Abstract
Context: Athletic trainers surveyed in 1999 demonstrated little consensus on the use of concussion grading scales and return-to-play criteria. Most relied on clinical examination or symptom checklists to evaluate athletes with concussion.
Objective: To investigate the current trends of certified athletic trainers in concussion assessment and management.
Design: Subjects were invited to participate in a 32-question Internet survey.
Setting: An Internet link to the survey was e-mailed to the subjects.
Patients or Other Participants: A total of 2750 certified athletic trainers and members of the National Athletic Trainers' Association were randomly e-mailed and invited to participate.
Main Outcome Measure(s): Survey questions addressed topics including years of certification, number of concussions evaluated each year, methods of assessing concussion, and guidelines used for return to play. Compliance with the recent position statement of the National Athletic Trainers' Association on sport-related concussion was also evaluated.
Results: Certified athletic trainers averaged 9.9 ± 7.3 years of certification and evaluated an average of 8.2 ± 6.5 concussions per year. To assess concussion, 95% reported using the clinical examination, 85% used symptom checklists, 48% used the Standardized Assessment of Concussion, 18% used neuropsychological testing, and 16% used the Balance Error Scoring System. The most frequently used concussion grading scale and return-to-play guideline belonged to the American Academy of Neurology (30%). When deciding whether to return an athlete to play, certified athletic trainers most often used the clinical examination (95%), return-to-play guidelines (88%), symptom checklists (80%), and player self-report (62%). The most important tools for making a return-to-play decision were the clinical examination (59%), symptom checklists (13%), and return-to-play guidelines (12%). Only 3% of certified athletic trainers surveyed complied with the recent position statement, which advocated using symptom checklists, neuropsychological testing, and balance testing for managing sport-related concussion.
Conclusions: Our findings suggest that only a small percentage of certified athletic trainers currently follow the guidelines proposed by the National Athletic Trainers' Association. Various assessment methods and tools are currently being used, but clinicians must continue to implement a combination of methods and tools in order to comply with the position statement.
Keywords: mild traumatic brain injury, mild brain injury, evaluation
Sports medicine clinicians and researchers have access to a variety of tools for evaluating and rehabilitating athletic injuries. These tools, for the most part, offer clinicians information about the presence and severity of injury. Additionally, they may suggest a timeframe for rehabilitation and return to play. However, this is not the case with sport-related concussion. No simple tests can be performed on the brain to determine the severity of a closed head injury and help clinicians establish goals for rehabilitation and return to play. The complexity of concussion injuries requires clinicians to use a variety of tools for information, but the current tendency is to base the return-to-play decision on the athlete's self-reporting of symptoms and ability to perform sport-specific tasks without a recurrence of concussion symptoms.1–4 Relying solely on this information can be dangerous because it creates an incomplete picture of the injury.
A multifaceted protocol has been proposed by several authors in the literature.1,2,5–9 The recent position statement of the National Athletic Trainers' Association (NATA) recommends the use of symptom checklists, neuropsychological testing, and postural stability assessment.5 Baseline testing on these measures is important for athletes participating in sports with a high concussion risk; however, if resources allow, then all athletes should receive baseline assessment. Follow-up testing should be conducted to aid in the decision process for return to play. Using all the available information may be the best approach to safely returning an athlete to play after a concussion.
Research on sport-related concussion has increased tremendously in the modern era. A literature search on PubMed revealed large increases in the amount of published material in scientific journals each decade since the 1960s (Table 1). This increase in research has expanded the information available to certified athletic trainers (ATCs) and led to a greater understanding of sport-related concussion. However, the literature has also raised more questions and forced clinicians to rethink their approach to concussion management.
Table 1. Number of Published Materials on Concussion in Sport in PubMed*.
Our study is based on a survey similar to one administered at the 1999 NATA Annual Meeting and Clinical Symposia.10 The authors analyzed trends in concussion assessment and management by ATCs. Little consensus was found on concussion grading scales and return-to-play criteria, and most ATCs relied on clinical examination or symptom checklists as evaluative tools for concussion assessment. The ATCs evaluated an average of 7 concussions per year and, along with team physicians, were primarily responsible for making return-to-play decisions. The majority of ATCs also indicated that standardized methods of concussion assessment (SMCA) would help provide more information for concussion management.10
In recent years, several journal special issues and position statements have been devoted solely to concussion in sport.5,7,8,11,12 Given the increase in published research findings in recent years, our purposes were to (1) investigate and update the current trends in athletic training practice for concussion assessment and management, (2) determine whether the trends have changed over the past 5 years, and (3) evaluate whether ATCs were compliant with the recent NATA position statement on sport-related concussion.
METHODS
A list of approximately 2750 ATCs was randomly generated from all regular certified members of the NATA. These members were contacted by e-mail, which included a link to the survey. The ATCs agreeing to participate in this study took approximately 20 minutes to complete the survey. The Academic Affairs Institutional Review Board approved the survey, and consent to participate in the study was implied by the subjects' submission of the online survey.
We adapted a 32-question survey (Table 2) from a 21-item survey used by Ferrara et al.10 Our intent was to evaluate the clinical practice habits and decision-making skills of ATCs in relation to sport concussion. The survey first gathered demographic data, the number of years certified, employment position and setting, and the sports covered by the clinician. It then asked for an average number of concussions seen by the clinician per year and selected symptoms observed with these injuries. The survey asked the subject to identify the clinical tools used and the individuals responsible for return-to-play decisions. Several questions asked about the use of SMCA, and ATCs were given examples such as the Standardized Assessment of Concussion (SAC),13 the Balance Error Scoring System (BESS),9 and neuropsychological testing. For our purposes, we further defined SMCA retrospectively as tools and methods described in the literature that are objective in nature and use standard scoring. Questions asked clinicians what decisions would be made for return to play given hypothetical information. Subjects were also asked if they consulted with neuropsychologists or thought that ATCs should be trained to administer neuropsychological examinations.
Table 2. Sample Questions from Athletic Trainer Concussion Questionnaire—2004.
The survey was posted on the Internet and hosted by SurveyMonkey.com. Questions were grouped in blocks of 3 to 5 for the ease of the respondents and were presented in mainly multiple choice and fill-in-the-blank formats. Respondents were not required to answer all questions and were free to pass over any questions or sections. The survey was free to all respondents and did not collect any personal information. The response data were available only to the researchers and were downloaded as a Microsoft Excel (version 2000; Microsoft Corp, Redmond, WA) spreadsheet.
Descriptive statistics were calculated on the data, followed by chi-square tests of association using SPSS (version 11.5; SPSS Inc, Chicago, IL). Alpha level was set a priori at .05 for all tests.
RESULTS
A total of 927 ATCs responded to the 2750 e-mails sent out, for a response rate of 33.7%. Surveyed ATCs averaged 9.94 ± 7.3 years of certification. All respondents were current ATCs except for 1 who had recently retired. More than 85% (n = 676/779 [86.78%]) reported being licensed if their state had athletic trainer licensure available. More than half (568/ 926 [61.34%]) of those surveyed had earned a master's degree or PhD.
The most common responses for primary employment position were the high school (323/911 [35.46%]), collegiate (314/911 [34.47%]), and sports medicine (109/911 [11.96%]) clinical settings. Subjects were most often responsible for covering women's basketball, men's basketball, football, baseball, and women's soccer. More than 30% (232/769) reported using the American Academy of Neurology14 recommendations as their primary return-to-play guidelines. The Colorado Medical Society15 and the 2001 Cantu evidence-based3 guidelines followed, with 20.7% (159/769) and 19.9% (153/769), respectively, whereas 13.1% (101/769) used some combination of guidelines or a site-specific guideline, and 8.6% (66/769) reported not using any return-to-play guidelines.
The average number of concussions diagnosed per year was 8.2 ± 6.5 (Table 3). Only 20% of ATCs reported evaluating more than 10 concussions per year, with more than 50% of those being in the high school setting.
Table 3. Concussions Evaluated Per Year by Athletic Trainers' Primary Employment Settings (Number, Percentage).
More than 80% of ATCs surveyed reported evaluating relatively few concussions (less than 25% of the total) that involved loss of consciousness, retrograde amnesia, or posttraumatic amnesia (Table 4). Of the ATCs who had evaluated cases of postconcussion syndrome, approximately 68% (465/686) said a physician had diagnosed the condition.
Table 4. Athletic Trainers' Witnessing of Selected Concussion Symptoms (Number, Percentage).
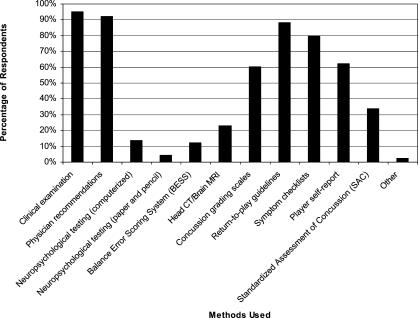
Respondents reported using a variety of methods to assess and evaluate concussion and make return-to-play decisions. The clinical examination and symptom checklists are used consistently for concussion evaluation (>85% of the time) among ATCs (Figure 1). Clinical examinations, physician recommendations, return-to-play guidelines, and symptom checklists are the most common return-to-play methods used (≥80% of the time), and the clinical examination was the most frequently reported primary method (Figures 2 and 3).
Figure 1. Frequency of methods used to evaluate and diagnose concussion. Subjects were asked to check all that apply.
Figure 2. Frequency of methods used to guide return-to-play decisions. Subjects were asked to check all that apply.
Figure 3. Frequency of primary method/tools used to guide return-to-play decisions. Subjects were asked to select the primary method guiding return-to-play decisions.
The team physician was reported to be the most responsible person in making return-to-play decisions, with the ATC as the second most responsible (Table 5).
Table 5. Caregivers Responsible for Making Return-to-Play Decisions (Number, Percentage)*.
Approximately 68% (518/762) reported that using SMCA would be more helpful than relying on the clinical examination alone. Just over 32% (244/762) stated that using SMCA would not add anything to the clinical examination. Thirty-five percent (266/752) stated that SMCA would have no effect on the return-to-play decisions, whereas 17.0% (128/752) declared that an athlete would likely return sooner if SMCA were used. Almost 48% (358/752) reported that, in their opinion, SMCA would prolong the amount of time an athlete would remain out of competition after a concussion. More than 62% (470/ 758) did not believe that SMCA could be misused to return an athlete to play sooner than usual.
Subjects were asked about a scenario in which an athlete sustained a mild head injury and had no loss of consciousness but posttraumatic amnesia for less than 1 minute. Three sets of hypothetical findings on follow-up examination were given and the ATCs asked if they would return the athlete to play (Table 6). Approximately 15% reported that they would return an athlete to play if the only abnormal findings were noted on SMCA.
Table 6. Athletic Trainers' Return-to-Play Decisions Based on Hypothetical Situations.
Of the ATCs surveyed, 135 reported using computerized neuropsychological testing. Seventy-five percent (100/135) used ImPACT (University of Pittsburgh Medical Center, Pittsburgh, PA) as their primary computerized neuropsychological test. Almost 10% (13/135) used ANAM (National Rehabilitation Hospital Assistive Technology and Neuroscience Center, Washington, DC), 4.5% (6/135) used CogState (CogState Ltd, Victoria, Australia), and 4.5% (6/135) used HeadMinder (HeadMinder Inc, New York, NY). Just over 25% (193/767) reported having access to a neuropsychologist for consultation after a concussion, but only about one fourth of those (48/198) said they routinely consult the neuropsychologist. Seventy-eight percent (593/757) stated that athletic trainers should be trained to administer neuropsychological tests to assess concussion.
Chi-square tests of association were performed to assess for trends between the number of years certified and the clinical tools used, the number of years certified and the primary position, the primary position and the clinical tools used, and the employment setting and the clinical tools used. A significant relationship was found between ATCs with more years of certification and increased use of computerized neuropsychological testing (χ24 = 14.12, P = .007). High school ATCs more frequently used symptom checklists (χ24 = 14.11, P = .007), and college and professional ATCs more frequently used computerized neuropsychological tests (χ24 = 27.92, P ≤ .001) compared with ATCs in different employment settings.
DISCUSSION
Our purpose was to examine the current trends in concussion assessment and management, to compare those trends with a comparable survey conducted 5 years earlier, and to investigate practice patterns of ATCs in relation to the NATA position statement on sport-related concussion. Currently, ATCs assess an average of 8.2 concussions per year, up from an average of 7.0 concussions per year reported 5 years ago.10 We were unable to determine whether this is a significant difference because we did not have access to the data from the original survey. Whether these findings reflect an increase in concussion incidence or better identification of concussions that may have previously gone undetected is unclear.
Scientific publications on sport-related concussion have increased by 17% during the last 4 years (172 from 2000 through 2004) over the prior decade (143 from 1990 through 1999) (see Table 1). Given the large increase in concussion research, ATCs have more information available on this topic and likely a higher level of awareness than 5 years ago.
Our survey data show that more ATCs are using tools available to them than 5 years ago. More than 95% of ATCs used the clinical examination, 85% used a symptom checklist, 48% used the SAC,13 16% used the BESS,9 and 18% used neuropsychological testing. These results help to describe the current trends in concussion management when compared with the findings of Ferrara et al10 that 33% used the clinical examination, 35% used symptom checklists, 10% used the SAC,13 5% used the BESS,9 and 15% used neuropsychological testing. With the reported increases in the use of these methods and tools, it seems that ATCs are now in better position to assess and manage concussions.
The suggestion that more concussions are occurring in sport, however, has not yet been substantiated, primarily because of the challenges faced in collecting both exposure and injury data. The Centers for Disease Control and Prevention estimated 300 000 sport-related concussions annually in the United States.16 The actual incidence per exposure to concussion could be decreasing, because participation in sports with concussion risks continues to grow every year while the number of injuries has remained fairly constant.17 Concussion incidence has primarily been reported in football. In 1983, Gerberich et al18 reported that 20% of high school football players sustained a concussion in a given season; however, this study has been widely criticized because of the retrospective collection of data by players and coaches. Collegiate football had an estimated 10% incidence rate in the 1980s,19 but a more recent investigation has indicated a lower incidence rate for both high school (5.6%) and collegiate football (4.4 to 5.5%).20 However, the number of concussions occurring may actually be higher than those evaluated and reported by ATCs, based on results of a recent study by McCrea et al21 that nearly 50% of all concussions during a high school football season were unreported. With advances in concussion research and the availability of more sophisticated assessment tools, clinicians may have become better at both identifying and assessing concussion.
There is still no consensus on concussion grading scales and return-to-play guidelines. Although the number of clinicians not using a grading system is less than previously reported, one grading scale does not appear to be overwhelmingly preferred over another. Most concussion guidelines rely on loss of consciousness and amnesia to help grade the severity of concussion. However, loss of consciousness and amnesia are seen in relatively few cases of concussion.20,22 Results from our study concur, as the clinicians reported evaluating few athletes with loss of consciousness and amnesia. Previous authors20,22,23 noted that concussed athletes present most often with headache, poor balance and dizziness, confusion, or feeling “slowed down.” The majority of concussion guidelines focus solely on loss of consciousness and posttraumatic amnesia, ignoring other signs and symptoms, as well as their duration and severity.
A discrepancy appears to exist between the current expectations that clinicians should regularly use SMCA and what occurs on the playing fields and in athletic training rooms across America. A smaller percentage of respondents in this study (68%) than in the previous study (86%)10 reported that using SMCA would be more effective than using the clinical examination alone. In both studies, ATCs reported (47% in both) that using SMCA would prolong the amount of time an athlete would be withheld from competition. Because more clinicians in our study reported that SMCA could be misused (38% versus 24%) or could prolong the amount of time an athlete would remain out of competition, it would seem that SMCA is not gaining popularity as might be expected given the abundance of published research on sport-related concussion in recent years. Also, when asked a hypothetical question (see Table 2) about a concussed athlete, more respondents in our study (12.6% versus 1.2% in the previous study) indicated they would allow an athlete to return to play who had a normal clinical examination but an abnormal SMCA. Clinicians should understand that SMCA gives reliable information about a player's status; an abnormal SMCA should caution the clinician against allowing the athlete to return to competition. As a follow-up to help explain our main findings, we conducted post hoc analyses (chi-square tests of association), which revealed no association between clinicians using SMCA and their responses to our hypothetical questions.
Although neuropsychological assessment is recommended for athletes both before participation and in guiding return to play,24 our survey shows that relatively few ATCs use this tool. Accessibility may be one barrier. Neuropsychological testing is relatively new to the sports medicine community, and ATCs often do not have the time or the resources to obtain baseline tests and perform follow-up assessments after concussion. Computerized neuropsychological testing is probably the most convenient protocol, but testing multiple subjects at one time requires multiple computers. If computer availability is limited, only a few athletes can be evaluated in 15 to 35 minutes, which may not be practical for many institutions. In the event of an injury, ATCs and physicians still need to involve a neuropsychologist to assist in interpreting the results before making a return-to-play decision. Paper-and-pencil testing is more available but typically requires a trained person to administer and interpret the test results. The problem of being able to test only a limited number of athletes at one time also restricts the use of paper-and-pencil testing.
We observed an association between an ATC's experience and the likelihood of using neuropsychological testing for managing concussion. The more years of experience an ATC reported, the more likely he or she was to use neuropsychological testing. This finding could suggest that entry-level athletic trainers are not being exposed to this tool in their athletic training experience. Experience in the field and exposure to neuropsychological testing through research may lead clinicians to incorporate this tool into their concussion management protocols.
The NATA position statement on concussion management recommends that all athletes, especially those playing sports with high concussion risks, be enrolled in a program involving cognitive and postural stability testing. These tests should be performed before the athlete engages in activity to establish a baseline for the individual and then after a concussion is diagnosed to identify any deficits that cannot be determined by self-reported symptoms.5 Our data indicate that only about 3% of those surveyed currently cover all 3 areas recommended by the NATA by using symptom checklists, neuropsychological testing, and the BESS for concussion assessment or return-to-play decisions. About 24% used at least 2 methods, and 80% used at least 1 method. The actual percentage is potentially higher because the only postural stability measure we inquired about was the BESS. Clinicians may use an alternate form of postural stability testing, such as forceplate measures. However, even if our survey included other forms of postural stability testing, we would not expect compliance with the NATA recommendations to improve.
Our study is restricted by the inherent limitations of survey research. We assume that the subjects answered the questions truthfully and honestly. We also assume that all subjects read and interpreted the questions in the same way. For example, although no return-to-play decision should be based on an individual tool, we did not provide specifics as to which tools were used in the hypothetical situations. Thus, this lack of information could have led to variable responses by the participants. Our response rate (34%) appeared low; however, we believe the response rate was actually higher than calculated because about 150 e-mail addresses returned mail server errors and were determined undeliverable. We estimated that another 10% of the e-mail addresses were no longer in use, because e-mail addresses tend to change frequently. We expect that our adjusted response rate would approach 40%, which is within the range (36% to 52%) for similarly administered Web-based surveys reviewed in the literature.25–27 Another potential limitation was that some of the surveys were not fully completed. We chose to include information on any question submitted, but this led to a variation in the number of responses for each survey item and to the number of responses we used in analysis.
In conclusion, our findings suggest that, in general, ATCs have made moderate progress in concussion assessment and management during the past 5 years. However, clinicians need to continue to incorporate and improve concussion protocols at their individual sites. Further research and education are important in evaluating and managing concussions. Clinicians should make a concerted effort to incorporate as many tools and methods as possible in order to obtain a complete picture of each individual's concussion. This will allow clinicians to make well-informed return-to-play decisions and will ultimately allow for safer participation for athletes. Future prospective studies involving interventions should allow us to more clearly investigate the role of SMCA in making safe return-to-play decisions after concussion.
Footnotes
Andrew J. Notebaert, MS, ATC, and Kevin M. Guskiewicz, PhD, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
Address correspondence to Kevin M. Guskiewicz, PhD, ATC, Department of Exercise and Sport Science, The University of North Carolina at Chapel Hill, Fetzer Gym CB#8700, Chapel Hill, NC 27599. Address e-mail to gus@email.unc.edu.
REFERENCES
- Guskiewicz KM, Cantu RC. The concussion puzzle: evaluation of sport-related concussion. Am J Med Sports. 2004;6:13–21. [Google Scholar]
- Oliaro S, Anderson S, Hooker D. Management of cerebral concussion in sports: the athletic trainer's perspective. J Athl Train. 2001;36:257–262. [PMC free article] [PubMed] [Google Scholar]
- Cantu RC. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36:244–248. [PMC free article] [PubMed] [Google Scholar]
- Durand P, Jr, Adamson GJ. On-the-field management of athletic head injuries. J Am Acad Orthop Surg. 2004;12:191–195. doi: 10.5435/00124635-200405000-00007. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, Bruce SL, Cantu RC. National Athletic Trainers' Association position statement: management of sport-related concussion. J Athl Train. 2004;39:280–297. et al. [PMC free article] [PubMed] [Google Scholar]
- McCrory P, Johnston K, Meeuwisse W. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Clin J Sport Med. 2005;15:48–55. doi: 10.1097/01.jsm.0000159931.77191.29. et al. [DOI] [PubMed] [Google Scholar]
- Aubry M, Cantu R, Dvorak J. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36:6–10. doi: 10.1136/bjsm.36.1.6. et al. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wojtys EM, Hovda D, Landry G. Current concepts: concussion in sports. Am J Sports Med. 1999;27:676–687. doi: 10.1177/03635465990270052401. et al. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, Ross SE, Marshall SW. Postural stability and neuropsychological deficits after concussion in collegiate athletes. J Athl Train. 2001;36:263–273. [PMC free article] [PubMed] [Google Scholar]
- Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36:145–149. [PMC free article] [PubMed] [Google Scholar]
- Special issue: concussion in sports. Clin J Sport Med. 2000;11(3)
- Special issue: concussion in athletes. J Athl Train.2001;36(3) [PMC free article] [PubMed]
- McCrea M, Randolph C, Kelly JP. Standardized Assessment of Concussion (SAC): Manual for Administration, Scoring and Interpretation. 2nd ed. Waukesha, WI: CNS Inc; 2000.
- Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- Colorado Medical Society Sports Medicine Committee. Guidelines for the management of concussion in sports. Proceedings of the Mild Brain Injury in Sports Summit. Dallas, TX: National Athletic Trainers' Association; 1994: 106–109.
- Centers for Disease Control and Prevention. Sports-related recurrent brain injuries: United States. MMWR Morbid Mortal Wkly Rep. 1997;46:224–227. [PubMed] [Google Scholar]
- Bray C. 1982–2003 Sports Sponsorship and Participation Report. Indianapolis, IN: National Collegiate Athletic Association; 2004.
- Gerberich SG, Priest JD, Boen JR, Straub CP, Maxwell RE. Concussion incidences and severity in secondary school varsity football players. Am J Public Health. 1983;73:1370–1375. doi: 10.2105/ajph.73.12.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barth JT, Alves W, Ryan T. Mild head injury in sports: neuropsychological sequela and recovery of function. et al. In: Levin H, Eisenberg H, Denton A, eds. Mild Head Injury. New York, NY: Oxford University Press; 1989:257–275.
- Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr. Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14:13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- Guskiewicz KM, McCrea M, Marshall SW. Cumulative effects of recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290:2549–2555. doi: 10.1001/jama.290.19.2549. et al. [DOI] [PubMed] [Google Scholar]
- Collins MW, Field M, Lovell MR. Relationship between postconcussion headache and neuropsychological test performance in high school athletes. Am J Sports Med. 2003;31:168–173. doi: 10.1177/03635465030310020301. et al. [DOI] [PubMed] [Google Scholar]
- McCrory P. Preparticipation assessment for head injury. Clin J Sport Med. 2004;14:139–144. doi: 10.1097/00042752-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Umefjord G, Petersson G, Hamberg K. Reasons for consulting a doctor on the Internet: Web survey of users of an Ask the Doctor service. J Med Internet Res. 2003;5:e26. doi: 10.2196/jmir.5.4.e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanelli F, Ryan M, Smith KM. Board of Pharmaceutical Specialties-certified faculty: a survey of United States colleges of pharmacy. Pharmacotherapy. 2004;24:395–400. doi: 10.1592/phco.24.4.395.33183. [DOI] [PubMed] [Google Scholar]
- Braithwaite D, Emery J, De Lusignan S, Sutton S. Using the Internet to conduct surveys of health professionals: a valid alternative? Fam Pract. 2003;20:545–551. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]