Abstract
Context: Neoprene sleeves are alleged to increase heat in skeletal muscle, but no published research supports this belief.
Objectives: To quantify anterior thigh skin and intramuscular temperature changes in varsity athletes wearing a neoprene thigh sleeve.
Design: A 2 × 2 × 3 × 5 factorial design with replicated measures on 3 variables. Independent variables included sex (male or female), neoprene sleeve (yes or no), exercise intensity (control, 50% intensity bicycle, 70% intensity bicycle), and exercise phase (5 minutes pre-exercise, 15 minutes of exercise, 0–10 minutes postexercise, 11–20 minutes postexercise, 21– 30 minutes postexercise).
Setting: Research laboratory.
Patients or Other Participants: 12 male (23 ± 0.95 years) and 12 female (20.59 ± 1.44 years) National Collegiate Athletic Association Division I collegiate athletes actively engaged in offseason strength and conditioning programs.
Intervention(s): We sampled skin and muscle temperatures every 10 seconds for 50 minutes with a telethermometer interfaced to a personal computer. Each 60-minute session included 15 minutes pre-exercise (temperatures recorded during the last 5 minutes), 15 minutes of exercise (control, 50% intensity, and 70% intensity), and 30 minutes postexercise. Skin temperature was measured on the anterior aspect of the thigh using surface thermocouples. Intramuscular temperature was measured in the vastus lateralis muscle at a depth of 2 cm below the subcutaneous fat using implantable thermocouples.
Main Outcome Measure(s): Skin and intramuscular temperature.
Results: Skin temperature was greater when subjects were wearing neoprene sleeves (1.4°C during control, 3.1°C during 70% exercise). Wearing a thigh sleeve had no effect on intramuscular temperature before or during exercise, but postexercise temperatures averaged 0.5°C higher. Exercise intensity showed 1.3°C to 2.0°C increases in temperature with the sleeve. Females had higher intramuscular temperatures than males when wearing sleeves (1.4°C during control, 1°C during 50% exercise, and 0.8°C during 70% exercise). Males had higher skin temperatures than females (0.8°C during 50% exercise, 1°C during 70% exercise).
Conclusions: Neoprene sleeves are effective in maintaining intramuscular temperature after 15 minutes of exercise and in increasing skin temperature during and after exercise. These results may be attributable to the insulating effects of the neoprene sleeve.
Keywords: heat retention, exercise intensity, prevention, treatment, intramuscular temperature
Athletic trainers treat muscle strains, sprains, and contusions with various modalities to promote healing by increasing tissue temperature. With modality treatments, athletic trainers traditionally recommend wearing neoprene sleeves during activity, based on the reported benefits of neoprene. Neoprene is promoted as an external device that will provide extra warmth for muscles,1 allow tissues to better handle the demands of activity,2 and decrease the likelihood of injury.3,4
Exercise alone causes skin and muscle temperature to increase.4–9 As intramuscular temperatures increase, extensibility of the musculotendinous unit increases, which decreases the likelihood of injury to that structure.4 Heat is dissipated from the body as skin blood flow increases and sweat is evaporated.5 Because evaporation is the body's main cooling system, it seems logical that wearing a neoprene sleeve or another insulating covering prevents evaporation and promotes heat retention.10 Although this conclusion is logical, no research has been published on the effects of neoprene on skin or muscle temperature during exercise. The only articles published describing the effects of neoprene involve proprioception,11–13 insulation when icing,9,14,15 and measures of core body temperature while exercising in full wet suits.16,17
Our purpose was to examine the effects of wearing a neoprene sleeve on skin and intramuscular temperature during exercise to quantify the benefit, if any, from wearing the sleeve. We hypothesized that skin temperature would be significantly higher on the leg wearing the sleeve, but intramuscular temperature would be similar, regardless of the presence of the sleeve. Influences on skin and intramuscular temperature were evaluated by comparing exercise intensities of 50% and 70% of maximum heart rate to a control condition with no exercise. Because of possible differences in adipose tissue, we tested males and females to determine whether responses differ between the sexes. We hypothesized that the greatest temperature changes would occur in the group that exercised at 70% of maximum heart rate. Finally, we investigated the ability of a neoprene sleeve to retain temperature by measuring skin and intramuscular temperature for 30 minutes after exercise. We also hypothesized that heat retention would be significantly greater in the leg wearing the sleeve than in the contralateral bare limb.
METHODS
The experimental design for this study was a 2 × 2 × 3 × 5 factorial with repeated measures on 3 factors. Independent variables included sex (male or female), wearing a sleeve (yes or no), exercise intensity (none, 50% of maximum heart rate, and 70% of maximum heart rate), and phase (5 minutes pre-exercise, 15 minutes of exercise, 0–10 minutes postexercise, 11–20 minutes postexercise, and 21–30 minutes postexercise). Dependent variables were skin temperature and intramuscular temperature. Subjects participated in each of the 3 exercise conditions while wearing a neoprene sleeve on 1 leg, while the opposite leg (without the sleeve) served as a control.
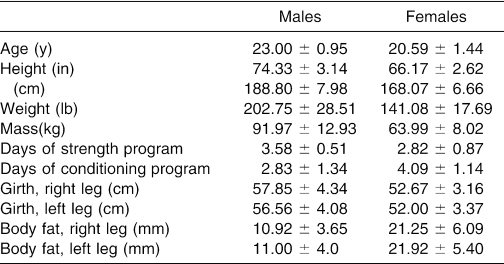
Subjects for this study included 12 male (23 ± 0.95 years) and 12 female (20.59 ± 1.44 years) National Collegiate Athletic Association Division I collegiate athletes who were participating in self-directed, offseason strength and conditioning programs. General information about height, weight, number of days of strength training, and number of days of conditioning was recorded for each subject (Table 1). Girth and skin-fold thickness of both thighs were also measured over the anterior aspect of the thigh.
Table 1. Subject Information.
Six treatment orders were established with 2 balanced Latin squares. Subjects were randomly assigned to 1 of these treatment orders. The leg chosen to wear the sleeve was also selected at random by a drawing out of a hat.
This study was approved by our university institutional review board, and informed consent was obtained. Subjects were tested at the same time of day for each condition with a minimum of 24 to 72 hours' rest between treatment sessions.
Girth measurements were assessed using a standard flexible tape measure. Thigh girth measurements were taken midway between the superior margin of the patella and the anterior superior iliac spine. Skin-fold measurements were taken using skin calipers at the location of the thermocouple insertion.3 The same person measured all skin folds for reliability. A line was drawn from the anterior superior iliac spine to the lateral femoral epicondyle, bisecting the vastus lateralis muscle. An intersecting perpendicular line was drawn one fourth of the distance from the lateral femoral epicondyle to the anterior superior iliac spine. Two skin thermocouples were placed 8 cm and 16 cm above this perpendicular line. One intramuscular thermocouple was placed at the bisection of the 8-cm skin thermocouple and the muscle belly of the vastus lateralis. Skin, air, and intramuscular temperatures were measured using a 16-channel Iso-Thermex telethermometer (Columbus Instruments, Columbus, OH) interfaced with a personal computer. Thermocouples were used to measure skin (model TX21; Columbus Instruments) and muscle (model TX-23-21; Columbus Instruments) temperature.
We used a Polar heart rate monitor (model 1901201; Polar Electro Inc, Lake Success, NY) to quantify heart rate during each exercise bout. Relative target heart rate values of 50% ± 5% of maximum heart rate for mild exercise and 65% ± 5% of maximum heart rate for vigorous exercise were maintained. Maximum heart rate was computed as 220 − age × heart rate percentage.
Subjects wore 0.125-in (0.32-cm) thick neoprene sleeves (DonJoy Inc, Vista, CA). The sleeves were sized small, medium, large, and extra large. They were fitted subjectively based on the subject's comfort, with specific instructions that the sleeve should be snug but not constricting. Sleeves were 9.84 in (24 cm) in length and were pulled up so that the bottom of the sleeve was resting one fourth of the distance from the lateral femoral epicondyle to the anterior superior iliac spine.
A standard bicycle ergometer was used to complete the exercise portion of the treatment. The subject was able to set the workload of the bicycle at a level of comfort that provided enough resistance to maintain the predetermined intensity for that day as described by the heart rate. Seat and handle adjustments were made for subject comfort.
Testing Protocol
On testing days, the test leg was shaved on the anterior portion of the thigh that would be under the sleeve. This area was cleansed with an iodine swab and then with an alcohol pad. Marks were made on the thigh where the bottom of the sleeve would rest and where the thermocouples would be secured. The area for implantation was prepared once measurement depths were calculated. A 32-mm, 20-gauge Teflon catheter (Du Pont, Wilmington, DE) was inserted into the vastus lateralis muscle. Before insertion, the catheter was measured and marked according to the target depth to ensure proper depth implantation. A mark was also placed on the thermocouple 3.15 in (8 cm) above the tip of the thermocouple to provide a way to measure slippage of the thermocouple once it was inserted through the catheter. With the catheter in place, the thermocouple was then inserted and fed through the catheter until the treatment administrator felt a definite end limit. Once the thermocouple was in place, the top lip of the catheter was bent sideways to secure the thermocouple inside the catheter. The catheter lip was then secured to the skin using Dermaclear tape (Johnson & Johnson Medical, Arlington, TX), and the thermocouple was similarly taped to the skin. The 2 skin-temperature thermocouples were placed 3.15 in (8 cm) and 6.30 in (16 cm) above the line for the base of the sleeve. The thermocouples were attached to the skin using Dermaclear tape with the tip of the thermocouple exposed.18 The neoprene sleeve was put on the test limb after the thermocouples were secured.
Temperature samples were obtained every 10 seconds for 50 minutes of the 60-minute experiment, producing a total of 300 samples. Each treatment began with 15 minutes of rest to establish the subjects' baseline temperature. Temperature recordings started in the last 5 minutes of the 15-minute rest. Subjects then either sat motionless on a cycle ergometer (control) or pedaled the bicycle (exercise) for 15 minutes.
During exercise treatments, subjects wore a Polar heart rate monitor to ensure heart rates remained within the calculated values. At the onset of exercise, subjects were instructed to increase their heart rates as quickly as possible to the calculated value and to then maintain that value for the duration of the exercise. Heart rate was checked once a minute during exercise.
The treatment conditions consisted of a control of no exercise and two 15-minute rides on a cycle ergometer, 1 at 50% and 1 at 70% of maximum heart rate. After exercise, subjects sat in a chair with hips and knees flexed to 90° and feet flat on the ground for 30 minutes. The 3 sessions occurred at approximately the same time of day, with 24 to 72 hours between sessions.
Upon completion of each testing session, the thermocouples and catheters were removed, and antibiotic ointment and bandages were applied over the insertion sites. Subjects were instructed on appropriate care and management of the insertion sites. The thermocouples were disinfected by immersion in Cidex 2% glutaraldehyde solution (Johnson & Johnson)19 for 20 minutes and needles disposed of in a biohazard container for sharp objects.
Analysis
We calculated means and standard deviations for both dependent variables (surface temperature and intramuscular temperature) by sleeve, sex, exercise condition, and phase. Two 2 × 2 × 3 × 5 analyses of variance (ANOVAs) with repeated measures on 3 of the factors were computed, 1 for each of the 2 dependent variables. We computed Tukey-Kramer multiple range tests for significant ANOVAs. Significance was set at P = .05.
To decrease the length of the article and increase readability, we summarized the reporting of F statistics as follows: an = sign indicates results from a single ANOVA, and a < or > sign indicates the results of multiple ANOVAs. The number before > is the largest value of the summarized tests and the number before < is the smallest value of the summarized tests.
RESULTS
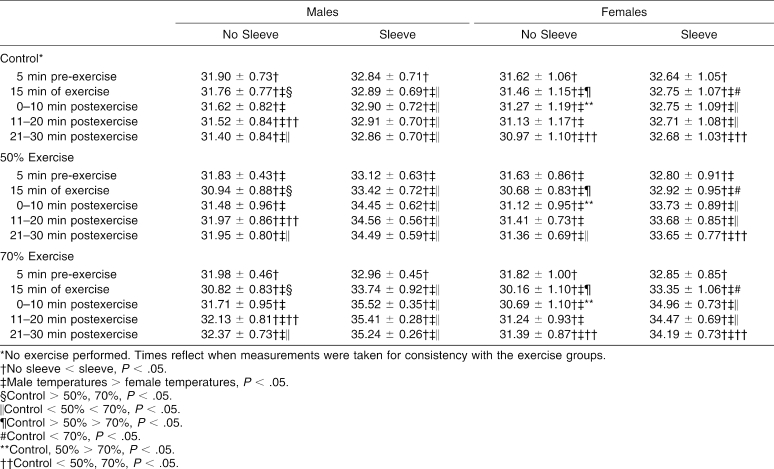
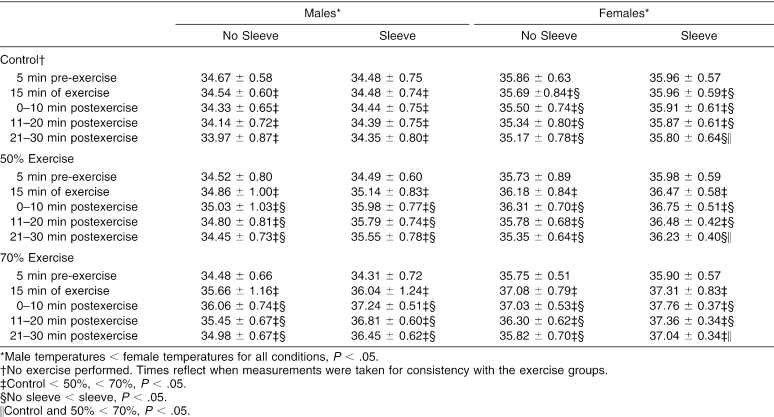
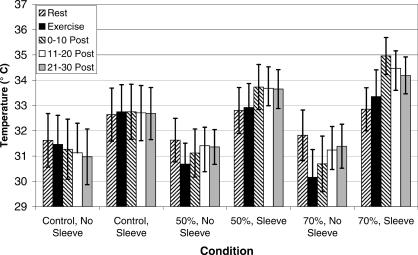
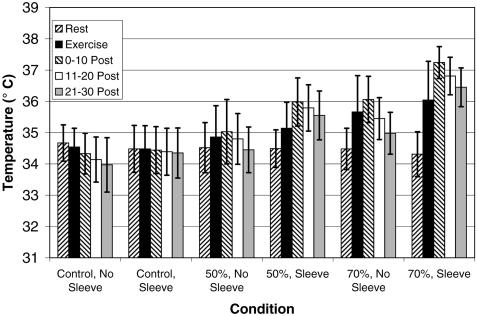
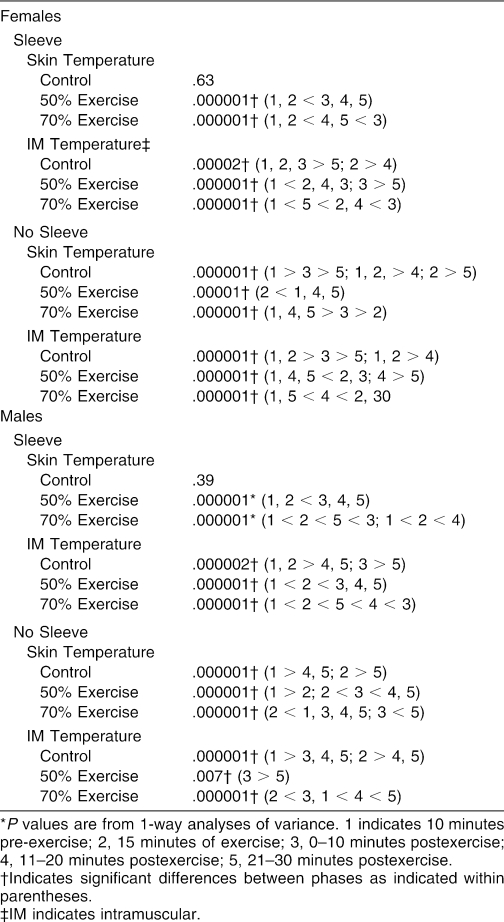
Because of significant interactions and the large number of variables, the results are presented in separate tables for skin (Table 2) and intramuscular (Table 3) temperatures, as well as in Figures 1 and 2.
Table 2. Skin Temperature for Each Condition (°C).
Table 3. Intramuscular Temperature for Each Condition (°C).
Figure 1. Females' skin temperature. 0–10, 11–20, and 21–30 indicate 0 to 10, 11 to 20, and 21 to 30 minutes postexercise, respectively; 50% and 70%, exercise intensity of 50% and 70% of maximum heart rate, respectively.
Figure 2. Males' intramuscular temperature. 0–10, 11–20, and 21– 30 indicate 0 to 10, 11 to 20, and 21 to 30 minutes postexercise, respectively; 50% and 70%, exercise intensity of 50% and 70% of maximum heart rate, respectively.
Two-way and 3-way interactions were significant for factorial ANOVAs (P < .02 for skin temperature, P < .03 for intramuscular temperature), necessitating simple main effects testing, which was done with 1-way ANOVAs.
Effect of Sex
The effect of sex by exercise was significant, so the results are separated by sex. Most skin temperatures were higher for males than for females (see Table 1), and most intramuscular temperatures were higher for females than for males (see Table 2). When wearing sleeves, males had higher skin temperatures than females during all phases of 50% exercise (F1,118 > 5.13, P < .03) and during all phases of 70% exercise except for the 5-minute pre-exercise phase (F1,358 > 14.28, P < .0002). Males' skin temperatures were on average 0.8°C higher during 50% exercise and 1°C higher during 70% exercise compared with control. When not wearing sleeves, males had higher skin temperatures than females under each treatment condition during all phases except for the 5-minute pre-exercise phase (F1,358 > 8.28, P < .004). Without the sleeve, males' skin temperatures were 0.4°C higher during control, 0.5°C higher during 50% exercise, and 0.9°C higher during 70% exercise. Females had higher intramuscular temperatures than males during all phases of each condition (F1,118 > 148.56, P < .000001). Intramuscular temperatures in females averaged 1°C higher during all conditions when not wearing the sleeve. When wearing the sleeve, females' intramuscular temperatures averaged 1.4°C higher during control, 1°C higher during 50% exercise, and 0.8°C higher during 70% exercise.
Effect of Sleeve
As hypothesized, wearing a sleeve resulted in higher skin temperatures during all 3 conditions for both males and females (see Table 2; F1,96 > 18.64, P < .001). Sleeved-limb skin temperatures averaged about 1°C higher during control, 2°C higher during 50% exercise, and 3°C higher during 70% exercise.
Intramuscular temperature responded differently for males and females wearing neoprene sleeves during the control condition (see Table 3). Wearing sleeves resulted in higher intramuscular temperatures for females during all phases of the control condition, except for the 5-minute pre-exercise phase (F1,336 > 5.17, P < .04). No significant differences were noted in males wearing sleeves during control conditions (F1,216 < 2.14, P > .17). Intramuscular temperature averaged about 0.7°C higher when wearing a sleeve during the 50% exercise and about 1°C higher during 70% exercise. During both exercise intensities, wearing sleeves resulted in higher intramuscular temperatures in both males and females during the 3 postexercise measurements (F1,216 > 6.51, P < .03).
Effect of Exercise
As hypothesized, skin and intramuscular temperatures were higher at 70% exercise intensity and usually higher than controls at 50% exercise (see Tables 2 and 3). Skin temperature was higher during 70% exercise intensity than during 50% intensity, which was higher than control skin temperature under both sleeve and no-sleeve conditions during exercise and all 3 postexercise phases (F2,537 > 16.87, P < .00004), except for 0 to 10 minutes postexercise when not wearing the sleeve (F2,324 < 1.91, P > .15).
At 30 minutes postexercise, males' skin temperature was significantly different between 70% exercise (35.24 ± 0.26°C), 50% exercise (34.49 ± 0.59°C), and control (32.86 ± 0.70°C).
During 0 to 10 and 11 to 20 minutes postexercise, wearing the sleeve resulted in significantly higher skin temperatures for females at 70% intensity than at 50%, which was higher than controls (F2,324 > 21.73, P < .000006). From 21 to 30 minutes postexercise, females' skin temperature was higher during 70% exercise than during both 50% intensity and control conditions (F2,324 > 7.88, P < .0004). Skin temperature for the control group was approximately 1.1°C higher during the exercise phase than that for the 70% exercise group (see Table 2).
Intramuscular temperature was higher at 70% exercise intensity than at 50% intensity, which was greater than control during exercise and all 3 postexercise phases in males (F2,537 > 20.21, P < .00001) and during exercise and minutes 0 to 10 and 11 to 20 postexercise in females (F2,537 > 158.9, P < .000001) (see Table 3). Males' intramuscular temperature was at least 0.5°C higher at 70% exercise than at 50% exercise, which was higher by at least 0.5°C than controls. Females' intramuscular temperature was at least 0.7°C higher at 70% exercise than 50%, which was again higher than controls by at least 0.7°C. At 21 to 30 minutes postexercise, females showed higher intramuscular temperatures at 70% intensity than at either 50% or controls (F2,324 > 25.10, P < .000002).
Effect of Phase
Complex interactions were seen between phase (pre-exercise, exercise, 0–10 minutes postexercise, 11–20 minutes postexercise, and 21–30 minutes postexercise) and each of the other variables (Table 4). During the control condition, no differences were noted in skin temperature between phases while wearing a sleeve (F4,540 < 1.05, P > .39). When not wearing a sleeve during the control condition, the pre-exercise and exercise phases resulted in higher skin temperatures than the 3 postexercise phases (F4,540 > 22.20, P < .000001). Skin temperature was generally higher in all 3 postexercise phases during both the 50% and 70% exercise intensities (F4,540 > 53.95, P < .000001).
Table 4. Effect of Phase on Skin and Intramuscular Temperatures by Sex, Sleeve, and Exercise Condition (P Values and Results of Multiple Range Tests)*.
Intramuscular temperature differed significantly among phases in all three exercise conditions. In general, temperature was higher at 0 to 10 minutes postexercise than during the other phases (F4,540 > 4.03, P < .007).
DISCUSSION
Neoprene sleeves appear to prevent tissue cooling rather than enhance tissue heating. Skin temperature depends on 4 things: tissue temperature, local level of sweating, local skin blood flow, and the thermal conductance of underlying tissues.20 As underlying tissues heat up and local blood flow increases, sweat is produced at the skin. Wearing a neoprene sleeve prevents sweat evaporation between the skin and the environment, and therefore skin temperatures remain elevated. Our observations are in agreement with those of Ho and Fan,21 who reported that adding clothing compromises heat exchange between the skin and the environment by influencing the rates of conduction, convection, radiation, and evaporation.
The elevated skin temperature in our subjects is consistent with findings on other types of coverings.21,22 However, the evaporative cooling of the skin during exercise was an outcome not previously documented. Skin temperatures decreased approximately 1°C during exercise in the leg that was not wearing a neoprene sleeve.
Intramuscular temperatures were also affected, but in a different manner than skin temperatures, by the wearing of a neoprene sleeve. As an individual begins to exercise, blood flow to the muscles must increase to meet the demands of increased metabolism.7 Muscle temperatures appeared to be unaffected by the sleeve until after exercise. After the exercise session, intramuscular temperatures in the sleeve condition remained higher than those in the nonsleeve condition. This elevation in intramuscular temperature remained greater for up to 30 minutes after exercise. Of particular interest, in both the 50% and 70% exercise conditions, intramuscular temperatures continued to increase after the exercise phase. This finding is most probably related to cardiac output. During exercise, cardiac output increases because of increases in heart rate and stroke volume4,23 to facilitate increased blood flow to the working muscles and meet the increased metabolic demands.4,5 Most of the increase is caused by heart rate, because stroke volume actually decreases during prolonged submaximal exercise.4,23 Blood flow also cools the tissues as it circulates through them. When exercise stops, however, cardiac output decreases because of a decrease in heart rate, while the metabolic demands of the muscle remain elevated. With this decrease in cardiac output, relative blood flow to the area decreases, reducing blood flow to the muscles. Thus, temperatures continue to increase or remain elevated after exercise.5,10,23,24
Skin and muscle temperatures increased at different rates.10 This is because thermoregulatory control of cutaneous circulation is enhanced during exercise, increasing skin blood flow as internal temperatures increase, and facilitating the body's ability to dissipate heat efficiently.5,6,23
Males had higher skin temperatures, but females had higher intramuscular temperatures. The differences between skin and intramuscular temperature increases may be partially accounted for by sex. Males' skin temperatures were higher than females' because sweating is linearly related to metabolic rates of the body, and the males' metabolism was most likely greater.9 The lower intramuscular temperatures in males, despite their having higher surface temperatures, is most likely a function of less adipose tissue in males and, thus, less insulation (skin-fold measurement was 11 mm for male subjects versus 21 mm for female subjects). Lean people are better able to dissipate heat and, therefore, keep their internal temperatures lower.5,9,23
Exercise intensity also affected changes in skin and intramuscular temperatures. As relative workload increased, sweat production apparently increased, causing changes in skin temperature depending on the sleeve. Legs wearing sleeves had higher skin temperatures after exercise than during exercise. However, bare legs showed a decrease in skin temperature during exercise as compared with controls. This decrease can be explained by sweating, which helps to maintain body temperature through evaporative cooling20 and the shunting of blood from the skin to the exercising muscle to meet the metabolic demands of that muscle.23 Similarly, 70% exercise intensity resulted in the greatest decrease in skin temperature in the leg without the sleeve. This indicates that higher intensities enhance sweat production, producing greater evaporative cooling. The temperature of the working muscle changes according to the relative workload, rather than the absolute amount of work achieved.7,25 This finding was also seen in our study, in which 70% intensity produced the greatest increases in intramuscular temperatures.
Another interesting finding was that temperature changes at 70% exercise without the sleeve mirrored temperature changes at 50% exercise with the sleeve. This suggests that 15 minutes of exercise while wearing a sleeve could be completed at a lower intensity and continue to provide significant temperature increases similar to those seen at higher intensities. Such a protocol would be beneficial for an athlete who is returning from an injury and not yet ready to exercise at 70% intensity.
Of particular concern to athletic trainers is the relationship between muscle temperature and muscle tears and strains. Warm (40°C) rabbit skeletal muscle can sustain greater deformation before failure occurs.3 Rising internal temperatures leads to increased extensibility of the musculotendinous unit, which may decrease injury to this structure.4 Gersten26 explained that to achieve these thermal benefits, tendon temperatures should be raised to between 39°C and 47°C. Typically, therapeutic modalities are used by clinicians to increase intramuscular temperature 3°C to 5°C.27–30 However, these increases are not long lasting.
Wearing neoprene sleeves during active exercise does not provide as great a temperature increase as therapeutic modalities, but the effects are longer lasting because tissue cooling after application is prevented. Maintenance of temperature increase was least effective after 3-MHz ultrasound treatments when temperature dropped 1°C in the first minute after treatment.28 Pulsed short-wave diathermy decreased temperature 0.97°C in 5 minutes after the treatment.27 Our study indicates that intramuscular temperatures remained elevated for at least 30 minutes postexercise when subjects were wearing a neoprene sleeve.
At 30 minutes postexercise, skin and intramuscular temperatures remained approximately 1°C and 2°C higher, respectively, than baseline during both the 50% and 70% exercise intensities with the neoprene sleeve. Intramuscular temperatures in our study reached as high as 37.76°C (a 2°C increase over baseline), which, according to Gersten,26 would not increase extensibility of the tissue. It seems logical, however, that a sustained increase of approximately 2°C would benefit the muscle by allowing more extensibility.2,4
Future Research
A study to build on this research would combine the use of a neoprene sleeve with another modality to see whether temperature changes are enhanced or maintained for even longer periods of time. Another area for further research is to compare different brands of neoprene to see whether manufacturers' differences cause changes in sustained temperatures. It would also be interesting to compare temperature differences between a neoprene sleeve and an elastic wrap. With regard to exercise, it would be compelling to analyze different phases of the exercise interval to determine the length of exercise needed to maintain a temperature change. Similarly, it would be beneficial to study exercise time as a variable to see its influence on length of time for heat retention.
CONCLUSIONS
Neoprene sleeves are beneficial in maintaining elevated skin and intramuscular temperatures after exercise. This finding may be beneficial in preventing and treating muscle strains in athletes whose activity is interspersed with periods of sitting or standing, as, for example, a basketball player who is taken out of a game or a football player who plays only defense. Both athletes have the possibility of being inactive for an extended time. Neoprene sleeves help to maintain higher skin and intramuscular temperature during periods of inactivity, decreasing the probability of a musculotendinous injury.
Footnotes
Alison A. Miller, MS, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and, drafting, critical revision, and final approval of the article. Kenneth L. Knight, PhD, ATC, FACSM; J. Brent Feland, PhD, PT; and David O. Draper, EdD, ATC, contributed to analysis and interpretation of the data and drafting, critical revision, and final approval of the article.
Address correspondence to Kenneth L. Knight, PhD, ATC, FACSM, Brigham Young University, 271 SFH, Provo, UT 84602. Address e-mail to ken_knight@byu.edu.
REFERENCES
- Cramer Products I, Sports Medicine 2000. Gardner, KS: Cramer Products; 2000.
- Safran MR, Garrett WE, Jr, Seaber AV, Glisson RR, Ribbeck BM. The role of warmup in muscular injury prevention. Am J Sports Med. 1988;16:123–129. doi: 10.1177/036354658801600206. [DOI] [PubMed] [Google Scholar]
- Noonan TJ, Best TM, Seaber AV, Garrett WE., Jr. Thermal effects on skeletal muscle tensile behavior. Am J Sports Med. 1993;21:517–522. doi: 10.1177/036354659302100407. [DOI] [PubMed] [Google Scholar]
- Wirth V, Van Lunen BL, Mistry D, Saliba EN, McCue FC. Temperature changes in deep muscles of humans during upper and lower extremity exercise. J Athl Train. 1998;33:382–385. [PMC free article] [PubMed] [Google Scholar]
- Johnson JM. Physical training and the control of skin blood flow. Med Sci Sports Exerc. 1998;30:382–386. doi: 10.1097/00005768-199803000-00007. [DOI] [PubMed] [Google Scholar]
- Kellogg DL, Jr, Johnson JM, Kenney WL, Pergola PE, Kosiba WA. Mechanisms of control of skin blood flow during prolonged exercise in humans. Am J Physiol. 1993;265:H562–H568. doi: 10.1152/ajpheart.1993.265.2.H562. (2, Pt 2) [DOI] [PubMed] [Google Scholar]
- Radegran G, Saltin B. Muscle blood flow at onset of dynamic exercise in humans. Am J Physiol. 1998;274:H314–H322. doi: 10.1152/ajpheart.1998.274.1.H314. (1, Pt 2) [DOI] [PubMed] [Google Scholar]
- Ramos RJ. Muscle Temperature Change During Exercise With a Commercial Back Plaster Applied to the Gastrocnemius Muscle. [master's thesis]. Provo, UT: Brigham Young University; 1999.
- Saltin B, Hermansen L. Esophageal, rectal, and muscle temperature during exercise. J Appl Physiol. 1966;21:1757–1762. doi: 10.1152/jappl.1966.21.6.1757. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Alonso J, Teller C, Andersen SL, Jensen FB, Hyldig T, Nielsen B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J Appl Physiol. 1999;86:1032–1039. doi: 10.1152/jappl.1999.86.3.1032. [DOI] [PubMed] [Google Scholar]
- Beynnon BD, Ryder SH, Konradsen L, Johnson RJ, Johnson K, Renstrom PA. The effect of anterior cruciate ligament trauma and bracing on knee proprioception. Am J Sports Med. 1999;27:150–155. doi: 10.1177/03635465990270020601. [DOI] [PubMed] [Google Scholar]
- Birmingham TB, Kramer JF, Inglis JT. Effect of a neoprene sleeve on knee joint position sense during sitting open kinetic chain and supine closed kinetic chain tests. Am J Sports Med. 1998;26:562–566. doi: 10.1177/03635465980260041601. et al. [DOI] [PubMed] [Google Scholar]
- Perlau R, Frank C, Fick G. The effect of elastic bandages on human knee proprioception in the uninjured population. Am J Sports Med. 1995;23:251–255. doi: 10.1177/036354659502300221. [DOI] [PubMed] [Google Scholar]
- Mancuso DL, Knight KL. Effects of prior physical activity on skin surface temperature response of the ankle during and after a 30-minute ice pack application. J Athl Train. 1992;27:242–249. [PMC free article] [PubMed] [Google Scholar]
- Myrer JW, Draper DO, Durrant E. Contrast therapy and intramuscular temperature in the human leg. J Athl Train. 1994;29:318–322. [PMC free article] [PubMed] [Google Scholar]
- Iwamoto J, Sagawa S, Tajima F, Miki K, Tanaka H, Shiraki K. Changes in insulation of body tissue and wet suits during underwater exercise at various atmospheric pressures. J Appl Physiol. 1990;68:659–664. doi: 10.1152/jappl.1990.68.2.659. [DOI] [PubMed] [Google Scholar]
- Kerr CG, Trappe TA, Starling RD, Trappe SW. Hyperthermia during Olympic triathlon: influence of body heat storage during the swimming stage. Med Sci Sports Exerc. 1998;30:99–104. doi: 10.1097/00005768-199801000-00014. [DOI] [PubMed] [Google Scholar]
- Merrick MA, Knight KL, Ingersoll CD, Potteiger JA. The effects of ice and compression wraps on intramuscular temperature at various depths. J Athl Train. 1993;28:236–245. [PMC free article] [PubMed] [Google Scholar]
- Favero M. Chemical Disinfection of Medical and Surgical Materials: Disinfection, Sterilization, and Preservation. 3rd ed. Philadelphia, PA: Lea & Febiger; 1983:469–486.
- Stolwijk JA, Saltin B, Gagge AP. Physiological factors associated with sweating during exercise. Aerosp Med. 1968;39:1101–1105. [PubMed] [Google Scholar]
- Ho SP, Fan SS. Effect of clothing on the temperature distribution of human thermal system. Comput Biol Med. 1975;5:203–219. doi: 10.1016/0010-4825(75)90005-0. [DOI] [PubMed] [Google Scholar]
- Nagata H. Evaporative heat loss and clothing. J Hum Ergol (Tokyo) 1978;7:169–175. [PubMed] [Google Scholar]
- MacDougall JD, Reddan WG, Layton CR, Dempsey JA. Effects of metabolic hyperthermia on performance during heavy prolonged exercise. J Appl Physiol. 1974;36:538–544. doi: 10.1152/jappl.1974.36.5.538. [DOI] [PubMed] [Google Scholar]
- Parkin JM, Carey MF, Zhao S, Febbraio MA. Effect of ambient temperature on human skeletal muscle metabolism during fatiguing submaximal exercise. J Appl Physiol. 1999;86:902–908. doi: 10.1152/jappl.1999.86.3.902. [DOI] [PubMed] [Google Scholar]
- Dawson B, Straton S, Randall N. Oxygen consumption during recovery from prolonged submaximal cycling below the anaerobic threshold. J Sports Med Phys Fitness. 1996;36:77–84. [PubMed] [Google Scholar]
- Gersten JW. Effect of ultrasound on tendon extensibility. Am J Phys Med. 1955;34:362–369. [PubMed] [Google Scholar]
- Draper DO, Knight KL, Fujiwara T, Castel JC. Temperature change in human muscle during and after pulsed short-wave diathermy. J Orthop Sports Phys Ther. 1999;29:13–22. doi: 10.2519/jospt.1999.29.1.13. [DOI] [PubMed] [Google Scholar]
- Draper DO, Ricard MD. Rate of temperature decay in human muscle following 3 MHz ultrasound: the stretching window revealed. J Athl Train. 1995;30:304–307. [PMC free article] [PubMed] [Google Scholar]
- Garrett CL, Draper DO, Knight KL. Heat distribution in the lower leg from pulsed short-wave diathermy and ultrasound treatments. J Athl Train. 2000;35:50–55. [PMC free article] [PubMed] [Google Scholar]
- Rose S, Draper DO, Schulthies SS, Durrant E. The stretching window part two: rate of thermal decay in deep muscle following 1-MHz ultrasound. J Athl Train. 1996;31:139–143. [PMC free article] [PubMed] [Google Scholar]