Abstract
Background: The pelvic floor muscles are active in normal erectile function. Therefore, it was hypothesised that weak pelvic floor muscles could be a cause of erectile dysfunction.
Aims: To compare the efficacy of pelvic floor muscle exercises and manometric biofeedback with lifestyle changes for men with erectile dysfunction.
Design of study: Randomised controlled trial.
Setting: The Somerset Nuffield Hospital, Taunton, United Kingdom.
Method: Fifty-five men with erectile dysfunction (median age 59.2 years; range 22–78 years) were enrolled from a local urology clinic. Of these, 28 participants were randomised to an intervention group and engaged in pelvic floor exercises, as well as receiving biofeedback and suggestions for lifestyle changes. Twenty-seven controls were solely advised on lifestyle changes. Baseline, 3- and 6-month assessments were: erectile function domain of International Index of Erectile Function (IIEF), Partner's International Index of Erectile Function (PIIEF), Erectile Dysfunction-Effect on Quality of Life (ED-EQoL), anal manometry, digital anal measurements, and clinical assessment by an assessor blind to treatment allocation. After 3 months, the control group were transferred to the active arm.
Results: At 3 months, compared with controls, men in the intervention group showed significant mean increases in the erectile function domain of the IIEF (6.74 points, P = 0.004); anal pressure (44.16 cmH2O, P<0.001); and digital anal grades (1.5 grades, P<0.001). All showed further improvement in these outcomes at 6 months. Similar benefits were seen in men of the control arm after transfer to active treatment. A total of 22 (40.0%) participants attained normal function, 19 (34.5%) participants had improved erectile function, and 14 (25.5%) participants failed to improve.
Conclusion: Pelvic floor muscle exercises and biofeedback are an effective treatment for men with erectile dysfunction.
Keywords: pelvic floor exercises, biofeedback, erectile dysfunction
Introduction
ERECTILE dysfunction was defined by a National Institute of Health (NIH) Consensus Development Panel as ‘the inability to achieve or maintain an erection sufficient for satisfactory sexual performance’ (for both partners).1 The exact prevalence of erectile dysfunction is unknown, although it is a common problem that may affect 10% of healthy men and significantly greater numbers of men with existing comorbidities such as hypertension (15%), diabetes (28%), and heart disease (39%).2,3 Men with erectile dysfunction may suffer from depression and low self-esteem, and experience difficulties establishing and maintaining relationships.4,5
Treatment regimens currently available for erectile dysfunction include psychotherapy, sex therapy, oral pharmacological agents, androgen replacement therapy, intraurethral therapy, intracavernosal injections, vacuum devices, and surgery. The pelvic floor muscles play a role in sexual activity. Contractions of the ischiocavernosus and bulbocavernosus muscles produce an increase in the intracavernous pressure and influence penile rigidity. The bulbocavernosus muscle compresses the deep dorsal vein of the penis to prevent the outflow of blood from an engorged penis.
Previous studies using pelvic floor muscle exercises for erectile dysfunction have been unrandomised or uncontrolled.6-11 We carried out the first randomised controlled trial to examine the effect of pelvic floor muscle exercises enhanced by manometric biofeedback for men with erectile dysfunction.
Method
Power calculation
A power calculation could not be performed as there were no data from similar studies using pelvic floor exercises. Data from this trial could be used to provide a power calculation for future larger studies.
Ethics approval
Approval was obtained from the West Somerset Local Research Ethics Committee and the University of the West of England Ethics Committee.
Sample
Men aged 20 years and over who had experienced erectile dysfunction for 6 months or more were referred to the physiotherapy department of The Somerset Nuffield Hospital for treatment by a consultant urologist. Those men with urological congenital abnormalities, neurological deficits, and previous urological surgery were excluded from the trial. However, men having undergone transurethral resection of prostate were included as it was considered that they would not have neurological impairment. The trial ran from June 2000 to April 2002.
HOW THIS FITS IN
What do we know?
There is a wide range of treatments for erectile dysfunction. Pelvic floor muscle exercises are not routinely used to treat erectile dysfunction and they have not been the subject of a randomised controlled trial.
What does this paper add?
Pelvic floor muscle exercises are effective in treating men with erectile dysfunction, and should be the first-line approach to treat the problem. They may be used in conjunction with other treatments for erectile dysfunction.
Randomisation and recruitment
A system of random odd- or even-numbered tickets in sealed envelopes for participant selection was used to randomise patients into either the intervention or the control group. Men selected and opened their sealed envelope from a box containing 150 sealed envelopes. Those who selected tickets with even numbers were placed in the intervention group. The sample consisted of 55 men who fulfilled the inclusion criteria and were enrolled into the trial. Table 1 shows baseline characteristics for both groups.
Table 1.
Description of subjects at baseline.
| Intervention group median (range) | Control group median (range) | |
|---|---|---|
| Number of subjects randomised | 28 | 27 |
| Age in years | 58 (22–78) | 61 (41–72) |
| Months with erectile dysfunction | 24 (6–360) | 54 (6–360) |
| Body mass index | 26 (21–42) | 29 (22–38) |
| Erectile function domain of International Index of Erectile Function score | 7.5 (1–28) | 7.0 (1–17) |
Intervention
The flow of participants through the study is shown in Figure 1. All participants underwent a full subjective and objective clinical assessment by the researcher, who is an experienced physiotherapist. The objective examination was conducted in supine position with knees bent and feet on the couch. An assessment was made of puborectalis muscle strength and the length of hold of the contraction in seconds by digital anal examination graded 0 (nil) to 5 (strong).12
Figure 1.
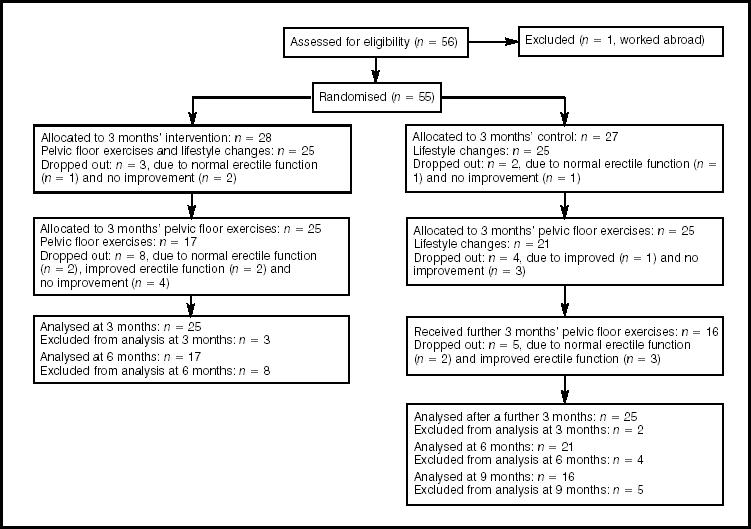
Algorithm of randomised controlled trial.
A further assessment was performed using anal manometry to test muscle strength; each participant was positioned supine as before, and with a view of the computer screen for feedback. The air-filled, sheathed and lubricated anal probe, with a diameter of 1 cm, was inserted into the anal canal as far as the probe external position marker (to a depth of 4 cm) in order to approximate to the puborectalis muscle. Participants were instructed to voluntarily tighten and lift the pelvic floor muscles as strongly as possible as if preventing the flow of urine, and to hold this contraction for 10 seconds. A scrotal lift and penile retraction was confirmed to ascertain that the pelvic floor muscles were contracting correctly. The maximum anal pressure reading achieved from the best of three pelvic floor muscle contractions (maximum anal pressure) and the lowest pressure obtained while attempting to maintain a 10-second hold (anal hold pressure) were recorded in cmH2O. A rest of 10 seconds was given between each contraction.
Men in the intervention group were educated about the mechanics of the pelvic floor musculature and individually taught specific pelvic floor muscle exercises enhanced with manometric biofeedback for strength and endurance. The exercise programme (Box 1) included occasionally lifting the pelvic floor muscles 50% of maximum while walking, and a post-void ‘squeeze out’ pelvic floor muscle contraction.13 These treatments were given in five 30-minute periods in consecutive weeks and included advice on lifestyle changes concerning smoking, alcohol intake, general fitness, a healthy diet, weight reduction, and saddle pressure. Each participant in the intervention group was given a list of pelvic floor muscle exercises to perform at home daily for 6 months.
Box 1. Pelvic floor muscle exercises for men.
-
In standing position
Stand with your feet apart and tighten your pelvic floor muscles as if you were trying to stop the flow of urine and wind escaping. If you look in a mirror, you should be able to see the base of your penis move nearer to your abdomen and your testicles rise.
Hold the contraction as strongly as you can.
Try to avoid holding your breath, pulling in your abdomen or tensing your buttocks.
Perform 3 maximal contractions in standing in the morning holding for __ seconds.
Perform 3 maximal contractions in standing in the evening holding for __ seconds.
-
In sitting position
Sit on a chair with your knees apart and tighten your pelvic floor muscles as if you were lifting your pelvic floor but not your buttocks off the chair.
Hold the contraction as strongly as you can.
Try to avoid holding your breath, pulling in your abdomen or tensing your buttocks.
Perform 3 maximal contractions in sitting in the morning holding for ___ seconds.
Perform 3 maximal contractions in sitting in the evening holding for ___ seconds.
-
In lying position
Lie on your back with your knees bent and your knees apart. Tighten your pelvic floor and hold the contraction as strongly as you can.
Try to avoid pulling in your abdomen or tensing your buttocks.
Perform 3 maximal contractions in lying in the morning holding for __ seconds.
Perform 3 maximal contractions in lying in the evening holding for __ seconds.
-
While walking
Try lifting your pelvic floor up 50% of maximum when walking.
-
After urinating
After you have voided urine, try tightening your pelvic floor muscles strongly to avoid the after-dribble.
-
During sexual activity
Try tightening your pelvic floor muscles rhythmically to achieve and maintain penile rigidity during sexual activity. Slow thrusting movements generate higher pressures inside the penis.
-
To delay ejaculation
For men with premature ejaculation, try tightening your pelvic floor muscles to delay ejaculation.
Men in the control group were given advice on lifestyle changes only, in five 30-minute periods in consecutive weeks. Following assessment of outcomes at 3 months, these men were offered the intervention as described above.
Outcome measures
The primary outcome measure was the validated erectile function domain of the International Index of Erectile Function (IIEF),14 which was self-completed at baseline, 3 months, and 6 months. There were six questions relating to erectile function in this domain (for example, ‘Over the past 4 weeks, how often were you able to get an erection during sexual activity?’), and each ranked 0–5 points:
5 = almost always or always,
4 = most times (much more than half the time),
3 = sometimes (about half the time),
2 = a few times (much less than half the time), and
1 = almost never or never, and
0 = no sexual activity.
It has been suggested that an increase in six points in this domain indicates a clinical improvement.15
Secondary outcome measures were the self-completed validated Erectile Dysfunction-Effect on Quality of Life (ED-EQoL),16 which addresses men's feelings concerning their erectile difficulties; digital anal measurements; anal manometric measurements; and assessments by a urologist blind to treatment allocation, to whom participants reported erectile function status (worse, same, improved, cured).
All men were requested to ask if their partner would like to complete the Partner's IIEF (PIIEF) in confidence and unaided.
Data analysis
All analyses were conducted using SPSS. The main analyses were based on analysis of covariance examining the difference between the two trial groups on each clinical outcome measure at 3 months, while controlling for baseline value of that same measure. Where parametric analyses were inappropriate (for example, for manometry measurements and digital anal grades), Mann–Whitney tests were conducted comparing the changes from baseline to 3-month follow-up between the two groups. The data from the assessor blind to treatment allocation was on an intention-to-treat basis to include those who dropped out from the trial.
Results
In total, 28 participants were randomised into the intervention group and 27 into the control group. Data at 3 months were available on 25 subjects in each group.
Erectile function
At 3 months, the intervention group scored significantly better than the control group on the primary outcome measure of erectile function, as assessed by the relevant domain of the IIEF (Table 2). All other domains showed weak benefit for the intervention group. The sexual desire domain (libido) remained constant for both groups.
Table 2.
International Index of Erectile Function domain scores in subjects and partners at 3-month follow-up.
| Intervention group mean (SD) | Control group (mean SD) | Corrected difference(95% CI)a | P-valuea | |
|---|---|---|---|---|
| Sample size for analysis | ||||
| Subjects | 25 | 25 | - | - |
| Partners | 17 | 22 | - | - |
| Erectile function | ||||
| Subjects | 17.2 (9.7) | 8.4 (7.3) | 7.0 (2.4 to 11.6) | 0.004 |
| Partners | 17.4 (10.7) | 10.0 (9.6) | 6.9 (1.1 to 12.8) | 0.02 |
| Intercourse satisfaction | ||||
| Subjects | 7.8 (3.9) | 4.6 (4.3) | 2.6 (0.5 to 4.7) | 0.02 |
| Partners | 7.9 (4.3) | 4.5 (4.5) | 3.3 (0.7 to 6.0) | 0.02 |
| Orgasmic function | ||||
| Subjects | 6.7 (3.3) | 4.1 (3.7) | 2.2 (0.4 to 4.1) | 0.02 |
| Partners | 6.6 (3.9) | 4.1 (3.9) | 2.3 (-0.09 to 4.6) | 0.06 |
| Sexual desire | ||||
| Subjects | 6.2 (2.3) | 5.9 (2.1) | 0.4 (-0.5 to 1.4) | 0.38 |
| Partners | 7.1 (2.0) | 4.7 (2.5) | 1.7 (0.4 to 3.0) | 0.01 |
| Overall satisfaction | ||||
| Subjects | 6.1 (2.3) | 4.1 (2.5) | 1.8 (0.5 to 3.0) | 0.008 |
| Partners | 6.9 (5.2) | 4.2 (2.9) | 2.0 (-0.5 to 4.4) | 0.11 |
aDifference is intervention group minus control group, derived from ANCOVA. SD = standard deviation.
Of the participants' partners, 47 (85.5%) were willing to complete the PIIEF at baseline. However this was only completed by 39 partners. Mean scores for partners (PIIEF) were similar to those for the subjects (IIEF), and again showed advantage for the intervention group in most domains (Table 2).
Following assessment at 3 months, the improvement in erectile function was maintained over the following 3 months when intervention subjects were advised to continue with the home-based pelvic floor exercises. The control group also showed a similar response (and maintenance) when they underwent the active treatment arm (Figure 2).
Figure 2.
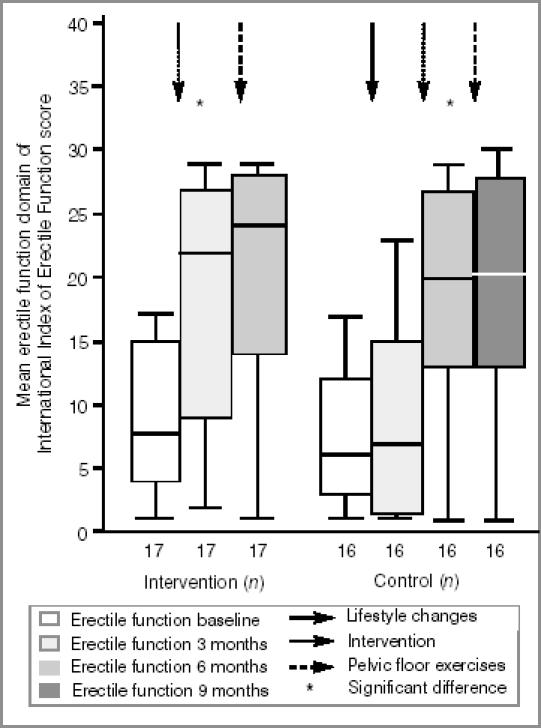
Mean erectile function domain of International Index of Erectile Function scores for both groups at each assessment.
Quality of life affected by erectile dysfunction (as measured by the ED-EQoL) improved slightly in both groups over the 3 months, more so in the intervention group but not significantly so (mean difference between groups estimated as ANCOVA 3.1, 95% confidence interval [CI] = -3.5 to 9.6, P = 0.35).
Manometry and digital anal measurements
The intervention group showed statistically significant improvements in manometric and digital anal measurements compared to the control group (Table 3). As with erectile function, these improvements were largely maintained over subsequent months, and the control group followed a similar pattern upon introduction of the intervention at 3 months (Figure 2). Participants in the intervention group who regained normal function attained anal pressure measurements of 100 cmH2O and above. However, four participants failed to achieve anal pressure measurements in excess of 85 cmH2O and showed no improvement. Anal manometric measurements were positively correlated with digital anal scales at baseline, 3 months, and 6 months (ρ>0.556, P=0.001) in both groups.
Table 3.
Manometric and digital anal measures at baseline and 3-month follow-up.a
| Outcome | Intervention group (n = 25) | Control group (n = 25) | P-valueb | ||
|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | ||
| Maximum anal pressure | 96 | 147 | 75 | 75 | <0.001 |
| Anal hold pressure | 85 | 130 | 70 | 69 | <0.001 |
| Digital anal measurements | 3 | 5 | 3 | 3 | <0.001 |
aAll values are medians
bMann–Whitney test comparing change in score between the two groups.
Withdrawals
Twenty-two (40%) participants did not remain in the trial for the intended duration; of these, six (10.9%) participants withdrew because they had achieved normal erectile function, and seven (12.7%) participants withdrew following improved erectile function. Nine (16.4%) participants withdrew showing no improvement. Participants who failed to improve reported possible reasons for this as testicular pain, severe low back pain, addiction to alcohol, saddle trauma, cardiac bypass surgery, cardiovascular problems, pacemaker, diabetes mellitus, Peyronie's disease, and bilateral orchidectomies with testosterone implants.
Blind assessment
The final analysis from the blind assessments of both groups combined, including those who withdrew from the trial, showed that a total of 22 (40.0%) participants attained normal function, 19 (34.5%) had improved erectile function, and 14 (25.5%) failed to improve.
Discussion
Summary of main findings
With a clinical improvement of 6.74 points on the erectile function domain of the IIEF, the intervention group showed a significant improvement (P = 0.004) in erectile function compared with the control group after 3 months. The control group showed no significant increase in erectile function following lifestyle changes (P = 0.658), but a highly significant increase following intervention at 6 months (P<0.001). At 6 months, there was clinical improvement of 9.88 points on the erectile function domain of the IIEF for the intervention group and 10.94 points for men initially assigned to the control group. There was, however, no further significant improvement with the pelvic floor exercises in either the intervention group (P = 0.108) or control group (P = 0.646). There was good correlation between the IIEF and the PIIEF. The ED-EQoL correlated poorly with the erectile function domain of the IIEF.
Manometric measurements and digital anal measurements showed that both groups improved significantly (P<0.001) after intervention. Further improvement after engaging in pelvic floor exercises was not significant.
After 3 months of intervention and 3 months of pelvic floor exercises, 40.0% of all participants had attained normal function, 34.5% had improved, and 25.5% failed to improve.
Strengths and limitations of this study
This was the first randomised controlled trial to use a validated outcome to measure the effectiveness of pelvic floor muscle exercises enhanced by manometric biofeedback. The anal pressure biofeedback displayed on a computer screen motivated the subjects to attain a pelvic floor muscle exercise contraction of maximum strength. The men worked hard to improve on previous readings. Results are in line with other non-randomised or uncontrolled trials using similar treatment modalities.7.9,10,17 Previously, pelvic floor exercises may not have been routinely given for erectile dysfunction following these non-randomised or uncontrolled trials due to their methodological limitations.
It was a limitation of the IIEF that it did not provide any specific information about the partner relationship or the non-erectile components of sexual response.14 It would be useful to have a tool that explored cultural, social, ethnic, and religious perspectives. Another perceived limitation was the use of the non-validated PIIEF; however, the inclusion of the PIIEF did involve partners in the research process and provided reinforcement to the accuracy of the IIEF responses by the subjects. A validated partner's questionnaire in this study may have indicated the different sexual and non-sexual needs of the partners, which could have been relayed to the men.
The study was limited by the small number of subjects. Further trials could be multicentred and thereby involve a larger sample size with an opportunity to investigate a more heterogeneous sample.
Comparison with existing literature
The blind assessment indicated that 40.0% of participants regained normal erectile function. These results were comparable to previous studies using pelvic floor muscle exercises which reported that 26–46% of men had regained normal function following a similar exercise regime.7,9,10,17
The number of participants who withdrew from the trial was a concern, although a high drop-out rate has been reported previously in this type of study18 and may reflect the embarrassment and unease suffered by this cohort of men or possibly the commitment involved in performing daily exercises. However, some of the men who withdrew from the study did so because they had achieved normal erectile function.
All participants who received the allocated intervention reported completion of their pelvic floor home exercise regime. All men were able to achieve a penile retraction and scrotal lift during training with pelvic floor muscle exercises, although, initially, this response was often difficult and slow. As muscle strength improved, this response was initiated at a faster rate. Examination of individual cases revealed the return of self-reported nocturnal erections following 1–4 weeks of pelvic floor muscle exercises and prior to regaining erectile function. Weak evidence showed that orgasmic and ejaculatory function also improved with pelvic floor muscle exercises. This improvement was not surprising as the bulbocavernosus muscle, which is strengthened by pelvic floor muscle exercises, pumps the ejaculate.19
The erectile function domain of the IIEF showed poor correlation with the ED-EQoL in both groups. These results were similar to the findings of MacDonagh et al,16 and demonstrated a clear reason for the clinical usefulness of the ED-EQoL to monitor men's feelings about their erectile difficulties. The quality of life of some men who experienced severe erectile function was unaffected by their lack of erectile function while others with less severe symptoms reported that their quality of life was severely negatively affected.
This was the first time that anal manometric measurements have been used as an outcome measure for pelvic floor muscle strength in men with erectile dysfunction. These measures have previously been shown to have good within-day and day-to-day intrarater reliability.20 Six participants who had low anal pressure measurements after intervention failed to achieve normal function, suggesting that weak pelvic floor muscles are a risk factor for erectile dysfunction.
In this trial the median age of the participants was 59.2 years and much higher than the subjects in all the other trials.7-9,17,21 The duration and severity of erectile dysfunction were not predictors of the results of therapy in this trial.
It was expected that the control group would show some improvement by reducing alcohol levels, quitting smoking, increasing fitness levels, losing weight, and avoiding saddle pressure. This did not seem to be the case. Although the majority of participants reduced alcohol levels, lost some weight, and performed daily exercises such as hill walking and running up and down stairs, no participant ceased smoking, and two participants remained addicted to alcohol. It may be that 3 months of lifestyle changes was too short a time to effect a reversal of symptoms.
Comparison with sildenafil. The results of this trial were compared with a large grade II trial using oral sildenafil for 329 participants with similar mixed aetiology.15 Both trials used the erectile function domain of the IIEF as the main outcome measure. In the sildenafil trial at 12 weeks, participants receiving up to 100 mg sildenafil based on efficacy and tolerance improved by 10 points to attain a score of 21 points (Figure 3). In our trial, participants in the intervention group improved at 3 months by eight points from the overall baseline score to attain a score of 17 points. An increase in six points was considered a clinical improvement as this indicated that the men moved up a category in each of the erectile function scores, for example, from ‘almost never’ to ‘a few times’, or from ‘sometimes’ to ‘most times’.
Figure 3.
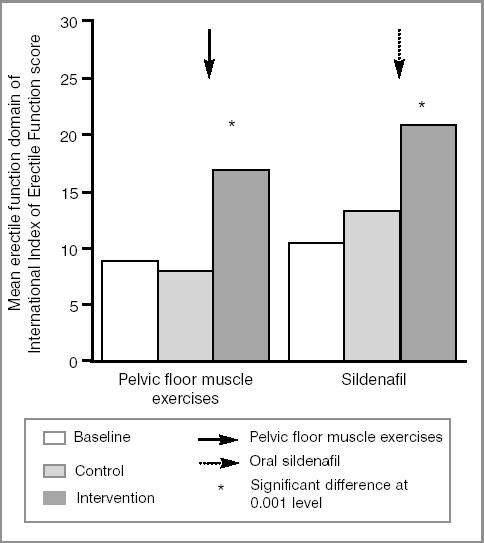
Comparison of pelvic floor muscle exercises in our trial and sildenafil15 at 3 months using the erectile function domain of the International Index of Erectile Function.
Implications for future research or clinical practice
Evidence has shown that pelvic floor muscle exercises are significantly effective for some men with erectile dysfunction. To obtain a benefit, pelvic floor muscle exercises should be properly taught and practised for at least 3 months. A maintenance programme may then be implemented for life.
Not all men with erectile dysfunction may be suitable for pelvic floor muscle training. Those men with severe arteriogenic and neurological causes may well not benefit. The results of this trial may have been more impressive if men with severe low back pain, addiction to alcohol, cardiovascular disease, diabetes mellitus, Peyronie's disease, and bilateral orchidectomies had been excluded in the first instance.
Pelvic floor muscle exercises could be considered as a first-line approach for men seeking resolution of erectile dysfunction without pharmacological and surgical interventions. Also, men receiving other forms of therapy for erectile dysfunction could be advised to practise pelvic floor muscle exercises in addition to the therapy prescribed. Although pelvic floor muscle exercises are more labour intensive than using a pharmacological agent, men could be given a choice of treatment. Some men may prefer a more natural approach. Figure 4 details a suggested management pathway for men with erectile dysfunction.
Figure 4.
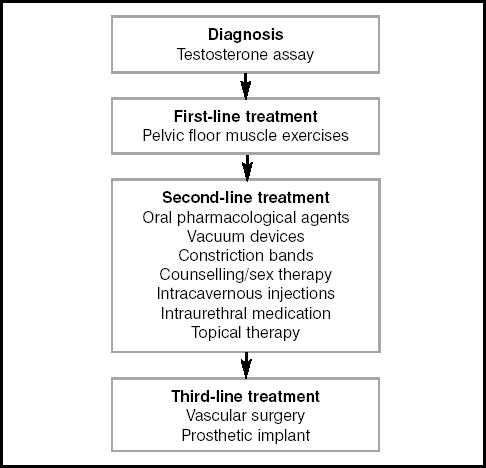
Suggested algorithm for treatment of erectile dysfunction.
Acknowledgments
We thank all the subjects who participated in the trial and The Somerset Nuffield Hospital, Taunton for their cooperation.
References
- 1.National Institutes of Health Consensus Development Panel on Impotence. Impotence. JAMA. 199;3(270):83–90. [Google Scholar]
- 2.Wagner TH, Patrick DL, McKenna SP, Froese PS. Cross-cultural development of a quality of life measure for men with erection difficulties. Qual Life Res. 1996;5(4):443–449. doi: 10.1007/BF00449919. [DOI] [PubMed] [Google Scholar]
- 3.Feldman HA, Goldstein I, Hatzichristou DG, et al. Impotence and its medical and psychological correlates: results of the Massachusetts Male Ageing Study. J Urol. 1994;151(1):54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 4.Hawton K. Integration of treatments for male erectile dysfunction. Lancet. 1998;351(9095):7–8. doi: 10.1016/S0140-6736(05)78097-1. [DOI] [PubMed] [Google Scholar]
- 5.Lording DW, McMahon CG, Conaglen JV, et al. Partners of affected men: attitudes to erectile dysfunction. Int J Imp Res; Proceedings of the 7th Biennial Asia-Pacific Meeting on Impotence October 26-30 1999 Tokyo, Japan; 2000. p. S16. [Google Scholar]
- 6.Schouman M, Lacroix P. Apport de la ré-éducation pelvi-périnéale au traitement des fuites veino-caverneuses. [Role of pelvic-perineal rehabilitation on the treatment of cavernous venous leakage.] Ann Urol (Paris) 1991;25(2):93–94. [PubMed] [Google Scholar]
- 7.Claes H, Baert L. Pelvic floor exercise versus surgery in the treatment of Impotence. Br J Urol. 1993;71(1):52–57. doi: 10.1111/j.1464-410x.1993.tb15880.x. [DOI] [PubMed] [Google Scholar]
- 8.Colpi GM, Negri L, Scroppo FI, Grugnetti C. Perineal floor rehabilitation: a new treatment for venogenic impotence. J Endocrin Invest. 1994;(17):334. [Google Scholar]
- 9.Claes H, Van Kampen M, Lysens R, Baert L. Pelvic floor exercises in the treatment of impotence. Eur J Phys Med Rehab. 1995;(5):135–140. [Google Scholar]
- 10.Van Kampen M, De Weerdt W, Claes H, et al. Katholieke Universiteit Leuven: Belgium; 1998. Contribution of pelvic floor muscles exercises in the treatment of impotence. PhD thesis. [Google Scholar]
- 11.Colpi GM, Negri L, Nappi RE, Chinea B. Perineal floor efficiency in sexually potent and impotent men. Int J Impot Res. 1999;11(3):153–157. doi: 10.1038/sj.ijir.3900413. [DOI] [PubMed] [Google Scholar]
- 12.Laycock J. Patient assessment. In: Laycock J, Haslam J, editors. Therapeutic management of incontinence and pelvic pain: pelvic organ disorders. London: Springer-Verlag; 2002. pp. 45–54. [Google Scholar]
- 13.Dorey G. Pelvic floor muscle exercises for erectile dysfunction. London: Whurr Publishers Ltd; 2003. [Google Scholar]
- 14.Rosen RC, Cappelleri JC, Gendrano N., III The International Index of Erectile Function (IIEF): a state-of-the-science review. Int J Impot Res. 2002;14(4):226–244. doi: 10.1038/sj.ijir.3900857. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein I, Lue TF, Padma-Nathan H, et al. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338(20):1397–1404. doi: 10.1056/NEJM199805143382001. [DOI] [PubMed] [Google Scholar]
- 16.MacDonagh R, Ewings P, Porter T. The effect of erectile dysfunction on quality of life: psychometric testing of a new quality of life measure for patients with erectile dysfunction. J Urol. 2002;167(1):212–217. [PubMed] [Google Scholar]
- 17.Claes HIM, Vandenbroucke HB, Baert LV. Pelvic floor exercise in the treatment of impotence. J Urol Suppl. 1996;157(4):786. [Google Scholar]
- 18.Nehra A, Pryor J, Althof SE, et al. Overview consensus statement, Second International Conference on Management of Erectile Dysfunction: new perspectives on treatment. Int J Impot Res. 2002;14(Suppl 1)):S1–S5. doi: 10.1038/sj.ijir.3900789. [DOI] [PubMed] [Google Scholar]
- 19.Shafik A, El-Sibai O. Mechanism of ejection during ejaculation: identification of a urethrocavernosus reflex. Arch Androl. 2002;44(1)):77–83. doi: 10.1080/014850100262443. [DOI] [PubMed] [Google Scholar]
- 20.Dorey G, Swinkels A. Test retest reliability of anal pressure measurements in men with erectile dysfunction. Urol Nurs. 2002;23(3)):204–212. [PubMed] [Google Scholar]
- 21.Lavoisier P, Courtois F, Barres D, Blanchard M. Correlation between intracavernous pressure and contraction of the ischiocavernosus muscle in man. J Urol. 2002;136(4):936–939. doi: 10.1016/s0022-5347(17)45135-4. [DOI] [PubMed] [Google Scholar]


