Abstract
Background: Reliable longitudinal data of patients with functional somatic symptoms in general practice are lacking.
Aims: To identify distinctive features in patients with chronic functional somatic symptoms, and to determine whether these symptoms support the hypothesis of the existence of specific somatic syndromes.
Design of study: Observational study, with a comparison control group.
Setting: Four primary care practices affiliated with the University of Nijmegen in the Netherlands.
Method: One hundred and eighty-two patients diagnosed between 1998 and 2002 as having chronic functional somatic symptoms and 182 controls matched by age, sex, socioeconomic status, and practice were included. Data on comorbidity, referrals, diagnostic tests, and hospital admissions over a period of 10 years prior to the diagnosis were collected. Medication use and number of visits to the general practitioner (GP) were extracted from the moment computerised registration was started.
Results: In the 10 years before the diagnosis of chronic functional somatic symptoms, significantly more patients than controls presented functional somatic symptoms in at least two body systems, and used more somatic and psychotropic drugs. They visited the GP twice as much, statistically had significantly more psychiatric morbidity, and were referred more often to mental health workers and somatic specialists. The number of patients undergoing diagnostic tests was higher for patients with chronic functional somatic symptoms than for controls, but hospital admissions rates were equal.
Conclusion: Patients with chronic functional somatic symptoms have a great diversity of functional somatic symptoms. They use more somatic and psychotropic drugs than controls in the years before diagnosis. Moreover, they show high rates of referrals and psychiatric morbidity. The diversity of symptoms of patients with chronic functional somatic symptoms supports the concept that symptoms do not cluster in well defined distinct syndromes. Therefore, patients with chronic functional somatic symptoms should preferably not be classified into medical subspecialty syndromes.
Keywords: somatoform disorders, psychophysiologic disorders, family practice, referral and consultation, comorbidity
Introduction
MEDICALLY unexplained symptoms are common, and account for one in five new consultations in primary care.1,2 In 25–50% of all primary care visits, no serious medical (that is, organic) cause is found to explain the patient's presenting symptom, and 20–40% of the patients seen by medical specialists do not receive a clear diagnosis.3,4 The presented symptoms are then referred to as ‘medically unexplained’ or ‘functional’.5 Functional, or rather medically unexplained, somatic symptoms are ranked second on the list of the 10 most common physical symptoms in primary care and have an incidence rate of 70 per 1000 patient years in the Netherlands.6
Although an occasional visit to the general practitioner (GP) for a functional somatic symptom seems natural, repeated consultations because of these symptoms rep-resent a serious problem. Patients who do this are often diagnosed as having ‘chronic functional somatic symptoms’. Psychological distress or psychosocial problems are presumed to be the underlying causes.7 As such, diagnosing chronic functional somatic symptoms requires the patient to repeatedly present physical symptoms that remain medically unexplained after adequate examination, and indications from the patient's personal circumstances of presumed psychosocial problems or psychological distress. When experiencing functional somatic symptoms seems to have become a regular way of presenting, a patient is registered as having chronic functional somatic symptoms.
As patients with chronic functional somatic symptoms are functionally impaired, have high rates of comorbid psychiatric disorders, and are at risk of unnecessary diagnostic procedures and treatments,1,4,8-11 a correct diagnosis is of paramount importance. However, most research on this topic has been performed either on unselected population-based samples,12,13 or in selected patients referred to secondary care.14,15 Moreover, most of these studies make use of questionnaires in which patients have to recall a variety of symptoms existing for a considerable amount of time.10,16,17 This method has been shown to produce unstable results in which lifetime symptoms present at baseline are not remembered at follow-up.18 Research on patients from primary care settings in whom the diagnosis had been made on reliable longitudinal data is generally lacking.
Moreover, there is considerable debate regarding the question of whether functional somatic symptoms cluster in well defined distinct syndromes, such as fibromyalgia, chronic fatigue syndrome, or tension headache, or whether these specific somatic syndromes are largely an artefact of medical specilisation.7,19 In this debate reliable data on primary care patients are also needed, whereas most research on this topic is performed in referred populations20,21 concentrating on specific symptoms,22-24 or in community samples25 using questionnaires in which inconsistencies of recall may have a great effect on the assessment of the ultimate diagnosis.18,26
HOW THIS FITS IN
What do we know?
For some 25–50% of patients accessing primary care, no serious medical reason can be given to explain their presenting symptoms. Patients with chronic functional somatic symptoms are restricted in daily life because they have both psychological and somatic symptoms.
What does this paper add?
In the 10 years before the diagnosis of chronic functional somatic symptoms patients have a great diversity of functional somatic symptoms. This supports the concept that patients do not cluster in specific somatic syndromes. Although the number of visits is twice as frequent, patients with chronic functional somatic symptoms do not have more somatic self-limiting or chronic disorders than controls, but the use of somatic and psychotropic drugs is much higher.
The aims of this study, therefore, are to explore with longitudinal data:
how and how often patients with chronic functional somatic symptoms present to their GP and other medical institutions,
whether patients with chronic functional somatic symptoms indeed present more functional somatic symptoms in the years before the diagnosis,
if symptoms presented by patients with chronic functional somatic symptoms support the existence of specific somatic syndromes.
Method
Continuous Morbidity Registration database
This study uses data from the Continuous Morbidity Registration (CMR) database, a project of the Department of Family Medicine of the University of Nijmegen in the Netherlands.27-30 This project was started in 1971 in four practices in and around Nijmegen31 and monitors a pop-ulation of approximately 12 000 patients, representative of the Dutch population with regard to age and sex. Every episode of illness seen by, or reported to, the GP is registered as soon as it is established using an adapted version of the E-list.32 Diagnoses and codes are corrected when necessary. Over many years, monthly meetings of all GPs involved are held to discuss classification problems, to monitor the application of diagnostic criteria, and to discuss coding problems of hypothetical case histories. As well as medical data, the following information is available: age, sex, socioeconomic status (low, middle and high), and marital status. In the beginning the registration was performed on the medical chart; since 1994 a computerised registration has been used.
Patients with chronic functional somatic symptoms
We selected all patients from the CMR database in whom chronic functional somatic symptoms were diagnosed for the first time between 1998 and 2002 (n = 182). For a per-iod of 10 years before this diagnosis, the following variables had been collected: sociodemographic characteristics; morbidity data; and data on referrals, diagnostic tests, and hospital admissions. Use of medical facilities was assessed by the number of contacts with the GP. Data on medication use could be extracted from when computerised regist-ration started, and medication data were transformed into the prescribed daily dose by using the Anatomical Therapeutical Chemical Classification/Defined Daily Doses (ATC/DDD) system.33 As a proxy of somatic morbidity, we assessed three prevalent categories of chronic disorders (diabetes mellitus, asthma/chronic obstructive pulmonary disease [COPD], and cardiovascular diseases) and three prevalent categories of self-limiting disorders (skin, musc-uloskeletal, and airway) in order to study the hypothesis that patients with chronic functional somatic symptoms are at risk of somatic morbidity.37
We allocated the registered functional somatic symptoms to specific body systems; for example, gastrointestinal or musculoskeletal, as described by Escobar et al.10 Irritable bowel syndrome and hyperventilation syndrome, sometimes regarded as medically unexplained symptoms, are not included in this study.
Controls
For each patient with chronic functional symptoms, a control matched by age, sex, socioeconomic status, and practice was drawn from the CMR population. The only exclusion criterion in the control group was the diagnosis of chronic functional somatic symptoms. Patients who were controls had to have had at least one registered episode of illness during the per-iod they had been on the practice list. For controls, the same information as described for patients with chronic functional somatic symptoms was obtained from 1990–2000.
Statistical methods
Our analysis primarily involved comparing patients with chronic functional somatic symptoms with their matched controls. Statistical analyses were conducted using SPSS 9.0. Descriptive statistics were calculated for all variables. The data on specific body systems were analysed using exploratory factor analysis, and then simplified by varimax rotation. The χ2 test and student's t-test were used for comparing means of consultations and medication use in both groups. Odds ratios (ORs) and 95% confidence intervals (CIs) were used as the main measurement for assoc-iations, particularly with regard to functional somatic symptoms, comorbidity, referrals, diagnostic tests, and hospital admissions. All P-values are two-tailed.
Results
Characteristics of subjects
Of the 182 patients with chronic functional somatic symptoms included in the study, 141 (77.5%) were women; the mean age of all patients was 42.0 years (range = 10–85 years). Most subjects were of low (44.5%) or middle (42.9%) socioeconomic class.
Functional somatic symptoms
The incidence rate of patients with chronic functional somatic symptoms was 3.5 per 1000 patient years, whereas the prevalence of patients known to have chronic functional somatic symptoms is established on 68.8 per 1000 patient years.
The presented functional somatic symptoms in various body systems in patients and controls is displayed in Table 1. For each symptom group, patients and controls differ significantly (P<0.05). It is remarkable that many patients had symptoms in various body systems — a finding that is supported by the factor analysis (Figure 1) — as it is often considered that there are a number of well-defined distinct functional somatic syndromes, clustering around physical symptoms of one body system. Moreover, factor analysis suggests that, on the one hand, gastrointestinal, cardiorespiratory, and pseudopsychiatric symptoms are linked and, on the other, that pseudoneurological symptoms, musculoskeletal symptoms, and headache and other pain, are linked with each other. Significantly more patients than controls presented symptoms in two or more body systems (87.9% versus 19.8%; OR = 29.5, 95% CI = 16.0 to 54.9). Of all the patients, 25% presented symptoms in four or more body systems.
Table 1.
Distribution of functional somatic symptoms in the various body systems (n = 182).
| Patients (%) | Controls (%) | Odds ratio (95% CI)a | |
|---|---|---|---|
| Pseudoneurological | 54 (29.7) | 13 (7.1) | 5.5 (2.8 to 11.1) |
| Gastrointestinal | 69 (37.9) | 15 (8.2) | 6.8 (3.6 to 13.1) |
| Musculoskeletal | 58 (31.9) | 6 (3.3) | 13.7 (5.5 to 36.5) |
| Cardiorespiratory | 74 (40.7) | 16 (8.8) | 7.1 (3.8 to 13.5) |
| Headache and other pain | 80 (44.0) | 15 (8.2) | 8.7 (4.6 to 16.6) |
| Pseudopsychiatric | 150 (82.4) | 48 (26.4) | 13.1 (7.7 to 22.4) |
| Others | 66 (36.3) | 10 (5.5) | 9.8 (4.6 to 12.2) |
| Unknown | 67 (36.8) | 0 (0) | - |
aStatistically significant difference between patients and controls.
Figure 1.
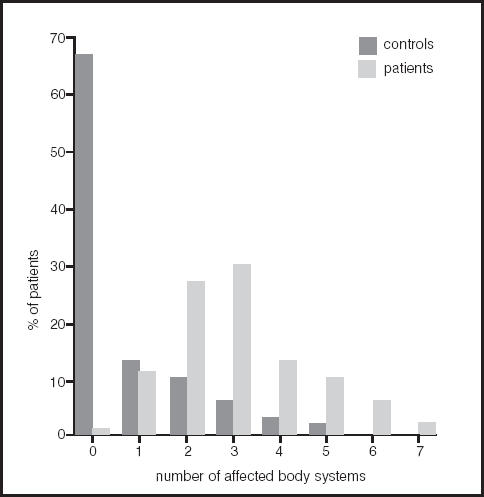
Symptom diversity in patients with chronic functional somatic symptoms and their matched controls.
Half of the patients had three or more episodes of functional somatic symptoms before he or she was diagnosed as having chronic functional somatic symptoms; 25% of patients had five or more episodes before chronic functional somatic symptoms were diagnosed.
Comorbidity: somatic and psychiatric
Patients with chronic functional somatic symptoms had significantly more psychiatric disorders in comparison with controls (OR = 2.4) (Table 2). Patients did not have a much higher rate of chronic and self-limiting somatic comorbidity, and they had only slightly more episodes of self-limiting airway problems than controls.
Table 2.
Number of consultations, comorbidity, referrals, diagnostic tests, and hospital admissions in patients and controls (n = 182).
| Patients | Controls | P-value | Odds ratio (95% CI) | |
|---|---|---|---|---|
| GP consultations in 1 yeara (mean [range]) | ||||
| Practice visits | 9.8 (2.5–26.8) | 4.2 (0–15.1) | <0.001b | – |
| Home visits | 0.2 (0–3.5) | 0.3 (0–7.1) | 0.53 | – |
| Comorbidity (n [%]) | ||||
| Somatic chronic: | ||||
| Diabetes mellitus | 5 (2.7) | 4 (2.2) | – | 1.3 (0.3 to 5.7) |
| Asthma/COPD | 20 (11.0) | 10 (5.5) | – | 2.1 (0.9 to 5.0) |
| Cardiovascular | 16 (8.8) | 8 (4.4) | – | 2.1 (0.8 to 5.5) |
| Somatic self-limiting | ||||
| Skin | 96 (52.7) | 82 (45.1) | – | 1.4 (0.9 to 2.1) |
| Musculoskeletal | 130 (71.4) | 115 (63.2) | – | 1.5 (0.9 to 2.3) |
| Airway | 136 (74.4) | 113 (62.1) | – | 1.8 (1.1 to 2.9)b |
| Psychiatricc | 41 (22.5) | 20 (11.0) | – | 2.4 (1.3 to 4.4)b |
| Referrals (n [%]) | ||||
| Somatic: medical | 130 (71.4) | 97 (53.3) | – | 2.2 (1.4 to 3.5)b |
| Somatic: paramedicald | 129 (70.9) | 87 (47.8) | – | 2.6 (1.7 to 4.2)b |
| Mental health | 59 (32.4) | 15 (8.2) | – | 5.3 (2.8 to 10.3)b |
| Diagnostic teste (n [%]) | 156 (85.7) | 140 (76.9) | – | 1.8 (1.0 to 3.2)b |
| Hospital admissions (n [%]) | ||||
| Somatic | 57 (31.3) | 51 (28.0) | – | 1.2 (0.7 to 1.9) |
| Psychiatric | 1 (0.5) | 1 (0.5) | – | 1.0 |
an = 118: one general practice did not use the computerised registration, so consultation could not be established in this practice.
bStatistically significant difference between patients and controls P<0.05.
cIncluding schizophrenia, depression, psychoses, hysteria, phobia, neuroses, post-traumatic stress disorder, alcoholism, use of street drugs.
dIncluding physiotherapist, dietician.
eIncluding haematological tests, x-ray examinations, ultrasonography, and electrocardiography.
Consultations, referrals, diagnostic tests and hospital admissions
The number of consultations in patients with chronic functional somatic symptoms is significantly higher (n = 9.8 versus n = 4.2, P<0.001), as is the number of subjects referred for diagnostic testing (n = 156 versus n = 140, OR = 1.8). The number of home visits was equal in both groups. About three-quarters of patients had been referred to somatic specialists, compared with about half of the controls. About one-third of the patients had been referred to mental health sources compared with less than 10% in controls. Hospital admissions were the same. These data are outlined in Table 2.
Medication use
The results regarding medication use are detailed in Table 3. We found that patients with chronic functional somatic symptoms used significantly more somatic medications (2.6 versus 1.5, P<0.001) and psychotropic drugs (0.4 versus 0.05, P<0.001) per year compared with controls. The number of patients using antidepressants and benzodiazepines is statistically different in both groups (35.6% versus 5.9%; 52.5% versus 12.7% respectively, P<0.001).
Table 3.
Medication use in patients and controlsa (n = 118).
| Patients | Controls | P-value | Odds ratio (95% CI) | |
|---|---|---|---|---|
| Number of somatic medications per year (mean [range]) | 2.6 (0–18.0) | 1.5 (0–7.5) | <0.001b | – |
| Number of psychotropic drugs per year (mean [range]) | 0.4 (0–9.0) | 0.05 (0–0.62) | <0.001 | – |
| Number of patients using psychotropic drugs (n [%]) | ||||
| Antidepressants | 42 (35.6) | 7 (5.9) | – | 7.5 (3.1 to 18.9) |
| Benzodiazepines | 62 (52.5) | 15 (12.7) | – | 5.8 (3.0 to 11.1) |
| Others | 3 (2.5) | 3 (2.5) | – | 1.0 |
| Days of psychotropic drug use per year (median [range]) | ||||
| Antidepressants | 19.5 (1.9–297.0)c | 5.0 (1.62–91.7)d | – | – |
| Benzodiazepines | 8.9 (0.4–322.5)c | 4.2 (1.1–90.8)d | – | – |
| Others | 34.3 (1.7–58.2)c | 3.8 (0.2–25.1)d | – | – |
| Prescribed daily doses (mean [range]) | ||||
| Antidepressants | 0.76 (0.20–1.37)c | 0.77 (0.13–2.00)d | – | – |
| Benzodiazepines | 0.62 (0.06–1.50)c | 0.61 (0.20–1.54)d | – | – |
| Others | 0.51 (0.25–0.75)c | 0.31 (0.25–0.40)d | – | – |
an = 118: one general practice did not use the computerised registration, so medication could not be established in this practice.
bStatistically significant difference between patients and controls P<0.05.
cFor patients with antidepressants, benzodiazepines and other psychotropic drugs, n = 42, 62, and 3, respectively.
dFor patients with antidepressants, benzodiazepines and other psychotropic drugs, n = 7, 15, and 3, respectively.
In patients using medication, antidepressants were used for a mean of 20 days a year and benzodiazepines for 9 days a year compared with 5 and 4 days, respectively, in controls. However, these findings do not reach statistical significance. Moreover, there is no difference in prescribed daily dose for patients and controls.
Discussion
Strengths and limitations of this study
The strength of the present study is that the patients who were included were those who consulted their GP, irrespective of the presented symptoms. Therefore, a threshold of relevance of the symptoms for the patient was established and we were able to analyse all symptoms presented. Most population-based studies assess all symptoms irrespective of the perceived need for help.10,16,17 Moreover, in popul-ation-based studies, interviewing patients repeatedly does not lead to a consistent classification of somatoform disorders,18 whereas our classification of the presented morbidity is based on very stable data,29,34 in which longitudinal research is allowed and recall bias will not occur.
The limitations of the study are the retrospective use of data in existing medical records and the possible interdoctor variation of the diagnosis of chronic functional somatic symptoms.35 The interdoctor variation is partly a con-sequence of not having explicitly stated criteria for chronic functional somatic symptoms in the CMR. This subjectivity will possibly always exist because diagnosing chronic functional somatic symptoms remains an interpretation of the symptoms, and is influenced by foreknowledge and context.27 However, it is known from the literature that the GP's judgement on somatisation seems valid in daily practice. Moreover, additional validation of clinical judgement is possible through longitudinal follow-up.36 The subjectivity of the diagnosis and the doctor–patient relationship also make important contributions to the genesis and persistence of functional somatic symptoms.37 The doctor's knowledge of the patient's complaints is an important issue and is associated with a better outcome.
Of all the variables described, only consultation frequency is directly linked with the diagnosis of chronic functional somatic symptoms — as such, the higher frequency of GP visits was to be expected a priori.38
Summary of main findings
This is the first observational study using longitudinal data describing patients in whom consulting the GP for functional somatic symptoms has become a regular way of presenting. During the 10 years before a diagnosis of chronic functional somatic symptoms is established by the GP, patients consult their GP twice as much, use much more somatic and psychotropic medication, have more psychiatric morbidity and are more often referred to mental health workers than controls. During these 10 years, the number of diagnostic tests is slightly higher in patients and the number of hospital admissions is equal in comparison with controls. Patients with chronic functional somatic symptoms are more likely to present symptoms in two or more body systems and they present a higher number and greater diversity of symptoms to the GP than control patients. GPs in this study appear to classify patients as having chronic functional somatic symptoms after three episodes of presenting with functional somatic symptoms.
Comparison with the existing literature
The finding that patients could be recognised as having chronic functional somatic symptoms after they had exp-erienced three episodes of functional somatic symptoms presented in two or more body systems, is an important one. Functional somatic symptoms are often recognised after having excluded other possible diagnoses. This may be associated with unnecessary and possibly harmful diagnostic strategies and may promote somatic fixation. Early identification of these patients could prevent somatic fixation, and enables the GP to modify his/her proceedings.39 Additionally, this finding was confirmed using factor analysis and shows that functional somatic symptoms probably do not cluster in well defined specific somatic syndromes. It also suggests that symptom variation is great in these patients.
The concept of patients with functional somatic syndromes presenting symptoms in many body systems has also been supported by recent studies.20 Therefore, the existence of specific somatic syndromes should be challenged. With a broad-based approach, the GP might be the appropriate practitioner to diagnose and treat these patients by emph-asising the biomedical as well as the psychosocial factors involved in symptom production and perception.40
The finding that patients with chronic functional somatic symptoms did not have a higher rate of chronic and self-limiting somatic comorbidity is remarkable because it is stated in the literature that somatisation with more frequent examination may increase the chance of chronic diseases being discovered.36 We found that more frequent consultation did not lead to more diagnosed chronic and self-limiting diseases in patients with chronic functional somatic symptoms.
The diagnosis of chronic functional somatic symptoms is not recorded as such in the DSM-IV classification. It no doubt exists as part of the spectrum somewhere between somatisation disorder and somatoform disorder not otherwise specified. The condition resembles the concept of ‘abridged somatisation’,10 but is not based on the number of symptoms. Both ‘abridged somatisation’ and chronic functional somatic symptoms presume underlying psychological distress. The prevalence of somatisation disorder according to the DSM-IV in primary care is low because of the stringent criteria.40,41 On the other hand, less severe forms of somatisation have a major impact on quality of life and on the use of health services, and are more prevalent.
Implications for further research and clinical practice
Patients with chronic functional somatic symptoms may be considered as persistent complainers and consequently labelled as ‘difficult’ patients. The condition may indeed reflect a greater propensity to complain; however, as is apparent from the excess of psychiatric comorbidity, patients with chronic functional somatic symptoms also have more reason to complain. With regard to these patients, it seems that consulting the GP for functional somatic symptoms has become a regular way of presenting, but it might also be that patients who attend more often are at higher risk of being considered as having chronic functional somatic symptoms. Moreover, the diagnosis might relate to frustrated doctors as a consequence of lack of understanding, or failures in the communication between doctor and patient.
Chronic functional somatic symptoms are a major cause of morbidity and deserve further investigation to estimate the importance of the doctor–patient relationship, the feasibility of treatments, and the understanding of the aetiology of functional symptoms to identify patients who are likely to become persistent complainers and develop the behavioural pattern of patients with chronic functional somatic symptoms.
Also, the overlap of chronic functional somatic symptoms with the various DSM-IV diagnoses should be studied. This is important because the validity of the classification of mental disorders is useful, but also questionable.42 Thinking in narrow syndromes might hinder an appropriate interpretation of the patient's syndromes.
Patients repeatedly presenting functional somatic symptoms to the GP in two or more body systems, particularly when combined with psychological complaints, should be regarded as candidates for the diagnosis of chronic functional somatic symptoms. It seems that the presented functional somatic symptoms are part of a single syndrome and that symptom variation is great in these patients. Therefore, the GP, who is considered as being knowledgeable about underlying psychosocial problems, should diagnose, treat, and accompany these patients.
Acknowledgments
We are grateful to the GPs and practice nurses for being able to carry out our research work in their CMR practices, and we would like also to thank Ank de Jonge and Vivien Moffat for reviewing the manuscript.
References
- 1.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86(3):262–266. doi: 10.1016/0002-9343(89)90293-3. [DOI] [PubMed] [Google Scholar]
- 2.Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29(6):563–569. doi: 10.1016/0022-3999(85)90064-9. [DOI] [PubMed] [Google Scholar]
- 3.Bass C. Somatisation: physical symptoms and psychological disorder. Oxford: Oxford University Press; 1990. [Google Scholar]
- 4.Barsky AJ, Borus JF. Somatisation and medicalisation in the era of managed care. JAMA. 1995;274(24):1931–1934. [PubMed] [Google Scholar]
- 5.Trimble MR. Functional diseases. Br Med J (Clin Res Ed) 1982;285(6387):1768–1770. doi: 10.1136/bmj.285.6357.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van de Lisdonk EH, van den Bosch WJ, Huygen FJA, Lagro-Janssen ALM. Psychische en Psychiatrische stoornissen. Ziekten in de huisartspraktijk. Nijmegen: Elsevier/Bunge; 1999. [Psychological and psychiatric disorders. Morbidity in general practice] [Google Scholar]
- 7.Barsky AJ, Borus JF. Functional somatic syndromes. Ann Intern Med. 1999;130(11):910–921. doi: 10.7326/0003-4819-130-11-199906010-00016. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59(Suppl 20):15–21. [PubMed] [Google Scholar]
- 9.Smith GR, Jr, Monson RA, Ray DC. Patients with multiple unexplained symptoms. Their characteristics, functional health, and health care utilisation. Arch Intern Med. 1986;146(1):69–72. [PubMed] [Google Scholar]
- 10.Escobar JI, Waitzkin H, Silver RC, Gara M, Holman A. Abridged somatisation: a study in primary care. Psychosom Med. 1998;60(4):466–472. doi: 10.1097/00006842-199807000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Katon W, Von Korff M, Lin E, et al. Distressed high utilisers of medical care. DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12(6):355–362. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- 12.Escobar JI, Golding JM, Hough RL, et al. Somatisation in the community: relationship to disability and use of services. Am J Public Health. 1987;77(7):837–840. doi: 10.2105/ajph.77.7.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fink P. The use of hospitalisations by persistent somatising patients. Psychol Med. 1992;22(1):173–180. doi: 10.1017/s0033291700032827. [DOI] [PubMed] [Google Scholar]
- 14.Golding JM, Smith GR, Jr, Kashner TM. Does somatisation disorder occur in men? Clinical characteristics of women and men with multiple unexplained somatic symptoms. Arch Gen Psychiatry. 1991;48(3):231–235. doi: 10.1001/archpsyc.1991.01810270043006. [DOI] [PubMed] [Google Scholar]
- 15.Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med. 1990;150(8):1685–1689. doi: 10.1001/archinte.150.8.1685. [DOI] [PubMed] [Google Scholar]
- 16.deGruy F, Columbia L, Dickinson P. Somatisation disorder in a family practice. J Fam Pract. 1987;25(1):45–51. [PubMed] [Google Scholar]
- 17.Feder A, Olfson M, Gameroff M, et al. Medically unexplained symptoms in an urban general medicine practice. Psychosomatics. 2001;42(3):261–268. doi: 10.1176/appi.psy.42.3.261. [DOI] [PubMed] [Google Scholar]
- 18.Simon GE, Gureje O. Stability of somatisation disorder and somatisation symptoms among primary care patients. Arch Gen Psychiatry. 1999;56(1):90–95. doi: 10.1001/archpsyc.56.1.90. [DOI] [PubMed] [Google Scholar]
- 19.Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354(9182):936–939. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- 20.Nimnuan C, Rabe-Hesketh S, Wessely S, Hotopf M. How many functional somatic syndromes? J Psychosom Res. 2001;51(4):549–557. doi: 10.1016/s0022-3999(01)00224-0. [DOI] [PubMed] [Google Scholar]
- 21.Nimnuan C, Hotopf M, Wessely S. Medically unexplained symptoms: an epidemiological study in seven specialities. J Psychosom Res. 2001;51(1):361–367. doi: 10.1016/s0022-3999(01)00223-9. [DOI] [PubMed] [Google Scholar]
- 22.Wessely S, Chalder T, Hirsch S, et al. Psychological symptoms, somatic symptoms, and psychiatric disorder in chronic fatigue and chronic fatigue syndrome: a prospective study in the primary care setting. Am J Psychiatry. 1996;153(8):1050–1059. doi: 10.1176/ajp.153.8.1050. [DOI] [PubMed] [Google Scholar]
- 23.Fukuda K, Dobbins JG, Wilson LJ, et al. An epidemiologic study of fatigue with relevance for the chronic fatigue syndrome. J Psychiatr Res. 1997;31(1):19–29. doi: 10.1016/s0022-3956(96)00046-5. [DOI] [PubMed] [Google Scholar]
- 24.Hickie I, Lloyd A, Hadzi-Pavlovic D, et al. Can the chronic fatigue syndrome be defined by distinct clinical features? Psychol Med. 1995;25(5):925–935. doi: 10.1017/s0033291700037417. [DOI] [PubMed] [Google Scholar]
- 25.Komaroff AL, Fagioli LR, Doolittle TH, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996;101(3):281–290. doi: 10.1016/S0002-9343(96)00174-X. [DOI] [PubMed] [Google Scholar]
- 26.Feinstein AR, Josephy BR, Wells CK. Scientific and clinical problems in indexes of functional disability. Ann Intern Med. 1986;105(3):413–420. doi: 10.7326/0003-4819-105-3-413. [DOI] [PubMed] [Google Scholar]
- 27.Van Weel-Baumgarten EM, van den Bosch WJ, van den Hoogen HJ, Zitman FG. The validity of the diagnosis of depression in general practice: is using criteria for diagnosis as a routine the answer? Br J Gen Pract. 2000;50(453):284–247. [PMC free article] [PubMed] [Google Scholar]
- 28.Van Weel-Baumgarten E, van den Bosch W, van den Hoogen H, Zitman FG. Ten year follow-up of depression after diagnosis in general practice. Br J Gen Pract. 1998;48:1643–1646. [PMC free article] [PubMed] [Google Scholar]
- 29.Van Weel C. Validating long term morbidity recording. J Epidemiol Community Health. 1995;49(Suppl 1):29–32. doi: 10.1136/jech.49.suppl_1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Weel C, Smith H, Beasley JW. Family practice research networks. Experiences from 3 countries. J Fam Pract. 2000;49(10):938–943. [PubMed] [Google Scholar]
- 31.Van Weel C, van den Bosch WJ, van den Hoogen HJ, Smits AJ. Development of respiratory illness in childhood — a longitudinal study in general practice. J R Coll Gen Pract. 1987;37(302):404–408. [PMC free article] [PubMed] [Google Scholar]
- 32.Eimerl TS. Organised curiosity. A practical approach to the problem of keeping records for research purposes in general practice. J Coll Gen Pract. 1960;3:246–252. [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organisation. Guidelines for ATC classification and DDD assignment. Oslo: World Health Organisation; 1996. [Google Scholar]
- 34.Van den Bosch WJ, Huygen FJ, van den Hoogen HJ, van Weel C. Morbidity in early childhood: differences between girls and boys under 10 years old. Br J Gen Pract. 1992;42(362):366–369. [PMC free article] [PubMed] [Google Scholar]
- 35.Reid S, Crayford T, Richards S, Nimnuan C, Hotopf M. Recognition of medically unexplained symptoms — do doctors agree? J Psychosom Res. 1999;47(5):483–485. doi: 10.1016/s0022-3999(99)00052-5. [DOI] [PubMed] [Google Scholar]
- 36.Schilte AF, Portegijs PJ, Blankenstein AH, Knottnerus JA. Somatisation in primary care: clinical judgement and standardised measurement compared. Soc Psychiatry Psychiatr Epidemiol. 2000;35(6):276–282. doi: 10.1007/s001270050239. [DOI] [PubMed] [Google Scholar]
- 37.Stewart MA, McWhinney IR, Buck CW. The doctor/patient relationship and its effect upon outcome. J R Coll Gen Pract. 1979;29(199):77–81. [PMC free article] [PubMed] [Google Scholar]
- 38.De Grauw WJ, van den Hoogen HJ, van de Lisdonk EH, et al. Control group characteristics and study outcomes: empirical data from a study on mortality of patients with type 2 diabetes mellitus in Dutch general practice. J Epidemiol Community Health. 1998;52(Suppl 1):9S–12S. [PubMed] [Google Scholar]
- 39.Grol R. To heal or to harm. The prevention of somatic fixation in general practice. London: Royal College of General Practitioners; 1981. [Google Scholar]
- 40.Katon W, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med. 2001;134(9 Pt 2):917–925. doi: 10.7326/0003-4819-134-9_part_2-200105011-00017. [DOI] [PubMed] [Google Scholar]
- 41.Katon W, Lin E, Von Korff M, et al. Somatisation: a spectrum of severity. Am J Psychiatry. 1991;148(1):34–40. doi: 10.1176/ajp.148.7.A34. [DOI] [PubMed] [Google Scholar]
- 42.Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160(1):4–12. doi: 10.1176/appi.ajp.160.1.4. [DOI] [PubMed] [Google Scholar]


