The World Health Organization considers that severe migraine can be as disabling as quadriplegia.1 The disorder affects as many of 15% of adults in North America and Western Europe and is probably one of the commonest reasons for patients to see their doctors. Traditionally, headache is given little time in medical teaching, but headache science is advancing rapidly, fuelled by developments in treatment and neuroscience, and there is a sense of excitement perhaps unrivalled in neurology. Many recent advances have particular relevance to clinical practice in terms of both diagnosis and management; I will highlight these. Interested readers should see recent monographs listed in the Further reading box for more detailed accounts of the management of headache disorders.
Methods
I based my selection of topics for this review on clinical themes that arise from referrals to the Headache Group at the National Hospital for Neurology and Neurosurgery. Thus the primary driver for the review is clinical practice. Information has come particularly from my reading large sections of a major reference work on headache as an editor (see Further reading box), and from the major headache journals, Cephalalgia and Headache, which I hand searched for the past decade. These sources are supplemented by PubMed searches and information from the most recent congress of the International Headache Society in Kyoto (10-12 October 2005). Some aspects of this review are based on a recent publication.2
Headache classification—improving and simplifying the diagnosis of migraine
The development and promulgation of the International Headache Society's diagnostic criteria in 1988 was an important milestone, giving clear guidance and having widespread acceptance. Migraine was defined by the component clinical parts of an attack so that the most important tool for the clinician was a good history (box 1). The second edition of the international classification of headache disorders (ICHD-II)3 has seen fine tuning of the migraine classification and refining of important issues around frequent headache. Some issues merit highlighting.
Summary points
Headache is a common, disabling clinical problem
Migraine is the commonest form of disabling headache presenting to doctors
Biologically pure, tension-type headache is rarely a cause for medical consultation
Migraine is a brain disorder involving abnormal sensory processing
Migraine can often be well managed by a combination of acute and preventive treatment
Childhood migraine
The classification of migraine has been modified for children by allowing headaches with fewer features. It seems clear that migraine is common in children, that the attacks are shorter than in adults, and that associated attack features, such as throbbing or unilateral pain or the presence of photophobia and phonophobia, are less common. Most adults who attend their general practitioner with disabling primary headache have migraine,4 and in my experience migraine is also the commonest basis for referral to a headache clinic in children. Differentiating between headaches with few features is the most fundamental clinical problem in managing headaches, and I will return to it below as the principles are generic.
In addition to straightforward migraine, further thought has been given to the childhood periodic syndromes—cyclical vomiting, abdominal migraine, and benign paroxysmal vertigo of childhood—which so often portend migraine in adolescence and adulthood. These syndromes need careful evaluation, although it seems clear that they have a strong association with migraine.
Chronic daily headache
Perhaps the most controversial issue in headache classification and management is how to deal with the problem of frequent, daily or near daily headache (box 2). Some 5% of North American and Western European populations have headache on at least 15 days a month for, on average, four or more hours a day. If one includes shorter lasting headaches, then chronic daily headache is simply a syndrome defined by frequency of headache.5 It is not just tension-type headache, nor is it all just due to medication overuse. Chronic daily headache is often incorrectly equated with the concept of transformed migraine, a term now superseded by the definition of chronic migraine, which is a subset of chronic daily headache (box 3). When a doctor gets a history of frequent headache they need to pursue its basis.
Box 1: Simplified diagnostic criteria for migraine (from ICHD-II3)
Repeated attacks of headache lasting 4-72 hours that have these features
A: Normal physical examination
B: No other reasonable cause for the headache
C: At least two of
Unilateral pain
Throbbing pain
Aggravation of pain by movement
Moderate or severe intensity of pain
D: At least one of
Nausea or vomiting
Photophobia and phonophobia
Core issues for general practitioners
In clinical practice there seem to be two core issues for general practitioners: who has sinister or secondary headache, and how can migraine be differentiated from tension-type headache.
Secondary headache
Although little new development has occurred in this area, some coverage is appropriate. In determining the likelihood of secondary headache, the most crucial clinical feature to elicit is the length of the history. Patients with a short history require prompt attention and may need quick investigation and management. Patients with a longer history generally require time and patience rather than speed. Certain features of the presentation demand attention:
Pain of sudden onset
Fever
Marked change in pain character or timing
Neck stiffness
Pain associated with higher centre complaints
Pain associated with neurological disturbance, such as clumsiness or weakness
Pain associated with local tenderness, such as of the temporal artery.
If a positive diagnosis that is benign cannot be made, patients with a headache that is of recent onset or with neurological signs require brain imaging with computed tomography or magnetic resonance imaging. Patients with a history of recurrent headache for a year or more that fulfils the criteria for migraine (box 1), and with a normal physical examination, rarely show positive results on brain imaging (only about 1/1000 images). A brain tumour is rarely the cause of a headache, particularly so if it is isolated and long term.7 Severity is a poor marker of secondary headache, with the most severe and disabling headaches being primary headaches.
Differentiating migraine and tension-type headache
There are two key ways to differentiate migraine from tension-type headache. Firstly, migraine is in essence head pain with associated features whereas tension-type headache is featureless head pain. This small compromise of the International Headache Society criteria results in a pragmatic test that generally yields a useful clinical answer. Secondly, migraine has biological signatures that tension-type headache does not seem to, namely the inherited tendency to headache when confronted with particular triggers (table 1). Determining whether a patient has a family history of headache, especially if it is migraine, and questioning about trigger factors help to differentiate migraine from tension-type headache. Details of a patient's susceptibility to triggers also provides important information about the patient's biology and offers a management strategy in terms of reducing headache by sensible behavioural change. Testing the reliability of this approach to distinguishing migraine from tension-type headache would be extremely useful but is complicated by there being no known biological marker against which to judge the outcome. In clinical practice, however, erring on the side of diagnosing migraine has few drawbacks and offers many options for management.
Table 1.
Differentiating migraine from tension-type headache
| Characteristics | Migraine | Tension-type headache |
|---|---|---|
| Pain features of acute attacks | Throbbing
|
Boring or squashing
|
| Unilateral
|
Bilateral
|
|
| Worsening of pain with movement | No effect of head movement | |
| Associated features | Nausea or vomiting
|
None |
| Photophobia and phonophobia | ||
| Triggering factors | Altered sleep patterns (too little or too much)
|
Psychological stress |
| Skipping meals
|
||
| Overexertion
|
||
| Change in stress level (too much or relaxation)
|
||
| Excess afferent stimuli (such as bright lights)
|
||
| Weather change
|
||
| Chemical (delayed headache after alcohol or glyceryl trinitrate)
|
||
| Menstruation |
Box 2: Classification of chronic daily headache
Headache on ≥ 15 days a month that may be due to a range of underlying mechanisms and may be complicated by, or caused by, drug overuse
Primary headache
For >4 hours daily
Chronic migraine—An IHCD-II3 term for, in essence, migraine without aura for ≥ 15 days a month. Transformed migraine is a more useful term in clinical practice (box 3 has a current working definition)
Chronic tension-type headache
Hemicrania continua
New daily persistent headache—An IHCD-II3 term, but I find a more generic approach useful6
For <4 hours daily
Chronic cluster headache—Patients may have > 4 hours of headache a day, but the attacks themselves are generally < 4 hours duration
Chronic paroxysmal hemicrania
Short lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT)
Hypnic headache
Secondary headache (list not exhaustive)
Post-traumatic—Head injury, iatrogenic, post-infectious
Inflammatory—Giant cell arteritis, sarcoidosis, Behçet's syndrome
Chronic infection of the central nervous system
Medication overuse headache
Box 3: Chronic migraine (modified criteria of the ICHD-II3)
A: Current or prior headache fulfils criteria for migraine without aura (see box 1)
B: Headache on ≥ 15 days a month
C: At least 8 headache days a month for the previous 3 months fulfilling at least one of the following:
Criteria C and D for migraine without aura (see box 1)
Criteria C and D for migraine without aura with the exception of a single sub-criterion, and not meeting criteria for tension-type headache (see table 2)
Headache that the patient believes to be migraine and is relieved by a 5-HT1B/1D receptor agonist
D: Not attributable to another disorder, including medication overuse headache
Genetics of migraine—explaining to patients why they have the problem
It seems logical to suppose that all sufferers of primary headaches have a genetic predisposition that is in some way activated by physiological and other life events, such as puberty, although the only genetic associations yet identified are for migraine. Migraine genetics offer a useful tool in clinical practice for helping to explain to patients that they were born with a tendency to headache—by establishing that their parents also had headaches, or by pointing out that the triggers listed in table 1 do not produce headache universally, the doctor can explain the cause. This is useful in allaying fear and setting the groundwork for improving the problem.
The first concrete example of inherited migraine was the identification of missense mutations in the Cav2.1 subunit of the gene for the P/Q type, voltage gated, calcium channel on chromosome 19 in families with familial hemiplegic migraine.w1 Since then, other cases of familial hemiplegic migraine have been found to be caused by mutations in the ATP1A2 gene, which encodes the α2 subunit of the Na+/K+ pump,w2 and in the SCN1A gene for the neuronal voltage-gated sodium channel.w3
The overall message is of migraine as an ionopathy, a disorder based on abnormal ion channels whose strategic function and anatomical distribution in the brain determine the clinical phenotype. If genetics can explain why patients have headaches and what the biochemical disorder may be, then we can ask the question, “Where is the problem?” or, framed in the terms of classic neurology, “Where is the lesion?”
Pathophysiology of headache—where is the lesion?
Classic neurology, as promulgated by Gowers, sought to provide anatomical answers to clinical questions. This approach has been successful, but the problems of primary headache will need a physiological approach.w4 To some extent, human functional imaging starts to do this.
In the 1960s and '70s migraine was considered a vascular phenomenon and is still often referred to incorrectly as a vascular headache. Wolff summarised in his classic book the referral patterns of structures that produced intracranial pain, taking a view that migraine aura was due to vasoconstriction and that the subsequent headache was due to a reactive vasodilatation. Olesen debunked this link. The spreading depression theory points out that the changes in blood flow follow metabolic demand—vasoneuronal coupling.w5 Considering features of the attack that do not occur in all cases (such as nausea, photophobia, and phonophobia) or of the premonitory phase (such as yawning or diuresis), the vascular hypothesis seems unattractive.
The lesion should be considered a functional concept. What structure or network of structures would produce a syndrome whose core features are unilateral head pain and sensitivity to light, sound, smells, and head movement, as well as have the potential to alter brain blood flow, be influenced by sleep or changing sleep patterns, and alter broadly cortical function in terms of attention and concentration. Brainstem aminergic neurones, such as the noradrenergic neurones of the locus coeruleus, could potentially have these broad effects,w6 so the hypothesis would predict functional imaging changes in the brainstem, indeed in the pons.
Functional brain imaging in migraine
Positron emission tomography in acute migraine has shown activations in the rostral brainstem that persisted after successful treatment of the attack but are not present interictally.8 These changes are not seen in experimentally induced ophthalmic division pain9 or in other primary headaches, such as cluster headache10 or paroxysmal hemicrania (fig).11 Indeed, we and others have consistently observed activation in the dorsolateral pons in both spontaneous and triggered episodic migraine.12-15 Moreover, in chronic migraine, defined as migraine without aura that occurs on ≥ 15 days a month for more than six months,3 the same area of the dorsolateral pons is activated,16 suggesting that infrequent and frequent migraine are ends of a shared spectrum. Use of blood oxygen level dependent (BOLD) contrast functional magnetic resonance imaging holds the promise of studying single patients and determining the site of abnormal activation.w7 Moreover, magnetic resonance angiography has shown that the blood flow changes seen in migraine14 and cluster headache10 are simply a result of ophthalmic division pain,17,18 not a cause of the syndrome.
Figure 1.
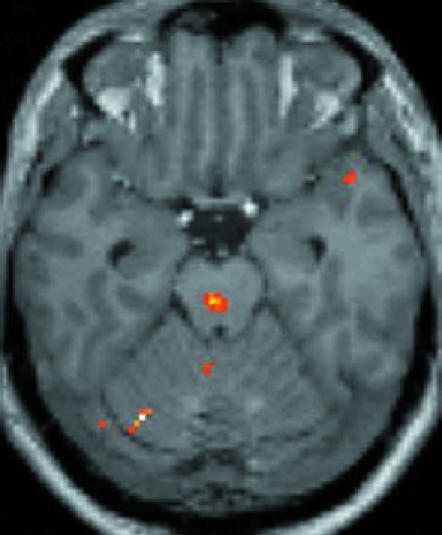
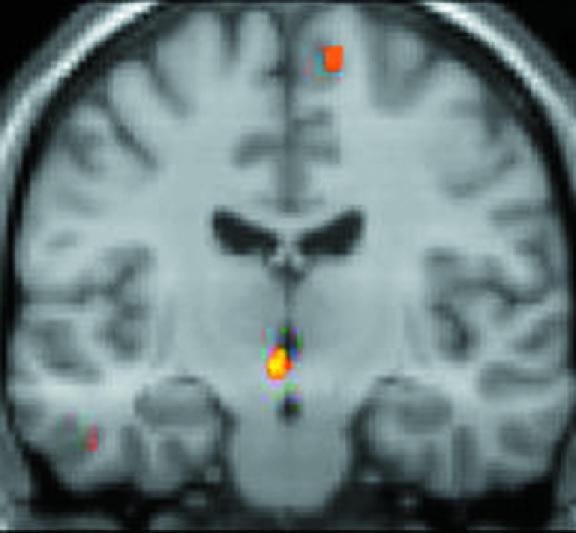
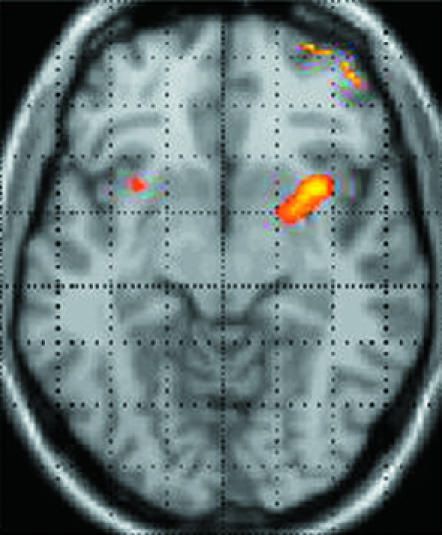
Positron emission tomography findings in migraine (left),14 cluster headache (centre),10 and experimentally induced head pain (right).9 Activation of rostral brainstem structures in migraine, and of posterior hypothalamic grey matter in cluster headache, seem relatively specific for the syndromes, as neither is seen in experimental ophthalmic division pain. The findings support the view that primary neurovascular headaches, migraine, and cluster headache are fundamentally disorders of the nervous system
Functional neuroimaging has recently shown that the changes in the dorsolateral pons in migraine lateralise with the attack: studies of typical migraine triggered by glyceryl trinitrate have revealed left sided brain activation in patients with left sided attacks, right sided activation in patients with right sided attacks, and bilateral activation in patients with bilateral pain.15 These data suggest that the dorsolateral pons is pivotal in the phenotypic expression of migraine. These changes in brain activation persisted after resolution of the pain with a triptan, were not present interictally, and were not seen in a control group who were scanned but in whom migraine did not develop. Moreover, the pontine change was not seen during the dull bilateral headache induced by glyceryl trinitrate in either controls or migraineurs.15 The extent to which the changes observed form part of a unique response to brain dysfunction elsewhere, or are themselves the pivotal changes, remains to be determined.
The implication of the studies for clinicians is to be able to tell patients that we are confident that the disorder is one that is localised in the brain. It seems clear that migraine is not a disorder of blood vessels but one of brain function. To this end we can assure patients who feel odd during attacks, perhaps have trouble concentrating, or simply feel a little befuddled that this is normal, indeed expected of a brain disorder of this type. More importantly, these insights must lead to new directions for the development of much needed new preventive treatments.
Migraine—what new treatments can we expect?
Triptans, selective 5-HT1B/1D receptor agonists, were the main advance in migraine treatment during the latter part of the 20th century. Many migraine sufferers were liberated in a way that they had not previously known, clinical trial guidelines were refined and revised, and clinical studies were well organised and uniform. After sumatriptan, came zolmitriptan, naratriptan, rizatriptan, almotriptan, eletriptan, and frovatriptanw8; donitriptan has now finished preclinical development. Ergotamine, the mainstay of specific acute treatment for most of the 20th century after its initial description in the 19th, now has few indications in which it is the treatment of choice.w9 It is clear what patients want—rapid, complete, and consistent pain reliefw10— but not entirely established how they make preference decisions among the available treatments.w11 What is established is that most patients do have preferences for individual triptans when asked. Box 4 sets out some situations in which the various triptans may be helpful, based on the results of meta-analyses of large scale controlled trials19-21 and clinical experience.
New treatments and unmet needs
Three unmet needs come readily to mind—new preventive drugs, acute treatments without vascular effects, and new strategies for managing intractable migraine.
Preventive drugs—On average, two thirds of patients will have a 50% reduction in headache frequency with most preventive drugs.22 They can then choose between the potential for sleepiness, exercise intolerance, erectile impotence, nightmares, dry mouth, weight gain, tremor, hair loss, or fetal deformities as possible side effects. The fact that migraineurs are prepared to accept such side effects indicates the level of disability they experience. The recent positive results from clinical trials of topiramate show its utility in migraine.23,24 Table 2 shows the range of options for prevention, none of which is ideal.
Table 2.
Preventive treatments in migraine*
| Agent | Dose* | Selected side effects |
|---|---|---|
| Commonly used drugs | ||
| Pizotifen | 0.5-2 mg daily | Weight gain, drowsiness |
| β blocker (propranolol) | 40-120 mg twice daily | Reduced energy, tiredness, postural symptoms, contraindicated in asthma |
| Ticyclics (amitriptyline, dothiepin, nortriptyline) | 25-75 mg nightly | Drowsiness (some patients are very sensitive and may need only a total dose of 10 mg, though 1-1.5 mg/kg body weight is generally required for a response) |
| Anticonvulsants: | ||
| Valproate | 400-600 mg twice daily | Drowsiness, weight gain, tremor, hair loss, fetal abnormalities, haematological or liver abnormalities |
| Topiramate | 25-100 mg twice daily | Paraesthesiae, cognitive dysfunction, weight loss, renal stones, glaucoma |
| Gabapentin | 900-3600 mg daily | Dizziness, sedation |
| Methysergide | 1-4 mg daily | Drowsiness, leg cramps, hair loss, retroperitoneal fibrosis (1 month drug holiday required every 6 months) |
| Flunarizine | 5-10 mg daily | Drowsiness, weight gain, depression, parkinsonism |
| Metabolic enhancers | ||
| Riboflavin | 400 mg daily | |
| Coenzyme Q10 | 100 mg thrice daily | |
| Non-pharmaceuticals | ||
| Feverfew | ||
| Butterbur | ||
|
Other preventives with controlled evidence for efficacy
| ||
| Lisinopril | 10-20 mg daily | Cough |
| Candesartan | 16 mg daily | |
|
No convincing controlled evidence
|
|
|
| Verapamil | ||
|
Shown to have no effect by controlled trials
|
|
|
| Nimodipine | ||
| Clonidine | ||
| Fluoxetine | ||
Usual doses and common side effects are given, but the local national formulary should be consulted for detailed information.
Non-vascular acute treatments are required for those patients who cannot take triptans and ergot derivatives. Publication of a clinical trial where BIBN4096BS, a potent calcitonin gene-related peptide (CGRP) antagonist, was effective in treating acute migraine,25 simultaneously answers the question of whether nerves or blood vessels are of primary pathophysiological importance and provides the promise of a new treatment that is safe for patients with cardiovascular disorders. This advance was predicted by laboratory work more than a decade ago,w12 w13 and the translation of the basic experimental work to clinical practice illustrates the importance of basic neurobiology to advancing clinical practice. It is now clear that vasoconstriction is not necessary for aborting acute migraine, recently confirmed by the demonstration that sildenafil, a phosphodiesterase inhibitor, can induce migraine without changes in cerebral vessel diameter.
Box 4: Clinical stratification of acute migraine treatments
Failed analgesics or NSAIDs
First tier—Sumatriptan 50 mg or 100 mg, rizatriptan 10 mg, almotriptan 12.5 mg, eletriptan 40 mg, zolmitriptan 2.5 mg (all tablets)
For slower effect or better tolerability—Naratriptan 2.5 mg, frovatriptan 2.5 mg (tablets)
Infrequent headache—Ergotamine 1-2 mg tablet, dihydroergotamine nasal spray 2 mg
Early nausea or difficulties taking tablets
• Sumatriptan 20 mg nasal spray, zolmitriptan 5 mg nasal spray, rizatriptan 10 mg dissolvable wafer, zolmitriptan 2.5 mg dispersible
Headache recurrence
• Ergotamine 2 mg (perhaps most effective taken rectally, usually with caffeine), naratriptan 2.5 mg tablet, eletriptan 80 mg tablet
Poor tolerance of acute treatments
• Naratriptan 2.5 mg, frovatriptan 2.5 mg (tablets)
Early vomiting
• Sumatriptan 25 mg suppository, sumatriptan 6 mg subcutaneous injection
Menstrually related headache
Prevention—Ergotamine tablet taken at night, oestrogen patches
Treatment—Triptans, dihydroergotamine nasal spray
Rapidly developing symptoms
• Sumatriptan 6 mg subcutaneous injection, dihydroergotamine 1 mg intramuscular injection
Treatment for intractable migraine—Patients with intractable migraine require a new way forward, this may at last be at hand. Controlled observations of occipital nerve stimulation in chronic migraine are extremely promising.16 There is good evidence from animal studies of a clear interaction between trigeminal and cervical afferents in the trigeminocervical complex, and a controlled trial has been initiated to examine this approach.
The future for migraine sufferers seems bright as the combination of good clinical research, basic neuroscience, and clinical investigation is delivering both understanding and new treatments for this common and disabling disorder.
Further reading
Lance JW, Goadsby PJ. Mechanism and management of headache. 7th ed. New York: Elsevier, 2005.
Silberstein SD, Lipton RB, Goadsby PJ, Smith RT. Headache in primary care. 1st ed. Oxford: Isis Medical Media, 1999.
Olesen J, Tfelt-Hansen P, Ramadan N, Goadsby PJ, Welch KMA. The headaches. Philadelphia: Lippincott, Williams, and Wilkins, 2005.
International Headache Society (IHS). www.i-h-s.org/
Supplementary Material
 Extra references w1-w13 appear on bmj.com
Extra references w1-w13 appear on bmj.com
Funding: PJG's work has been supported by the Wellcome Trust and the Migraine Trust.
Competing interests: PJG has consulted for or received support for research from the pharmaceutical companies Almirall, Amgen, Advanced Bionics, AstraZeneca, Janssen, Medtronic, MSD, GSK, Pozen, and Pfizer.
References
- 1.Menken M, Munsat TL, Toole JF. The global burden of disease study—implications for neurology. Arch Neurol 2000;57: 418-20. [DOI] [PubMed] [Google Scholar]
- 2.Goadsby PJ. Advances in headache management. In: Haskard D, ed. Horizons in medicine. Vol 17. London: Royal College of Physicians, (in press).
- 3.Headache Classification Committee of the International Headache Society. The international classification of headache disorders (second edition). Cephalalgia 2004;24(suppl 1): 1-160. [DOI] [PubMed] [Google Scholar]
- 4.Tepper SJ, Dahlof CG, Dowson A, Newman L, Mansbach H, Jones M, et al. Prevalence and diagnosis of migraine in patients consulting their physician with a complaint of headache: data from the landmark study. Headache 2004;44: 856-64. [DOI] [PubMed] [Google Scholar]
- 5.Goadsby PJ, Dodick D, Silberstein SD. Chronic daily headache for clinicians. Hamilton, Canada: BC Decker, 2005.
- 6.Goadsby PJ, Boes C. New daily persistent headache. J Neurol Neurosurg Psychiatr 2002;72(suppl 2): ii6-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goadsby PJ. To scan or not to scan in headache: that is the question. BMJ 2004;329: 469-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiller C, May A, Limmroth V, Juptner M, Kaube H, Schayck RV, et al. Brain stem activation in spontaneous human migraine attacks. Nature Med 1995;1: 658-60. [DOI] [PubMed] [Google Scholar]
- 9.May A, Kaube H, Buechel C, Eichten C, Rijntjes M, Jueptner M, et al. Experimental cranial pain elicited by capsaicin: a PET-study. Pain 1998;74: 61-6. [DOI] [PubMed] [Google Scholar]
- 10.May A, Bahra A, Buchel C, Frackowiak RSJ, Goadsby PJ. Hypothalamic activation in cluster headache attacks. Lancet 1998;352: 275-8. [DOI] [PubMed] [Google Scholar]
- 11.Matharu MS, Cohen AS, Frackowiak RSJ, Goadsby PJ. Posterior hypothalamic activation in paroxysmal hemicrania. Ann Neurol (in press). [DOI] [PubMed]
- 12.Afridi S, Giffin NJ, Kaube H, Friston KJ, Ward NS, Frackowiak RSJ, et al. A PET study in spontaneous migraine. Arch Neurol 2005;62: 1270-5. [DOI] [PubMed] [Google Scholar]
- 13.Denuelle M, Fabre N, Payoux P, Chollet F, Gereud G. Brainstem and hypothalamic activation in spontaneous migraine attacks. Cephalalgia 2004;24: 775-814. [DOI] [PubMed] [Google Scholar]
- 14.Bahra A, Matharu MS, Buchel C, Frackowiak RSJ, Goadsby PJ. Brainstem activation specific to migraine headache. Lancet 2001;357: 1016-7. [DOI] [PubMed] [Google Scholar]
- 15.Afridi S, Matharu MS, Lee L, Kaube H, Friston KJ, Frackowiak RSJ, et al. A PET study exploring the laterality of brainstem activation in migraine using glyceryl trinitrate. Brain 2005;128: 932-9. [DOI] [PubMed] [Google Scholar]
- 16.Matharu MS, Bartsch T, Ward N, Frackowiak RSJ, Weiner RL, Goadsby PJ. Central neuromodulation in chronic migraine patients with suboccipital stimulators: a PET study. Brain 2004;127: 220-30. [DOI] [PubMed] [Google Scholar]
- 17.May A, Buchel C, Turner R, Frackowiak RSJ, Goadsby PJ. Neurovascular dilatation of intracranial vessels in experimental headache. Cephalalgia 1999;19: 464-5. [Google Scholar]
- 18.May A, Buchel C, Turner R, Goadsby PJ. MR-angiography in facial and other pain: neurovascular mechanisms of trigeminal sensation. J Cereb Blood Flow Metab 2001;21: 1171-6. [DOI] [PubMed] [Google Scholar]
- 19.Tfelt-Hansen P. Efficacy and adverse events of subcutaneous, oral, and intranasal sumatriptan used for migraine treatment: a systematic review based on number needed to treat. Cephalalgia 1998;18: 532-8. [DOI] [PubMed] [Google Scholar]
- 20.Ferrari MD, Goadsby PJ, Roon KI, Lipton RB. Triptans (serotonin, 5-HT1B/1D agonists) in migraine: detailed results and methods of a metaanalysis of 53 trials. Cephalalgia 2002;22: 633-58. [DOI] [PubMed] [Google Scholar]
- 21.Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine. A comparative review of pharmacology, pharmacokinetics and efficacy of triptans in migraine. Drugs 2000;6: 1259-87. [DOI] [PubMed] [Google Scholar]
- 22.Silberstein SD, Goadsby PJ. Migraine: preventative treatment. Cephalalgia 2002;22: 491-512. [DOI] [PubMed] [Google Scholar]
- 23.Brandes JL, Saper JR, Diamond M, Couch JR, Lewis DW, Schmitt J, et al. Topiramate for migraine prevention: a randomized controlled trial. JAMA 2004;291: 965-73. [DOI] [PubMed] [Google Scholar]
- 24.Silberstein SD, Neto W, Schmitt J, Jacobs D. Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol 2004;61: 490-5. [DOI] [PubMed] [Google Scholar]
- 25.Olesen J, Diener H-C, Husstedt I-W, Goadsby PJ, Hall D, Meier U, et al. Calcitonin gene-related peptide (CGRP) receptor antagonist BIBN4096BS is effective in the treatment of migraine attacks. N Engl J Med 2004;350: 1104-10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


