lifton, P. Racz, K. Tenner-Racz, M. Dalesandro, B. J. Scallon, J. Ghrayeb, M. A. Forman, D. C. Montefiori, E. P. Rieber, N. L. Letvin, and K. A. Reimann. 1999. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283:857-860. [DOI] [PubMed] [Google Scholar]
- 59.Severino, M. E., N. V. Sipsas, P. T. Nguyen, S. A. Kalams, B. D. Walker, R. P. Johnson, and O. O. Yang. 2000. Inhibition of human immunodeficiency virus type 1 replication in primary CD4+ T lymphocytes, monocytes, and dendritic cells by cytotoxic T lymphocytes. J. Virol. 74:6695-6699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sopper, S., E. Koutsilieri, C. Scheller, S. Czub, P. Riederer, and V. ter Meulen. 2002. Macaque animal model for HIV-induced neurological disease. J. Neural Transm. 109:747-766. [DOI] [PubMed] [Google Scholar]
- 61.Spring, M., W. Bodemer, C. Stahl-Hennig, T. Nisslein, G. Hunsmann, and U. Dittmer. 1997. Impaired mitogen-driven proliferation and cytokine transcription of lymphocytes from macaques early after simian immunodeficiency virus (SIV) infection. Viral Immunol. 10:65-72. [DOI] [PubMed] [Google Scholar]
- 62.ten Haaft, P., N. Almond, G. Biberfeld, A. Cafaro, M. Cranage, B. Ensoli, G. Hunsmann, N. Polyanskaya, C. Stahl-Hennig, R. Thortensson, F. Titti, and J. Heeney. 2001. Comparison of early plasma RNA loads in different macaque species and the impact of different routes of exposure on SIV/SHIV infection. J. Med. Primatol. 30:207-214. [DOI] [PubMed] [Google Scholar]
- 63.Tomaras, G. D., S. F. Lacey, C. B. McDanal, G. Ferrari, K. J. Weinhold, and M. L. Greenberg. 2000. CD8+ T cell-mediated suppressive activity inhibits HIV-1 after virus entry with kinetics indicating effects on virus gene expression. Proc. Natl. Acad. Sci. USA 97:3503-3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tsubota, H., C. I. Lord, D. I. Watkins, C. Morimoto, and N. L. Letvin. 1989. A cytotoxic T lymphocyte inhibits acquired immunodeficiency syndrome virus replication in peripheral blood lymphocytes. J. Exp. Med. 169:1421-1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Venet, A., I. Bourgault, A. M. Aubertin, M. P. Kieny, and J. P. Levy. 1992. Cytotoxic T lymphocyte response against multiple simian immunodeficiency virusA (SIV) proteins in SIV-infected macaques. J. Immunol. 148:2899-2908. [PubMed] [Google Scholar]
- 66.Verrier, B., R. Le Grand, Y. Ataman-Onal, C. Terrat, C. Guillon, P. Y. Durand, B. Hurtrel, A. M. Aubertin, G. Sutter, V. Erfle, and M. Girard. 2002. Evaluation in rhesus macaques of Tat and rev-targeted immunization as a preventive vaccine against mucosal challenge with SHIV-BX08. DNA Cell Biol. 21:653-658. [DOI] [PubMed] [Google Scholar]
- 67.Walker, C. M., and J. A. Levy. 1989. A diffusible lymphokine produced by CD8+ T lymphocytes suppresses HIV replication. Immunology 66:628-630. [PMC free article] [PubMed] [Google Scholar]
- 68.Walker, C. M., D. J. Moody, D. P. Stites, and J. A. Levy. 1986. CD8+ lymphocytes can control HIV infection in vitro by suppressing virus replication. Science 234:1563-1566. [DOI] [PubMed] [Google Scholar]
- 69.Yasutomi, Y., K. A. Reimann, C. I. Lord, M. D. Miller, and N. L. Letvin. 1993. Simian immunodeficiency virus-specific CD8+ lymphocyte response in acutely infected rhesus monkeys. J. Virol. 67:1707-1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang, L., W. Yu, T. He, J. Yu, R. E. Caffrey, E. A. Dalmasso, S. Fu, T. Pham, J. Mei, J. J. Ho, W. Zhang, P. Lopez, and D. D. Ho. 2002. Contribution of human α-defensin-1, -2, and -3 to the anti-HIV-1 activity of CD8 antiviral factor. Science 298:995-1000. [DOI] [PubMed] [Google Scholar]