Abstract
Objective: To determine whether children with attention-deficit hyperactivity disorder (ADHD) and learning disabilities respond differently to methylphenidate (MPH) compared with children with ADHD only. Methods: We conducted a prospective, double-blind, placebo-controlled, randomized, 2-week crossover trial of MPH, during which response to MPH was assessed. Learning ability was appraised using the Wide Range Achievement Test, Revised (WRAT-R), for English-speaking students and the Test de rendement pour francophones for French-speaking students. The study was conducted at the Douglas Hospital, a McGill University–affiliated teaching hospital in Montréal. Ninety-five children, aged 6–12 years, who met the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), criteria for ADHD participated in the study, which ran from 2001 to 2004. The outcome measure used was the Consensus Clinical Response, an indicator of the degree of clinical improvement shown when taking MPH. Results: The proportion of children with learning disabilities who responded to MPH (55%) was significantly smaller (χ21 = 4.5, p = 0.034) than the proportion of children without learning disabilities who responded adequately to MPH (75%). This difference was mainly because of children with mathematics disability being particularly unresponsive to MPH (χ21 = 4.5, p = 0.034). Children with reading disability did not show this pattern of poor response (χ21 = 1.0, p = 0.33). Conclusion: Children with ADHD and comorbid learning disability tended to respond more poorly to MPH. In particular, children with disability in mathematics responded less to MPH than those without disability in mathematics. Additional therapy may be indicated for this group of patients.
Medical subject headings: attention deficit disorder with hyperactivity, learning disorders, methylphenidate
Abstract
Objectif : Savoir si les enfants qui ont un trouble d'hyperactivité avec déficit de l'attention (THADA) et des difficultés d'apprentissage réagissent différemment au méthylphénidate (MPH) comparativement aux enfants qui ont un THADA seulement. Méthodes : Nous avons procédé à une étude prospective croisée à double insu sur le MPH, contrôlée par placebo, randomisée et d'une durée de deux semaines, au cours desquelles on a évalué la réaction au MPH. On a évalué la difficulté d'apprentissage au moyen du Wide Range Achievement Test, Revised (WRAT-R), pour les élèves anglophones et du Test de rendement pour francophones pour les élèves francophones. L'étude s'est déroulée à l'Hôpital Douglas, hôpital d'enseignement affilié à l'Université McGill de Montréal. Quatre-vingt-quinze enfants âgés de 6 à 12 ans qui satisfaisaient aux critères du Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV), pour le THADA ont participé à l'étude, qui a duré de 2001 à 2004. On a utilisé comme mesure de résultats le Consensus Clinical Response, indicateur du degré d'amélioration clinique manifestée lorsque les sujets prennent le MPH. Résultats : Le pourcentage des enfants atteints de difficultés d'apprentissage qui ont répondu au MPH (55 %) était beaucoup plus faible (χ21 = 4,5, p = 0,034) que celui des enfants sans difficultés d'apprentissage qui ont répondu adéquatement au MPH (75 %). Cet écart était attribuable principalement au fait que les enfants qui ont des difficultés en mathématiques sont particulièrement insensibles au MPH (χ21 = 4,5, p = 0,034). Ceux qui avaient des difficultés de lecture n'ont pas manifesté cette tendance à une mauvaise réponse (χ21 = 1,0, p = 0,33). Conclusion : Les enfants qui avaient un THADA et une difficulté d'apprentissage comorbide avaient tendance à répondre moins bien au MPH. Les enfants qui avaient des difficultés en mathématiques en particulier répondaient moins au MPH que ceux qui n'avaient pas ce problème. Une thérapie supplémentaire peut être indiquée dans le cas de ce groupe de patients.
Introduction
Attention-deficit hyperactivity disorder (ADHD) is a prevalent psychiatric disability in children, affecting 8%–12% worldwide.1 The cardinal features of ADHD are hyperactivity, impulsivity and inattention. Neurocognitive studies have indicated that these behavioural abnormalities in children with ADHD may occur as a result of executive control dysfunction.2 This disorder of executive control results in poor behavioural self-regulation, preventing the devising of approaches to performing and carrying out new tasks.3–5
Although the precise pathological mechanisms implicated in this disorder are not known, there are several lines of evidence implicating the frontostriatal pathway and its associated mesocortical dopamine systems.1,6 Indeed, children with ADHD have been shown to have a lack of or delay in the maturity of frontostriatal circuitry.7,8 In addition, structural imaging studies have reported an appreciably smaller volume of the right frontal cortex in subjects with ADHD associated with impaired response inhibition.9,10
The term learning disability refers to problems with reading, spelling, vocabulary and arithmetic. Mathematics mainly involves the parietal, prefrontal and cingulate areas of the brain,11 and particularly the intraparietal sulcus.12 Disruption of the neural circuits in these areas results in number concept difficulties, counting-skill deficits, difficulties with arithmetic skills, procedural disorders, memory disorders and visual– spatial deficits.13 Broca's area, Wernicke's area, the visual cortex and angular gyrus are parts of the brain involved in reading. Lesions in these areas can lead to deficiencies in vocabulary storage, reasoning, concept formation and interpretation.14
Learning disabilities affect about the same percentage of the population as ADHD.15 The degree to which these 2 populations overlap could be as high as 45%.16 However, genetic epidemiological studies suggest that these 2 disorders are independently transmitted in families.17
Although the underlying neurocognitive mechanisms of learning disabilities and ADHD may be different,18 it has been suggested that children with ADHD and learning disabilities may have a common frontal lobe dysfunction.2 In a study by Lazar and Frank,2 the ADHD and learning disability and the learning disability–only groups performed worse than the ADHD-only group on tests of attention– inhibition–cueing, working memory and problem solving. Shaywitz et al19 arrived at the same conclusion from their research, finding ADHD and learning disabilities (especially reading disability) to be distinct disorders identified by separate executive impairments and specific processing skills. Children with comorbid ADHD and reading disability were found to have a combination of cognitive abnormalities observed in children with a reading disability only and in children with ADHD only, suggesting that the association between ADHD and reading disability may arise from a combination of factors that are involved in both of these disorders.20 In contrast to reading disability, which has been well studied in the context of ADHD, disability in mathematics has been poorly investigated and is in need of further research to establish its causal basis and relation to ADHD. Swanson21 determined that both executive and phonological processes are of importance in mathematical problem solving in children with learning disabilities. It has also been reported that children with ADHD and mathematics disability have greater deficits in executive functions compared with children with ADHD but no mathematics disability.22 Psychostimulant drugs, particularly methylphenidate (MPH), are the most commonly prescribed drugs in children for the treatment of ADHD. In the largest controlled study of treatment efficacy, the Multimodal Treatment Study of Children with ADHD, it was shown that medication alone or medication associated with intensive behavioural therapy were equally effective in reducing the core symptoms of ADHD.23 It is also clear that not all children (and in the same child, not all dimensions of psychopathology24) benefit to the same extent from this medication. Although cases that are refractory to treatment are rare,25 only 70% of the children treated with psychostimulant drugs present a clinically significant improvement.26
It has been reported that children with ADHD receiving psychostimulant medication had improved executive control compared with children with ADHD who were not receiving medication.27,28 Tannock et al29 were the first to demonstrate improvement in response inhibition by MPH in pediatric ADHD. More recently, Mehta et al30 showed that MPH enhances cerebral blood flow to the dorsolateral prefrontal cortex, a cortical region believed to be of primary importance in executive control. If the therapeutic response of MPH is influenced by the modulation of executive control functions, one would expect that patients with both ADHD and learning disabilities, particularly those with arithmetic disability, would present poorer improvement under MPH treatment. The purpose of this research is to compare patients diagnosed with ADHD and learning disabilities with those without learning disabilities regarding their therapeutic response to MPH.
Methods
Children were recruited sequentially from the Severe Disruptive Behaviour Disorders Program and from the outpatient clinics at the Douglas Hospital, a psychiatric teaching hospital in Montréal. Ninety-five percent of those subjects invited by the research assistants to participate in our study agreed to take part. They had no considerable psychosocial intervention preceding the trial.
The sample comprised 81 boys and 14 girls aged between 6 and 12 years. Fifty-three percent of the subjects were English-speaking, and 47% were French-speaking.
Two experienced child psychiatrists substantiated the diagnoses of ADHD according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV),31 that were based on clinical examination, information collected from different sources and a structured interview using the Diagnostic Interview Schedule for Children Version IV (DISC-IV). Children with an IQ lower than 70 on the Wechsler Intelligence scale for Children-III,32 a history of Tourette's syndrome, pervasive developmental disorder or psychosis were excluded from the study. Those with previous intolerance or allergic reaction to MPH were also excluded. Sixty-six percent of children had previously been on some medication; this was ceased 2 weeks before starting the trial.
Parents signed informed consent, and all the children agreed to participate in this 2-week, double-blind, placebo-controlled, crossover, randomized MPH trial.
After an initial week of baseline assessments, children randomly received either placebo or 0.5 mg/kg of body weight of MPH divided in 2 equal doses (morning and noon) daily over a 1-week period and crossed over in the second week. Randomization was completed by a research psychologist who did not have any contact with the patients. MPH and placebo were prepared in coloured gelatin capsules by a clinical pharmacist who was not otherwise involved in the study. No important adverse events or side effects were noted.
A series of ecological and laboratory measures were performed during the MPH and placebo weeks. Behaviour at school was evaluated by asking teachers to complete the Conners Global Index–Teacher's Version (CGI-T),33 and parents assessed behaviour at home using Conners' Global Index–Parent Version (CGI-P)34 on the Sunday after giving the children their medication on the weekend. Both scales determined the frequency of 10 types of ecologically relevant behaviour. In the morning of the third day of each week, the children came to the laboratory. An experienced research assistant administered the Clinical Global Impression Scale,35 which evaluates severity of illness. The Restricted Academic Situation Scale (RASS), a laboratory measure identified as a sensitive tool in the detection of ADHD in children,36 was used to assess the following behaviours: being off-task, fidgeting, vocalizing, playing with objects and being out of seat. The Conners' Continuous Performance Task (CPT)37 was used to measure impulse control along with sustained attention. The RASS and the CPT were assessed before and 60 minutes after the administration of the medication. The effect of the medication on global behaviour was assessed by the Clinical Global Impression Scale for improvement by the same research assistant.
At the conclusion of the trial and before breaking the code, the research team (2 experienced child psychiatrists, a psychologist, child care workers and research assistants) attributed the consensus clinical response (CCR) score based on overall degree of improvement for each week of the trial on the following 4-point Likert scale: large response = 3, moderate response = 2, mild response = 1 and nonresponder = 0. The CCR combined all available ecological and laboratory measures in light of relevant information, such as the reliability of parents or if the child was feeling sick on the day of the assessment. The CCR takes into account multiple factors that vary from objective and acute measures like RASS to personal impressions of clinicians, researchers and parents.
To evaluate learning disability, subjects wrote the Wide Range Achievement Test, Revised (WRAT),37 or the Test de rendement pour francophones (TRF),38 according to their language of schooling, at some point during the study separate from the medication trial.
The WRAT assessed academic performance and consisted of reading, spelling and arithmetic subtests. The standard scores obtained in these subtests were ascribed a grade level. The WRAT is widely used to assess a child's scholastic ability.39 The TRF measures the scholastic abilities of subjects whose primary language is French. There are different tests with the level of difficulty corresponding to the 3 stages of schooling from grades 1 to 12. The student is given the test appropriate to his or her grade level. The student's scores in the vocabulary, written comprehension and arithmetic subsections are also translated into grade equivalents.
If there was a difference in reading or mathematics grade levels greater than or equal to 2 years with respect to expected grade level given the age of the child, the child was considered to have a learning disability in the subject.
In order to test for the association between learning disabilities and therapeutic response to MPH, we separated the patients into 2 groups according to their CCR (CCR = 0 or 1 and CCR = 2 or 3) and whether they had a learning disability or not. We used a χ2 statistic with the appropriate degrees of freedom in order to test for the association between the diagnostic group and response to MPH as determined by the CCR. We also analyzed the data by contrasting children with ADHD and mathematics disability (regardless of their reading disability status) with children without mathematics disability (regardless of their reading disability status) on the one hand and children with ADHD and reading disability (regardless of their mathematics disability status) with children without reading disability (regardless of their mathematics disability status). This analysis was carried out to determine whether a specific learning disability (reading disability or mathematics disability) has a stronger relation to therapeutic response to MPH.
The clinical and demographic characteristics of the children belonging to the 2 diagnostic groups (ADHD with learning disability and ADHD without learning disability) were compared using appropriate statistics (analysis of variance [ANOVA] or χ2) depending on the nature of the variable.
Results
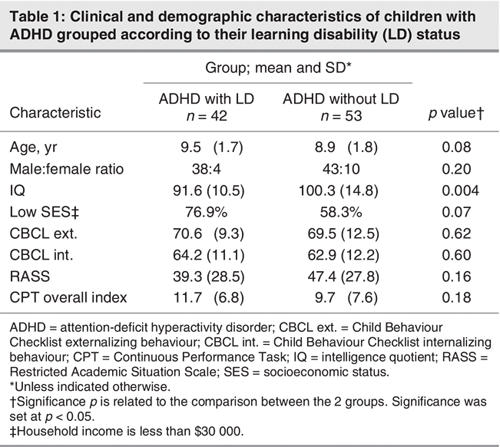
Table 1 shows the demographic and clinical characteristics of the children grouped according to their learning disability status. All variables were similar across the 2 diagnostic groups, except for IQ. Children with ADHD and a learning disability had a significantly lower IQ compared with children with ADHD and without a learning disability (mean 91.6, standard deviation [SD] 10.5 v. mean 100.3, SD 14.8; F1,76 = 8.6, p = 0.004).
Table 1
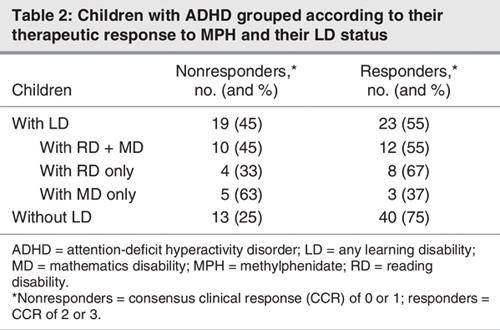
The overall proportion of therapeutic response as assessed by the CCR was 66%, which is in line with previous reports on response to MPH.23 Table 2 shows the proportion of responders and nonresponders to MPH in children with learning disabilities and those without learning disabilities. The proportion of children with learning disabilities (55%) who responded positively to MPH was significantly lower than the proportion of children without learning disabilities (75%) who responded to MPH. Conversely, there were more nonresponders in the group of children with learning disabilities (45%) compared with children without learning disabilities (25%). These differences were statistically significant (χ21 = 4.5, p = 0.034).
Table 2
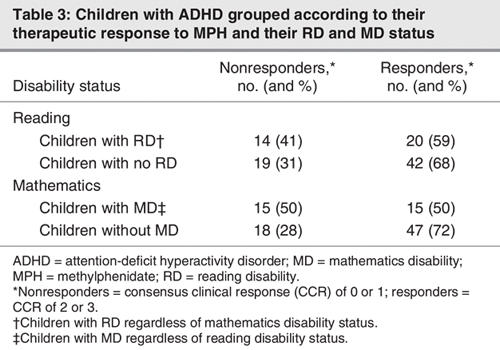
In order to explore whether the association of learning disability and therapeutic response to MPH is at least partially specific to mathematics disability or reading disability, we contrasted children with ADHD and mathematics disability (regardless of their reading disability status) with children without mathematics disability (regardless of their reading disability status) on the one hand and children with ADHD and reading disability (regardless of their mathematics disability status) with children without reading disability (regardless of their mathematics disability status) (Table 3). The results of these analyses suggest that the association between learning disability and therapeutic response to MPH may be mediated through mathematics disability. Indeed, the association between mathematics disability and therapeutic response was significant (χ21 = 4.5, p = 0.034), whereas the association between reading disability and therapeutic response was not (χ21 = 1.0, p = 0.33).
Table 3
In order to rule out the possibility that the observed association between mathematics disability and therapeutic response to MPH was not mediated by different levels of attention or hyperactivity problems displayed by each group of subjects, we compared children with ADHD and mathematics disability with those with ADHD and no mathematics disability. No significant differences (F1,91 = 0.5, p = 0.5) were found on the mean number of DISC inattention items for the children with mathematics disability (mean 7.1 [SD 1.8]) compared with those with no mathematics disability (mean 6.7 [SD 2.4]); no significant differences (F1,91 = 0.18 , p = 0.7) were found on the mean number of DISC hyperactivity items for children with mathematics disability (mean 6.4 [SD 2.5]) compared with those with no mathematics disability (mean 6.2 [SD 2.4]).
Discussion
A substantial proportion of children with ADHD have comorbid learning disabilities. Although these 2 neurodevelopmental disorders seem to be distinct in nature, they share some of their pathological determinants, because executive function deficits have been reported in both. Moreover, it has been noted that children with ADHD and learning disabilities, particularly those with disability in mathematics, have higher executive dyscontrol compared with children with pure forms of ADHD. Under the assumption that MPH exerts its effects through modulation of executive function, the goal of our study was to determine whether children with ADHD and learning disabilities have a poorer therapeutic response to MPH compared with children with ADHD only.
Past studies have tended to focus on one form of learning disability or the other, whereas looking at both together makes the analysis more challenging. We considered mathematics and reading disability separately, because the neurocognitive determinants of these 2 abilities may be at least partially distinct. Grade equivalents were assessed using the WRAT and TRF test score conversion scales. The grade equivalents were confirmed using the evaluations of teachers and psychiatrists, thus giving a very accurate picture of the student's capacity for learning.
Studies by Tirosh et al18 suggest that ADHD with a learning disability is different from a learning disability alone from a pathogenetic point of view, because their neurocognitive patterns differ. Therefore, it would seem probable that children with ADHD and learning disabilities have altered neurocircuitry that causes them to respond differently to MPH from their peers with ADHD alone. In line with this hypothesis, we found that children with ADHD and a learning disability in general do not perform as well on MPH (55% response rate) as children with ADHD without learning disabilities (75% response rate). However, when looking at reading disabilities in particular, 59% of children with ADHD and a reading disability showed improvement with respect to ADHD symptoms when treated with MPH, a response rate that was not significantly different from that of children with ADHD and no reading disability (68%). This corroborates the results of a previous study that found a similar response to MPH in children with ADHD and a reading disability and those with ADHD only.40
Our results show that the symptoms of children with ADHD and a learning disability in mathematics do not show as much improvement in response to MPH as the symptoms of children with ADHD without disability in mathematics, with a 50% response rate for the former group versus 72% for the latter. This finding probably accounts for the difference in therapeutic response to MPH in children with ADHD and a learning disability as compared with those without a learning disability. This can be explained by the postulated higher degree of executive dysfunction in children with a mathematics disability.
An analysis of inattention and hyperactivity was also carried out in order to see whether these 2 manifestations of ADHD were related to the level of learning disability in either reading or mathematics. The degree of inattention and hyperactivity in children with ADHD and children with ADHD and learning disabilities was not significantly different. Therefore, children with learning disabilities and ADHD did not simply have higher levels of the 2 characteristic symptoms related to ADHD, and the presence of comorbid learning disabilities could not be explained simply by an increase in inattention or hyperactivity in these children.
The interpretation of this study's results should take into consideration some methodological limitations. First, because of the bilingual nature of our patient population, we could not administer the same testing to all our students. However, we tried to mitigate this possibly distorting factor by using language-specific instruments and ascertaining grade levels with teachers' evaluations. Second, the definition of a learning disability as being a 2-year delay in reading or mathematics may not be adequate for all ages. For example, it is sometimes difficult to tell whether a child under the age of 8 has a learning disability for certain. In these cases, the 2-year delay definition of learning disability did not hold; therefore, we again placed emphasis on assessing learning status using teachers' evaluations and a psychiatrist's evaluations.
Third, because some study subjects had a comorbid reading disability and mathematics disability, it is probable that a skill required mainly for reading (such as vocabulary) has a negative effect on mathematical ability in a nonspecific way. This could have been a minor limitation, in that it could have influenced the labelling of a student as disabled in mathematics, whereas in fact they are not. Fourth, we conducted a total of 3 tests, which may have increased the possibility of a type I error in our study. Although a Bonferroni correction (nominal p = 0.016) may protect against type I error, we felt that this was too conservative as the 3 tests were not independent. However, a larger sample would be necessary to confirm the results of the present study. Finally, a higher dose of MPH possibly could have been beneficial in children with ADHD and a comorbid mathematics disability. However, in view of the controversial data regarding the relation between cognitive performances and the dose of MPH,41,42 more clinical studies with various dosages of MPH are warranted for patients with ADHD and a mathematics disability.
In conclusion, our study shows that MPH has a significantly lesser rate of efficacy in treating children with ADHD and a learning disability, particularly in mathematics. Our study's findings of decreased efficacy of MPH in children with ADHD and a concomitant mathematics disability will, we hope, stimulate investigations into alternative approaches to ADHD symptomatology in these children.
Acknowledgments
We would like to thank the Canadian Institutes of Health Research (CIHR) for its financial support to this research project and Johanne Bellingham, Anna Polotskaia and Nicole Pawliuk for their help in data collection.
Footnotes
Contributors: Drs. Grizenko and Joober conceived and designed the study; Dr. Grizenko and Ms. Ter-Stepanian acquired the data; Drs. Grizenko, Bhat and Joober and Mr. Schwartz analyzed the data. Drs. Grizenko and Bhat drafted the article; Drs. Grizenko and Joober, Mr. Schwartz and Ms. Ter-Stepanian critically reviewed the article. All authors gave final approval for the article to be published.
Competing interests: None declared.
Correspondence to: Dr. Natalie Grizenko, Bond Pavilion, Douglas Hospital, 6875 LaSalle Blvd., Montréal QC H4H 1R3; fax 514 762-3041; grinat@douglas.mcgill.ca
References
- 1.Biederman J, Faraone SV. Attention deficit hyperactivity disorder. Lancet 2005;366:237-48. [DOI] [PubMed]
- 2.Lazar JW, Frank Y. Frontal systems dysfunction in children with attention-deficit hyperactivity disorder and learning disabilities. J Neuropsychiatry Clin Neurosci 1998;10:160-7. [DOI] [PubMed]
- 3.Westby C, Watson S. Perspectives on attention-deficit hyperactivity disorder: executive functions, working memory, and language disabilities. Semin Speech Lang 2004;25:241-54. [DOI] [PubMed]
- 4.Schachar R, Tannock R, Logan G. Inhibitory control, impulsiveness, and attention deficit hyperactivity disorder. Clin Psychol Rev 1993;13:721-39.
- 5.Scheres A, Oosterlaan J, Geurts H, et al. Executive functioning in boys with ADHD: primarily an inhibition deficit? Arch Clin Neuropsychol 2004;19:569-94. [DOI] [PubMed]
- 6.Sullivan RM, Brake WG. What the rodent prefrontal cortex can teach us about attention-deficit/hyperactivity disorder: the critical role of early developmental events on prefrontal function. Behav Brain Res 2003;146:43-55. [DOI] [PubMed]
- 7.Durston S, Tottenham NT, Thomas KM, et al. Differential patterns of striatal activation in young children with and without ADHD. Biol Psychiatry 2003;53:871-8. [DOI] [PubMed]
- 8.Schulz KP, Fan J, Tang CY, et al. Response inhibition in adolescents diagnosed with attention deficit hyperactivity disorder during childhood: an event-related FMRI study. Am J Psychiatry 2004; 161:1650-7. [DOI] [PubMed]
- 9.Casey BJ, Castellanos FX, Giedd JN, et al. Implication of right frontostriatal circuitry in response inhibition and attention-deficit/ hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1997;36:374-83. [DOI] [PubMed]
- 10.Semrud-Clikeman M, Steingard RJ, Filipek P, et al. Using MRI to examine brain-behavior relationships in males with attention deficit disorder with hyperactivity. J Am Acad Child Adolesc Psychiatry 2000;39:477-84. [DOI] [PubMed]
- 11.Dehaene S, Spelke E, Pinel P, et al. Sources of mathematical thinking: behavioral and brain-imaging evidence. Science 1999;284:970-4. [DOI] [PubMed]
- 12.Dehaene S, Piazza M, Pinel P, et al. Three parietal circuits for number processing. Cognit Neuropsychol 2003;20:487-506. [DOI] [PubMed]
- 13.Geary DC. Mathematical disorders: an overview for educators. International Dyslexia Association. Perspectives 2000;26:6-9.
- 14.Sousa DA. How the special needs brain learns. Thousand Oaks (CA): Corwin; 2001.
- 15.Shaywitz SE, Shaywitz BA, Fletcher JM, et al. Prevalence of reading disability in boys and girls: results of the Connecticut longitudinal study. JAMA 1990;264:998-1001. [PubMed]
- 16.Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit with conduct, depressive, anxiety and other disorders. Am J Psychiatry 1991;148:564-77. [DOI] [PubMed]
- 17.Faraone SV, Biederman J, Lehman BK, et al. Evidence for the independent familial transmission of attention deficit hyperactivity disorder and learning disabilities: results from a family genetic study. Am J Psychiatry 1993;150:891-5. [DOI] [PubMed]
- 18.Tirosh E, Berger J, Cohen-Ophir M, et al. Learning disabilities with and without attention deficit hyperactivity disorder: parent's and teacher's perspective. J Child Neurol 1998;13:261-70. [DOI] [PubMed]
- 19.Shaywitz B, Fletcher J, Holahan J, et al. Interrelationships between reading disability and attention deficit hyperactivity disorder. Child Neuropsychology 1995;1:170-86.
- 20.Willcutt EG, Pennington BF, Olson RK, et al. Neuropsychological analyses of comorbidity between reading disability and attention deficit hyperactivity disorder: in search of the common deficit. Dev Neuropsychol 2005;27:35-78. [DOI] [PubMed]
- 21.Swanson HL. Mathematical problem solving and working memory in children with learning disabilities: both executive and phonological processes are important. J Exp Child Psychol 2001; 79:294-321. [DOI] [PubMed]
- 22.Seidman LJ, Biederman J, Monuteaux MC, et al. Learning disabilities and executive dysfunction in boys with attention-deficit/ hyperactivity disorder. Neuropsychology 2001;15:544-56. [DOI] [PubMed]
- 23.MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 1999;56:1073-86. [DOI] [PubMed]
- 24.Swanson JM, Wigal SB, Udrea D, et al. Evaluation of individual subjects in the analog classroom setting: I. Examples of graphical and statistical procedures for within-subject ranking of responses to different delivery patterns of methylphenidate. Psychopharmacol Bull 1998;34:825-32. [PubMed]
- 25.Elia J, Borcherding BG, Rapoport JL, et al. Methylphenidate and dextroamphetamine treatments of hyperactivity: Are there true nonresponders? Psychiatry Res 1991;36:141-55. [DOI] [PubMed]
- 26.Spencer T, Biederman J, Wilens T, et al. Pharmacotherapy of attention-deficit hyperactivity disorder across the life cycle. J Am Acad Child Adolesc Psychiatry 1996;35:409-32. [DOI] [PubMed]
- 27.Barnett R, Maruff P, Vance A, et al. Abnormal executive function in attention deficit hyperactivity disorder: the effect of stimulant medication and age on spatial working memory. Psychol Med 2001;31:1107-15. [DOI] [PubMed]
- 28.Konrad K, Gunther T, Hanisch C, et al. Differential effects of methylphenidate on attentional functions in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 2004;43:191-8. [DOI] [PubMed]
- 29.Tannock R, Schachar RJ, Carr RP, et al. Effects of methylphenidate on inhibitory control in hyperactive children. J Abnorm Child Psychol 1989;17:473-91. [DOI] [PubMed]
- 30.Mehta MA, Owen AM, Sahakian BJ, et al. Methylphenidate enhances working memory by modulating discrete frontal and parietal lobe regions in the human brain. J Neurosci 2000;20:1-6. [DOI] [PMC free article] [PubMed]
- 31.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV). Washington: The Association; 2002.
- 32.Wechsler D. Wechsler Intelligence Scale for Children. 3rd ed. San Antonio (TX) Psychological Corporation; 1991.
- 33.Conners CK, Sitarenios G, Parker JD, et al. Revision and restandardization of the Conners Teacher Rating Scale (CTRS-R): factor structure, reliability and criterion validity. J Abnorm Child Psychol 1998;26:279-91. [DOI] [PubMed]
- 34.Conners CK, Sitarenios G, Parker JD, et al. The revised Conners Parent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 1998;26:257-68. [DOI] [PubMed]
- 35.National Institute of Mental Health. CGI (Clinical Global Impressions) scale. Psychopharmacol Bull 1985;21:839-41
- 36.Milich R, Loney J, Landau S. Independent dimensions of hyperactivity and aggression: a validation with playroom observation data. J Abnorm Psychol 1982;91:183-98. [DOI] [PubMed]
- 37.Conners CK. Conner Continuous Performance Test program. Toronto: MHS; 1995.
- 38.Sarrazin G. Test de rendement pour francophones Toronto: Harcourt & Brace; 1995.
- 39.Jastak S, Wilkinson GS. The Wide Range Achievement Test, revised. Wilmington (DE): Jastak Associates; 1985.
- 40.Dykman RA, Ackerman PT. Attention deficit disorder and specific reading disability: separate but often overlapping disorders. J Learn Disabil 1991;24:96-103. [DOI] [PubMed]
- 41.Kupietz SS, Bartlik B, Angrist B, Winsberg BG. Psychostimulant plasma concentration and learning performance. J Clin Psychopharmacol 1985;5:293-5. [DOI] [PubMed]
- 42.Pearson DA, Santos CW, Casat CD, et al. Treatment effects of methylphenidate on cognitive functioning in children with mental retardation and ADHD. J Am Acad Child Adolesc Psychiatry 2004;43:677-85. [DOI] [PubMed]


