Abstract
Bipolar depression is the underrecognized and unappreciated phase of bipolar disorder. Nevertheless, bipolar depression is responsible for much of the morbidity and mortality associated with the disorder. Depressive symptoms are far more prevalent than hypomanic or manic symptoms in bipolar patients, and they are associated with a heavier burden of illness, including reduced functioning, increased risk of suicidal acts, and high economic costs. Because most patients with bipolar disorder present with depression, misdiagnoses of major depressive disorder are common, even typical. Comorbid psychiatric disorders are also prevalent and may obscure the diagnosis and complicate treatment strategies. Depressed patients should be carefully assessed for manic or hypomanic symptoms to help reveal possible bipolar disorder. In addition to evaluation of psychiatric symptoms, a close examination of family history, course of illness, and treatment response will aid the clinician in making an accurate diagnosis. Treatment of acute depression in bipolar patients may require therapy combining agents such as lithium, divalproex, lamotrigine, carbamazepine, and atypical antipsychotics or using such agents in combination with an anti-depressant. Olanzapine/fluoxetine combination is the only medication currently approved for the treatment of bipolar depression. Antidepressant monotherapy should not be used, because there is evidence that such treatment increases the risk of switching into mania/hypomania and could induce treatment-refractory conditions such as mixed or rapid-cycling states. Maintenance therapy will be required by most patients, since discontinuation of mood stabilizers or antidepressants frequently leads to relapses in depressive symptoms. Prompt diagnosis and the use of specific therapeutic agents with evidence of efficacy may help reduce the disease burden associated with bipolar depression.
Bipolar disorder is a mood disorder involving a range of manic symptoms typically preceded by and interspersed with depressive episodes. Although a lifetime prevalence of 1% is often quoted for bipolar disorder with manic states (DSM-IV bipolar I), when subsyndromal manic symptoms (DSM-IV bipolar II, bipolar disorder not otherwise specified [NOS], and cyclothymic disorder) are included, its prevalence is seen to be higher than 6%.1 The high prevalence of bipolar disorder is particularly noteworthy because of the significant burden associated with this condition, not only for patients but for family caregivers and employers as well.2–9 Although mania and hypomania specifically identify bipolar illness, depression is of major concern in patients with bipolar disorder, because depressive symptoms are far more frequent than manic symptoms and most suicides occur during the depressive phase.10–12
The prompt diagnosis and treatment of bipolar disorder may help reduce the burden associated with this condition. However, patients with bipolar disorder usually present in the depressive stage, and thus they often receive a diagnosis of major depressive disorder (MDD).13,14 Misdiagnosis or delayed diagnosis of bipolar disorder may result in inappropriate therapy. In particular, antidepressant monotherapy—a common treatment for MDD—may lead to acute mania, mixed states, or rapid-cycling states in patients with bipolar disorder.15,16
This review summarizes recent studies on bipolar depression and explores approaches to accurate diagnosis. Treatment strategies are examined, with an emphasis on agents that have shown evidence of efficacy in bipolar depression.
THE BURDEN OF BIPOLAR DEPRESSION
Bipolar disorder has a negative impact on virtually every facet of a patient's life, with depressive symptoms having a particularly strong effect on patient well-being. Depressive symptoms predominate over hypomanic/manic symptoms in the courses of both bipolar I and bipolar II disorders. In prospective studies of the natural history of bipolar disorder, bipolar I patients reported experiencing depression for 31.9% of weeks and hypomanic/manic symptoms for only 8.9%,10 whereas bipolar II patients reported depression for 50.3% of weeks and hypomanic/ manic symptoms for only 1.3%.11
Similar findings on the prevalence of depressive symptoms were reported in a study of 258 outpatients admitted to the Stanley Foundation Bipolar Network. Approximately 25% of these patients reported being ill for more than three quarters of the year, with a mean of 214 days depressed, and 40% were intermittently ill, with a mean of 120 days depressed.17 An overview of findings from the Stanley Foundation Bipolar Network concluded that, despite treatment, bipolar outpatients remain significantly affected by their illness, with depressive symptoms posing a greater problem for effective treatment than mania.18
As might be expected on the basis of the large part of each year during which symptoms are experienced, bipolar disorder results in a diminished quality of life, even when compared with other mental disorders,2 and in reduced functioning and well-being, compared with chronic medical illness or MDD.19 In particular, bipolar patients report more difficulties with work-related performance, social and leisure activities, and social and family interactions than do MDD patients.9 Depressive symptoms and the number of depressive episodes appear to be primarily responsible for reductions in functioning and quality of life.20,21 However, even patients in manic or hypomanic phases report that their quality of life is reduced,20 indicating that these phases of bipolar disorder are not necessarily associated with an increased sense of well-being or euphoria. The enormous impact of bipolar disorder on the well-being of patients is reflected by the suicide rate, which is more than 20-fold higher than in the general population.5 Suicidal acts are especially likely to occur during the depressive phase or after repeated, severe depression.5,12
Productivity and employment are also adversely affected by bipolar disorder, and this effect has both personal and societal implications. Economic costs for health conditions are usually divided into 2 categories—indirect costs, which include unemployment and decreased productivity, and direct costs, which include prescriptions and medical encounters. Both the indirect and direct costs of bipolar disorder are very high. Over 60% of patients in the Stanley Center Bipolar Disorder Registry were unemployed, despite the fact that 30% had completed college.3 In a study of outpatients with bipolar disorder, 41% believed that their occupational functioning had been adversely affected by their illness.22 Direct costs for patients with bipolar disorder, including prescriptions and medical encounters, far exceed those for individuals who do not have bipolar disorder.
In a cross-sectional study,6 patients with bipolar disorder were found to a receive a mean of 15 central nervous system drug prescriptions per person during the 1-year study period, at an average cost of $582, whereas nonbipolar patients received a mean of 1 central nervous system prescription, at an average cost of $33. Medical encounters were also far more costly and common for patients with bipolar disorder,6 with inpatient costs being almost twice as high as outpatient costs.23 An analysis of the lifetime costs of bipolar disorder in the United States, based on 1998 figures, concluded that the average cost per case ranged from $11,720 for patients with a single manic episode to $624,785 for patients with nonresponsive or chronic episodes.7
The total annual cost of bipolar disorder in the United States was estimated at $45 billion (1991 values), with $7 billion attributed to direct costs for inpatient and out-patient care and $38 billion due to lost productivity of wage earners, homemakers, individuals who were in institutions or who had committed suicide, and caregivers.24 An analysis of data from a multiemployer database found that bipolar disorder was the most costly mental health disorder for employers.4
A recent study25 highlighted the hidden costs associated with a delayed diagnosis of bipolar disorder. This study examined 9009 patients treated for depression with antidepressants. “Unrecognized” bipolar patients were considered to be those who met the criteria for bipolar disorder after initiation of antidepressant therapy, while “recognized” bipolar patients met the criteria at or before initiation of therapy. Unrecognized bipolar patients had significantly greater mean monthly medical costs than recognized bipolar patients ($1179 vs. $801) and were less likely to receive a mood stabilizer. These data suggest that timely recognition of bipolar disorder may lead to better treatment and reduced costs.
The effects of bipolar disorder on family members and caregivers are more difficult to measure but are also substantial, ranging from practical difficulties to emotional stresses. In a study of 266 caregivers of patients, almost all caregivers reported moderate or greater distress associated with caring for a patient with bipolar disorder.8
DIAGNOSING BIPOLAR DEPRESSION
Misdiagnosis: A Common Problem
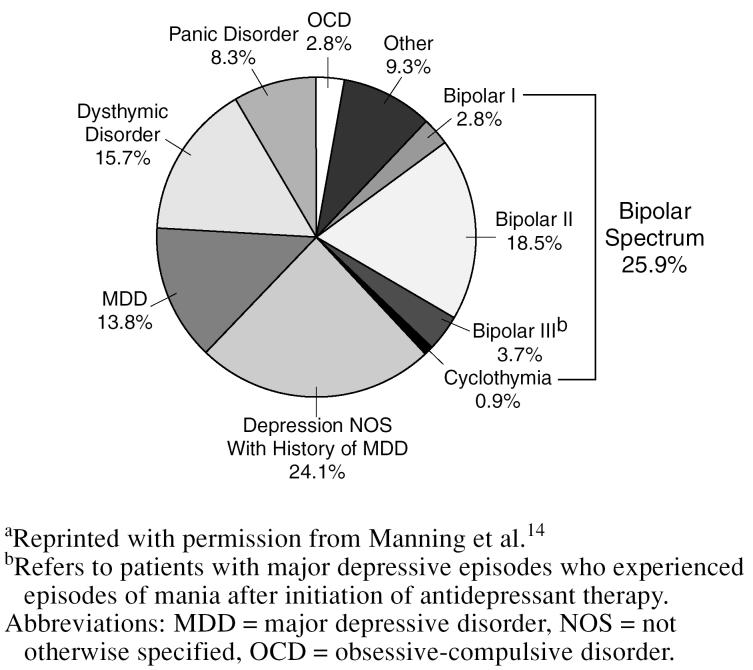
Primary care clinicians are the health care professionals most likely to see patients with bipolar disorder. In a prospective evaluation conducted at a private family practice center, 108 consecutive anxious and/or depressed patients underwent a semistructured diagnostic interview conducted by a family physician with special training in mood disorders.14 Of these patients, 28 (26%) were found to have disorders within the bipolar spectrum (Figure 1). In another prospective study,26 bipolar disorder was found to be the most common diagnosis among patients presenting at a primary care mood disorders clinic. Evaluations of 187 consecutively referred patients determined that 39% had bipolar disorder (I, II, or NOS).26
Figure 1.
Primary Diagnoses for 108 Consecutive Depressed and/or Anxious Patients in a Family Practice Settinga
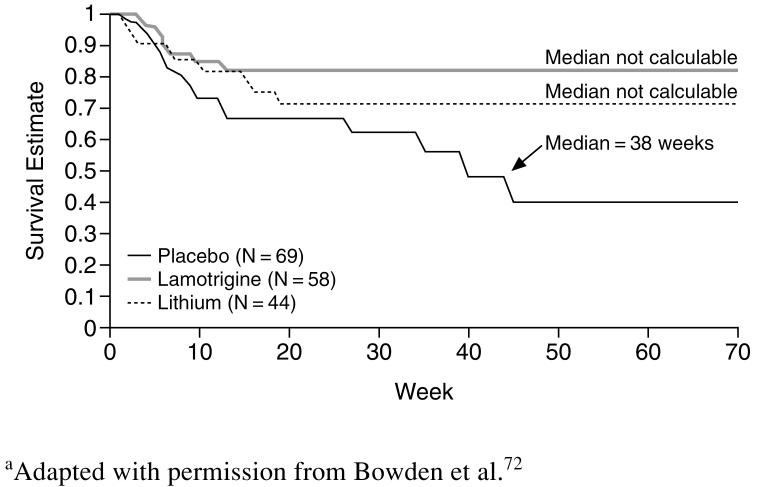
The manic and depressive symptoms required for the DSM-IV diagnosis of disorders of the bipolar spectrum (bipolar I, bipolar II, bipolar disorder NOS, and cyclothymic disorder) are summarized in Table 1.27,28 All of these disorders are characterized by the presence of manic (bipolar I and bipolar NOS) or hypomanic (bipolar II and cyclothymic) episodes. In addition, they are all typically associated with depressive episodes. Although depressive symptoms are not required for the diagnosis of bipolar I or bipolar NOS, they are still frequently observed in these patients. In the Stanley Foundation Bipolar Network, more than 50% of patients with bipolar disorder I said that depressive symptoms had been their first bipolar symptoms.29 Among bipolar I patients, 76% reported more than 4 episodes of depression during the course of their illness, and 44% reported more than 20 episodes of depression.29 Similarly, a study in which bipolar patients were followed for a mean of 12.8 years found depression to be the predominant symptom.10 The major difference between disorders of the bipolar spectrum and major depressive disorder, then, is a history of hypomanic or manic symptoms.
Table 1.
Manic and Depressive Symptom Criteria for Disorders of the Bipolar Spectruma
Since many patients with bipolar disorder present with depression, it can be easy to overlook a history of manic or hypomanic symptoms when making a diagnosis. In a recent survey of bipolar patients involved with National Depressive and Manic-Depressive Association support groups, 69% reported that they were initially misdiagnosed by psychiatrists; a mean of 3.5 other diagnoses were received and 4 psychiatrists were consulted before an accurate diagnosis was received.13 For 60% of patients, the misdiagnosis was MDD. Women were more likely than men to be misdiagnosed with MDD (68% vs. 43%).13
A study30 of outpatients with bipolar disorder found similarly high rates of misdiagnosed MDD (56%) among these patients, with a mean lag time of 8.9 years between the time the patient first sought medical help and the time he or she received an accurate diagnosis of bipolar disorder. Notably, even among patients who experienced their first manic or hypomanic episode before their first visit to a health care professional, 37% still received a diagnosis of MDD.30 Other common misdiagnoses include schizophrenia (particularly in men), various anxiety disorders, borderline personality disorder, substance abuse, and schizoaffective disorder.13
There are several factors that may contribute to the problem of misdiagnoses in patients with bipolar disorder. Foremost is an incomplete understanding of bipolar disorder by health professionals. Bipolar illness is often narrowly viewed as consisting of individuals who experience mania. This is far from the truth. As has been stated, bipolar illness is much broader in its presentation and impact. Most affected individuals never experience syndromal manic episodes. Further, episodes of depression typically precede the appearance of manic symptoms and outnumber periods of hypomania or mania, causing a greater proportion of dysfunction related to the illness. In short, bipolar illness is usually one of significant depression interspersed—or combined—with periods of manic symptoms. Differential diagnosis of the illness involves several steps, beginning with an understanding of its prevalence and an appreciation that although we may define bipolar illness on the basis of manic symptoms, it is bipolar depression that will be seen more often. From this understanding, we can suggest essential principles in the clinical assessment of every depressed and anxious patient. Chief among these is to anticipate an ultimate diagnosis of bipolar illness by carefully differentiating its phenomenology (symptoms), family history, longitudinal course, and treatment response from those of MDD (see “Steps to Diagnosis”).
Educational programs can make a substantial difference in the ability of physicians to recognize mood disorders. In a study26 in which 51 residents received training on the clinical assessment of mood disorders, the rate of their mood disorder recognition was found to increase significantly after the training. Another factor that contributes to misdiagnoses of bipolar disorder is incomplete reporting of symptoms by patients. Such underreporting is widespread. In one study,13 between 25% and 50% of patients admitted to not reporting key symptoms of mania, and about 20% failed to report symptoms of depression.
Comorbid Disorders
The high prevalence of comorbid disorders can complicate not only the diagnosis of bipolar disorder but also its treatment.31 In a recent analysis of 288 outpatients with bipolar disorder, McElroy et al.32 found that 65% of patients with bipolar disorder also met DSM-IV criteria for at least 1 comorbid Axis I disorder during their lifetime, with similar rates seen in bipolar I (67%) and bipolar II (57%) patients. Patients had a mean of 1.7 comorbid diagnoses during their lifetime, with approximately one quarter reporting 3 or more comorbid Axis I disorders. Anxiety disorders were particularly common, affecting 42% of bipolar patients during their lifetime. The most common anxiety disorder was panic disorder/agoraphobia (20%), followed by social phobia (16%), simple phobia (10%), and obsessive-compulsive disorder (9%).32
Comorbid anxiety disorders are significantly associated with a depressive temperament in bipolar patients.33 Several studies suggest that comorbid anxiety disorders are more common in patients with bipolar disorder than in patients with MDD, although the reports are not fully consistent. In 1 study, comorbid panic disorder was found to have a 2-fold higher lifetime prevalence in bipolar patients than in MDD patients,34 but in another study, current prevalence rates were similar between the 2 groups.35 Similarly, social phobia was found to be more strongly associated with bipolar disorder than with MDD in 1 study36 but not in another.35 Social anxiety as a temperamental trait has been significantly associated with bipolar II disorder in an 11-year prospective study of major depression.37 Obsessive-compulsive disorder has been reported to be approximately twice as common in patients with bipolar disorder than in those with MDD.35
Another common comorbid psychiatric diagnosis for patients with bipolar disorder is substance abuse. The study by McElroy and colleagues32 found that 42% of bipolar patients had a comorbid substance use disorder during their lifetime, with a slightly higher prevalence among bipolar I patients (45%) compared with bipolar II patients (31%). Alcohol was the most commonly abused substance (33%), followed by marijuana (16%), stimulants (9%), and cocaine (9%).32 Other investigators document even higher rates.38
Steps to Diagnosis
Evaluation of symptoms
A thorough evaluation of symptoms is an important component of all psychiatric diagnoses. Because many bipolar patients present with depression, clinicians should be especially careful to query depressed patients about manic symptoms and manic/ hypomanic episodes. Several tools exist to help the clinician in uncovering these symptoms, including the Mood Disorder Questionnaire (MDQ)39 and the DIGFAST mnemonic for symptoms of a manic episode (distractibility, indiscretion, grandiosity, flight of ideas, activity increase, sleep deficit, talkativeness).40 The MDQ is a patient self-rated assessment that samples 13 manic symptoms for concurrence and severity to achieve a sensitivity of 70% and a specificity of 90% in psychiatric outpatients. Although this instrument has not yet been validated in primary care outpatient settings, it may be a reasonable and useful screener in this setting.
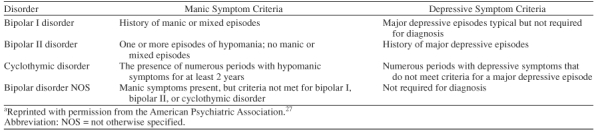
Mania and hypomania are differentiated on the basis of duration (7 vs. 4 days per DSM-IV) and severity criteria (marked vs. nonmarked impairment). Both cause unequivocal changes in function. Hypomania is, by definition, nonpsychotic and is more common than syndromal mania, even in bipolar I (manic) patients. Hypomania can be difficult for patients to recall in depressed episodes.28 Table 2 lists some questions that may help elicit information on hypomanic symptoms.41
Table 2.
Suggested Questions for Uncovering Hypomaniaa
Family history
A carefully taken family history can also aid in the diagnosis of bipolar disorder. Bipolar patients, particularly those presenting in adolescence, frequently have a family history of bipolar disorder or mania.42–44 In fact, people with a first-degree relative with bipolar disorder have an almost 14-fold higher risk of developing bipolar disorder than people who do not have such a relative.45 In addition, the family histories of bipolar patients are more often loaded for mood disorders and other psychiatric disorders, such as schizophrenia, than are the family histories of MDD patients.44,46
Course of illness
The course of illness in a presenting patient may provide further clues to help differentiate between bipolar disorder and MDD. Some of the features that are associated with bipolar disorder include an early onset (under the age of 25 years), usually with a depressive or mixed episode; abrupt onset and termination; escalating episode intensity; and a postpartum onset for the first major depressive episode.42 The Stanley Foundation Bipolar Treatment Outcome Network found adolescent (age ≤ 17 years) onset of bipolar disorder to be significantly associated with a family history of bipolar disorder; learning disability; multiple (≥ 20) episodes of depression, mania/hypomania, and ultradian cycling; a history of worsening course of illness; and a history of abuse.29 First episodes of illness were usually depressive. No significant differences between early-onset and late-onset bipolar illness were noted for gender, suicide attempts, substance abuse, mood disorder in first-degree relatives, or household income.29
Treatment response
Treatment response may also suggest a bipolar diagnosis. Antidepressant-induced mania/ hypomania is observed in 10% to 40% of bipolar patients.16,22,47 Although antidepressant-induced mania/ hypomania is not a DSM-IV–recognized criterion for bipolar disorder, many clinicians are convinced of its relevance, and it is referred to by some as bipolar III.48 Antidepressant-induced mania occurs at a higher rate in bipolar disorder patients than in MDD patients15,16 and is more likely to occur in bipolar I than in bipolar II patients.49 Antidepressant-induced mania is more frequent and more severe with tricyclic antidepressants and monoamine oxidase inhibitors than with selective serotonin re-uptake inhibitors (SSRIs), including fluoxetine, fluvoxamine, paroxetine, and sertraline.15,50 The rate of switching into mania or hypomania among patients treated with bupropion was similar to that in patients treated with SSRIs.49
In a comparative study in which bipolar patients on treatment with mood stabilizers were treated with venlafaxine or an SSRI (paroxetine) for 6 weeks, 3% of paroxetine-treated patients switched to mania or hypomania compared with 13% of venlafaxine-treated patients.51 Data from the Stanley Foundation Bipolar Network also indicate that venlafaxine is associated with a higher rate of switching than bupropion or the SSRI sertraline, although these findings have not yet been published in full.22 Together, these data suggest that SSRIs and bupropion are associated with similarly low levels of antidepressant-induced mania, while the switching rates associated with tricyclic antidepressants, monoamine oxidase inhibitors, and venlafaxine are higher.
A lack of response to treatment may also signal the existence of undiagnosed bipolar disorder. A study of medical records of patients with diagnosed depression who received antidepressant medication revealed that patients with treatment-resistant depression were far more likely to have bipolar disorder than those whose depression was not refractory to treatment.52 Similarly, a need for multiple psychotropic medications may suggest bipolar disorder. In a study3 of patients with bipolar disorder, more than a third were taking at least 3 types of psychotropic medications.
TREATMENT STRATEGIES FOR BIPOLAR DEPRESSION
Treatment response to therapeutic agents is far less studied in patients with bipolar depression than in patients with mania. Available data indicate that current treatment modalities do not adequately address the needs of most patients with bipolar depression. Even among patients with bipolar disorder receiving intensive pharmacotherapy with an average of 4 medications, 26% reported being ill most of the year and 41% reported being intermittently ill; depressive symptoms accounted for the majority of the reported illness.18 In another study,22 patients with bipolar depression who responded to a 10-week course of therapy with an antidepressant were offered double-blind continuation with the treatment for 1 year. Of the patients who entered the continuation trial, 30% dropped out because their depression recurred.22 In a comparison of MDD and bipolar disorder patients with depression, nonresponse to antidepressants was 1.6 times as common in bipolar patients, and loss of response during treatment with antidepressants occurred 3.4 times as often.16 A need thus remains for new agents and approaches to managing bipolar depression.
Because of the scarcity of research on this topic, there are no evidence-based guidelines available for the treatment of bipolar depression. The following discussion of treatment options is in general agreement with the American Psychiatric Association Practice Guideline for the Treatment of Patients With Bipolar Disorder (Revision)27 and guidelines from the British Association for Psychopharmacology,53 with some additional points included for the reader's consideration.
Acute, Mild Depressive Episodes
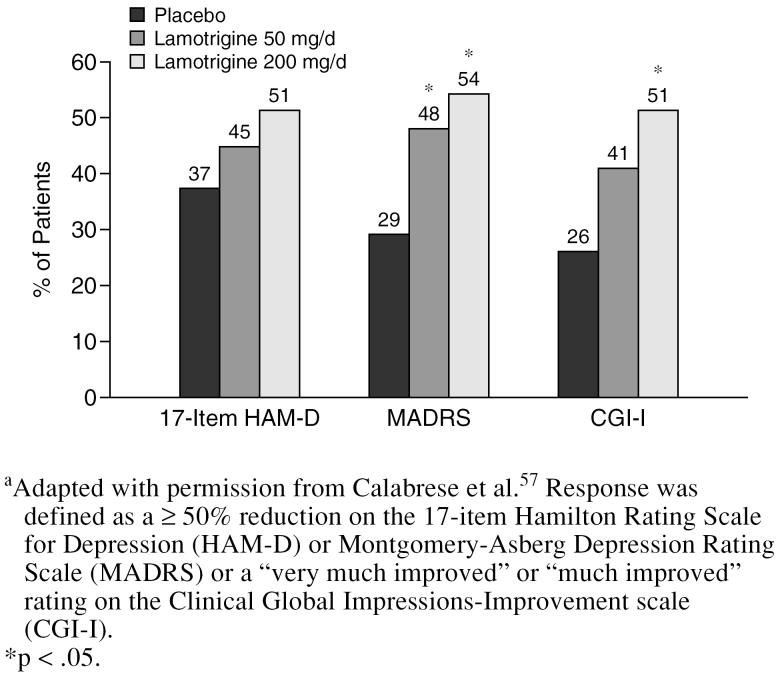
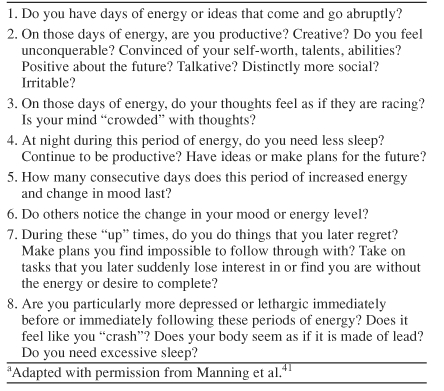
For acute episodes of mild depression in patients with bipolar disorder, monotherapy with mood stabilizers such as lithium or lamotrigine is often used.27 Both agents have been found superior to placebo in the treatment of acute bipolar depression.54 The proven efficacy of lithium is summarized in Table 3,55,56 and patient response to lamotrigine monotherapy in acute bipolar I depression is shown in Figure 2.57
Table 3.
Summary of Research on the Efficacy of Lithium in Bipolar Depressiona
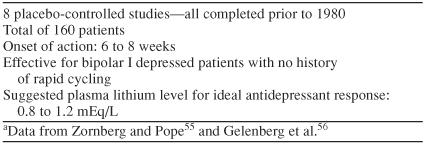
Figure 2.
Patients With Acute Bipolar I Depression Responding to Lamotrigine vs. Placeboa
Newer agents also appear to hold promise for the treatment of bipolar depression. In particular, monotherapy with olanzapine, a novel mood stabilizer/ antipsychotic, is significantly more effective than placebo for improving depressive symptoms in patients with bipolar depression.58–60
Refractory or Severe Depression
For refractory or more severe depression, combination therapy is often necessary. A common treatment strategy is to combine lithium or an anticonvulsant (carbamazepine, divalproex, or lamotrigine) with an antidepressant (SSRI or bupropion preferred).61 There is strong evidence that the concomitant use of lithium decreases the rate of switching to hypomania or mania in patients treated with antidepressants.62,63 The case for anticonvulsants is less clear. In a study63 concerning risk factors associated with antidepressant-induced mania, antidepressant-treated patients who received lithium or lithium plus an anticonvulsant showed substantially lower rates of switching than patients who received antidepressant therapy without lithium, without any mood stabilizer, or with an anticonvulsant. These data confirm the anti-switching effect of lithium but suggest that anticonvulsants do not fully share this property.
Electroconvulsive therapy is also effective in refractory bipolar depression.64 However, relapse rates are high, and continuation therapy with medication is usually required to maintain response.65
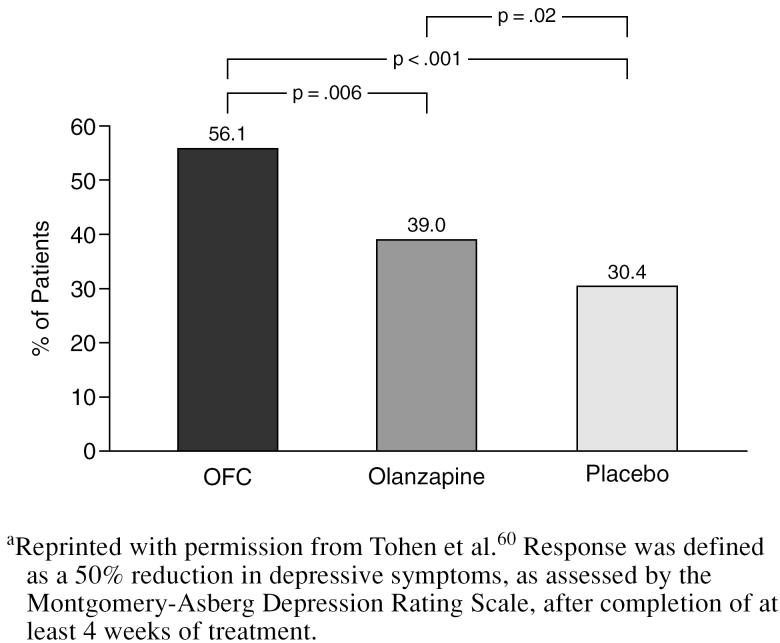
Recent data provide support for the use of olanzapine/ fluoxetine combination in the treatment of bipolar depression. In patients with bipolar I depression, olanzapine/ fluoxetine combination was markedly and statistically superior to placebo and to olanzapine alone in rate of response (50% reduction in depressive symptoms after at least 4 weeks of treatment) and time to response (Figure 3).60 The olanzapine/fluoxetine combination group and the olanzapine monotherapy group were comparable to the placebo group in the rate of treatment-emergent mania (6.4%, 5.7%, and 6.7%, respectively), indicating that olanzapine/fluoxetine combination was not associated with an increased rate of switching into syndromal mania.60 It should be noted, however, that close clinical observation for progression toward a manic episode is advisable for any bipolar patient given an antidepressant, with appropriate clinical interventions based on treatment response. Olanzapine/fluoxetine combination is the first treatment to be approved by the U.S. Food and Drug Administration (FDA) for the treatment of bipolar depression.
Figure 3.
Comparison of Response Rates With Olanzapine/ Fluoxetine Combination (OFC; N = 86), Olanzapine Monotherapy (N = 370), and Placebo (N = 377) in the Treatment of Bipolar I Depressiona
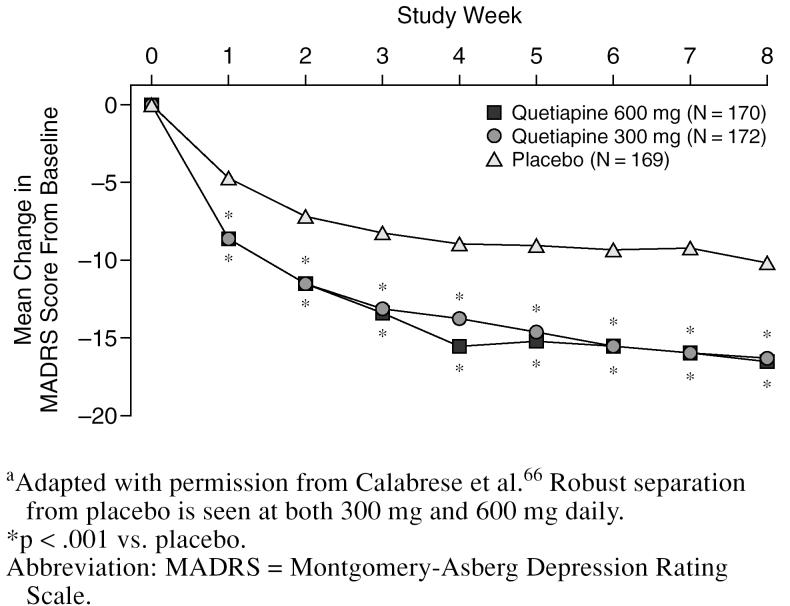
A recent trial of quetiapine monotherapy in bipolar I and II patients showed robust separation from placebo at both 300 mg and 600 mg daily (Figure 4).66 A subsequent trial will be needed to confirm this effect.
Figure 4.
Change in MADRS Score With Quetiapine Monotherapy vs. Placebo in a Randomized Controlled Trial of Patients With Bipolar Depressiona
Regardless of the combination regimen chosen, thyroid levels should be checked before initiation of antidepressant therapy, since up to 75% of patients have a thyroid profile (low free thyroxine index or high thyroid-stimulating hormone levels) that is suboptimal for antidepressant response.67 An increased incidence of antithyroid antibodies is another common finding in patients with bipolar disorder.18
Maintenance Therapy
Maintenance therapy is likely to be the backbone of effective therapy for bipolar depression, but little is known about this aspect of treatment. Patients with bipolar disorder have been shown to be at a constant risk for recurrence up to the age of 70 years or older,68 suggesting that lifelong prophylactic treatment may be required. Maintenance therapy may improve patient functioning and quality of life and may be more critical to the successful treatment of bipolar depression than to that of MDD. Depressive relapses after antidepressant discontinuation were found to be almost 5 times as common in patients with bipolar depression as in patients with MDD.16
Other studies have also documented high rates of depressive relapse after discontinuation of antidepressants in successfully treated bipolar patients. In a retrospective chart review of patients with bipolar depression who improved in response to antidepressant therapy, the rate of depressive relapses was much higher in patients who discontinued antidepressant therapy than in patients who continued treatment (68% vs. 32% at 1 year).69 Most patients were using polypharmacy with mood stabilizers and antidepressants in combination. Further analyses showed that patients who discontinued therapy early had a 3-fold greater risk for depressive relapse, but that their risk for mania relapse was not significantly reduced.69
A follow-up study70 confirmed these findings, with 70% of patients who discontinued antidepressants experiencing a depressive relapse within 1 year, compared with 36% of patients who continued antidepressants. As in the earlier study, continuation did not result in a higher rate of manic switching.70 Increased risk of antidepressant-induced mania is a possible rationale for discontinuing antidepressant therapy, but these data suggest that the risk is small and that continued antidepressant therapy is preferable in patients with stable, robust responses.
Termination of mood stabilizers may also have negative effects in patients with bipolar disorder. In published studies of patients with bipolar disorder who discontinued lithium treatment, suicide rates rose 20-fold and affective illness recurred in 67% of patients during the first year after discontinuation of lithium.12 Termination of treatment with other mood stabilizers, including the atypical antipsychotics, may be associated with negative outcomes.
Lamotrigine has recently been approved by the FDA for maintenance therapy in bipolar disorder on the basis of a controlled comparison of lamotrigine-treated patients to placebo- and lithium-treated patients. Its maintenance effect is predominantly the ability to prevent the reoccurrence of bipolar depression (Figure 5).71,72
Figure 5.
Time to Intervention for Depression After a Depressive Episode With Lamotrigine vs. Lithium and Placebo as Bipolar Maintenance Therapy (Kaplan-Meier analysis)a
IMPACT OF LATE DIAGNOSIS AND SUBOPTIMAL THERAPY
Bipolar disorder can be a frustrating condition to treat, but aggressive treatment is essential to improved patient outcomes. As noted earlier, unrecognized bipolar patients have higher mean monthly medical costs than recognized bipolar patients and are less likely to receive a mood stabilizer.25 Lithium treatment is associated with a substantial reduction in disease morbidity and suicidal acts in bipolar patients,12 and there is evidence that response to lithium is diminished in patients who have had several previous depressive or manic episodes.73 Delayed initiation of mood stabilizers has also been associated with poorer social functioning, more hospitalizations, and a greater likelihood of attempted suicide.74 Such findings emphasize the need for early recognition of bipolar disorder in order to maximize treatment response, improve patient functioning, and reduce costs. There is currently a lag time of almost 9 years between the time a patient with bipolar disorder first seeks care and the time a correct diagnosis is received.30 Reducing this intervening period could result in tangible benefits for patients.
CONCLUSIONS
Depressive symptoms are a critical component of bipolar disorder and are associated with reduced quality of life, impaired functioning, and increased mortality due to suicidal acts. Accurate diagnosis and prompt, appropriate treatment are currently our best hope for reducing this disease burden. It is therefore critical that clinicians carefully screen depressed patients for bipolar disorder and be aware of confounding comorbid disorders, such as anxiety disorders and substance abuse. The possibility of manic episodes in undiagnosed bipolar disorder treated with antidepressant monotherapy should also be kept in mind, since these episodes may help point the clinician toward a correct diagnosis. Because bipolar depression is often refractory to treatment, aggressive therapy may be required. The substantial residual disease morbidity even in heavily treated patients suggests that new agents and combinations of agents may be required for the successful management of bipolar depression. Delayed diagnosis and suboptimal therapy are associated with significant personal and economic consequences, whereas effective therapy may reduce disease burden. Our challenge now is to identify agents and combinations of agents best suited to controlling bipolar depression.
Drug names: bupropion (Wellbutrin and others), carbamazepine (Carbatrol, Equetro, and others), divalproex (Depakote), fluoxetine (Prozac and others), lamotrigine (Lamictal), lithium (Lithobid, Eskalith, and others), olanzapine (Zyprexa), olanzapine/fluoxetine (Symbyax), paroxetine (Paxil, Pexeva, and others), quetiapine (Seroquel), sertraline (Zoloft), venlafaxine (Effexor).
Footnotes
Funding for manuscript development was provided by Eli Lilly and Company.
Dr. Manning has been a consultant for Eli Lilly and AstraZeneca.
The author recognizes the editorial support of John Cooke and Fred Myers, M.A., of BioScience Communications.
REFERENCES
- Judd LL, Akiskal HS.. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. J Affect Disord. 2003;73:123–131. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- ten Have M, Vollebergh W, and Bijl R. et al. Bipolar disorder in the general population in the Netherlands (prevalence, consequences and care utilisation): results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). J Affect Disord. 2002 68:203–213. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, and Grochocinski VJ. et al. Demographic and clinical characteristics of individuals in a bipolar disorder case registry. J Clin Psychiatry. 2002 63:120–125. [DOI] [PubMed] [Google Scholar]
- Goetzel RZ, Hawkins K, and Ozminkowsky RJ. et al. The health and productivity cost burden of the “top 10” physical and mental health conditions affecting six large US employers in 1999. J Occup Environ Med. 2003 45:5–14. [DOI] [PubMed] [Google Scholar]
- Tondo L, Isacsson G, Baldessarini R.. Suicidal behavior in bipolar disorder: risk and prevention. CNS Drugs. 2003;17:491–511. doi: 10.2165/00023210-200317070-00003. [DOI] [PubMed] [Google Scholar]
- Stender M, Bryant-Comstock L, Phillips S.. Medical resource use among patients treated for bipolar disorder: a retrospective, cross-sectional, descriptive analysis. Clin Ther. 2002;24:1668–1676. doi: 10.1016/s0149-2918(02)80070-4. [DOI] [PubMed] [Google Scholar]
- Begley CE, Annegers JF, and Swann AC. et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001 19:483–495. [DOI] [PubMed] [Google Scholar]
- Perlick D, Clarkin JF, and Sirey J. et al. Burden experienced by caregivers of persons with bipolar affective disorder. Br J Psychiatry. 1999 175:56–62. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Hirschfield RM, and Reed M. et al. Impact of bipolar disorder on a U.S. community sample. J Clin Psychiatry. 2003 64:425–432. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, and Schettler PJ. et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002 59:530–537. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, and Schettler PJ. et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. 2003 60:261–269. [DOI] [PubMed] [Google Scholar]
- Baldessarini RJ, Tondo L, Hennen J.. Effects of lithium treatment and its discontinuation on suicidal behavior in bipolar manic-depressive disorders. J Clin Psychiatry. 1999;60(suppl 2):77–84. [PubMed] [Google Scholar]
- Hirschfeld RM, Lewis L, Vornik LA.. Perceptions and impact of bipolar disorder: how far have we really come? results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–174. [PubMed] [Google Scholar]
- Manning JS, Haykal RF, and Connor PD. et al. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997 38:102–108. [DOI] [PubMed] [Google Scholar]
- Peet M.. Induction of mania with selective serotonin re-uptake inhibitors and tricyclic antidepressants. Br J Psychiatry. 1994;164:549–550. doi: 10.1192/bjp.164.4.549. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Rosenquist KJ, and Ko JY. et al. Antidepressant treatment in bipolar versus unipolar depression. Am J Psychiatry. 2004 161:163–165. [DOI] [PubMed] [Google Scholar]
- Post RM, Denicoff KD, and Leverich GS. et al. Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method. J Clin Psychiatry. 2003 64:680–690. [DOI] [PubMed] [Google Scholar]
- Post RM, Leverich GS, and Altshuler LL. et al. An overview of recent findings of the Stanley Foundation Bipolar Network, pt 1. Bipolar Disord. 2003 5:310–319. [DOI] [PubMed] [Google Scholar]
- Cooke RG, Robb JC, and Young LT. et al. Well-being and functioning in patients with bipolar disorder assessed using the MOS 20-ITEM short form (SF-20). J Affect Disord. 1996 39:93–97. [DOI] [PubMed] [Google Scholar]
- Vojta C, Kinosian B, and Glick H. et al. Self-reported quality of life across mood states in bipolar disorder. Compr Psychiatry. 2001 42:190–195. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Young LT, and Robb JC. et al. Effect of number of episodes on wellbeing and functioning of patients with bipolar disorder. Acta Psychiatr Scand. 2000 101:374–381. [DOI] [PubMed] [Google Scholar]
- Post RM, Leverich GS, and Nolen WA. et al. A re-evaluation of the role of antidepressants in the treatment of bipolar depression: data from the Stanley Foundation Bipolar Network. Bipolar Disord. 2003 5:396–406. [DOI] [PubMed] [Google Scholar]
- Peele PB, Xu Y, Kupfer DJ.. Insurance expenditures on bipolar disorder: clinical and parity implications. Am J Psychiatry. 2003;160:1286–1290. doi: 10.1176/appi.ajp.160.7.1286. [DOI] [PubMed] [Google Scholar]
- Wyatt RJ, Henter I.. An economic evaluation of manic-depressive illness: 1991. Soc Psychiatry Psychiatr Epidemiol. 1995;30:213–219. doi: 10.1007/BF00789056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birnbaum HG, Shi L, and Dial E. et al. Economic consequences of not recognizing bipolar disorder patients: a cross-sectional descriptive analysis. J Clin Psychiatry. 2003 64:1201–1209. [DOI] [PubMed] [Google Scholar]
- Manning JS, Zylstra RG, Connor PD.. Teaching family physicians about mood disorders: a procedure suite for behavioral medicine. Prim Care Companion J Clin Psychiatry. 1999;1:18–23. doi: 10.4088/pcc.v01n0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients With Bipolar Disorder [Revision] Am J Psychiatry. 2002;159(suppl 4):1–50. [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association. 2000 [Google Scholar]
- Suppes T, Leverich GS, and Keck PE. et al. The Stanley Foundation Bipolar Treatment Outcome Network, 2: demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001 67:45–59. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Boiman EE, Goodwin FK.. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. J Clin Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- Manning JS.. Treating panic disorder: its comorbidity with bipolar disorders [letter] J Am Board Fam Pract. 1999;12:102–103. [PubMed] [Google Scholar]
- McElroy SL, Altshuler LL, and Suppes T. et al. Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. Am J Psychiatry. 2001 158:420–426. [DOI] [PubMed] [Google Scholar]
- Henry C, Van den Bulke D, and Bellivier F. et al. Anxiety disorders in 318 bipolar patients: prevalence and impact on illness severity and response to mood stabilizer. J Clin Psychiatry. 2003 64:331–335. [PubMed] [Google Scholar]
- Chen YW, Dilsaver SC.. Comorbidity of panic disorder in bipolar illness: evidence from the Epidemiologic Catchment Area Survey. Am J Psychiatry. 1995;152:280–282. doi: 10.1176/ajp.152.2.280. [DOI] [PubMed] [Google Scholar]
- Pini S, Cassano GB, and Simonini E. et al. Prevalence of anxiety disorders comorbidity in bipolar depression, unipolar depression and dysthymia. J Affect Disord. 1997 42:145–153. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang P, and Wittchen HU. et al. Lifetime comorbidities between social phobia and mood disorders in the US National Comorbidity Survey. Psychol Med. 1999 29:555–567. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Maser JD, and Zeller PJ. et al. Switching from “unipolar” to bipolar II: an 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry. 1995 52:114–123. [DOI] [PubMed] [Google Scholar]
- Sonne SC, Brady KT.. Substance abuse and bipolar comorbidity. Psychiatr Clin North Am. 1999;22:609–627. doi: 10.1016/s0193-953x(05)70098-8. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Williams JB, and Spitzer RL. et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000 157:1873–1875. [DOI] [PubMed] [Google Scholar]
- Carlat DJ.. The psychiatric review of symptoms: a screening tool for family physicians. Am Fam Physician. 1998;58:1617–1624. [PubMed] [Google Scholar]
- Manning JS, Connor PD, Sahai A.. The bipolar spectrum: a review of current concepts and implications for the management of depression in primary care. Arch Fam Med. 1998;6:63–71. doi: 10.1001/archfami.7.1.63. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Walker P, and Puzantian VR. et al. Bipolar outcome in the course of depressive illness: phenomenologic, familial, and pharmacologic predictors. J Affect Disord. 1983 5:115–128. [DOI] [PubMed] [Google Scholar]
- Somanath CP, Jain S, Reddy YC.. A family study of early-onset bipolar I disorder. J Affect Disord. 2002;70:91–94. doi: 10.1016/s0165-0327(00)00372-4. [DOI] [PubMed] [Google Scholar]
- Winokur G, Coryell W, and Keller M. et al. A family study of manic-depressive (bipolar I) disease: is it a distinct illness separable from primary unipolar depression? Arch Gen Psychiatry. 1995 52:367–373. [DOI] [PubMed] [Google Scholar]
- Mortensen PB, Pedersen CB, and Melbye M. et al. Individual and familial risk factors for bipolar affective disorders in Denmark. Arch Gen Psychiatry. 2003 60:1209–1215. [DOI] [PubMed] [Google Scholar]
- Benazzi F.. Clinical differences between bipolar II depression and unipolar major depressive disorder: lack of an effect of age. J Affect Disord. 2003;75:191–195. doi: 10.1016/s0165-0327(02)00047-2. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Truman CJ.. Antidepressant-induced mania: an overview of current controversies. Bipolar Disord. 2003;5:407–420. doi: 10.1046/j.1399-5618.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Hantouche EG, and Allilaire JF. et al. Validating antidepressant-associated hypomania (bipolar III): a systematic comparison with spontaneous hypomania (bipolar II). J Affect Disord. 2003 73:65–74. [DOI] [PubMed] [Google Scholar]
- Joffe RT, MacQueen GM, and Marriott M. et al. Induction of mania and cycle acceleration in bipolar disorder: effect of different classes of antidepressant. Acta Psychiatr Scand. 2002 105:427–430. [DOI] [PubMed] [Google Scholar]
- Boerlin HL, Gitlin MJ, and Zoellner LA. et al. Bipolar depression and antidepressant-induced mania: a naturalistic study. J Clin Psychiatry. 1998 59:374–379. [DOI] [PubMed] [Google Scholar]
- Vieta E, Martinez-Aran A, and Goikolea JM. et al. A randomized trial comparing paroxetine and venlafaxine in the treatment of bipolar depressed patients taking mood stabilizers. J Clin Psychiatry. 2002 63:508–512. [DOI] [PubMed] [Google Scholar]
- Crown WH, Finkelstein S, and Berndt ER. et al. The impact of treatment-resistant depression on health care utilization and costs. J Clin Psychiatry. 2002 63:963–971. [DOI] [PubMed] [Google Scholar]
- Goodwin GM for the Consensus Group of the British Association for Psychopharmacology. Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. J Psychopharmacol. 2003;17:149–173. doi: 10.1177/0269881103017002003. [DOI] [PubMed] [Google Scholar]
- Yatham LN, Calabrese JR, Kusumakar V.. Bipolar depression: criteria for treatment selection, definition of refractoriness, and treatment options. Bipolar Disord. 2003;5:85–97. doi: 10.1034/j.1399-5618.2003.00019.x. [DOI] [PubMed] [Google Scholar]
- Zornberg GL, Pope HG Jr.. Treatment of depression in bipolar disorder: new directions for research. J Clin Psychopharmacol. 1993;13:397–408. [PubMed] [Google Scholar]
- Gelenberg AJ, Kane JM, and Keller MB. et al. Comparison of standard and low serum levels of lithium for maintenance treatment of bipolar disorder. N Engl J Med. 1989 321:1489–1493. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Bowden CL, and Sachs GS. et al. A double-blind placebo-controlled study of lamotrigine monotherapy in outpatients with bipolar I depression. Lamictal 602 Study Group. J Clin Psychiatry. 1999 60:79–88. [DOI] [PubMed] [Google Scholar]
- Chengappa KN, Baker RW, and Shao L. et al. Rates of response, euthymia and remission in two placebo-controlled olanzapine trials for bipolar mania. Bipolar Disord. 2003 5:1–5. [DOI] [PubMed] [Google Scholar]
- Baker RW, Tohen M, and Fawcett J. et al. Acute dysphoric mania: treatment response to olanzapine versus placebo. J Clin Psychopharmacol. 2003 23:132–137. [DOI] [PubMed] [Google Scholar]
- Tohen M, Vieta E, and Calabrese J. et al. Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry. 2003 60:1079–1088. [DOI] [PubMed] [Google Scholar]
- Thase ME, Sachs GS.. Bipolar depression: pharmacotherapy and related therapeutic strategies. Biol Psychiatry. 2000;48:558–572. doi: 10.1016/s0006-3223(00)00980-x. [DOI] [PubMed] [Google Scholar]
- Bottlender R, Rudolf D, and Strauss A. et al. Mood stabilizers reduce the risk of developing antidepressant-induced maniform states in acute treatment of bipolar I depressed patients. J Affect Disord. 2001 63:79–83. [DOI] [PubMed] [Google Scholar]
- Henry C, Sorbara F, and Lacoste J. et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001 62:249–255. [DOI] [PubMed] [Google Scholar]
- Daly JJ, Prudic J, and Devanand DP. et al. ECT in bipolar and unipolar depression: differences in speed of response. Bipolar Disord. 2001 3:95–104. [DOI] [PubMed] [Google Scholar]
- Sackeim HA, Haskett RF, and Mulsant BH. et al. Continuation pharmacotherapy in the prevention of relapse following electroconvulsive therapy: a randomized controlled trial. JAMA. 2001 285:1299–1307. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Keck PE Jr, and Macfadden W. et al. A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry. 2005 162:1351–1360. [DOI] [PubMed] [Google Scholar]
- Cole DP, Thase ME, and Mallinger AG. et al. Slower treatment response in bipolar depression predicted by lower pretreatment thyroid function. Am J Psychiatry. 2002 159:116–121. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, and Sellaro R. et al. Recurrence of bipolar disorders and major depression: a life-long perspective. Eur Arch Psychiatry Clin Neurosci. 2003 253:236–240. [DOI] [PubMed] [Google Scholar]
- Altshuler L, Kiriakos L, and Calcagno J. et al. The impact of antidepressant discontinuation versus antidepressant continuation on 1-year risk for relapse of bipolar depression: a retrospective chart review. J Clin Psychiatry. 2001 62:612–616. [DOI] [PubMed] [Google Scholar]
- Altshuler L, Suppes T, and Black D. et al. Impact of antidepressant discontinuation after acute bipolar depression remission on rates of depressive relapse at 1-year follow-up. Am J Psychiatry. 2003 160:1252–1262. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Bowden CL, and Sachs G. et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently depressed patients with bipolar I disorder. J Clin Psychiatry. 2003 64:1013–1024. [DOI] [PubMed] [Google Scholar]
- Bowden CL, Calabrese JR, and Sachs G. et al. A placebo-controlled 18-month trial of lamotrigine and lithium maintenance treatment in recently manic or hypomanic patients with bipolar I disorder. Arch Gen Psychiatry. 2003 60:392–400. [DOI] [PubMed] [Google Scholar]
- Swann AC, Bowden CL, and Calabrese JR. et al. Mania: differential effects of previous depressive and manic episodes on response to treatment. Acta Psychiatr Scand. 2000 101:444–451. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Ernst CL.. Features associated with the delayed initiation of mood stabilizers at illness onset in bipolar disorder. J Clin Psychiatry. 2002;63:985–991. doi: 10.4088/jcp.v63n1105. [DOI] [PubMed] [Google Scholar]