Abstract
Background: Hypertension is a major public health concern and, as the population ages, the size of the problem is likely to increase. However, detection rates and treatment of hypertension have been low. The introduction of new guidelines for the detection and treatment of hypertension have been encouraged but without any consideration to their cost-effectiveness.
Aim: To assess the potential cost-effectiveness of implementing new guidelines for the treatment of hypertension in general practice.
Design of study: Model examining the incremental costs and effects of the new guidelines compared with the old.
Setting: A large general practice in north Yorkshire.
Method: Two thousand and twenty-three patients reporting for a new health patient check had the costs and outcomes under the old and new guidelines estimated.
Results: Implementing new guidelines for the detection, management, and treatment of hypertension in a primary care setting is more costly than the implementation of previous guidelines, but more effective in reducing the risk of cardiovascular disease. The incremental cost per cardiovascular disease event avoided is £30 000, although sensitivity analysis shows that the estimate is subject to considerable uncertainty.
Conclusions: Compared with previous guidelines, introducing new guidelines for the management and treatment of hypertension in new patients in general practice is likely to be cost-effective. However, the workforce implications for general practitioners (GPs) and practice nurses should be considered.
Keywords: cost-effectiveness, guidelines, hypertension
Introduction
HYPERTENSION is a major risk factor in cardiovascular disease (CVD) and a main cause of death in older people. It also has a strong association with the occurrence of stroke.1
It has been estimated that in the United Kingdom (UK) over half of the 10 million people over the age of 65 years have hypertension.2 Where hypertension is defined as either taking hypertensive medication and/or having systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg, of all adults in England, the prevalence of hypertension was, in 2002, 37.4% among men and 33.8% among women.3
Hypertension is a major public health concern and, as the population ages, the size of the problem is likely to increase. However, detection rates and treatment of hypertension have been low.4 General practitioners (GPs) have been reluctant to adhere to guidelines for the treatment of hypertension5 partly because of the costs incurred by the practice from treating the majority of its older patients.6
Antihypertensive drug treatments are effective in reducing mortality from stroke, CVD, and overall mortality7,12 and morbidity in older people. The cost-effectiveness of drug therapy has not been proven in the UK, although a recent publication suggests that the lower-cost antihypertensive drugs, such as generic diuretics and ß-blockers, are likely to prove cost-effective for the older patient.1
National guidelines13 from the British Hypertension Society recommend reducing the levels at which a patient is considered to be hypertensive, thereby increasing the number of patients diagnosed and treated for hypertension. These guidelines (Table 1) also suggest that diastolic and systolic readings should be regarded as equally important; previously the emphasis was on the diastolic reading. They also suggest that those patients who record readings of ≥135/85 should be monitored on a regular basis (weekly, monthly, or annually depending on the level of the reading), and that people in Britain aged between 16 and 18 years should be screened at least once every 5 years.
Table 1.
A comparison of the old and new guidelines for the detection and treatment of hypertension (based on Ramsey et al13).
| New guidelines | ||
|---|---|---|
| Group | Definition | Treatment |
| N5 | SBP = >200 mmHg or DBP = >110 mmHg | Drugs |
| N4 | SBP = 160–199 mmHg or DBP = 100–109 mmHg | Drugs |
| N3(ii) | SBP = 140–159 mmHg or DBP = 90–99 mmHg; and clinical reason for screen or a high 10-year risk of CHD | Drugs |
| N3(i) | SBP = 140–159 mmHg or DBP= 90–99 mmHg; and no clinical reason for screen and a low 10-year risk of CHD | Monitoring |
| N2 | SBP = 135–139 mmHg or DBP = 85–89 mmHg | Monitoring (frequency depending on reading) |
| N1 | SBP = <135 mmHg and DBP<85 mmHg | Reassessment in 5 years |
| Old guidelines | ||
|---|---|---|
| Group | Definition | Treatment |
| O4 | DBP = >100 mmHg | Drugs |
| O3(i) | DBP = 90–99 mmHg; and clinical reason for screen or a higher 10-year risk of CHD | Drugs |
| O3(ii) | DBP = 90–99 mmHg; and no clinical reason for screen and a low 10-year risk of CHD | Monitoring |
| O2 | SBP = >160 and aged over 60 years | Drugs |
| O1 | All other patients | No treatment |
SBP = systolic blood pressure; DBP = diastolic blood pressure; CHD = coronary heart disease.
Although studies of implementation have become increasingly popular, little attention has been paid to the economics of implementation.14 Increasing the treatment and monitoring of hypertensive patients could substantially reduce the morbidity and mortality associated with hypertension and could also, therefore, generate overall cost savings for the National Health Service (NHS). However, the new guidelines could have serious resource implications, for example, with regard to GPs' and nurses' time, as well as additional medication, for the general practices that implement them. This article assesses the cost-effectiveness of guideline implementation for hypertension in a general practice setting, and examines the uncertainty around the costs and effectiveness. The cost estimates are also relevant for the design of incentives to encourage general practices to implement these new guidelines.15
HOW THIS FITS IN
What do we know?
New guidelines for the detection and treatment of hypertension have been introduced, which are likely to lead to a reduction in morbidity and mortality from cardiovascular disease (CVD).
What does this paper add?
The new guidelines could increase National Health Service (NHS) costs both in terms of increased workload for practice based staff and the cost of treating additional cases, although there may also be reductions in the costs of treating CVD events in future. Cost-effectiveness, as well as clinical effectiveness, of implementing new guidelines should be considered. Given the assumptions of this model, it is likely that the new guidelines for the management and treatment of hypertension represent a cost-effective use of resources.
Setting
The setting for this study comprised a large general practice in north Yorkshire, UK, with 16 GPs (approximately 10 whole-time equivalents (WTEs) and seven practice nurses (approximately 3.5 WTEs). The practice has a patient population of approximately 25 000 and is broadly representative of the north Yorkshire area in terms of the age/sex distribution and the majority of socioeconomic variables. The age/sex distribution of the sample is also broadly representative of the UK population. The practice has 3.9% of patients in Jarman band 1, with 2.0% in Jarman band 2; the remaining 94.1% did not qualify as deprived and, as such, there are no Jarman scores for this group.
Method
Outline
We took a sample of all new patients aged over 16 years who presented for a health check during the period when the old guidelines were in operation. Information on how the patients were treated under the old guidelines was obtained. It was then possible to estimate how the sample of patients presenting under the old guidelines would have been treated if the new guidelines, with lower threshold levels for triggering treatment, had been in effect.
We estimated both the practice resource implications and the effects of treatment on the risk of coronary heart disease and stroke under the old and new guidelines for each patient. Using the estimated effects and costs we calculated the cost-effectiveness of the new guidelines compared with the old, conducted sensitivity analysis, and estimated the value of better information.
The time horizon for these calculations was 1 year. Future costs and benefits beyond this period were discounted and annualised appropriately. To simplify the model, the potential side effects of treatments were not included.
Patient sample
The patient sample was made up of 2023 new adult patients (45.9% male, 54.1% female, with a mean age of 34 years) presenting for new patient health checks at the study practice in the 18 months prior to the introduction of new guidelines for hypertension (January 1998–July 1999). Patient level data were collected on age, sex, self-reported smoking status, systolic and diastolic blood pressure, clinical condition (if any), referrals, and prescribed medication for hypertension.
Assessment of risk of coronary heart disease and stroke
Data on individual patients were entered into the Cardiac Risk Assessor software, together with estimates of cholesterol levels derived from age and sex-specific mean cholesterol levels from the Health Survey for England.16 The software, which uses the Framingham risk equations, generated a 10-year risk from both coronary heart disease and stroke for each patient. This was converted into an annual rate to give for each patient an individually estimated yearly risk from coronary heart disease and stroke in the absence of treatment.
Estimates of effectiveness
The estimated effectiveness of drug treatment for coronary heart disease was based on a Cochrane Library review17 that reported a non-significant mean risk reduction of 0.03 (odds ratio). The effectiveness of preventative treatments for stroke in terms of mean risk reduction was estimated at 0.3 (odds ratio) in line with Collins et al's study.18 The latter estimate was subjected to extensive sensitivity analysis.
Resource use
Old and new guidelines differed in both the number of patients described as being at risk and the consequences of being at risk; for example, the new guidelines recommend increased monitoring of certain individuals.
The treatment options under the two sets of guidelines are described in Table 1, in which patient groups are defined in terms of their systolic and diastolic blood pressure readings, and level of coronary heart disease risk. Resource use was estimated by two GPs: one from within the practice, one from another practice. Unit costs were applied to resource use to estimate costs. Future costs were discounted at 6% in line with Department of Health recommendations;19 future effects were not discounted20 in the base case, although, in the sensitivity analysis, a 6% discount rate on future effects was considered. A separate sensitivity analysis using a 3.5% discount rate on costs was also conducted.
In the base case, patients with low blood pressure readings (N1, systolic blood pressure <135 mmHg and diastolic blood pressure <85 mmHg) were assumed to be reassessed in 5 years; higher levels required monitoring or treatment. In the base case estimate, patients who were assessed as requiring monitoring were assigned a cost equivalent to two nurse appointments and one GP appointment in a 12-month period, plus a blood and (surgery-based) urine test. Those who required treatment (N3i) under the new guidelines were costed with a daily dose of 50 mg atenolol, 2.5 mg bendrafluazide, plus three nurse and three GP consultations throughout the year.
Estimation of cost-effectiveness
Using the estimates of cost and effect per year under the old and new guidelines for the 2023 patients, a mean cost and a mean effectiveness for the old and new guidelines were calculated. The mean additional costs of implementing the new guidelines were divided by the mean additional effects in terms of coronary heart disease and strokes avoided to yield an incremental cost-effectiveness ratio (ICER) or cost per case of CVD avoided.
An expected net benefit from the new guidelines, compared with the old guidelines, was also calculated by applying a monetary valuation to each case of CVD avoided. With λ as the value in pounds sterling that a decision maker would be willing to pay to avoid a case of CVD, the incremental net benefit (INB), that is, the additional benefit derived from introducing the new guideline, is highlighted by the following formula:
INB = λ × (CVD avoided under new guidelines − CVD avoided under old guidelines) − (cost under new guidelines − cost under old guidelines)
As the costs incurred only by the practice are measured, λ includes both the monetary value of any health gain and any net cost saving elsewhere in the NHS or to the patient.
Allowing for uncertainty
Sensitivity analysis. As unit cost and effectiveness data were derived from the literature, and resource use data were estimated from expert opinion as well as patient records, extensive sensitivity analysis was performed. This process involved varying the resources used in monitoring and treating hypertension as well as the estimate of the effectiveness of preventative treatments for stroke.
Statistical analysis
Two-tailed paired t-tests (because the same patients were considered) were applied to the differences in costs and effects under the new and old guidelines. Confidence intervals (CIs) of 95% were calculated around the mean difference in costs and effects on the observed data under the new guidelines.
‘Bootstrapping’,21 a technique used to estimate standard errors and other methods of statistical precision, was also used to generate a distribution of mean costs and cases of CVDs avoided. A replicated sample was generated from the actual patient sample by making 2023 random draws, with replacement. The mean cost and cases of CVDs avoided were calculated for the replicated sample. The replication procedure was repeated 10 000 times.
The resulting joint distribution of mean costs and cases of CVDs avoided was then used to calculate the probability that the INB was positive for a specified value of λ (in this instance, the cost of an avoided cases of CVD). As the specified value of λ is increased, the probability that the INB is positive also increases. The relationship between λ and the probability that the INB is positive was then plotted as the cost-effectiveness acceptability curve.22 The cost-effectiveness acceptability curve is a graphical representation of the probability of an intervention being cost-effective over a range of monetary values for a decision maker's willingness to pay for an additional unit of health gain; in this instance the avoidance of CVD events.
Results
Unit cost estimates
The unit cost estimates that were applied to the resource use estimates described previously are presented in Table 2.
Table 2.
Unit cost estimates (1998–1999 prices).
| Resource | Unit cost (£ sterling) | Source |
|---|---|---|
| Cost of GP consultation | 13 | PSSRUa 200025 |
| Cost of nurse consultation | 7.58 | PSSRU 200025 |
| Cost of blood test | 3.90 | York Health Services Trust 199926 |
| Cost of urine test | 0.17 | York Health Services Trust 199926 |
| Cost of 50 mg atenolol | 0.06 | British National Formulary27 |
| Cost of bendrafluazide 5 mg | 0.03 | British National Formulary27 |
| Cost of simvastatin 20–40 mg | 1.06 | British National Formulary27 |
| Cost of cardiology outpatient visit | 66.59 | Department of Health28 |
| Costs of coronary heart disease | 1230 | Department of Health28 |
| Cost of stroke | 2080 | Department of Health28 |
aPersonal Social Services Research Unit.
Costs and effects
Using the old guidelines, 90.4% of patients would have received no treatment, 5.5% would have been ‘observed,’ and 4.1% would have received medication for hypertension. Under the new guidelines, no immediate action would have been taken for 77.3% of patients, but they would be reassessed in 5 years, 3.8% would be reassessed in 1 year, 13.4% would have been observed, and 5.5% would have been prescribed hypertensive medication.
Table 3 shows the costs and effects (per new patient) under both sets of guidelines and are presented for the base case analysis. The base case estimate had a significantly higher cost under the new guidelines compared with the old guidelines (£22.38 compared with £11.20, P<0.001), as well as a significantly reduced risk of CVD per annum (3.496 × 10−3, compared with 3.864 × 10−3, P<0.001). The ICER for the base case is £30 384 per case of CVD avoided.
Table 3.
Total cost and effectiveness of the detection and treatment of hypertension under the new and old guidelines.
| Old guidelines | New guidelines | Mean difference (95% CI) | Incremental cost-effectiveness ratio in £ sterling | |
|---|---|---|---|---|
| Base case (total costs in £ sterling) | 11.20 | 22.38 | 11.18 (10.69 to 11.67) | |
| Cardiovascular disease risk | 3.864 × 10−3 | 3.496 × 10−3 | 3.68 × 10−4 (3.24 to 4.12 × 10−4) | 30 384 |
| 6% discount rate on effects (total costs in £ sterling) | 11.20 | 22.38 | 11.18 (10.69 to 11.67) | |
| Cardiovascular disease risk | 2.932 × 10−3 | 2.653 × 10−3 | 2.79 × 10−4 (2.45 to 3.12 × 10−4) | 40 043 |
| Higher resource use under new guidelines (total costs in £ sterling) | 11.20 | 29.77 | 18.57 (14.20 to 24.70) | |
| Cardiovascular disease risk | 3.864 × 10−3 | 3.496 × 10−3 | 3.68 × 10−4 (3.24 to 4.12 × 10−4) | 50 454 |
| Lower effect of new guidelines (total costs in £ sterling) | 11.20 | 22.38 | 11.18 (10.69 to 11.67) | |
| Cardiovascular disease risk | 3.677 × 10−3 | 3.496 × 10−3 | 1.81 × 10−4 (1.60 to 2.08 × 10−4) | 61 775 |
Sensitivity analyses
Table 3 also reports estimated costs and effects under alternative assumptions. Lower and higher estimates of drug treatment and monitoring were assumed for patients assessed as having high blood pressure readings, or moderately high readings coupled with other risk factors, such as organ damage (N3, N4, N5). The lower estimate consisted of treatment with one drug (50 mg atenolol daily) plus two GP and two nurse consultations in the year. The higher estimate included treatment with three drugs (50 mg atenolol, 5 mg bendrafluazide, and 20 mg simvastatin), six appointments with the nurse and six with the GP, together with an outpatient appointment at a cardiology clinic. These are felt to reflect the extremes likely to occur in practice. The incremental cost per case of CVD avoided varies between £29 156 for low resource use (and base case measures of effectiveness) and £50 454 for the higher levels of resource use.
In the base case analysis, a discount rate was applied to the costs but not to the benefits. We investigated the impact of applying a discount rate of 6% to the measure of effectiveness; using this resulted in a reduced differential effectiveness and, therefore, an increase in the ICER to £40 043 per case of CVD avoided. Using a discount rate of 3.5% on costs only, resulted in an ICER of £36 280 per case of CVD avoided.
If trials overstate the effectiveness of interventions, the cost-effectiveness will also be overstated. Varying the effectiveness of preventative treatments for stroke from a risk reduction to 0.3 (odds ratio) of initial risk to 0.1 results in an increase in the incremental cost per case of CVD avoided of £61 775 for the new guidelines. Conducting two-way sensitivity so that the lower level of effectiveness and the higher levels of resource use are employed (that is, both favouring the use of existing guidelines) resulted in an incremental cost per case of CVD avoided of £97 056 associated with the new guidelines.
Incremental net benefit
The probability of the new guidelines being cost-effective depends on the value placed on the avoidance of CVD events. Figure 1 shows the cost-effectiveness acceptability curve associated with the implementation of new guidelines. It can be seen that at low values of willingness to pay to avoid CVD events, it is less likely that the new guidelines are better than the old. The reason is that the new guidelines have higher costs but also avoid more cases of CVD. In this instance, new guidelines are more likely to be of a higher net benefit when the societal willingness to pay to avoid a CVD event exceeds £30 000; below this value, the old guidelines are more likely to be cost-effective.
Figure 1.
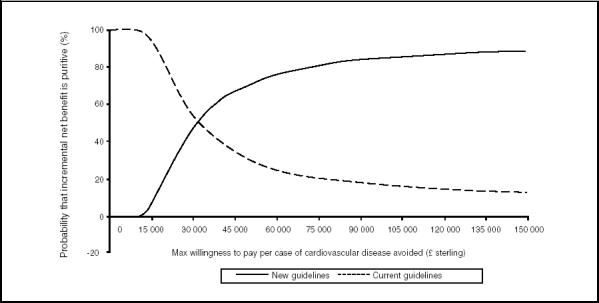
Cost-effectiveness acceptability curve showing probability that incremental net benefit of new versus old guidelines is positive.
Discussion
Summary of main findings
The main conclusion of this analysis is that the implementation of new guidelines is likely to be cost-effective at a willingness to pay £30 000 per CVD event avoided, although there is considerable uncertainty around the estimates. It is important to include an assessment of cost-effectiveness before guidelines are implemented, as efficiency considerations may alter the recommendations.
Limitations of the study
This approach considers the cost-effectiveness of implementing new guidelines for the identification, management, and treatment of hypertension of all new adult patients presenting at general practices. This may influence the generalisability of the study, as may the large practice size; although the population sample was demographically similar to other practice populations in north Yorkshire, large practices are able to operate differently to their small counterparts because of the differences regarding economies of scale and scope. To simplify the analysis, a limited time period was also considered; however, it is unlikely that a change in this factor would impact on the results of the cost-effectiveness analysis.
The model is based on data derived from the Framingham work. These data, as well as some of the other estimates used in the model, are now somewhat dated, a factor that may influence these results. Additionally, if the consequences of hypertension (in terms of CVD events) is overstated, then the positive results derived from implementing these guidelines are also likely to be overstated.
The sample is unusual in that the patients were all new, rather than existing, patients who attended the general practice surgery. In addition, the costs and effects, although estimated over a 10-year period, are reduced to annual risks; this is likely to underestimate the risk of events, as the risk of events is not linear but increases with age. This sample and time period were chosen because of the difficulty of modelling the impact of changing guidelines.
Existing literature
These estimates of the cost-effectiveness of implementing new guidelines for hypertension compare favourably with other estimates of avoidance of coronary and cardiovasc-ular events. Haq et al23 estimated an ICER of between £35 000 and £111 000 per coronary event saved (1995 prices) by targeting those with serum cholesterol of >5.5 mmol/l.
If the value of avoiding a case of CVD (including coronary heart disease and stroke) exceeds £30 000, the new guidelines for hypertension have a higher probability of being cost-effective than the old guidelines. Is £30 000 per CVD event avoided a price worth paying? The answer depends crucially on the type of CVD, together with life expectancy and quality of life after the event. Using estimates from Hartunian et al,24 approximately 38.6% of coronary events in 55-year-old males result in death. If it is also assumed that life expectancy in those who survive is 5 years, a figure of approximately £15 000 per life year gained is generated (£30 000/[5 × 0.386]).
Clearly, these are crude estimates, with the percentage of deaths from coronary heart disease likely to be an overestimation for a general population, but this is countered by the likely underestimation of 5 years of life expectancy in those who survive. In addition, the new guidelines also reduce risk of stroke as well as coronary heart disease, resulting in the cost of £15 000 per life year gained being lowered. There may also be cost savings elsewhere in the NHS systems that have not been considered in this analysis. All these factors are likely to increase the value of a case of CVD avoided to above £30 000, thus increasing the likelihood that implementation of the new guidelines would be cost-effective.
The finding that implementing new guidelines for the treatment of hypertension in a general practice setting is likely to be cost-effective has obvious implications for practices. Although it may be suggested that adherence to these guidelines is desirable, the model does not consider the implications for personnel and staffing levels within general practices. It is feasible that this approach would create a greater workload for practices that may be difficult to maintain without more training for existing staff or the hiring of additional personnel. The analysis assumes that hiring additional personnel is possible without affecting the labour market for these individuals and hence their unit cost.
The greatest burden of implementing these guidelines will clearly fall on the practices themselves, as the cost of performing a new patient health check will be increased. This disincentive should be considered when devising quality targets for GPs as under the new contract and setting the level of the fee for new patient health checks.
Implications for future research
Future research efforts should assess the cost-effectiveness of implementing guidelines before implementation. In the area of hypertension treatment guidelines, improved estimates of the long-term effectiveness of treatment would reduce the uncertainty surrounding the estimates of cost-effectiveness.
Acknowledgments
The study was partly funded by the Priory Medical Group, York. The National Primary Care Research and Development Centre (NPCRDC), University of Manchester receives funding from the Department of Health. The views expressed are not necessarily those of the funders. We are grateful to Liz Fenwick for help and advice.
References
- 1.NHS Centre for Reviews and Dissemination. Drug treatment of essential hypertension in older people. Effectiveness Matters. 1999;2(4) http://www.york.ac.uk/inst/crd/em.htm (accessed 22 Jul 2004) [Google Scholar]
- 2.Colhoun HM, Dong W, Poulter NR. Blood pressure screening, management and control in England: results from the health survey for England 1994. J Hypertens. 1998;16(6):747–752. doi: 10.1097/00004872-199816060-00005. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health. Health Survey for England 2002. London: Stationary Office; 2002. http://www.publications.doh.gov.uk/stats/tables/adults2002tab3a.xls (accessed 6 Sep 2004) [Google Scholar]
- 4.Salvetti A, Versari D. Control of blood pressure in the community: an unsolved problem. Curr Pharm Des. 2003;9(29):2385–2402. doi: 10.2174/1381612033453848. [DOI] [PubMed] [Google Scholar]
- 5.Fahey T, Silagy C. General practitioners' knowledge of and attitudes to the management of hypertension in elderly patients. Br J Gen Pract. 1994;44(387):446–449. [PMC free article] [PubMed] [Google Scholar]
- 6.Hart JT. Rule of halves: implications of increasing diagnosis and reducing dropout for future workload and prescribing costs in primary care. Br J Gen Pract. 1992;42(356):116–119. [PMC free article] [PubMed] [Google Scholar]
- 7.Mulrow C, Lau J, Cornell J, et al. The Cochrane Library. Issue 4. Oxford: Update Software; 2001. Pharmacotherapy for hypertension in the elderly. Cochrane Collaboration. http://www.mediscope.ch/cochrane-abstracts/ab000028.htm (accessed 6 Sep 2004) [DOI] [PubMed] [Google Scholar]
- 8.Mulrow CD, Cornell JA, Herrera CR, et al. Hypertension in the elderly. Implications and generalisability of randomised trials. JAMA. 1994;272(24):1932–1938. [PubMed] [Google Scholar]
- 9.Insua JT, Sacks HS, Lau TS, et al. Drug treatment of hypertension in the elderly: a meta-analysis. Ann Intern Med. 1994;121(5):355–362. doi: 10.7326/0003-4819-121-5-199409010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Pearce KA, Furberg CD, Rushing J. Does antihypertensive threatment of the elderly prevent cardiovascular events or prolong life? A meta-analysis of hypertension treatment trials. Arch Fam Med. 1995;4(11):943–949. doi: 10.1001/archfami.4.11.943. [DOI] [PubMed] [Google Scholar]
- 11.Thijs L, Fagard R, Lijnen P, et al. A meta-analysis of outcome trials in elderly hypertensives. J Hypertens. 1992;10(10):1103–1109. doi: 10.1097/00004872-199210000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Lievre M, Leizorovicz A. Treatment of high blood pressure in patients aged over 60 years: lessons from randomized clinical trials. Cardiol Elderly. 1995;3(3):217–222. [Google Scholar]
- 13.Ramsay LE, Williams B, Johnston GD, et al. British Hypertension Society guidelines for hypertension management 1999: summary. BMJ. 1999 Sep 4;319(7210):630–635. doi: 10.1136/bmj.319.7210.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mason J, Eccles M, Freemantle N, Drummond M. NICEly does it: economic analysis within evidence based clinical guidelines. Centre for Health Economics (CHE) Discussion paper 164, York: CHE; 1998. Dec, http://www.york.ac.uk/inst/che/DP164.pdf (accessed 21 Jul 2004) [Google Scholar]
- 15.NHS Confederation News Releases. New GMS contract will reward family doctors for higher quality services. 2003. Feb 21, www.nhsconfed.org/press/releases/walesgms.asp?kh=%22new%2BGMS%2Bcontract%2Breward%2Bfamily%2Bdoctors%2Bhigher%2Bquality%2Bservices%22&smode=or (accessed 21 July 2004)
- 16.Department of Health. Health Survey for England. London: Department of Health; 1998. [Google Scholar]
- 17.Ebrahim S, Davey-Smith G Cochrane Collaboration. Cochrane Library. Issue 2. Oxford: Update Software; 2000. Multiple risk factor interventions for primary prevention of coronary heart disease. CD001561. [DOI] [PubMed] [Google Scholar]
- 18.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990 Apr 7;335(8693):827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 19.Department of Health. Discount rates and the cost of capital. London: Department of Health; 1997. (EL (97)71.) [Google Scholar]
- 20.Gravelle H, Smith D. Discounting for health effects in cost benefit and cost-effectiveness analysis. Health Econ. 2001;10(7):587–599. doi: 10.1002/hec.618. [DOI] [PubMed] [Google Scholar]
- 21.Efron B, Tibishirani RJ. An introduction to the bootstrap. New York: Chapman and Hall; 1994. [Google Scholar]
- 22.Fenwick E, Claxton K, Sculpher M, Briggs A. Improving the efficiency and relevance of health technology assessment: The role of iterative decision analytic modelling. 2001. p. 179. Centre for Health Economics Discussion paper.
- 23.Haq IU, Yeo WW, Jackson PR, Ramsay LE. Should cholesterol be measured in all hypertensives? J Hum Hypertens. 1995 Jun;9(6):417–421. [PubMed] [Google Scholar]
- 24.Hartunian NS. The incidence and economic costs of major health impairments: a comparative analysis of cancer, motor vehicle injuries, coronary heart disease, and stroke. Lexington: Lexington Books; 1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Netten A, Curtis L. Unit costs of health and social care 2000. Canterbury: Personal Social Services Research Unit, University of Kent; 2000. [Google Scholar]
- 26.York Health Services Trust. GP Fundholders Tariff. York: York Health Services Trust; 1999. [Google Scholar]
- 27.British National Formulary. London: British Medical Association and the Royal Pharmaceutical Society of Great Britain; 1999. [Google Scholar]
- 28.Department of Health. NHS Reference Costs. London: Department of Health; 2000. [Google Scholar]


