Abstract
Background: Providing patients with an audiotape of their medical consultation has been a relatively common practice in oncology clinics for some years. However, broader generalisability of the technique has yet to be examined.
Aims: To investigate the efficacy of providing patients with an audiotape of their consultation in a general practice setting.
Design of study: Randomised controlled trial: 95 experimental participants, 85 controls.
Setting: Routine surgeries run by two general practitioners (GPs) in two different health centres.
Method: All patients attending GP appointments were eligible for inclusion. Patients were followed up by telephone 7–10 days later.
Results: More than half (61%) of the patients who received a tape listened to it. Among listeners, 64% rated the tape useful or very useful; 24% noticed information not heard in the consultation. Half of listeners (46%) said that their understanding of the consultation improved after listening to the tape. Half of the listeners (48%) shared the tape with others, of whom 71% found sharing helpful or very helpful. However, 21% of those who shared the information with others found this unhelpful or very unhelpful, suggesting that patients may need to be briefed on the potential risks of sharing. At follow-up a week later, it emerged that being given a tape had no effect on adherence with GPs' advice, nor on anxiety about conditions.
Conclusion: Providing patients with an audiotape of their GP consultation was positively rated by many patients. Although there were no detectable clinical effects at follow-up, the technique merits further evaluation in general practice.
Keywords: anxiety, family practice, patient compliance, physician–patient relations, randomised controlled trial, tape recording
Introduction
THE potential benefits of providing medical patients with an audiotaped recording of a consultation were first written about 25 years ago.1 A recent review of studies carried out in oncology units concluded that audiotapes were preferred by patients over a summary letter, created less clinical workload than summary letters, and were well received by patients and their families.2 Tapes are listened to by about three-quarters of the patients who take a tape home, and the majority of them share it with one or more relatives or family friends.3 Averaging across studies, roughly 80% of those who listen to an audiotape of their medical consultation rate it as useful or very useful.4 Oncology studies have reported the technique's positive contribution to:
patient satisfaction with treatment,2
reducing anxiety and depression,4
increasing patient–practitioner partnership,5
increasing patient recall,6 and
helping patients share information about their medical condition with people in their support network.7
Audiotapes of a consultation comprise a personal and wholly relevant information package, especially when compared with alternative supplementary information such as leaflets or general videotapes.8 Offering patients the option of an audiotape also locates the patient–doctor relationship in a more egalitarian framework.9 McConnell et al10 noted a gradually increasing endorsement among medical practitioners for patients having personalised information about their illness. This runs parallel to recent National Health Service (NHS) endorsement of patient empowerment and improved partnership between doctor and patient,11 as well as the Department of Health's recent support for developing expert patient models.12 Most studies evaluating audiotapes of consultations have taken place in oncology clinics, usually with a single clinician,7 and few have been well-controlled experiments.13 The present study investigates audiotapes in general practice, and comprises the first investigation of their use in family medicine. The aims of the study are:
To assess the efficacy of taping consultations from patients' points of view.
To examine whether patients who are provided with a tape show better adherence to general practitioner (GP) advice.
To examine whether patients who are provided with a tape express less anxiety than controls when asked about their condition at follow-up.
HOW THIS FITS IN
What do we know?
Providing patients with a tape recording of their medical consultation is well known for its efficacy in oncology clinics.
What does this paper add?
This study is the first randomised controlled trial of the technique in general practice. Although being given a tape had no measurable clinical effects, patients' assessments of being given a tape were primarily positive. For example, more than half of the experimental group listened to the tape, two-thirds of listeners rated it helpful, and a quarter of listeners noticed new information from the consultation. Given the low cost and minimal time needed to use tapes as an aid to patient communication, they could make a modest contribution to clinical efficacy.
Method
The study comprised a randomised controlled trial, approved by the University of Ulster Local Research Ethics Committee. A consolidated standard for reporting clinical trials (CONSORT) flow diagram (Figure 1) details the sample and process of the study.
Figure 1.
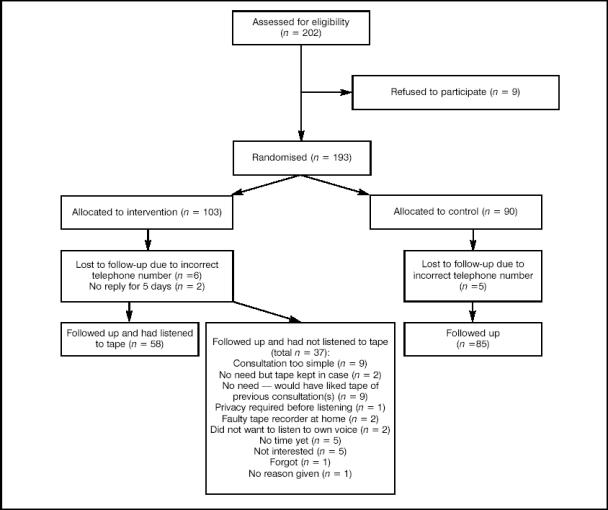
Details of sample.
Consenting patients (n = 193) were recruited from two Northern Ireland general practice surgeries as they arrived for routine appointments. All consenters had their consult-ation audiotaped. Patients were assigned to experimental and control groups at the end of the consultation, by choosing between two upturned beakers under which discs had been placed. A red disc assigned them to the experimental group (n = 103), and these patients were given their audiotape to take home. A blue disc assigned patients as controls (n = 90); their tapes were placed in a sealed disposal unit. To help ensure that patients trusted the randomisation procedure, both beakers were scrambled around before being choosen. After assignment to the appropriate group, patients were then shown the colour of the disc under the remaining cup — a sometimes neglected element of achieving informed consent from patients, who may otherwise doubt whether the discs were of a different colour, or wonder whether they had in fact been pre-assigned to a particular group.14 Before leaving, patients scrambled the beakers again ready for the next patient. A member of the health centre's support staff completed a form detailing consenters' age, sex, and consulting frequency over the previous 6 months.
After 7–10 days, a researcher contacted experimental and control patients by telephone. Patients were identifiable only by code number, telephone number, and first name.
Measures and scoring
Measures were selected with four considerations in mind:
Minimal time should be required by patients in order to participate in the study.
Measures were generic enough to suit the wide range of ailments about which patients were consulting their GP.
Measures were robust enough to permit reasonably accurate responses from patients after a 7-day time lapse between consultation and follow-up.
Measures were suitable for a short telephone follow-up, rather than paper-and-pencil administration.
The most important consideration was that patients should not have to invest much time participating in the study. People attending their GP for a routine appointment were unlikely to return detailed questionnaires through a postal follow-up, and were equally unlikely to consent to a telephone follow-up lasting more than 10 minutes. The aim of this study was to assess tape efficacy in the widest GP context, and patients who dropped out at the review stage, or did not consent in the first place because the study required effort, would have biased the results. Hence, each variable comprised a single-item measure rated on a 4- or 5-point Likert scale. Table 1 describes the measures in brief, with a fuller account contained in Supplementary Tables 1 and 2.
Table 1.
Measures used to assess the effects of audiotape provision.
| Variable | Measure used | ||
|---|---|---|---|
| Matching variables (gathered from all participants) | Age | ||
| Sex | |||
| Frequency of consultation in last 6 months | |||
| Control over condition: extent to which patients felt they could maintain good health through their own actions | 4-point scale | ||
| Understanding: patients rated how much they understood the consultation at the time they left the GP | 5-point scale | ||
| Satisfaction: patients rated their satisfaction with the consultation at the time they left the GP | 5-point scale | ||
| Outcome variables (all participants) | Adherence: level of concordance with GP's advice at the time of follow-up | 5-point scale | |
| Anxiety: how anxious patients felt at time of follow-up | 5-point scale | ||
| Tape use: | |||
| All | How many times listened? | ||
| Non-listeners | Reason for not listening | ||
| Listeners | Understanding of consultation: after listening to the tape | 5-point scale | |
| Usefulness of tape | 5-point scale | ||
| Extra information: item(s) on the tape that had not been heard during the consultation | Yes/No | ||
| Did anyone else listen? | Yes/No | ||
| Who? | |||
| How helpful was sharing the tape? | 5-point scale | ||
Experimental and control groups were compared using an intention-to-treat paradigm, that is, the experimental group includes all the original patients who were intended for treatment, regardless of whether they had listened to the tape or not.15
Statistical methods
Descriptive statistics and 95% confidence intervals (CIs) for the differences between the means of the experimental and control groups on the patient characteristics are listed in Table 2. A 2 × 2 between subjects analysis of variance was performed on ‘anxiety about condition at follow-up’ and ‘adherence with doctor's advice’. Independent variables were sex and treatment (tape/no tape), factorially combined. Analyses were performed using SPSS for Windows version 10, using a Type III Method for decomposing the sums of squares. This corresponds to Overall and Spiegel's16 Method 1, which Tabachnik and Fidell17 recommend for non-orthogonal designs of this nature. Because of the risk of a Type I error introduced by the testing of multiple statistical hypotheses, a more rigorous level of P<0.01 was applied when assessing statistical significance.
Table 2.
Patient characteristics: experimental and control groups.
| Measure | Total | Tape | No tape | 95% CI for differences between means |
|---|---|---|---|---|
| Total participants | 180 | 95 | 85 | |
| Females | 88 | 43 | 45 | |
| Males | 92 | 52 | 40 | |
| Mean age in years | 40 | 40 | 39 | |
| Control over condition: mean rating (SD) where 4 = very high control | 2.15 (1.12) | 2.15 (1.10) | 2.15 (1.15) | −0.33 to 0.34 |
| Mean consultation frequency in past 6 months (SD) | 1.09 (0.81) | 1.09 (0.86) | 1.09 (0.75) | −0.24 to 0.24 |
| Pre-tape understanding of consultation: mean rating (SD) where 4 = very good | 3.76 (0.45) | 3.73 (0.49) | 3.80 (0.40) | −0.06 to 0.21 |
| Pre-tape satisfaction with consultation: mean rating (SD) where 4 = very good | 3.73 (0.59) | 3.75 (0.60) | 3.71 (0.57) | −0.21 to 0.13 |
aSD = standard deviation.
Prior to carrying out the factorial analysis of variance between groups (ANOVAs), a power analysis was conducted.18 This indicated that with n = 200, α = 0.05 and a small-to-medium effect size (for example F = 0.20) the power of a test for the two main effects and the interaction effect would be 0.80 for the primary outcome, namely ‘anxiety about condition’. Setting the α level to 0.01 for the secondary outcome, ‘adherence with doctor's advice’, yielded a power value of 0.59.
Results
As indicated in Figure 1, 202 patients were asked to participate in the study, nine refused, and 13 (eight experimental, five control) were lost at follow-up (mainly because of incorrect mobile telephone numbers). This yielded a final sample of 95 experimental patients and 85 controls. Patients lost at follow-up did not differ greatly in age, sex, or consulting frequency from those patients who were traced. Table 2 outlines patient characteristics. As expected, experimental and control groups were equivalent in aspects such as age, sex, and mean consulting frequency. Patients had derived a generally high level of understanding and satisfaction from their consultation, even before the experimental group took the tape home.
Tape usage
More than half (61%) of patients who were offered a tape had listened to it by 7–10 days post-consultation. In most instances, the tape was listened to one or two times (mean = 1.5). About half (48%) of the patients who listened to their tape also shared it with others, usually their spouse. Almost three-quarters (71%) of patients who shared a tape with others rated this as ‘helpful’ or ‘very helpful’, although 21% of sharers found sharing ‘somewhat unhelpful’ or ‘very unhelpful’. Two-thirds of those who listened to the tape (64%) rated it as useful or very useful. Additionally, 46% of listeners said that the tape improved their understanding of the consultation. A quarter of listeners (24%) noticed additional information on the tape.
Experimental participants who had not listened to the tape (n = 37), were asked if there was any particular reason why they had not done so. Of these, two patients had encountered faulty tape recorders, one patient was awaiting privacy, and two said they still intended to listen. A quarter of those who declined to listen to the tape (26%) felt that it had not been needed because their consultation had been straightforward, and/or for a very simple health matter, such as a sore throat. Nine of these patients would have liked a tape of one or more previous consultations with their GP.
Exploratory analyses using binary logistic regression compared listeners with non-listeners in terms of age, sex, number of previous consultations, satisfaction with the consultation, understanding of consultation, and control over condition. None of these factors differentiated listeners from non-listeners.
Experimental and control group comparisons
As noted earlier, experimental and control group comparisons were carried out using an intention-to-treat paradigm; results are contained in Tables 3, 4 and 5. For ‘anxiety about condition’ there was neither a significant sex difference in the scores, nor was there a significant difference in anxiety between the tape/no tape groups. The interaction effect was also non-significant.
Table 3.
Experimental and control group comparisons for outcome variables.
| Outcome measure | Total | Tape | No tape | 95% CI for differences between means |
|---|---|---|---|---|
| Level of anxiety about condition at follow-up: mean rating (SD) where 4 = very anxious | 1.44 (1.46) | 1.21 (1.35) | 1.69 (1.54) | 0.06 to 0.91 |
| Adherence with doctor's advice at follow-up: mean rating (SD) where 4 = adhered entirely with doctor's advice | 3.61 (0.79) | 3.63 (0.73) | 3.58 (0.85) | −0.29 to 0.18 |
aSD = standard deviation.
Table 4.
Analysis of variance for anxiety about condition at follow-up.
| Source | Sum of squares | Degrees of freedom | Mean squares | f | P-value | Partial eta squareda |
|---|---|---|---|---|---|---|
| Sex | 1.33 | 1 | 1.33 | 0.65 | 0.421 | 0.004 |
| Tape/no-tape | 10.19 | 1 | 10.19 | 4.97 | 0.027 | 0.027 |
| Sex × tape/no-tape | 8.24 | 1 | 8.24 | 4.02 | 0.046 | 0.022 |
| Error | 360.59 | 176 | 2.05 | |||
| Corrected totalb | 380.33 | 179 |
aPartial eta squared is SS effect/(SS effect + SS error) where SS effect is the sum of squares for the main or interaction effect and SS error is the sum of squares for the error term. It indicates the proportion of variance of the dependent variable that is accounted for by a particular main or interaction effect.
bTotals are corrected for degrees of freedom, therefore they are not the sum of squares.
Table 5.
Analysis of variance for adherence with general practitioners' advice.
| Source | Sum of squares | Degrees of freedom | Mean squares | f | P-value | Partial eta squareda |
|---|---|---|---|---|---|---|
| Sex | 2.35 | 1 | 2.35 | 3.84 | 0.052 | 0.021 |
| Tape/no-tape | 0.22 | 1 | 0.22 | 0.36 | 0.551 | 0.002 |
| Sex × tape/no-tape | 1.02 | 1 | 1.02 | 1.67 | 0.199 | 0.009 |
| Error | 107.65 | 176 | 0.61 | |||
| Corrected totalb | 110.99 | 179 |
aPartial eta squared is SS effect/(SS effect + SS error) where SS effect is the sum of squares for the main or interaction effect and SS error is the sum of squares for the error term. It indicates the proportion of variance of the dependent variable that is accounted for by a particular main or interaction effect.
bTotals are corrected for degrees of freedom, therefore they are not the sum of squares.
A similar analysis was carried out using ‘adherence with doctor's advice’ as the dependent variable. As indicated in Tables 3 and 5, experimental and control groups did not greatly differ in their adherence rates, nor was there any main effect for sex, nor any interaction between tape/no-tape and sex. The probability values given in Table 5 should be regarded as approximate, since the data were negatively skewed — the majority of patients rated their adherence as being either very high (76%) or high (12%).
Discussion
Summary of main findings
Every patient attending a consultation during the data collection phase was eligible for inclusion. Although the study detected no significant clinical effects at follow-up, more than half (61%) of the experimental group listened to their audiotape. This represents a high participation rate, given that several factors mitigated against tape usage.
When non-listeners were asked if there was any particular reason why they had not listened to the tape, the most common explanation given (by 26%) was that they had attended the GP about very minor issues, and saw no need to listen to the tape. Additionally, at follow-up patients rated their understanding of, and satisfaction with, the consultation (as they perceived these when they left the surgery) very highly. Given these factors, listening rates seem highly satisfactory, comparing well with rates of between 56%19 and 75%7 that have been reported in oncology studies.
Although 46% of those who had listened to their tape said that it improved their understanding of the consultation, a larger number (64%) of listeners rated their tape as ‘useful’ or ‘very useful’. Given the same mitigating factors that are mentioned previously, this compares well with 81%4 to 96%7 of oncology patients who gave tapes a favourable usefulness rating. Taken together, these data suggest that some of the benefits of tapes go beyond a simple process of improved comprehension. An opportunity to share information with others might have been an additional advantage, since half (48%) of the patients who listened to the tape also shared it with others.
Of those who shared the tape with others, sharing was rated ‘helpful’ or ‘very helpful’ by almost three-quarters (71%). Some of the benefit participants see in tapes might lie in the potential that such tapes afford for accurate sharing of information. On the negative side however, 21% of sharers found the sharing ‘somewhat’ or ‘very unhelpful’. When selecting patients suitable for taping, GPs may wish to consider potential negative effects of sharing, and patients may need to be advised about the risks associated with this.
A quarter (24%) of listeners heard information they had not heard during the consultation, compared with 61% of cancer patients.8 This is likely to be the result of routine GP consultations being typically less stressful experiences, and to there being less new information to take in.
Strengths and limitations of this study
The measures used in the study were single items rated on a 4- or 5-point scale. This ensured that patients were required to invest relatively little time and effort in the study and helped ensure high levels of participation and follow-up. Through this an unbiased assessment of tape efficacy in general practice could be made. However, more detailed measures, perhaps using postal follow-up and paper and pencil assessments, could be considered for future studies.
The study did not explore a sustained programme of providing patients with audiotapes, that is, across several consultations. Schapira et al,5 for example, reported that cancer patients become more active in their decision-making over time, after their involvement in recording. Ford et al6 also highlighted the value of using the next consultation as a follow-up measure, reporting an increase in patient requests for clarification based on what they had heard on the tape.
Patients might also be able to use a more regular prov-ision of tapes as a means for honing their doctor–patient communication skills. As McGee and Cegala20 argued, considerable attention has been given to the enhancement of doctors' communication skills, although patients too might benefit from tools that help them articulate their concerns.
The longer-term benefits of sharing the tape with others also cannot be estimated from the present study. Researchers have hypothesised that sustained effects on adherence can be mediated through the network of family members with whom information has been shared.21
Implications for future research and clinical practice
Given that patients rated their level of understanding/satisfaction with the consultation highly on leaving the surgery, results are moderately encouraging in terms of patient uptake and subsequent responses to having received a tape. The recording process, when used routinely, takes only seconds to set up, as does offering a patient the tape at the end of a consultation. As such, it is a time-efficient means of improving communication, and one which could usefully supplement the range of techniques GPs are currently employing to achieve better doctor–patient understanding.
Although there are risks associated with sharing tapes, further research could explore whether these may be outweighed by potential benefits to sustained adherence — particularly in conditions where patients are counselled at the outset about risks associated with sharing the tape.
In addition, studies could explore whether audiotapes in general practice might benefit certain types of patients more than others. For example, in paediatric consultations children are commonly accompanied by a parent or caregiver. Since children are also commonly cared for by other caregivers, the opportunity to share a tape might be especially useful. Additionally, the distractions of managing a child in the GP's surgery may mean that a caregiver misses some elements of advice; these can be picked up when a tape is listened to later.
Many elderly patients, too, are cared for by others, particularly when they are ill. Some elderly patients might also experience difficulty hearing information, concentrating on the consultation for several minutes, or remembering the advice given. Benefits could also extend into other areas of health centre service: for example, where complex or detailed guidelines are being given to patients (perhaps by dieticians or diabetic clinic nurses) tape recordings could prove a valuable asset, both in terms of letting other family members have access to the guidelines, and in terms of assisting patients with recall.
Supplementary Information
Additional information accompanies this paper at: http://www.rcgp.org.uk/journal/index.asp
Supplementary Material
Acknowledgments
The study was funded by the Primary Care Development Fund, Northern Health and Social Services Board, Northern Ireland. Jacq Wray, Eleanor Craig, and the staff in both health centres assisted with data collection. Participating patients are thanked for their cooperation.
References
- 1.Butt HR. A method for better physician — patient communication. Ann Intern Med. 1977;86:478–480. doi: 10.7326/0003-4819-86-4-478. [DOI] [PubMed] [Google Scholar]
- 2.Bruera E, Pituskin E, Calder K, et al. The addition of an audiocassette recording of a consultation to written recommendations for patients with advanced cancer. Cancer. 1999;86:2420–2425. [PubMed] [Google Scholar]
- 3.Ah-Fat FG, Sharma MC, Damato BE. Taping outpatient consultations: a survey of attitudes and responses of adult patients with ocular malignancy. Eye. 1998;12:789–791. doi: 10.1038/eye.1998.204. [DOI] [PubMed] [Google Scholar]
- 4.Thomas R, Daly M, Perryman B, Stockton D. Forewarned is forearmed — benefits of preparatory information on video cassette for patients receiving chemotherapy or radiotherapy — a randomised controlled trial. Eur J Cancer. 2000;356:1536–1543. doi: 10.1016/s0959-8049(00)00136-2. [DOI] [PubMed] [Google Scholar]
- 5.Schapira MM, Meade C, Nattinger AB. Enhanced decision-making: the use of a videotape decision-aid for patients with prostate cancer. Patient Educ Couns. 1997;30:119–127. doi: 10.1016/s0738-3991(96)00943-3. [DOI] [PubMed] [Google Scholar]
- 6.Ford S, Fallowfield L, Hall A, Lewis S. The influence of audiotapes on patient participation in the cancer consultation. Eur J Cancer. 1995;31A:2264–2269. doi: 10.1016/0959-8049(95)00336-3. [DOI] [PubMed] [Google Scholar]
- 7.Ong LML, Visser MRM, Lammes FB, et al. Effect of providing cancer patients with the audiotaped initial consultation on satisfaction, recall, and quality of life: a randomised, double-blind study. J Clin Oncol. 2000;18:3052–3060. doi: 10.1200/JCO.2000.18.16.3052. [DOI] [PubMed] [Google Scholar]
- 8.Wicklin N, Forster J. The effects of a personal versus a factual approach videotape on the level of preoperative anxiety of same day surgery patients. Patient Educ Counsel. 1994;23:107–114. doi: 10.1016/0738-3991(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 9.Noble LM. Doctor–patient communication and adherence to treatment. In: Myers L, Midence K, editors. Adherence to treatment in medical conditions. Amsterdam: Harwood Academic Publishers; 1998. pp. 51–82. [Google Scholar]
- 10.McConnell D, Butow PN, Tattersall MHN. Audiotapes and letters to patients: the practice and views of oncologists, surgeons, and general practitioners. Br J Cancer. 1999;79:1782–1788. doi: 10.1038/sj.bjc.6690284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health. The NHS Plan. A plan for investment: a plan for reform. London: Department of Health; 2003. http://www.dh.gov.uk/PolicyAndGuidance/OrganisationPolicy/Modernisation/NHSPlan/fs/en?CONTENT_ID=4082690&chk=/DU1UD (accessed 15 Jul 2004) [Google Scholar]
- 12.Tattersall R. The expert patient: a new approach to chronic disease management for the twenty-first century. Clin Med. 2002;2:227–229. doi: 10.7861/clinmedicine.2-3-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McClement SE, Hack TF. Audio-taping the oncology treatment consultation: a literature review. Patient Educ Couns. 1999;36:229–238. doi: 10.1016/s0738-3991(98)00095-0. [DOI] [PubMed] [Google Scholar]
- 14.Featherstone K, Donovan JI. Random allocation or allocation at random? Patients' perspectives of participation in a randomised controlled trial. BMJ. 1998;317:1177–1180. doi: 10.1136/bmj.317.7167.1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frangakis CE, Rubin DB. Addressing complications of intention-to-treat analysis in the combined presence of all-or-none treatment-noncompliance and subsequent missing outcomes. Biometrika. 1999;86:365–379. [Google Scholar]
- 16.Overall JE, Spiegel DK. Concerning least squares analysis of experimental data. Psych Bull. 1969;72:311–322. [Google Scholar]
- 17.Tabachnick GD, Fidell LS. Using multivariate statistics. 3rd edn. New York: Harper Collins; 1996. [Google Scholar]
- 18.Buchner A, Erdfelder E, Faul F. How to use G power. 28 March 2001. http://www.psycho.uni-duesseldorf.de/aap/projects/gpower/how_to_use_gpower.html (1 Sept. 2003)
- 19.de Wit R, van Dam F, Zandbelt L. A pain education program for chronic cancer patients: follow-up from a randomised controlled trial. Pain. 1997;73:55–69. doi: 10.1016/s0304-3959(97)00070-5. [DOI] [PubMed] [Google Scholar]
- 20.McGee DS, Cegala DJ. Patient communication skills training for improved communication competence in the primary care medical consultation. J Appl Commun Res. 1998;26:412–430. [Google Scholar]
- 21.Haerem JW, Ronning EJ, Leidal R. Home access to hospital discharge information on audiotape reduces sick leave and readmissions in patients with first-time myocardial infarction. Scand Cardiovasc J. 2000;34:219–222. doi: 10.1080/14017430050142297. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


