Abstract
Objective:
To present an overview of the medical conditions experienced by athletes competing in the National Basketball Association (NBA) from the 1988-1989 through the 1997-1998 seasons.
Design and Setting:
Athletic trainers completed profiles that provided demographic information for each player. Injury reports indicated when and where the injury occurred, pathology, onset, activity, and the mechanism of injury. The amount of time lost, injured list status, hospitalization, and surgery were also reported. Reportable injuries were those that resulted in (1) physician referral, (2) a practice or game being missed, or (3) emergency care being rendered.
Subjects:
A total of 1094 players appeared in the database 3843 times (mean, 3.3 ± 2.6 seasons). Mean player demographics were age 26.7 (± 3.7) years, NBA playing experience 4.1 (± 3.7) years, height 200.8 (± 9.9) cm, and weight 100.2 (± 13.5) kg. Players averaged 52 (± 34.7) games and 1263.1 (± 1073.8) minutes played.
Measurements:
The frequency of injury, time lost, and game exposures were tabulated, and game-related injury rates were then calculated.
Results:
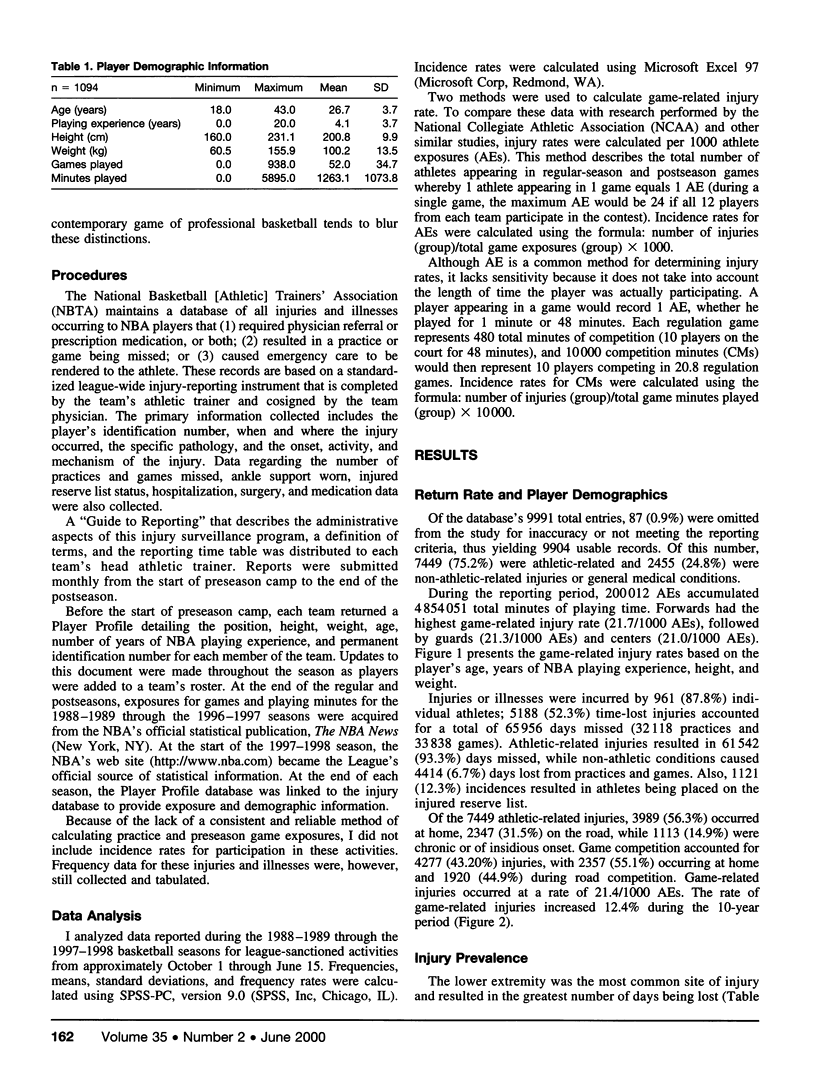
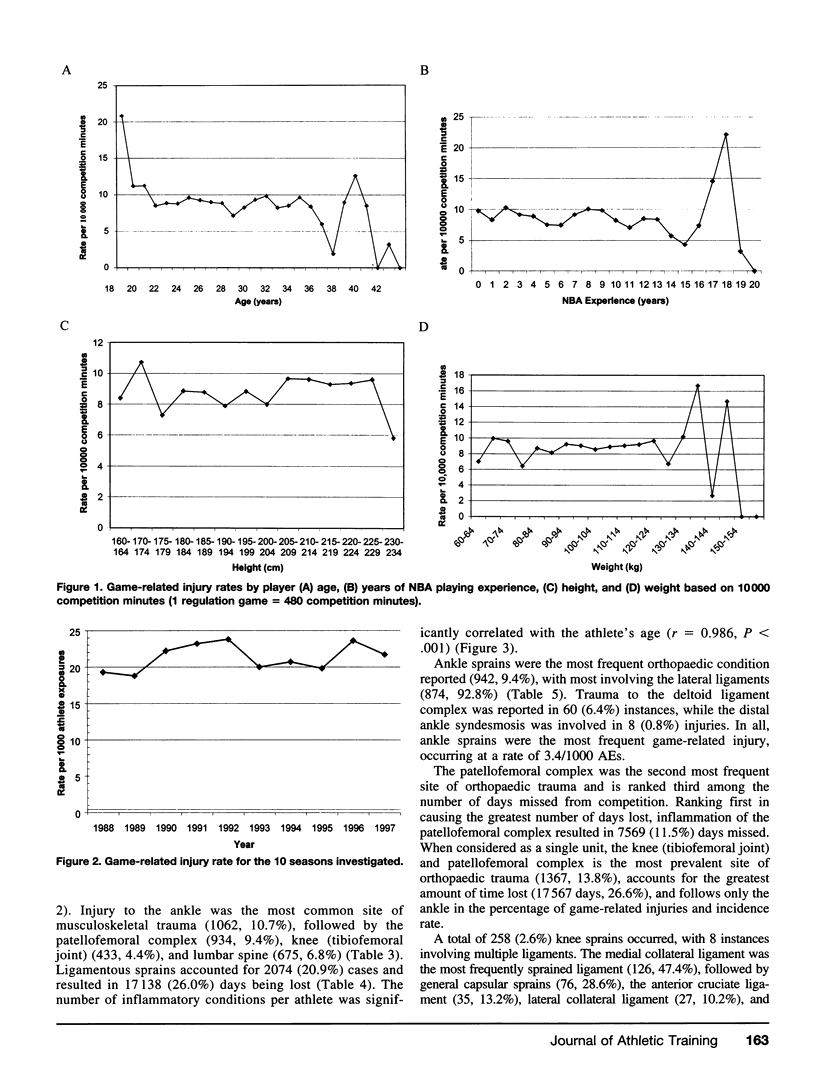
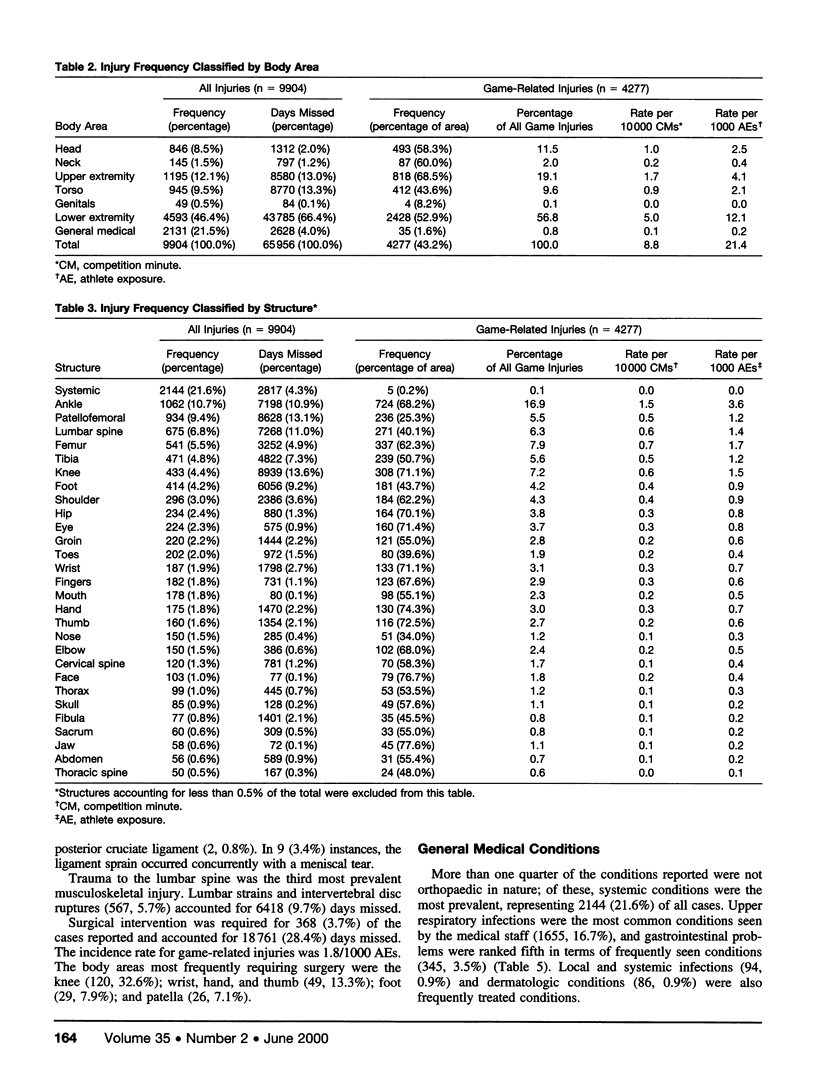
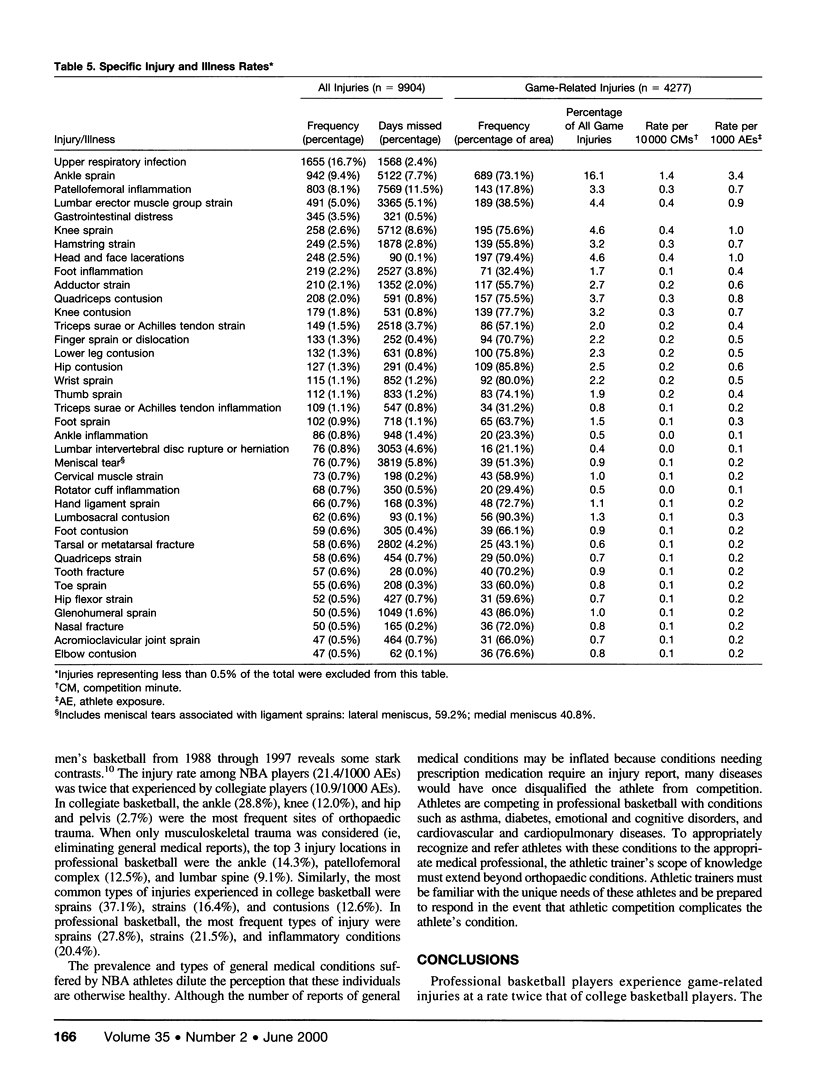
Ankle sprains were the most frequently occurring orthopaedic injury (942, 9.4%), followed by patellofemoral inflammation (803, 8.1%), lumbar strains (491, 5.0%), and knee sprains (258, 2.3%). The greatest number of days missed were related to patellofemoral inflammation (7569, 11.5%), knee sprains (5712, 8.6%), ankle sprains (5122, 7.7%), and lumbar strains (3365, 5.1%).
Conclusions:
Professional athletes in the NBA experience a rate of game-related injuries that is twice as high as their collegiate counterparts. Patellofemoral inflammation is a significant problem among NBA players.
Keywords: epidemiology, professional sports, ankle sprains, knee sprains
Full text
PDF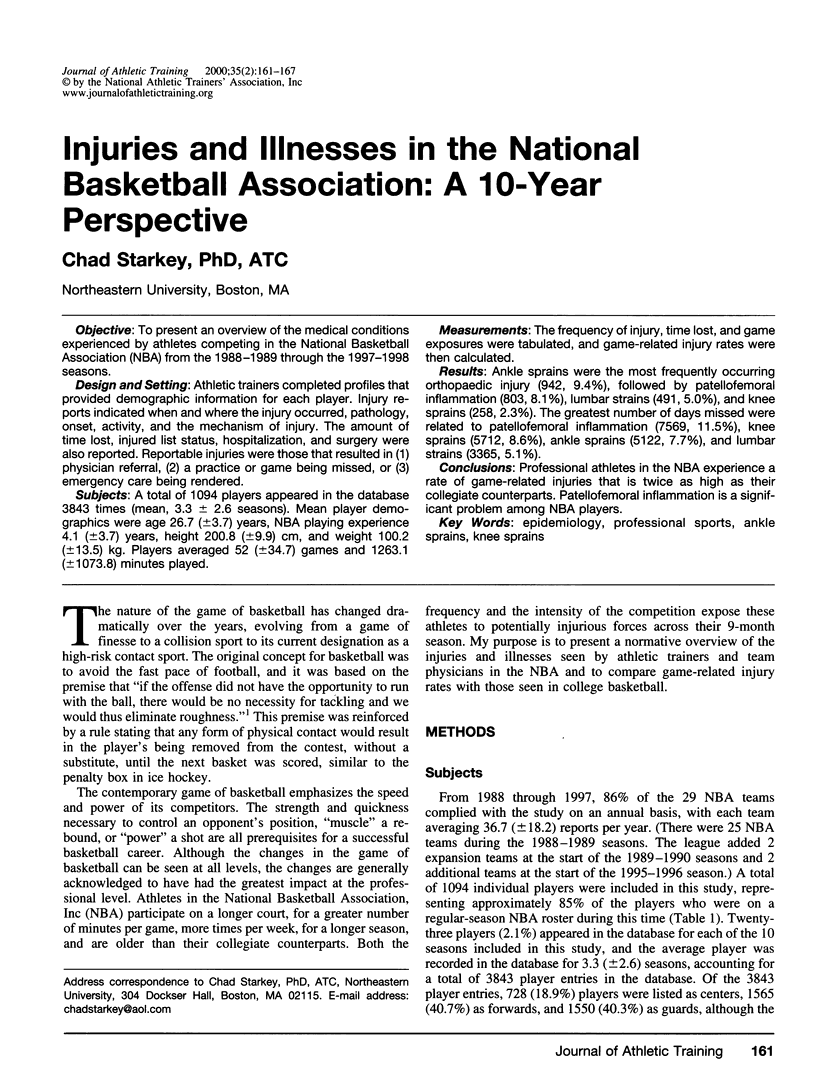

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barrett J. R., Tanji J. L., Drake C., Fuller D., Kawasaki R. I., Fenton R. M. High- versus low-top shoes for the prevention of ankle sprains in basketball players. A prospective randomized study. Am J Sports Med. 1993 Jul-Aug;21(4):582–585. doi: 10.1177/036354659302100416. [DOI] [PubMed] [Google Scholar]
- Emerson R. J. Basketball knee injuries and the anterior cruciate ligament. Clin Sports Med. 1993 Apr;12(2):317–328. [PubMed] [Google Scholar]
- Herskowitz A., Selesnick H. Back injuries in basketball players. Clin Sports Med. 1993 Apr;12(2):293–306. [PubMed] [Google Scholar]
- Krinsky M. B., Abdenour T. E., Starkey C., Albo R. A., Chu D. A. Incidence of lateral meniscus injury in professional basketball players. Am J Sports Med. 1992 Jan-Feb;20(1):17–19. doi: 10.1177/036354659202000105. [DOI] [PubMed] [Google Scholar]
- Leanderson J., Nemeth G., Eriksson E. Ankle injuries in basketball players. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):200–202. doi: 10.1007/BF01560206. [DOI] [PubMed] [Google Scholar]
- Sitler M., Ryan J., Wheeler B., McBride J., Arciero R., Anderson J., Horodyski M. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at West Point. Am J Sports Med. 1994 Jul-Aug;22(4):454–461. doi: 10.1177/036354659402200404. [DOI] [PubMed] [Google Scholar]
- Zagelbaum B. M., Starkey C., Hersh P. S., Donnenfeld E. D., Perry H. D., Jeffers J. B. The National Basketball Association eye injury study. Arch Ophthalmol. 1995 Jun;113(6):749–752. doi: 10.1001/archopht.1995.01100060075035. [DOI] [PubMed] [Google Scholar]


